Abstract
Recently, relentless efforts to develop rapid, cost-effective, and reliable laboratory methods for daily diagnosis of fungal diseases such as aspergillosis appear to be materialized in the relatively new, but revolutionary matrix-assisted laser desorption ionization-time-of-flight (MALDI-TOF) mass spectrometry (MS) technology. As for Aspergilli, MALDI-TOF MS profiling of isolates growing in culture—characteristic protein spectra are obtainable by means of simple and reproducible preanalytical and analytical procedures—ensures that single species within the different sections or complexes can be easily and accurately identified, including species that are morphologically and phylogenetically similar to each other. Thus, resort to longer and more onerous molecular biology techniques is restricted to those cases for which no spectra in the reference fungal database or library are available at the time of analysis. However, it is necessary to interrogate reference libraries composed of spectra that have been obtained using procedures similar to those used to obtain the test isolate’s mass spectrum, as well as to continuously update these libraries for enriching them with fungal strains/species not (or not well) represented in their current versions. Compared to mold identification, very limited work was reported on the use of MALDI-TOF MS to perform strain typing or antifungal susceptibility testing for Aspergilli. If these complementing areas will be potentiated in the near future, MALDI-TOF MS could effectively support the clinical microbiology/mycology laboratory in its primary role of assisting either infection control specialists or physicians for the diagnosis and treatment of aspergillosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
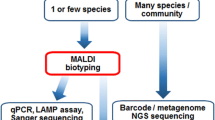
The clinical microbiology/mycology laboratory ability to diagnose fungal infections has been complicated over the recent years by the evolving and widening “spectrum” of human fungal pathogens, including those belonging to the genus Aspergillus [1]. By relying on the analysis of colony morphology and microscopic characteristics, phenotypic identification of filamentous fungi or molds is typically time-expensive and labor-consuming [2], and erroneous results may be produced even in experienced reference laboratories [3]. By contrast, new genomic and proteomic approaches are showing great potential for the identification of fungal pathogens, in addition to be more rapid and to need less skills in traditional identification techniques [4]. However, strict regulations severely limit the routine use of DNA-based molecular platforms for identification of filamentous fungi in many diagnostic laboratories [5], whereas mass spectrometry (MS) and specifically matrix-assisted laser desorption ionization-time-of-flight (MALDI-TOF) seems to meet all of key requirements for an efficient microbial diagnostic, including high throughput, specificity, and speed of analysis [6].
The genus Aspergillus comprises a large number of clinically relevant species, originally separated into various groups or sections (also called complexes) based on overlapping morphological features [7]. This makes the identification of different species within each of the Aspergillus species complexes very problematic by means of traditional macroscopic and microscopic analyses [8]. Thus, while clinical mycologists can still establish a species complex-level classification of Aspergillus isolates solely by morphological methods [9], the Aspergillus species delineation currently relies on phenotypic (morphology and extrolite profiles) and molecular (e.g., ITS, calmodulin, β-tubulin, actin) characters in a polyphasic approach [10]. However, partial β-tubulin or calmodulin sequences are now the most promising loci for robust species discrimination within a given Aspergillus species complex [9]. This is because of conventional loci—the nuclear ribosomal ITS regions (ITS1, 5.8S rRNA, and ITS2)—not variable enough to allow resolution of closely related species of filamentous fungi [4]. Using these additional loci, the number of species within Aspergillus section Fumigati now approaches 50 [11], and some of novel cryptic (or sibling) species—morphologically indistinguishable from each other but separable with only DNA-based molecular methods [12]—exhibit in vitro antifungal susceptibility profiles which differ significantly from that of Aspergillus fumigatus sensu stricto [13]. Accordingly, over 10 % of the isolates associated with invasive aspergillosis in transplant recipients—available from the US transplant-associated infection surveillance network—were found to be cryptic species, and several of these species, including Aspergillus lentulus (section Fumigati) and Aspergillus calidoustus (section Usti), had high in vitro minimum inhibitory concentrations (MICs) to antifungal agents [14].
As the precise recognition of individual species within the Aspergillus sections is a cornerstone of therapeutic decision making and disease outcome [15], clinical microbiology/mycology laboratories should routinely perform sequence-based identification on clinically relevant Aspergillus isolates [13]. However, this process needs to be overseen by a skilled molecular biologist to avoid potential errors in the species identification [16]. In addition, molecular biology techniques are able to separate the Aspergillus flavus/Aspergillus oryzae group from the Aspergillus parasiticus/Aspergillus sojae group within the Aspergillus section Flavi, but do not distinguish A. flavus—the second leading cause of human aspergillosis [17]—from A. oryzae, because of high-degree genetic identity between the two species [18]. Again in the section Flavi, it is not infrequent that Aspergillus nomius and Aspergillus tamarii—reported as causes of human infections in the last decade—are misidentified as A. flavus by conventional phenotypic methods [19], as well as it is not surprising that β-tubulin or the calmodulin gene are the gene target of choice for differentiating clinical isolates of A. flavus, A. nomius, and A. tamarii [20].
MALDI-TOF Mass Spectrometry in Clinical Mycology
Since fungal cultures remain integral also in a modern clinical mycology laboratory, the identification of colony-growing Aspergilli from patients’ specimens can be accelerated using the new proteomic technology MALDI-TOF MS, which has merited in 2009 the “revolutionary technique” designation [21] and is today perceived as a “fundamental shift” in the routine clinical microbiology practice [22]. Currently, two MALDI-TOF MS instruments are available in Europe for routine clinical microbiology, commercialized by Bruker Daltonics (Germany) and bioMérieux (France); while the first provides the MALDI Biotyper (software and database), the second includes the Vitek MS, and the SARAMIS (AnagnosTec, Germany) databases—referred to as Vitek MS IVD system. A third system, the Andromas SAS (France), provides a different type of database and software, but, at present, neither system is approved by the US Food and Drug Administration [23]. Theoretically, it is possible for users to create and/or supplement their own libraries of reference mass spectra by including locally important strains or species/strains not (or not well) represented in the commercial libraries, but this is actually more practicable with the Biotyper software [24].
The MALDI-TOF mass spectrum, generated from a given fungal isolate following a simple preparatory process, never matches a “main spectrum profile” (MSP) in the reference database with absolute identity. So, the result of mass spectral comparison is expressed by a value which represents the degree of similarity against a list of species matches. The Biotyper software—the most represented in the literature [25] —generates a “score value” ranging from 0 to 3, with log(scores) of ≥2 and ≥1.7 recorded as species-level or genus-level identifications, respectively; the SARAMIS software generates a “confidence value” expressed as percentage of identity with the MSP, with >90 % recommended for species-level identification and >70 % for genus-level identification; the Andromas software reports percentages as identification criteria [24]. In general, a 70 % is ± comparable to a Bruker log(score) of 1.7 [25], although a precise equivalence of the two values needs to be defined. The spectra obtainable from microbial cells with a basic sample preparation—in “intact-cell” (IC) or “whole-cell” MS—are protein fingerprints showing high similarity within a species and high reproducibility for individual bacterial and fungal strains, which seem to be only minimally influenced by growth conditions [26].
However, MALDI-TOF MS—already considered as a revolution of the clinical bacteriology—was acquired slowly by the clinical mycology laboratory, particularly with respect to molds [24], essentially because of the intrinsic difficulty of studying fungi as a whole due to their biological complexity, as well as the different (hyphal or conidial) phenotypes coexisting in the same fungal isolate [27]. Another possible reason for this slow acquisition should be sought in the doubt whether differences and similarities in mass spectral patterns are completely consistent with the established taxonomy, or in the lack of comprehensive databases covering all clinically relevant species [26]. Nonetheless, further development in sample preparation protocols [28] and in fungus-specific databases [29] allowed to fill the gap between laboratory research and routine clinical use with respect to the MALDI-TOF MS-based identification of filamentous fungi. It was noted that highest concordance between acquired (experimental) spectra and those included in each system’s reference library (e.g., MALDI Biotyper) is achievable only if the sample preparatory procedure used for the MALDI-TOF MS system at hand is not dissimilar from that used to construct the system’s reference library [24, 30]. Also, increasing the number of mass spectra originated from distinct subcultures of fungal strains, representing each species in the reference library, yields a remarkable improvement in the MALDI-TOF MS-based mold identification, partly compensating for the relatively low number of specific strains available to construct effective reference spectra libraries [29].
Identification of Aspergilli by MALDI-TOF Mass Spectrometry
In a systematic review of recent studies reporting MALDI-TOF MS performance for identification of clinical isolates of filamentous fungi, a clear-cut separation between studies that use an IC approach—a single colony is smeared directly onto a MALDI target plate and covered by an acidic organic MALDI matrix solution—and studies that use a cell lysis (CL) approach—an ethanol–formic acid procedure for complete protein extraction, consisting of short incubation and centrifugation steps prior to depositing supernatant onto the target—was put into evidence [25]. According to the manufacturers’ recommendations, “fast formic acid”—the smeared colony is lysed onto the target with a 25–70 % formic acid solution—is the ideal procedure with the SARAMIS, Andromas, and Vitek MS systems, as the complete extraction method is with Biotyper [24]. Except than in a few studies, mold isolates were identified by comparing their own spectra with those included in an in-house reference library, and notably identification failures mainly involved fungal species with no entries in the reference databases used therein [25]. Table 1 summarizes the characteristics of studies mainly focusing on the identification of clinically relevant Aspergillus species by MALDI-TOF MS.
In one of these studies that use commercial databases, the Andromas software was able to differentiate Aspergillus species into the sections Fumigati (55 A. fumigatus, 1 Neosartorya pseudofisheri, and 1 A. lentulus), Flavi (3 A. flavus and 1 A. tamarii), and Terrei (2 Aspergillus terreus), with an overall identification rate of 98.4 % (63 of 64 isolates); 9 isolates, at the first run, yielded no “good identification” (4 were “identification to be confirmed”, and 5 were “no identification”), but only one remaining isolate, at the second run, required to be identified by multilocus sequencing [31]. In a similar study, the Vitek MS system was evaluated utilizing a single-deposit strategy without prior protein extraction [32]; a limited number of Aspergillus isolates (44 isolates of which 33 were A. fumigatus, 2 A. flavus, and 1 A. niger) were studied, but none of 8 isolates belonging to species absent from the database (Aspergillus sydowi, A. terreus, Aspergillus tubingensis, A. calidoustus, Aspergillus nidulans, and Aspergillus puniceus) were misidentified—showing the good specificity of the method—whereas no identification occurred primarily because of the restricted number of Aspergillus species (A. fumigatus, A. flavus, A. niger, and A. versicolor) present in the current Vitek MS database.
To validate a standardized procedure for MALDI-TOF MS-based identification of filamentous fungi, Cassagne et al. [28] analyzed prospectively mold isolates obtained from sequential clinical samples, by using a chemical (acid formic and acetonitrile) extraction of the fungal colonies and a database built with the reference spectra from 146 mold strains. Eighty-seven percent (154/177) of isolates, including 86 A. fumigatus, 38 other Aspergilli (9 species), and 53 other molds (23 species), were identified to the species level, whereas the MALDI-TOF MS-based approach failed in 12 % (21/177) of isolates from species not represented in the 146-strain library. The last named isolates included 2 Aspergillus alliaceus, 1 Aspergillus clavatus, 1 Aspergillus melleus, and 1 A. oryzae [28]. Later, Lau et al. [33] using a mechanical lysis method challenged a own self-constructed mold database (named the NIH mold database) for MALDI-TOF MS fungal identification against 421 clinical isolates. A total of 294 reference spectra from individual isolates of 152 clinically relevant fungal species, which comprise 63 Aspergillus species, were included in the database. As compared to the Bruker BioTyper library (version 3.1), a stronger performance was shown by the NIH mold database, with correct species-level identification for 370 (88.9 %) isolates and a further 18 (4.3 %) isolates identified to the genus level. Confirming earlier observations, no isolates were misidentified and importantly, the Bruker’s original cutoff scores of ≥2.0 for species- and ≥1.7 for genus-level identifications could be retained without compromising sensitivity; those 33 (7.8 %) isolates failing identification—their scores were <1.7—were species not represented in the database [33].
Nonetheless, a simple and rapid IC method that involves depositing the superficial material of a fungal colony (a water mixture of spores, conidiophores, and mycelium) directly onto the MALDI target plate can enable the protein biomarker desorption to generate a MALDI-TOF mass spectrum [27]. By means of this method, Alanio et al. [34] used the Andromas software to engineer a database including species-specific spectral fingerprints of young and mature colonies of 28 reference strains, corresponding to 28 Aspergillus species from 7 sections—to cover common and uncommon species currently described as being responsible for human infection. The performance of this database was evaluated on 124 clinical and 16 environmental isolates of Aspergillus, resulting in 98.6 % correct identification. Two isolates, one with absent conidiogenesis and the other with atypical sporulation, could not be identified—127 isolates were identified after a single run, 11 were identified after two runs—but no isolate was misidentified, leading to 100 % specificity [34]. In a similar analysis, using water suspensions of fungal mycelia and/or conidia and the BioTyper 2.0 software, we constructed a reference MALDI-TOF MS database with the spectra of 109 culture collection strains—representing 55 species of Aspergillus (33), Fusarium (12), and Mucorales (10)—and challenged it with 103 blind-coded clinical isolates, 81 from 14 Aspergillus species and 22 from other 15 species [35]. Excluding isolates that were not contained in the database, MALDI-TOF MS identified 91 of 94 isolates (96.8 %) of Aspergillus, Fusarium, and Mucorales, according to their designated species. Interestingly, the log(score) values of 91 isolates with correct results were all higher than 2.0; the remaining 3 isolates (1 Emericella nidulans, 1 A. niger, and 1 Aspergillus versicolor) could be identified only to the genus level, as their log(score) value was of <2.0 (1.817, 1.874, and 1.796, respectively), but had concordant species designations as compared with the multilocus sequencing results. By contrast, isolates belonging to the species not included in our database had all log(score) values of <1.7, confirming the specificity of MALDI-TOF MS identification [35].
Extended Use of MALDI-TOF Mass Spectrometry for Aspergilli
Closely Related Species Differentiation
As mass spectra of different fungal species are distinct from one another, specific mass peaks can be identified in a typical spectral range of 2,000–20,000 m/z leading to discriminate between closely related species and to classify organisms at the subspecies level [26]. As above mentioned, A. flavus and A. oryzae are difficult to separate by means of β-tubulin sequence analysis, thereby requiring a labor-intensive DNA-based technique for their final species designation (discussed in [35]). In our study, MALDI-TOF MS was shown to easily differentiate A. flavus and A. oryzae on the species level, and interestingly, clinical isolates of A. oryzae and A. flavus formed separate clusters with their corresponding reference strains, and both the clusters could be distinguished from those of A. parasiticus and A. alliaceus, respectively [35]. Although A. flavus produces harmful aflatoxins while A. oryzae does not, nonaflatoxigenic isolates of A. flavus are highly related to A. oryzae, and this is consistent with the hypothesis that an atoxigenic lineage of A. flavus has gradually evolved into a domesticated A. oryzae through selection by humans [36]. As several non(afla)toxigenic A. flavus isolates are phenotypically more similar to A. oryzae than to other A. flavus isolates, a molecular-phenotypic approach such as MALDI-TOF MS could be very useful for discriminating toxigenic from atoxigenic strains within the A. flavus species [24].
By analyzing with MALDI-TOF MS intact conidia of isolates from the species A. flavus, A. oryzae, A. parasiticus, and A. sojae, Li et al. previously showed that aflatoxigenic strains and nonaflatoxigenic strains have different mass peak profiles, although nonaflatoxigenic A. flavus and A. parasiticus conidia were very similar to those of the closely related A. oryzae and A. sojae [37]. Consistent with these findings, highly reproducible mass spectral fingerprints were obtained with 12 species of Aspergillus and 5 different strains of A. flavus, leading the authors to classify each species and strain of Aspergillus tested with 100 % accuracy in their MALDI-TOF MS analysis [38]. Indeed, while the mass spectra of 2 strains of A. flavus and A. parasiticus slightly differed from each other, a canonical discriminant analysis was able to resolve the spectra from 8 replicate cultures for each of 5 A. flavus strains tested—4 from geographically distinct areas and 1 reference strain—despite the high degree of similarity between strains [38].
In the aforementioned study by Tam et al. [20], only 6 and 3 of the 9 A. flavus strains analyzed—8 clinical isolates and 1 reference strain—were identified correctly using the SARAMIS (Vitek MS RUO system) and Vitek MS (Vitek MS IVD system) databases with confidence levels of 78.5–99.9 and 73.7–97.5 %, respectively. Notably, none of the strains of A. nomius—2 clinical isolates and 1 reference strain—and A. tamarii—1 clinical isolate and 1 reference strain—was correctly identified by MALDI-TOF MS. However, hierarchical clustering of the MALDI-TOF MS spectra from the 11 clinical isolates—reported as A. flavus by phenotypic methods—and the 3 reference strains showed that the 9 strains of A. flavus, 3 strains of A. nomius, and 2 strains of A. tamarii were separated into three clusters. Therefore, A. flavus, A. nomius, and A. tamarii could confidently be identified to the species level using MALDI-TOF MS, provided that the MALDI-TOF MS database is enhanced to include adequate spectra of different strains from each species [20].
Antifungal Susceptibility Testing
It has become important to perform antifungal susceptibility testing (AFST) in daily routine practice [39], particularly for those fungal species exhibiting resistance to commonly prescribed antifungal drugs [40, 41]. Despite the recent advances in reference methods and the availability of commercial tests, novel AFST assays based on short-time drug exposure of patients’ isolates may represent upcoming tools to closely survey antifungal resistance in many clinical settings [42], and MALDI-TOF MS offers in this sense an exciting possibility, although in its infancy [43].
By relying on previous findings showing that proteomic profile changes are induced by exposure of fungal cells to fluconazole [44], we developed a MALDI-TOF MS-based assay for testing susceptibility of fungal species to the echinocandin caspofungin [45]. The echinocandins exert their antifungal effects by noncompetitively inhibiting β-1,3-glucan synthase, an enzyme required for cell wall components of medically important fungi, including Candida and Aspergillus. In Candida albicans exposure to caspofungin was shown to alter the abundance of several proteins, including enzymes involved in cell wall biosynthesis and integrity, as well as the regulator of β-1,3-glucan synthase, Rho1p [46]. In our assay, after a 15-h incubation of fungal cells with serial antifungal drug concentrations, the fungal pellets were suspended in 10 % formic acid and analyzed on MALDI-TOF MS, using a composite correlation index (CCI)-based approach. This allowed to determine the minimal profile change concentration (MPCC), an endpoint alternative to the classical MIC [44], that was defined as the CCI value at which a fungal spectrum is more similar to the spectrum observed at maximal (32 µg/ml) caspofungin concentration than the fungal spectrum observed at null (0 µg/ml) caspofungin concentration [45]. Using a set of wild-type and fks mutant isolates—mutations in fks genes confer reduced susceptibility/resistance to echinocandin antifungals—of Candida (34 isolates) and Aspergillus (10 isolates) species, we then showed that the MPCC was in full essential agreement with the MIC or the minimum effective concentration (MEC) for 100 % of the isolates tested. In particular, MPCCs of 0.5 and 0.25 μg/ml were able to capture, respectively, all of 6 A. fumigatus and 4 A. flavus isolates tested, according to the MEC values. Although the endpoint readings achieved with the version of assay presented there—we later proposed a more rapid simplification of the assay [47]—provide only a slight time saving compared to the AFST reference methods (15 h versus 24 h) at least for Candida species, our MALDI-TOF MS-based AFST method has the great advantage of eliminating subjective readouts, especially when Aspergillus species and other filamentous fungi are tested for echinocandin (caspofungin) susceptibility. In this case, it would allow to avoid the microscopic assessment of the MEC, which remains technically difficult to determine [48].
Limits and Potentials of MALDI-TOF Mass Spectrometry for Aspergilli
In the face of accuracy, rapidity, and superiority over conventional phenotypic methods, MALDI-TOF MS has limitations (discussed in [23]). Whereas the instrument cost remains comparable to that of other common laboratory equipment, however, the low operating costs—minimal consumables and hands-on time are required for sample processing and analysis—are counterbalanced by the frequent instrumental maintenance and the short lifetime of the laser necessitating an appropriate service plan. Another drawback concerns the mold databases that may be updated by user addition of mass spectral entries to expand their identification capability or constructed ad hoc in specialized mycology laboratories, but these databases are not publicly available unlike sequence databases such as GenBank. In addition, there is the disadvantage that antimicrobial susceptibility is not directly determined with the current MALDI-TOF MS-based diagnostic strategy.
Apart from, and partly related to, these limits, the future work will have to face other very promising issues in medical mycology, such as the AFST or the epidemiological typing of fungal isolates. Although encouraging results are obtained in proof-of-concept studies [44, 45, 47], it is necessary to better define reproducibility and standardization of the MALDI-TOF MS-based AFST assays, as well as to extend the applicability to all antifungal drugs in order to facilitate the adoption of these assays by clinical microbiology laboratories in the next future. These studies will also have to regard the correlation of MALDI-TOF MS results with the clinically derived breakpoints for Aspergilli, which are currently used to interpret the MIC values for identifying potentially resistant isolates [49]. As local surveillance MIC data, derived from a routine microbiology laboratory workflow, can aid to develop treatment strategies, studies will have to prove, ultimately, the impact of the MALDI-TOF MS results on the appropriate antifungal treatment and the clinical course of aspergillosis.
Concerning the potential for MALDI-TOF MS to provide epidemiological data, aforementioned studies have shown the ability of MALDI-TOF MS to discriminate highly related microbial organisms, including fungi. Unfortunately, to the authors’ knowledge, use of MALDI-TOF MS has never been reported to establish the extent of an outbreak and to elucidate the sources and the spread of fungal infections, as well as sporadic are MALDI-TOF MS data about the strain typing or genetic relatedness of fungal isolates [50–53]. By contrast, several strain typing methods, based on molecular techniques, can be used for fungal epidemiological investigations, but these analyses are not routinely performed in many clinical laboratories, resulting in delayed times to detection of hospital-associated infections and outbreaks [22]. Thus, having this type of data readily available, through the use of MALDI-TOF MS, could be advantageous, particularly in the context of A. fumigatus infections. This considering that ever more patients are at risk of azole-resistant aspergillosis, due to the presence of resistant strains in the environment [41], the emergence and geographical migration of highly resistant strains [54] and the evolving of new mechanisms for azole resistance in this species [41]. If performing rapid susceptibility testing of Aspergillus isolates before and during antifungal treatment can be clinically relevant [39, 42], both patients’ specimens and hospital’s environmental samples could be analyzed in “real time” for the presence of azole-resistant A. fumigatus isolates, as more experience is gained in MALDI-TOF MS fungal databases to be used for the species- and strain-specific identification.
Conclusion
Despite ever-increasing utility of MALDI-TOF MS for fungal species identification, there is still controversy as to whether the extraction protein or the direct colony deposition has to be used for the sample preparation prior to MALDI-TOF MS analysis. Although the methods employed by investigators at each single center proved to work well in their own evaluations, multicenter studies are needed to standardize the MALDI-TOF MS-based mold identification in the clinical microbiology/mycology laboratory. At the time, to our and other clinical laboratory scientists’ opinion, it is important to interrogate the database libraries composed of spectra that have been obtained under the same experimental conditions [24, 30]. Also, while continuous enrichment of the existing (in-house or commercial) databases with rare, new, or emerging strains/species is imperative [22, 55], the practice of database expansion/improvement should be the prerogative of centralized reference laboratories, particularly in those environments not subjects to regulatory body restrictions [56]. With regards to less explored applications of MALDI-TOF MS, further studies are warranted prior to using this technology for epidemiological investigations or rapid detection of antifungal resistance in pathogenic fungi. Thus, we expect that these areas will be potentiated in the near future, in order to enhance and diversify the clinical diagnostic usefulness of MALDI-TOF MS. As delayed and incorrect diagnoses potentially lead to high mortality and morbidity for invasive fungal infection, implementing a rapid, accurate, and cost-effective MALDI-TOF MS-based mold analysis could result in drastically shortened diagnosis times and in significant benefits for the patients’ care.
References
Miceli MH, Lee SA. Emerging moulds: epidemiological trends and antifungal resistance. Mycoses. 2011;54:e666–78.
Posteraro B, Torelli R, De Carolis E, Posteraro P, Sanguinetti M. Update on the laboratory diagnosis of invasive fungal infections. Mediterr J Hematol Infect Dis. 2011;3:e2011002.
Balajee SA, Nickle D, Varga J, Marr KA. Molecular studies reveal frequent misidentification of Aspergillus fumigatus by morphotyping. Eukaryot Cell. 2006;5:1705–12.
Borman AM, Johnson EM. Genomics and proteomics as compared to conventional phenotypic approaches for the identification of the agents of invasive fungal infections. Curr Fungal Infect Rep. 2013;7:235–43.
Lau A, Chen S, Sleiman S, Sorrell T. Current status and future perspectives on molecular and serological methods in diagnostic mycology. Future Microbiol. 2009;4:1185–222.
Kliem M, Sauer S. The essence on mass spectrometry based microbial diagnostics. Curr Opin Microbiol. 2012;15:397–402.
Geiser DM, Klich MA, Frisvad JC, Peterson SW, Varga J, Samson RA. The current status of species recognition and identification in Aspergillus. Stud Mycol. 2007;59:1–10.
Balajee SA, Houbraken J, Verweij PE, Hong SB, Yaghuchi T, Varga J, Samson RA. Aspergillus species identification in the clinical setting. Stud Mycol. 2007;59:39–46.
Balajee SA, Borman AM, Brandt ME, Cano J, Cuenca-Estrella M, Dannaoui E, Guarro J, Haase G, Kibbler CC, Meyer W, O’Donnell K, Petti CA, Rodriguez-Tudela JL, Sutton D, Velegraki A, Wickes BL. Sequence-based identification of Aspergillus, Fusarium, and Mucorales species in the clinical mycology laboratory: where are we and where should we go from here? J Clin Microbiol. 2009;47:877–84.
Samson RA, Varga J. What is a species in Aspergillus? Med Mycol. 2009;47(Suppl 1):S13–20.
Johnson EM, Borman AM. Identification of Aspergillus at the species level: the importance of conventional methods; microscopy and culture. In: Pasqualotto Alessandro, editor. Aspergillus and Aspergillosis. New York: Springer; 2009. p. 55–74.
Hawksworth DL. Pandora’s mycological box: molecular sequences vs. morphology in understanding fungal relationships and biodiversity. Rev Iberoam Micol. 2006;23:127–33.
van der Linden JW, Warris A, Verweij PE. Aspergillus species intrinsically resistant to antifungal agents. Med Mycol. 2011;49(Suppl 1):S82–9.
Balajee SA, Kano R, Baddley JW, Moser SA, Marr KA, Alexander BD, Andes D, Kontoyiannis DP, Perrone G, Peterson S, Brandt ME, Pappas PG, Chiller T. Molecular identification of Aspergillus species collected for the Transplant-Associated Infection Surveillance Network. J Clin Microbiol. 2009;47:3138–41.
Ostrosky-Zeichner L. Invasive mycoses: diagnostic challenges. Am J Med. 2012;125(Suppl 1):S14–24.
Klich MA. Identification of clinically relevant aspergilli. Med Mycol. 2006;44(Suppl 1):S127–31.
Krishnan S, Manavathu EK, Chandrasekar PH. Aspergillus flavus: an emerging non-fumigatus Aspergillus species of significance. Mycoses. 2009;52:206–22.
Chang PK, Ehrlich KC. What does genetic diversity of Aspergillus flavus tell us about Aspergillus oryzae? Int J Food Microbiol. 2010;138:189–99.
Varga J, Frisvad JC, Samson RA. Two new aflatoxin producing species, and an overview of Aspergillus section Flavi. Stud Mycol. 2011;69:57–80.
Tam EW, Chen JH, Lau EC, Ngan AH, Fung KS, Lee KC, Lam CW, Yuen KY, Lau SK, Woo PC. Misidentification of Aspergillus nomius and Aspergillus tamarii as Aspergillus flavus: characterization by internal transcribed spacer, β-tubulin, and calmodulin gene sequencing, metabolic fingerprinting, and matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2014;52:1153–60.
Seng P, Drancourt M, Gouriet F, La Scola B, Fournier PE, Rolain JM, Raoult D. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Infect Dis. 2009;49:543–51.
Clark AE, Kaleta EJ, Arora A, Wolk DM. Matrix-assisted laser desorption ionization-time of flight mass spectrometry: a fundamental shift in the routine practice of clinical microbiology. Clin Microbiol Rev. 2013;26:547–603.
Patel R. Matrix-assisted laser desorption ionization-time of flight mass spectrometry in clinical microbiology. Clin Infect Dis. 2013;57:564–72.
Posteraro B, De Carolis E, Vella A, Sanguinetti M. MALDI-TOF mass spectrometry in the clinical mycology laboratory: identification of fungi and beyond. Expert Rev Proteomics. 2013;10:151–64.
Vermeulen E, Verhaegen J, Indevuyst C, Lagrou K. Update on the evolving role of MALDI-TOF MS for laboratory diagnosis of fungal infections. Curr Fungal Infect Rep. 2012;6:206–14.
Welker M. Proteomics for routine identification of microorganisms. Proteomics. 2011;11:3143–53.
Santos C, Paterson RR, Venâncio A, Lima N. Filamentous fungal characterizations by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. J Appl Microbiol. 2010;108:375–85.
Cassagne C, Ranque S, Normand AC, Fourquet P, Thiebault S, Planard C, Hendrickx M, Piarroux R. Mould routine identification in the clinical laboratory by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. PLoS ONE. 2011;6:e28425.
Normand AC, Cassagne C, Ranque S, L’ollivier C, Fourquet P, Roesems S, Hendrickx M, Piarroux R. Assessment of various parameters to improve MALDI-TOF MS reference spectra libraries constructed for the routine identification of filamentous fungi. BMC Microbiol. 2013;13:76.
Bader O. MALDI-TOF-MS-based species identification and typing approaches in medical mycology. Proteomics. 2013;13:788–99.
Bille E, Dauphin B, Leto J, Bougnoux ME, Beretti JL, Lotz A, Suarez S, Meyer J, Join-Lambert O, Descamps P, Grall N, Mory F, Dubreuil L, Berche P, Nassif X, Ferroni A. MALDI-TOF MS Andromas strategy for the routine identification of bacteria, mycobacteria, yeasts, Aspergillus spp. and positive blood cultures. Clin Microbiol Infect. 2012;18:1117–25.
Iriart X, Lavergne RA, Fillaux J, Valentin A, Magnaval JF, Berry A, Cassaing S. Routine identification of medical fungi by the new Vitek MS matrix-assisted laser desorption ionization-time of flight system with a new time-effective strategy. J Clin Microbiol. 2012;50:2107–10.
Lau AF, Drake SK, Calhoun LB, Henderson CM, Zelazny AM. Development of a clinically comprehensive database and a simple procedure for identification of molds from solid media by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2013;51:828–34.
Alanio A, Beretti JL, Dauphin B, Mellado E, Quesne G, Lacroix C, Amara A, Berche P, Nassif X, Bougnoux ME. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry for fast and accurate identification of clinically relevant Aspergillus species. Clin Microbiol Infect. 2011;17:750–5.
De Carolis E, Posteraro B, Lass-Flörl C, Vella A, Florio AR, Torelli R, Girmenia C, Colozza C, Tortorano AM, Sanguinetti M, Fadda G. Species identification of Aspergillus, Fusarium and Mucorales with direct surface analysis by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Microbiol Infect. 2012;18:475–84.
Gibbons JG, Salichos L, Slot JC, Rinker DC, McGary KL, King JG, Klich MA, Tabb DL, McDonald WH, Rokas A. The evolutionary imprint of domestication on genome variation and function of the filamentous fungus Aspergillus oryzae. Curr Biol. 2012;22:1403–9.
Li TY, Liu BH, Chen YC. Characterization of Aspergillus spores by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Rapid Commun Mass Spectrom. 2000;14:2393–400.
Hettick JM, Green BJ, Buskirk AD, Kashon ML, Slaven JE, Janotka E, Blachere FM, Schmechel D, Beezhold DH. Discrimination of Aspergillus isolates at the species and strain level by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry fingerprinting. Anal Biochem. 2008;380:276–81.
Eschenauer GA, Carver PL. The evolving role of antifungal susceptibility testing. Pharmacotherapy. 2013;33:465–75.
Pfaller MA. Antifungal drug resistance: mechanisms, epidemiology, and consequences for treatment. Am J Med. 2012;125(Suppl 1):S3–13.
Vermeulen E, Lagrou K, Verweij PE. Azole resistance in Aspergillus fumigatus: a growing public health concern. Curr Opin Infect Dis. 2013;26:493–500.
Posteraro B, Torelli R, De Carolis E, Posteraro P, Sanguinetti M. Antifungal susceptibility testing: current role from the clinical laboratory perspective. Mediterr J Hematol Infect Dis. 2014;6:e2014030.
Kostrzewa M, Sparbier K, Maier T, Schubert S. MALDI-TOF MS: an upcoming tool for rapid detection of antibiotic resistance in microorganisms. Proteomics Clin Appl. 2013;7:767–78.
Marinach C, Alanio A, Palous M, Kwasek S, Fekkar A, Brossas JY, Brun S, Snounou G, Hennequin C, Sanglard D, Datry A, Golmard JL, Mazier D. MALDI-TOF MS-based drug susceptibility testing of pathogens: the example of Candida albicans and fluconazole. Proteomics. 2009;9:4627–31.
De Carolis E, Vella A, Florio AR, Posteraro P, Perlin DS, Sanguinetti M, Posteraro B. Use of matrix-assisted laser desorption ionization-time of flight mass spectrometry for caspofungin susceptibility testing of Candida and Aspergillus species. J Clin Microbiol. 2012;50:2479–83.
Hoehamer CF, Cummings ED, Hilliard GM, Rogers PD. Changes in the proteome of Candida albicans in response to azole, polyene, and echinocandin antifungal agents. Antimicrob Agents Chemother. 2010;54:1655–64.
Vella A, De Carolis E, Vaccaro L, Posteraro P, Perlin DS, Kostrzewa M, Posteraro B, Sanguinetti M. Rapid antifungal susceptibility testing by matrix-assisted laser desorption ionization-time of flight mass spectrometry analysis. J Clin Microbiol. 2013;51:2964–9.
Lass-Flörl C. In vitro susceptibility testing in Aspergillus species: an update. Future Microbiol. 2010;5:789–99.
Verweij PE, Howard SJ, Melchers WJ, Denning DW. Azole-resistance in Aspergillus: proposed nomenclature and breakpoints. Drug Resist Updat. 2009;12:141–7.
Carolis ED, Hensgens LA, Vella A, Posteraro B, Sanguinetti M, Senesi S, Tavanti A. Identification and typing of the Candida parapsilosis complex: MALDI-TOF MS vs. AFLP Med Mycol. 2014;52:123–30.
Pulcrano G, Roscetto E, Iula VD, Panellis D, Rossano F, Catania MR. MALDI-TOF mass spectrometry and microsatellite markers to evaluate Candida parapsilosis transmission in neonatal intensive care units. Eur J Clin Microbiol Infect Dis. 2012;31:2919–28.
Firacative C, Trilles L, Meyer W. MALDI-TOF MS enables the rapid identification of the major molecular types within the Cryptococcus neoformans/C. gattii species complex. PLoS ONE. 2012;7:e37566.
Posteraro B, Vella A, Cogliati M, De Carolis E, Florio AR, Posteraro P, Sanguinetti M, Tortorano AM. Matrix-assisted laser desorption ionization-time of flight mass spectrometry-based method for discrimination between molecular types of Cryptococcus neoformans and Cryptococcus gattii. J Clin Microbiol. 2012;50:2472–6.
van der Linden JW, Camps SM, Kampinga GA, Arends JP, Debets-Ossenkopp YJ, Haas PJ, Rijnders BJ, Kuijper EJ, van Tiel FH, Varga J, Karawajczyk A, Zoll J, Melchers WJ, Verweij PE. Aspergillosis due to voriconazole highly resistant Aspergillus fumigatus and recovery of genetically related resistant isolates from domiciles. Clin Infect Dis. 2013;57:513–20.
Mancini N, Burioni R, Sanguinetti M, Clementi M. Risks of “blind” automated identification systems in medical microbiology. J Clin Microbiol. 2013;51:3911.
Westblade LF, Jennemann R, Branda JA, Bythrow M, Ferraro MJ, Garner OB, Ginocchio CC, Lewinski MA, Manji R, Mochon AB, Procop GW, Richter SS, Rychert JA, Sercia L, Burnham CA. Reply to “risks of ‘blind’ automated identification systems in medical microbiology”. J Clin Microbiol. 2013;51:3912.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanguinetti, M., Posteraro, B. MALDI-TOF Mass Spectrometry: Any Use for Aspergilli?. Mycopathologia 178, 417–426 (2014). https://doi.org/10.1007/s11046-014-9757-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-014-9757-1