Abstract
We report a case of eczema-like cutaneous mucormycosis caused by Rhizopus arrhizus. A 4-year-old child was presented to our hospital with a history of gradually enlarging papule and plaque in the periumbilical area for nearly 4 years since 2 weeks after his birth, and it has been misdiagnosed as eczema for nearly 3 years. Based on histopathology examination, the fungus culture test and DNA sequencing, it was revealed that R. arrhizus should be the responsible fungus for skin infection. The patient was successfully cured by combination of intravenous drip and percutaneous injection amphotericin B for nearly 3 months, and no recrudescence was seen during a follow-up of 6-month observation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As a life-threatening disease, mucormycosis almost invariably occurs in immunocompromised patients, especially those with uncontrolled diabetes mellitus, neutropenia, organ transplant and even congenital immunodeficiency [1]. Mucormycosis generally progresses rapidly, with a high mortality rate, approximately ranging from 23 to 100% [2], which may be attributed to the delayed diagnosis and subsequent antifungal treatment, partly due to highly intrinsic resistance to many commonly used antifungal drugs. Mucormycosis has different clinical presentations including rhinocerebral, sinusal, pulmonary, cutaneous and disseminated as the main clinical forms, with various underlying and triggering risk factors [3]. The clinical presentations and prognosis are also associated with the isolated microorganism, and Rhizopus sp. is one of the most frequently isolated fungus [3]. However, cutaneous mucormycosis caused by Rhizopus arrhizus has been rarely reported, especially in child which is usually characterized by progressive swelling, ulceration, tissue necrosis, disfigurement and even death in severe cases. In recent years, our team has reported several primary cutaneous mucormycosis in China [4, 5], indicating focus on skin infection by Mucorales. Here, we report a case mucormycosis caused by R. arrhizus in a 4-year-old boy presenting as an eczema-like lesion in his periumbilical area and successfully treated by intravenous drip and percutaneous injection amphotericin B.
Case Presentation
In July 2017, a 4-year-old boy was admitted to our hospital with a history of gradually enlarging papule and plaque in the periumbilical area for nearly 4 years. Upon recalling his birth history, we found that this boy was born through full-term normal delivery and has normal birth weight. Since 2 weeks after his birth, a red papule was found near his navel without any obvious trauma. At first, it was misdiagnosed as bacterial folliculitis and treated with antibiotic ointment. As time going on, the papule grew in number and merged into plaque with erythema and without any exudation or scales in the periumbilical area. Then, it was misdiagnosed as eczema and prescribed with glucocorticoid cream for topically using. Only until histopathology examination of the skin lesion biopsy was done about a year before his admission to our hospital, mucormycosis was considered. So, itraconazole syrup (8 ml per day) and terbinaphthyl cream were prescribed for nearly 6 months. As a result, the lesions shrinked mildly without an anticipated improvement.
On physical examination, the patient had normal temperature, pulse, respiration and blood pressure. His body weight was 16 kg. A dark red, irregular plaque was seen on the patient’s periumbilical area in size of 7 × 10 cm, with some red papules distributed, but without exudation. The surface of the lesion was partially covered by very thin layers of scales with relatively clear boundary on the edge (Fig. 1a). The palpation revealed some deep nodules.
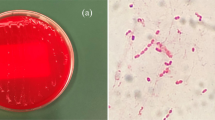
a A dark red, irregular plaque area in size of approximately 7 × 10 cm was seen on the patient’s periumbilical with some red papules distributed. b The lesion did not recede fast enough as expected upon prescribing amphotericin B (0.625 mg/kg/day) for 15 days. c Pigmentation left when he got out of hospital. d Hematoxylin-eosin (HE)-stained, e periodic-acid-Schiff (PAS)-stained and f periodic acid-silver metheramine (PASM) of histopathological specimen showed non-septate hyphae with pectinate hyphae with right-angled branching in the dermis (magnification, 200×). g Colonies of Rhizopus arrhizus grown on Sabouraud dextrose agar (SDA) at 26, 37 and 40 °C (from right to left). h Slide culture showed broad aseptate hyphae, sporangia and sporangiophores with opposite rhizoids (magnification, 200×). (Color figure online)
A histopathology examination with hematoxylin-eosin (HE)-stained (Fig. 1d), periodic-acid-Schiff (PAS)-stained (Fig. 1e) and periodic acid-silver metheramine (PASM) (Fig. 1f) sections revealed the presence of non-septate hyphae with pectinate hyphae with right-angled branching in the dermis, which are surrounded by mixed inflammatory cell composed of lymphocytes, neutrophils and multinucleated giant cells. For fungal identification, biopsy tissues were inoculated and cultured on Sabouraud dextrose agar (SDA) at 26, 37 and 40 °C (Fig. 1g). Microscopy result showed broad, aseptate hyphae, sporangia and rhizoids (Fig. 1h). DNA extraction was carried out for polymerase chain reaction by using fungus universal primers, and the sequence results were completely consistence with the records of R. arrhizus (GenBank Accession No. KF717369.1). It was diagnosed as mucormycosis caused by R. arrhizus consequently. Broth microdilution method (M38-A2) [6] was performed to determine susceptibility of antifungal agents. The MICs were amphotericin B (0.25 mg/ml), itraconazole (0.25 mg/ml), voriconazole (4 mg/ml), posaconazole (0.5 mg/ml), anidulafungin (> 8 mg/ml), micafungin (> 8 mg/ml) and fluconazole (> 256 mg/ml).
Based on the results of susceptibility of antifungal agents test, intravenous amphotericin B was used and it was started from 0.0625 to 0.625 mg/kg/day in the first 6 days and then sustained for 15 days. The lesion did not recede fast enough as expected (Fig. 1b); thus, amphotericin B was increased to 0.738 mg/kg/day and lasted for 20 days. During systematic using of amphotericin B, percutaneous injection amphotericin B was adopted at the same time. Many papules and plaque decreased significantly, only with pigmentation left (Fig. 1c). Further, the patient was recommended to continue treatment with itraconazole capsule (100 mg per day) for orally and amphotericin B for percutaneous injection for about 2 months after he got out of the hospital. The boy almost completely recovered, and no recrudescence was seen during a follow-up of 6-month observation.
Discussion and Conclusion
Mucormycosis (zygomycosis) is the third most common type of invasive fungal infection (IFI), and the mortality rate can be as high as more than 50% [7]. R. arrhizus is among the widespread species worldwide that can cause opportunistic infections for those with immune disturbance [8]. There have been more than 20 cases reported in mainland China, most of them are with diabetes mellitus or chronic renal failure, and there is only one child infected but resulting in death pitifully for aplastic anemia complications [9]. Though rare incidence in children, Rhizopus spp. is the second most common pathogen in children with invasive mold infections [10], and it is inclined to affect preterm or immunocompromised newborns in most cases [11, 12]. No predisposing conditions can be found in this boy.
Cutaneous mucormycosis caused by R. arrhizus is rarely reported compared with rhinocerebral and pulmonary infections, and it occurs mostly due to wound or disruption of cutaneous barrier [3]. But in this case reported, the parents denied any trauma since his birth. Hemorrhagic or necrotic tissue is the most common representation of cutaneous zygomycosis for its tendency to invade vessels, and bull’s eye appearance of skin has also been reported to be a distinct manifestation of mucormycosis [13], but eczema-like lesion can easily be misrecognized as eczema or dermatitis thus leading to improper treatment consequently. Julie L et al. once presented a 10-year-old acute myelogenous leukemia (AML) girl with a single erythematous plaque with annular bulla on her arm which was misdiagnosed as a reaction to insect bite initially, and diagnosis of zygomycosis was not made until histological examination [14]. In this case, similarly, the lesion did not possess any typical characteristics and the boy was treated inappropriately for more than 2 years, making conditions even worse. We can conclude that this is a rare case of primary cutaneous zygomycosis inflicts with an immunocompetent child imitating eczema atypically, and direct microscopy of the biopsy and culture confirmation are recommended when experiential treatment do not work well in clinical practice [15].
As for the treatment of mucormycosis, combination of amphotericin B and surgical debridement is highly recommended according to most reports [3, 8, 16,17,18]. And posaconazole as recorded has been an emerging agent to use in clinical, but data concerning with children are very limited [19,20,21,22]. Percutaneous injection of antifungal agents directly to the lesion can achieve the highest concentration at the site of infection [23], and this method can not only avoid long time using of antifungal agents but reduce the recurrence rate to some extent as well. Back in 2005, Zhang DL has used intralesional, intravenous and intrathecal amphotericin B to cure disseminated cryptococcosis successfully [24], and several cases have been reported about topical injection of amphotericin B in cutaneous leishmaniasis patients [23, 25, 26]. In this case presented, both intravenous drip and percutaneous injection of amphotericin B are adopted together and works better compared with oral itraconazole or intravenous amphotericin B alone. We can conclude that percutaneous injection of amphotericin B can serve as an effective supplementary method to treat cutaneous mucormycosis as well. However, decreased susceptibility of amphotericin B in Rhizopus spp. has been detected [27]. Thus, susceptibility test is strongly recommended upon diagnosis made in order to prescribe the most effective agents.
References
Binder U, Maurer E, Lass-Florl C. Mucormycosis—from the pathogens to the disease. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2014;20(Suppl 6):60–6. https://doi.org/10.1111/1469-0691.12566.
Barratt DM, Van Meter K, Asmar P, Nolan T, Trahan C, Garcia-Covarrubias L, et al. Hyperbaric oxygen as an adjunct in zygomycosis: randomized controlled trial in a murine model. Antimicrob Agents Chemother. 2001;45(12):3601–2. https://doi.org/10.1128/AAC.45.12.3601-3602.2001.
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41(5):634–53. https://doi.org/10.1086/432579.
Liang GZ, Xu WQ, Zheng XL, Mei H, Lv GX, Shen YN, et al. Successful treatment by surgery of a primary cutaneous mucormycosis caused by mucor irregularis. Mycopathologia. 2017. https://doi.org/10.1007/s11046-017-0219-4.
Lu XL, Liu ZH, Shen YN, She XD, Lu GX, Zhan P, et al. Primary cutaneous zygomycosis caused by rhizomucor variabilis: A new endemic zygomycosis? A case report and review of 6 cases reported from China. Clin Infect Dis. 2009;49(3):e39–43. https://doi.org/10.1086/600817.
CLSI. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi: Approved standard-Second Edition. CLSI document M38-A2. Wayne, PA: Clinical and Laborary Standards Institute; 2008.
Pana ZD, Seidel D, Skiada A, Groll AH, Petrikkos G, Cornely OA, et al. Invasive mucormycosis in children: an epidemiologic study in European and non-European countries based on two registries. BMC Infect Dis. 2016;16(1):667. https://doi.org/10.1186/s12879-016-2005-1.
Sundararajan T, Kumar CPG, Menon T, Rekha K, Venkatadesikalu M. Cutaneous zygomycosis due to Rhizopus oryzae in a patient with acute lymphoblastic leukemia. Mycoses. 2004;47:521–3.
Zhang AP, Liu W, Hu B. Cutaneous mucormycosis due to Rhizopus arrhizus: report 3 cases. J Clin Dermatol. 2012;41(3):163–5 (in Chinese with English abstract).
Wattier RL, Dvorak CC, Hoffman JA, Brozovich AA, Bin-Hussain I, Groll AH, et al. A prospective, international cohort study of invasive mold infections in children. J Pediatr Infect Dis Soc. 2015;4(4):313–22. https://doi.org/10.1093/jpids/piu074.
Prasad PA, Vaughan AM, Zaoutis TE. Trends in zygomycosis in children. Mycoses. 2012;55(4):352–6. https://doi.org/10.1111/j.1439-0507.2011.02124.x.
Dabritz J, Attarbaschi A, Tintelnot K, Kollmar N, Kremens B, von Loewenich FD, et al. Mucormycosis in paediatric patients: demographics, risk factors and outcome of 12 contemporary cases. Mycoses. 2011;54(6):e785–8. https://doi.org/10.1111/j.1439-0507.2011.02025.x.
Rubin AI, Grossman ME. Bull’s-eye cutaneous infarct of zygomycosis: a bedside diagnosis confirmed by touch preparation. J Am Acad Dermatol. 2004;51(6):996–1001. https://doi.org/10.1016/j.jaad.2004.07.027.
Cantatore-Francis JL, Shin HT, Heilman E, Glick SA. Primary cutaneous zygomycosis in two immunocompromised children. Pediatr Dermatol. 2007;24(3):257–62. https://doi.org/10.1111/j.1525-1470.2007.00398.x.
Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Chakrabarti A, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2014;20(Suppl 3):5–26. https://doi.org/10.1111/1469-0691.12371.
Martin LB, Rodriguez MAM, Mercier N, Lafont MO, Fernandez EO, de la Parte AR, et al. Rhizopus arrhizus invasive infection due to self-inflicted scratch injuries in a diabetic patient with non-ketotic acidosis. Mycopathologia. 2017;182(9–10):927–31. https://doi.org/10.1007/s11046-017-0158-0.
Zaoutis TE, Roilides E, Chiou CC, Buchanan WL, Knudsen TA, Sarkisova TA, et al. Zygomycosis in children: a systematic review and analysis of reported cases. Pediatr Infect Dis J. 2007;26(8):723–7. https://doi.org/10.1097/INF.0b013e318062115c.
Shoham S, Magill SS, Merz WG, Gonzalez C, Seibel N, Buchanan WL, et al. Primary treatment of zygomycosis with liposomal amphotericin B: analysis of 28 cases. Med Mycol. 2010;48(3):511–7. https://doi.org/10.3109/13693780903311944.
van Burik JAH, Hare RS, Solomon HF, Corrado ML, Kontoyiannis DP. Posaconazole is effective as salvage therapy in zygomycosis a retrospective summary. Clin Infect Dis. 2006;42:e61–5.
De Decker K, Van Poucke S, Wojciechowski M, Ieven M, Colpaert C, Vogelaers D, et al. Successful use of posaconazole in a pediatric case of fungal necrotizing fasciitis. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2006;7(5):482–5. https://doi.org/10.1097/01.pcc.0000235255.68759.05.
Snaith J, Burns K, Kok J, Chen S, Cheung NW. A case of rhino-orbital mucormycosis in diabetes with haematogenous cerebral spread. Med Mycol Case Rep. 2016;13:22–4. https://doi.org/10.1016/j.mmcr.2016.10.002.
Wildenbeest JG, Oomen MW, Bruggemann RJ, de Boer M, Bijleveld Y, van den Berg JM, et al. Rhizopus oryzae skin infection treated with posaconazole in a boy with chronic granulomatous disease. Pediatr Infect Dis J. 2010;29(6):578. https://doi.org/10.1097/INF.0b013e3181dc8352.
Mushtaq S, Dogra D, Dogra N. Clinical response with intralesional amphotericin B in the treatment of old world cutaneous leishmaniasis: a preliminary report. Dermatol Ther. 2016;29(6):398–405. https://doi.org/10.1111/dth.12377.
Zhang DL. Nursing experience of one child with disseminated cryptococcosis. Sichuan Med J. 2005;26(6):697–8 (in Chinese).
Nikandish M, Goyonlo VM, Taheri AR, Kiafar B. Ocular leishmaniasis treated by intralesional amphotericin B. Middle East Afr J Ophthalmol. 2016;23(1):153–5. https://doi.org/10.4103/0974-9233.171801.
Goyonlo VM, Vosoughi E, Kiafar B, Nahidi Y, Momenzadeh A, Taheri AR. Efficacy of intralesional amphotericin B for the treatment of cutaneous leishmaniasis. Indian J Dermatol. 2014;59(6):631. https://doi.org/10.4103/0019-5154.143571.
Vitale RG, de Hoog GS, Schwarz P, Dannaoui E, Deng S, Machouart M, et al. Antifungal susceptibility and phylogeny of opportunistic members of the order mucorales. J Clin Microbiol. 2012;50(1):66–75. https://doi.org/10.1128/JCM.06133-11.
Acknowledgements
This study was funded by Special Program for Basic work of science and technology, funded by the Ministry of Science and Technology of China (2013FY113700), supported by National Natural Science Foundation of China (81471905) and was funded by the Chinese Academy Medical Sciences Initiative for Innovative Medicine (2016-I2M-3-021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Handling Editor: Yuping Ran.
Mei-hua Fu and Jia Liu have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Fu, Mh., Liu, J., Liang, Gz. et al. Successful Treatment of Eczema-Like Mucormycosis in a Child by Combination of Intravenous Drip and Percutaneous Injection Amphotericin B. Mycopathologia 184, 309–313 (2019). https://doi.org/10.1007/s11046-018-0273-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-018-0273-6