Abstract
We conducted this cross-sectional retrospective study using clinical and laboratory data from two tertiary hospitals in Cuiabá, Mato Grosso, Brazil, in order to explore the risk factors and estimate mortality, prevalence and lethality of candidemia between 2006 and 2011. A total of 130 episodes of candidemia were identified. The prevalence of candidemia was 1.8 per 1,000 admissions, the mortality rate was 0.9 per 1,000 admissions, and the lethality was 49.2 %. The main agent in this population was Candida parapsilosis (n = 50), followed by C. albicans (n = 45). Comparison between the numbers of episodes in the two triennia revealed that the non-albicans group grew by 48.2 %. The distribution of yeast species of Candida per hospital unit revealed that C. albicans was more prevalent than C. parapsilosis in the adult ICU and C. parapsilosis was more prevalent than C. albicans in the neonatal ICU. Patients remained hospitalized for an average of 53.5 days. Central venous catheters, parenteral nutrition and age were the variables that proved to be independent in the multivariate analysis and that maintained a statistically significant association with the incidence of death in patients with candidemia. The annual prevalence of candidemia showed a significant increase in the second triennium (2009–2011) compared with the first (2006–2008) probably due to increased exposure to risk factors: central venous catheter, H2 blockers, nutrition parenteral corticosteroids and mean hospital duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bloodstream infections (BSI) caused by Candida species are often difficult to diagnose and are responsible for high attributable mortality and high hospital costs [1–9].
The species Candida albicans is considered the main etiologic agent of candidemia; however, other species of the genus (e.g., C. parapsilosis, C. tropicalis, C. glabrata, C. krusei) have been classified as emerging pathogens in this type of infection [10–15].
Candidemia is among the top four most common causes of BSI in critically ill patients and their epidemiology has been well studied in the United States and Europe, but not in Latin America. In Brazil, the incidence rates are fragmented when considering data from all regions of the country [1, 16–20].
Colombo et al. [1] conducted one of the most important works in Brazil concerning the incidence of candidemia, in 11 tertiary and university hospitals in nine cities; however, this study did not include the university hospitals of Cuiabá, in the State of Mato Grosso. Thus, this work represents the first study of the Midwest region of Brazil that addresses the epidemiology and prevalence of candidemia, species distribution and associated risk factors over a period of 6 years.
Methods
Data Collection
Our group investigated episodes of candidemia in two university hospitals in the mid-size city of Cuiabá, Mato Grosso, Brazil. One of the hospitals included in this study is a reference center for infectious diseases and the other is a reference center for maternity; together, they have 271 beds. The clinical and laboratorial data were stored in the database of the EpiData statistical program. The patients selected did not suffer any risk exposure due to the epidemiological design of the study and their identities were preserved.
Study Design and Inclusion Criteria
This is an observational, retrospective, laboratory-based, cross-sectional study. The sample consisted of laboratory confirmed cases of candidemia that occurred in two tertiary hospitals from January 2006 to December 2011.
One episode of candidemia was defined by the isolation of Candida species from one or more blood cultures in a patient with clinical signs of infection if more than one blood culture was positive, and a new episode was defined if more than 30 days had elapsed since the first positive blood culture.
Neutropenia was defined as an absolute neutrophil count of <500 cells/mm3. Fever was defined as a temperature of 38 °C or greater. Patients were considered adults when aged 14 years old or over.
Microbiological Methods
The presence of microorganisms was detected in blood culture bottles using the BacT/ALERT-3D® automated system (bioMérieux). For species identification, we used the VITEK®2 automated system (bioMérieux) based on preestablished biochemical methods measuring 46 tests, including carbon source use, nitrogen use and enzymatic activities.
We used the following classic methods: germ tube, micromorphological characteristics [21] in microculture on Corn-meal agar (DIFCO, USA) and Tween-80, growth on CHROMagar Candida® (DIFCO, USA) and zymogram/auxanogram.
Patient Characteristics
The following variables were considered: patients admitted, patients with candidemia, age, sex, use of central venous catheters, parenteral nutrition, corticosteroids, H2 blockers, prematurity, antifungal treatment, low birth weight, mechanical ventilation, neutropenia, fever, previous surgery and hospitalization period.
Statistical Analysis
Infection prevalence was calculated by the number of BSI caused by Candida yeasts per 1,000 admissions. Statistical analysis was performed using STATA (version 5.0). Categorical variables were analyzed using the chi-square test, for which a p value <0.05 was the criterion for significance. To determine the independent effect of each variable on the exploratory response variable, we used forward stepwise multiple logistic regressions. The variables selected for this model were those that had p values of less than 0.20 in the univariate analysis or that were biologically plausible.
Results
We identified 130 episodes of candidemia in 124 patients (six patients had two episodes) in a total of 72.767 patients admitted. The prevalence of BSI caused by Candida species was 1.8 per 1,000 admissions (Fig. 1). Comparison between the numbers of episodes in the two triennia revealed that the non-albicans group grew by 48.2 %. The mortality rate in patients with candidemia was 0.9 per 1,000 admissions and lethality was 49.2 % (Table 1).
Regarding sex, 58.5 % (n = 76) of patients were female. Patient mean age was 31.4 years old (median 38.4; SD 27.6; 95 % CI 23.1–39.7); 61.5 % (n = 80) were adults, 13.1 % (n = 17) were pediatric patients, and 25.4 % (n = 33) were neonates. The highest number of patients was concentrated in the age group ranging from 35 to 74 years old (48.5 %, n = 63).
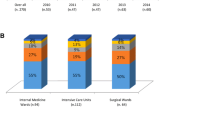
Considering admission distribution, 69.2 % (n = 90) of patients were hospitalized in intensive care units (ICUs); these were distributed equally between the neonatal and adult ICUs. Other admission units included surgery (16.2 %, n = 21), internal medicine (10.8 %, n = 14) and pediatrics (3.8 %, n = 5). Patients remained hospitalized for an average of 53.5 days (median 42.5, SD 45.5, 95 % CI 45.6–61.4). Considering the admission period, a higher concentration of patients remained hospitalized for between 21 and 60 days (54.4 %, n = 71).
The antifungal agents most widely used in therapeutic management were fluconazole (50.4 %, n = 65), amphotericin B (47.3 %, n = 61), caspofungin (1.6 %, n = 2) and ketoconazole (0.8 %, n = 1). No association between exposure to antifungals and the outcome of the clinical case was observed.
The risk exposures that showed statistical significance with the outcome of death in the univariate analysis were as follows: mechanical ventilation (p < 0.001), central venous catheter (p < 0.05), steroids (p = 0.05), ICU admission (p < 0.05) and parenteral nutrition (p < 0.001). However, in the multivariate analysis, central venous catheters, parenteral nutrition and age were the variables that proved to be independent and that maintained a statistically significant association with the incidence of death in patients with candidemia. Patient characteristics in relation to the species of Candida yeasts are presented in Table 2.
The characteristics of the population in the univariate analysis that were statistically significant in relation to the presence of yeasts of the isolated Candida species were as follows: C. parapsilosis (p < 0.05) and C. albicans with female patients (p = 0.05); and parenteral nutrition and C. tropicalis (p < 0.05). However, in the multivariate analysis, sex (p < 0.05; OR 0.3; 95 % CI 0.17–0.86) and neutropenia (p = 0.05; OR 2.4; 95 % CI 0.98–5.96) and independent variables were statistically significant for the presence of C. albicans as a causative agent of blood stream infections by Candida species. Likewise, an independent association was observed between sex and C. parapsilosis (p < 0.01; OR 3.0; 95 % CI 1.45–6.33); and parenteral nutrition and C. tropicalis (p < 0.05; OR 0.3; 95 % CI 0.13–0.81).
The distribution of yeast species of Candida per hospital unit revealed that C. albicans was more prevalent than C. parapsilosis in the adult ICU and C. parapsilosis was more prevalent than C. albicans in the neonatal ICU. Generalizing these values for all ICUs, C. parapsilosis was predominant compared with C. albicans (n = 38 and n = 32, respectively).
Discussion
This study was composed of a greater number of adult patients; however, even though no statistical association was demonstrated between patients aged 60 years old or over and death; proportionally, the coefficient of mortality due to candidemia among the elderly was higher than among neonates, pediatric and adult patients (including the elderly).
It is likely that this group of patients was more susceptible to infection due to compromised immunity, unlike newborns, who normally present progressive maturity of the immune system over time after receiving intensive care. Analysis of the data revealed that candidemia prevalence in neonates was higher than in the elderly, but the mortality rate was higher in the elderly than in neonates in the sample evaluated in this study.
In both hospitals evaluated in the Midwest region of Brazil, the incidence of mortality due to candidemia was lower to that described by Blumberg et al. [3] in six US hospitals, in which the mortality rate was 41 % (n = 4276; 1993–1995); by Gudlaugsson et al. [22] in a university hospital in Iowa, USA, 61 % (n = 108, 1997–2001); and by Colombo et al. [12] in four university hospitals in São Paulo, Brazil, 61 % (n = 282, 2002–2003). This information reinforces the importance of candidemia as an aggravating factor for the occurrence of death.
Although fluconazole was the most widely used antifungal drug in the treatment of candidemia, the incidence of death diminished, with a consequent increase in hospital discharge. In the hospitals evaluated, antifungal susceptibility testing was only used in cases of treatment failure.
The prevalence of candidemia in this study was lower than the incidences reported in the several countries: USA 9.8 per 1,000 admissions [3], Brazil 2.5 per 1,000 admissions [1], France 0.4 per 1,000 admissions [23] and Spain 1.5 per 1,000 admissions [24]. Several studies have shown higher incidences in male patients with candidemia [1, 3, 7, 22, 25, 26].
The mean age of patients verified in this study was lower compared with the literature [13, 16, 27, 28]. This is probably due to the fact that approximately 25 % of the population evaluated in hospitals in Midwest Brazil was neonates aged up to 30 days old who were submitted to blood collection for cultures.
A study conducted in 23 US hospitals by Horn et al. [16], between 2004 and 2008, involving 2019 patients with candidemia, determined a statistically significant association between the following variables and the Candida yeasts isolated: age (p < 0.001), male sex (p = 0.002), prior antifungal therapy (p < 0.01), neonatal ICU admission (p < 0.01), previous surgery (excluding transplantation) (p < 0.05), mechanical ventilation (p < 0.05), parenteral nutrition (p < 0.05), neutropenia (<500 cells/mm3) (p < 0.01) and steroid use (p < 0.01).
In this study, we verified a statistically significant association between sex, neutropenia and parenteral nutrition and the isolation of Candida species. This fact is noteworthy because although the American sample consisted of 2019 patients [16], approximately 15-fold greater than that reported for this study (n = 130), our data corroborated some of the variables cited, supported by the statistical associations determined in this study.
Bassetti et al. [29] evaluated 348 episodes of candidemia in Italy, correlating the species of Candida yeasts with the pathology and the hospital admission unit. The species C. albicans was the most frequently isolated in the ICU, internal medicine and hematology–oncology. In the Midwest hospitals evaluated in Brazil, we observed that C. albicans was responsible for 17 episodes in the adult ICU and 15 in the neonatal ICU, while C. parapsilosis caused 16 episodes in the adult ICU and 22 in the neonatal ICU. Considering the overall number of episodes in both ICUs in this study, C. parapsilosis (n = 38) was the most frequently isolated in the hospitals evaluated in the Midwest region, in disagreement with the data reported by Bassetti et al. [29].
An interesting work was published by Nucci and Colombo [30], who reported that the early removal of the central venous catheter in patients with candidemia does not contribute to the eradication of the fungal agent, persistence or recurrence rate of infection in the bloodstream. These authors conducted a cohort study involving 842 patients with candidemia who were followed prospectively, and early removal of the central venous catheter was not associated with any clinical benefit.
Finally, it is worth remembering that the presence of central venous catheters in patients with candidemia was considered an independent factor by multivariate analysis (p = 0.01) and increased the odds of death almost sixfold (OR 5.7) in hospitals evaluated in the Midwest region of Brazil.
In summary, we believe it is worth comparing the second triennium (2009–2011) with the first (2006–2008), since this reveals that the increasing incidence of candidemia was related to increased exposure to risk factors (central venous catheter, H2 blockers, nutrition parenteral corticosteroids and mean hospital duration).
Hinrichsen et al. [31], Ghahri et al. [32] and Medrano et al. [33] reported C. parapsilosis as the most frequent etiologic agent in candidemia. However, Nucci et al. [34] reported C. tropicalis as the most frequent etiologic agent in fungemia in cancer patients. Ha et al. [35] estimate that the cost of treating candidemia is approximately USD 4,743 per patient.
A preliminary study published by Colombo et al. [1] revealed results from the Brazilian candidemia network (n = 712 cases, with an incidence of 2.49 cases per 1,000 admissions) and reported that the species C. albicans was the most frequently isolated in a study that involved nine major Brazilian cities and 11 medical centers.
After 1 year, another study [30] was published describing the clinical, epidemiological and microbiological characteristics of 188 episodes of candidemia by C. tropicalis that occurred among 924 cases in 12 tertiary hospitals located in 10 cities from the South, Southeast and Midwest regions; however, the state of Mato Grosso was not included in this work. The patients who had candidemia by C. tropicalis were essentially those who presented neutropenia.
The reason for describing the Brazilian data here, particularly those conducted in a larger number of hospitals and involving the State of Sao Paulo and other Brazilian cities, is to show the regional epidemiological differences [36] in the prevalence of the species most often associated with the peculiarities of each hospital unit, type of inpatient (underlying diseases and comorbidities); thus, emphasizing that in this study, the most frequently identified species was Candida parapsilosis, rather than C. albicans or C. tropicalis. For this reason, it is essential to have a working understanding of the local and regional epidemiology, together with analysis and conclusions regarding the patient’s clinical response.
Important differences are observed between the rates of candidemia determined in different countries and tertiary hospitals, especially in Brazil. These are based on the representativeness of the mean age of patients, which reflect different populations, variations concerning precautions and practices used in intensive care units and other units of admission, the laboratorial methodology for detecting fungal isolates in the bloodstream, and the use of antibiotics.
References
Colombo AL, Nucci M, Park BJ, et al. Epidemiology of candidemia in Brazil: a nationwide sentinel surveillance of candidemia in eleven medical centers. J Clin Microbiol. 2006;44:2816–23.
Ruhnke M, Rickerts V, Cornely OA, et al. Diagnosis and therapy of Candida infections: joint recommendations of the German Speaking Mycological Society and the Paul-Ehrlich-Society for Chemotherapy. Mycoses. 2011;54:279–310.
Blumberg HM, Jarvis WR, Soucie JM, et al. Risk factors for Candida bloodstream infections in surgical intensive care unit patients: the NEMIS prospective multicenter study. Clin Infect Dis. 2001;33:177–86.
Chen LY, Liao SY, Kuo SC, et al. Changes in the incidence of candidaemia during 2000–2008 in a tertiary medical centre in northern Taiwan. J Hosp Infect. 2011;78:50–3.
Garnacho-Montero J, Díaz-Martín A, García-Cabrera G, et al. Risk factors for fluconazol-resistant candidemia. Antimicrob Agents Chemother. 2010;54:3149–54.
Yamamoto AC, Paula CR, Dias LB, et al. Epidemiological and clinical characteristics of nosocomial candidiasis in university hospitals in Cuiabá-Mato Grosso, Brazil. Rev Iberoam. Micol. 2012;29:164–8.
Cisterna R, Ezpeleta G, Telleria O, et al. Nationwide sentinel surveillance of bloodstream Candida infections in 40 tertiary care hospitals in Spain. J Clin Microbiol. 2010;48:4200–6.
Benjamin DK, Stoll BJ, Gantz MG, et al. Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics. 2010;126:e865–73.
Ortega M, Marco F, Soriano A, et al. Candida species bloodstream infection: epidemiology and outcome in a single institution from 1991 to 2008. J Hosp Infect. 2011;77:157–61.
Chang MR, Correia FP, Costa LC, et al. Candida bloodstream infection: data from a teaching hospital in MatoGrosso do Sul, Brazil. Rev Inst Med Trop Sao Paulo. 2008;50:265–8.
Das I, Nightingale P, Patel M, Jumaa P. Epidemiology, clinical characteristics, and outcome of candidemia: experience in a tertiary referral center in the UK. Int J Infect Dis. 2011;15:e759–63.
Colombo AL, Guimarães T, Silva LRBF, et al. Prospective observational study of candidemia in São Paulo, Brazil: Incidence rate, epidemiology, and predictors of mortality. Infect Control Hosp Epidemiol. 2007;28:570–6.
Camargo TZS, Marra AR, Silva CV, et al. Secular trends of candidemia in a tertiary care hospital. Am J Infect Control. 2010;38:546–50.
Chaiwarith R, Ounbang P, Khamwan C, et al. Epidemiology of adult candidemia at Chiang Mai University Hospital. Southeast Asian J Trop Med Public Health. 2011;42:1505–14.
Ylipalosaari P, Ala-Kokko TI, Karhu J, et al. Comparison of the epidemiology, risk factors, outcome and degree of organ failures of patients with candidemia acquired before or during ICU treatment. Crit Care. 2012;16:1–9.
Horn DL, Neofytos D, Anaissie EJ, et al. Epidemiology and outcomes of candidemia in 2019 patients: data from the prospective antifungal therapy alliance registry. Clin Infect Dis. 2009;48:1695–703.
Bruder-Nascimento A, Camargo CH, Sugizaki MF, et al. Species distribution and susceptibility profile of Candida species in a Brazilian public tertiary hospital. BMC Res Notes. 2010;3:1–5.
Nucci M, Queiroz-Telles F, Tobón AM, Restrepo A, Colombo AL. Epidemiology of opportunistic fungal infections in Latin America. Clin Infect Dis. 2010;51:561–70.
Zaoutis TE, Prasad PA, Localio AR, et al. Risk factors and predictors for candidemia in pediatric intensive care unit patients: implications for prevention. Clin Infect Dis. 2010;51:e38–45.
Tumbarello M, Fiori B, Trecarichi EM, et al. Risk factors and outcomes of candidemia caused by biofilm-forming isolates in a tertiary care hospital. PLoS ONE. 2012;7:1–9.
De Hoog GS, Guarro J, Gené J, Figueras MJ. Atlas of clinical fungi. 2011. 2th [electronic version 3.1] ISBN/EAN: 978-90-70351-65-6.
Gudlaugsson O, Gillespie S, Lee K, et al. Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis. 2003;37:1172–7.
Richet H, Roux P, Des Champs C, et al. Candidemia in French hospitals: incidence rates and characteristics. Clin Microbiol Infect. 2002;8:405–12.
Fortún J, Martín-Dávila P, Pedrosa EGG, et al. Emerging trends in candidemia: a higher incidence but a similar outcome. J Infect. 2012;65:64–70.
França JCB, Ribeiro CEL, Queiroz-Telles F. Candidemia in a Brazilian tertiary care hospital: incidence, frequency of different species, risk factors and antifungal susceptibility. Rev Soc Bras Med Trop. 2008;41:23–8.
Gómez J, García-Vázquez E, Espinosa C, et al. Nosocomial candidemia at a general hospital: the change of epidemiological and clinical characteristics. A comparative study of 2 cohorts. Rev Iberoam Micol. 2009;26:184–8.
Ajenjo MCH, Aquevedo AS, Guzmán AMD, et al. Epidemiological profile of invasive candidiasis in intensive care units at a university hospital. Rev Chilena Infectol. 2011;28:118–22.
Chalmers C, Gaur S, Chew J, et al. Epidemiology and management of candidaemia: a retrospective, multicentre study in five hospitals in the UK. Mycoses. 2011;54:e795–800.
Bassetti M, Taramasso L, Nicco E, et al. Epidemiology, species distribution, antifungal susceptibility and outcome of nosocomial candidemia in a tertiary care hospital in Italy. PLoS ONE. 2011;6:1–6.
Nucci M, Colombo AL. Candidemia due to Candida tropicalis: clinical, epidemiologic, and microbiologic characteristics of 188 episodes occurring in tertiary care hospitals. Diagn Microbiol Infect Dis. 2007;58:77–82.
Hinrichsen SL, Falcão E, Vilella TAS, et al. Candidemia in a tertiary hospital in northeastern Brazil. Rev Soc Bras Med Trop. 2008;41:394–8.
Ghahri M, Mirhendi H, Fooladi AAI, Beyraghi S. Species identification of candida strains isolated from patients with candidemia, hospitalized in Tehran, by enzymatic digestion of ITS-rDNA. J Isfaham Med School. 2012;29. http://www.jims.mui.ac.ir/index.php/jims/article/view/1393/1853. Accessed 30 Jan. 2013.
Medrano DJA, Brilhante RSN, Cordeiro RA, et al. Candidemia in a Brazilian hospital: the importance of Candida parapsilosis. Rev Inst Med Trop Sao Paulo. 2006;48:17–20.
Nucci M, Silveira MI, Spector N, et al. Fungemia in cancer patients in Brazil: predominance of non-albicans species. Mycopathologia. 1998;141:65–8.
Ha YE, Peck KR, Joo EJ, et al. Impact of first-line antifungal agents on the outcomes and costs of candidemia. Antim Agents Chemother. 2012. http://aac.asm.org/content/early/2012/04/17/AAC.06258-11.abstract. Accessed 30 Jan. 2013.
Nucci M, Queiroz-Telles F, Alvarado-Matute T, et al. Epidemiology of candidemia in Latin America: a laboratory-based survey. PLoS ONE. 2013;8:e59373.
Acknowledgments
Cor Jesus Fernandes Fontes, PhD for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoffmann-Santos, H.D., Paula, C.R., Yamamoto, A.C.A. et al. Six-Year Trend Analysis of Nosocomial Candidemia and Risk factors in Two Intensive Care Hospitals in Mato Grosso, Midwest Region of Brazil. Mycopathologia 176, 409–415 (2013). https://doi.org/10.1007/s11046-013-9705-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-013-9705-5