Abstract
Despite the fact that a range of molecular methods have been developed as tools for the diagnosis of Malassezia species, there are several drawbacks associated with them, such as inefficiency of differentiating all the species, high cost, and questionable reproducibility. In addition, most of the molecular methods require cultivation to enhance sensitivity. Therefore, alternative methods eliminating cultivation and capable of identifying species with high accuracy and reliability are needed. Herein, a multiplex polymerase chain reaction (PCR)-based method was especially developed for the detection of eleven Malassezia species. The multiplex PCR was standardized by incorporating a consensus forward primer, along with Malassezia species-specific reverse primers considering the sizes of the PCR products. In the method, the multiplex-PCR primer content is divided into three parts to circumvent the problem of increased nonspecific background resulting from the use of a large number of primers. DNA extraction protocol described by Harju and colleagues was modified using liquid nitrogen instead of −80 °C to break down the yeast membrane. By a modified extraction procedure followed by multiplex PCR and electrophoresis, the method enables identification and differentiation of Malassezia species from both of the samples obtained directly from skin and yeast colonies grown in culture. Fifty-five patients who were confirmed with pityriasis versicolor were enrolled in the study. Multiplex PCR detected and differentiated all 55 samples obtained directly from the patients’ skin. However, 50 out of 55 samples yielded Malassezia colony in the culture. In addition, eight of 50 colonies were misdiagnosed or not completely differentiated by conventional methods based on the sequence analysis of eight colonies. The method is capable of identifying species with high accuracy and reliability. In addition, it is simple, quick, and cost-effective. More importantly, the method works efficiently for the diagnosis of Malassezia species obtained directly from patient samples.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
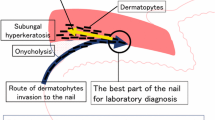
The Malassezia species are implicated in the pathogenesis of common skin diseases such as pityriasis versicolor (PV), atopic dermatitis, seborrheic dermatitis, and psoriasis. Additionally, the species M. pachydermatis and M. furfur can cause systemic infections [1, 2]. The major antifungal agents are the main choice treatment for Malassezia infection. However, there are variations in the susceptibilities of Malassezia spp. to major antifungal drugs, including tacrolimus, and the azole agents itraconazole and ketoconazole [3, 4].
On the basis of common DNA sequences and molecular methods, Malassezia species expanded to 14 species [5]. Remarkably, 10 of them including M. globosa, M. restricta, M. sympodialis, M. furfur, M. obtusa, M. slooffiae, M. pachydermatis, M. dermatis, M. japonica, and M. yamatoensis were found to be related to human diseases [2, 5]. Several investigators involved in Malassezia yeast research still use the culture-based techniques based on their morphology and biochemical features [6–8]. The phenetic analyses, however, are usually a time-consuming, multistep process, necessitating several experimental techniques [5].
To overcome this limitation, studies have used a variety of molecular methods such as the nested polymerase chain reaction (PCR), real-time PCR, pulsed-field gel electrophoresis (PFGE), amplified fragment length polymorphism (AFLP), denaturing gradient gel electrophoresis (DGGE), random amplification of polymorphic DNA (RAPD), single-strand conformation polymorphism, terminal fragment length polymorphism, restriction fragment length polymorphism (RFLP), and sequence analysis [5, 9]. Despite the usefulness of these molecular techniques, there are several drawbacks associated with them, such as inefficiency of differentiating all the species, requirement of technical devices, high cost of analysis, and questionable reproducibility. In addition, most of the methods mentioned above require cultivation to enhance sensitivity, thereby increasing both the potential for culture bias and the turnaround time for analysis [5].
The discrepancies between molecular methods and culture-based techniques showed that there is the need for well-controlled, comparative PCR studies of samples taken directly from the skin as well as the same samples following in vitro culturing. Therefore, objectives of this study were to increase the sensitivity of the method to eliminate the need for cultivation and thereby increase the detection rate and eliminate cultural bias in the results. In this investigation, an alternative multiplex PCR-based method developed for the detection of 11 Malassezia species is presented. By a modified extraction procedure followed by multiplex PCR and electrophoresis, the method enables identification and differentiation of 11 Malassezia species from both of the samples obtained directly from skin and yeast colonies grown in culture.
Materials and Methods
Standard Strains
Eleven reference strains, including M. dermatis (CBS 9,145), M. furfur (CBS 7,019), M. japonica (CBS 9,432), M. globosa (CBS 7,966), M. nana (CBS 9,561), M. obtusa (CBS 7,876), M. pachydermatis (CBS 1,879), M. slooffiae (CBS 7,956), M. sympodialis (CBS 7,222), M. yamatoensis (CBS 9,725), and M. restricta (CBS 7,877), were purchased from the Centraalbureau voor Schimmelcultures Fungal Biodiversity Centre, Utrecht, The Netherlands.
Patients
A total of 62 patients clinically suspected of PV, referred to the Mycology Laboratory of the Ankara University of School of Medicine, were recruited. Fifty-five patients were confirmed with PV, based on the presence of both hyphae and yeasts in direct microscopy; the Malassezia spp. were isolated from 50 patients. The samples from the 55 patients and 50 Malassezia spp. grown in the culture were used in the tests.
Collection and Culture of Sample
Samples were collected by scraping the skin with a sterile blunt scalpel blade in sterile petri dishes. The amount of samples is around 5–10 mg. The only inclusion criterion was the presence of a sufficient amount of material for investigation by DNA extraction and culture analysis. Half of the samples were used directly for DNA extraction, and the other half was inoculated in modified Leeming–Notman agar (MLNA) (1 % w/v peptone, 1 % w/v glucose, 0.2 % w/v yeast extract, 0.8 % desiccated ox bile, 0.1 % v/v glycerol, 0.05 % w/v glycerol monostearate, 0.5 % v/v Tween 60, 2 % v/v oleic acid, and 1 % w/v agar in distilled water) supplemented with cycloheximide (0.5 %) and chloramphenicol (0.05 %) as recommended by Sugita et al. [10]. The culture was incubated at 32 °C for 2 weeks.
Morphological and Physiological Characteristics
Growth in Sabouraud dextrose agar (SDA) (Becton, Dickinson and Company, NJ, USA), morphological examination on MLNA after incubation at 32 °C for 7 days, Tween 20, 40, 60, and 80 utilization, and catalytic reactions were performed [11–13].
Designing Primers for M-PCR
The forward primer assigned as ITSANA-F was chosen from highly conserved regions within 5.8S ribosomal RNA of Malassezia species using a multiple DNA sequence alignment program (http://www.ebi.ac.uk/clustalw). Reverse primers for the individual Malassezia species were chosen from the Malassezia strains’ DNA sequences considering specificity to individual strains’ DNA sequences and size of the PCR product. The primers for the strains and the expected size of the PCR products are shown in Table 1. The GenBank accession numbers of the sequences used in the study are as follows: M. dermatis AY390285, M. furfur HM014469, M. japonica EF140669, M. globosa KC152884, M. nana EF140667, M. obtusa GU291269, M. pachydermatis FJ545240, M. slooffiae EU915458, M. sympodialis AY743650, M. yamatoensis AB125262, and M. restricta EU400587. In addition to these, the sequences of the other strains of the individual species were also considered during the primer selection. The accuracy of the designed primers was confirmed by NCBI-BLAST program. Primers were synthesized by the company Integrated DNA Technologies, Coralville, IA.
DNA Extraction
For DNA extraction from both the scraped skin samples and the fresh yeast colonies grown in culture, methods of Harju et al. [14] with some modification were used. Skin samples or colonies were resuspended in 200 μL of lysis buffer [2 % Triton X-100, 1 % SDS, 100 mM NaCl, 10 mM Tris–HCl (pH 8.0), and 1 mM EDTA (pH 8.0)]. The tubes were placed in liquid nitrogen until they were completely frozen and thawed at boiling water for 30 s. The process was repeated two times, and the tubes were vortexed vigorously for 30 s at each repetition. Two hundred microliters of phenol–chloroform was added, and the tubes were vortexed for 2 min and then centrifuged for 3 min at room temperature at 10,000×g. The aqueous layer was transferred to a tube containing 500 μL of ice-cold 100 % ethanol. The samples were centrifuged for 12 min at 4 °C at 12,000×g. Supernatants were discarded, and DNA pellets were washed with 1 mL of 70 % ethanol followed by drying at room temperature. DNA was resuspended in 50 μL double-distilled H2O. The whole DNA extraction procedure takes 30–40 min.
DNA Amplification
DNA amplification was carried out in sterile ultrapure water with PCR buffer, with 1.5 mmol/L MgCl2 (Fermentas-Life science technologies, Vilnius, Lithuania), 100 μmol/L each of dNTPs (Fermentas-Life science technologies), 0.5 μmol/L each of oligonucleotides, and 2.5 U of Taq DNA polymerase (Fermentas-Life science technologies), in a 0.2-mL sterile thin-walled PCR tube, with a total volume of 50 μL. Using an Eppendorf Mastercycler personal thermocycler, template DNAs were initially denatured at 94 °C for 2 min. After this cycle, 39 thermocycles, each consisting of 30 s at 94 °C, 45 s at 60 °C, and 45 s at 72 °C, were performed. To ensure complete extension, the reaction mixtures were further incubated for 10 min at 72 °C. Amplified DNA was analyzed by gel electrophoresis using 2.0 % (w/v) agarose in a Tris–borate buffer containing ethidium bromide for detection of DNA under ultraviolet transillumination. One-kilobase marker was used to confirm the size of resolved DNA.
Subcloning of PCR Products and PCR Sensitivity Assay
To obtain well-characterized positive controls and to determine the further sensitivity of the PCR method, we cloned the PCR products of each of the Malassezia strains into the pBSK vector. Briefly, individual virus DNA sequences were amplified with the primers and control yeast DNAs described herein above, followed by gel extraction and cleaning of PCR product using the gene clean kit (GeneMark, Hopegen Biotechnology, Dali City, Taiwan). For subcloning of the PCR product into pBSK vector plasmid, first, pBSK-T PCR cloning vector was prepared. Briefly, pBSK vector was cut with EcoRV enzyme followed by the T nucleotide added to the ends of vector using dTP, DNA polymerase, and appropriate buffer (Fermentas-Life science technologies). The individual Malassezia PCR products were subcloned into pBSK-T vector using T4 ligation enzyme (Fermentas-Life science technologies). Prepared pBSK-M. dermatis, pBSK-M. furfur, pBSK-M. japonica, pBSK-M. globosa, pBSK-M. nana, pBSK-M. obtusa, pBSK-M. pachydermatis, pBSK-M. slooffiae, pBSK-M. sympodialis, pBSK-M. yamatoensis, and pBSK-M. restricta plasmids were used to define the M-PCR sensitivity. To determine the sensitivity of the PCR assay, we diluted individual plasmid stock preparations at 1 × 104 copies/μL in tenfold steps to 1 × 10−1 copies/μL and completed the PCR.
M-PCR
Multiplex PCR was performed in three PCR tubes considering the sizes of the PCR products to differentiate 11 Malassezia species. According to their sizes, the PCR products were categorized into four groups: Sizes of the M. restricta, M. pachydermatis, and M. slooffiae PCR products are between 135 and 150 bp; sizes of the M. sympodialis, M. obtusa, and M. nana PCR products are between 204 and 207 bp; sizes of the M. japonica, M. furfur, and M. yamatoensis PCR products are between 250 and 256 bp; and sizes of the M. globosa and M. dermatis PCR products are between 330 and 345 bp as shown in Table 1. Primers for the three multiplex PCR tubes were arranged such that the first multiplex PCR tube contains primers for M. restricta, M. sympodialis, M. japonica, M. globosa, and ITSANA-F; the second multiplex PCR tube contains primers for M. pachydermaditis, M. obtusa, M. furfur, M. dermatis, and ITSANA-F; and the third multiplex PCR tube contains primers for M. slooffiae, M. nana, M. yamatoensis, and ITSANA-F.
DNA Sequencing
DNA sequencing was performed with BigDye terminator sequencing chemistry on an automatic DNA sequencer ABI 377 (Applied Biosystems, Foster City, CA, USA). DNAs of the seven Malassezia species which were unidentified or identified different with the conventional method were sequenced to verify the specificity of the multiplex PCR. PCR products were obtained using primers ITSANA-F and ITSANA-R from the DNAs of the individual colonies, and DNA sequencing was performed using the same primers. The n-BLAST program was used for sequence analysis.
Results
The Evaluation and the Efficacy of the Modified DNA Extraction Protocol
DNA extraction protocol described by Harju and colleagues was modified using liquid nitrogen instead of −80 °C to break down the yeast membrane. Ten skin samples and 10 grown colonies were subjected to DNA extraction methods of Harju et al. and modified method. Clear and strong bands were obtained from 20 PCRs in which DNAs were obtained using modified extraction method. No bands or weak bands were obtained from 20 PCRs in which DNAs obtained using DNA extraction protocol were described by Harju and colleagues.
Analysis of M-PCR Products
The sensitivity of combinations of primer pairs is tested with simple PCR and the consensus, and reverse primers that give the best results were selected. In this step, the sensitivity evaluation of the primer sets was made according to the density of the PCR products in agarose gel. The further sensitivity of multiplex PCR was determined using different dilution of individual pBSK plasmids containing PCR product of the individual Malassezia. We found that multiplex PCR can detect as low as 10–100 DNA copies in 50 μL of PCR tube depending on plasmids described in “Materials and Methods.” The next step includes performing multiplex PCR in three PCR tubes as described in “Materials and Methods.” The multiplex PCR can recognize and differentiate all individual DNAs of the strains in each PCR tube (Fig. 1). The sizes of the PCR products were observed around the range of 150, 200, 250, and 340 bp in the agarose gel as expected (Table 1).
Results of M-PCRs using the first, second, and third M-PCR tubes with template DNAs obtained from standard Malassezia strains. M molecular size marker, 1 M. restricta, 2 M. sympodialis, 3 M. japonica, 4 M. globosa, 5 M. pachydermaditis, 6 M. obtusa, 7 M. furfur, 8 M. dermatis, 9 M. slooffiae, 10 M. nana, 11 M. yamatoensis, and 12 and 13 negative control
Specificity of Multiplex PCR
In the next experiment, the DNAs of the individual standard Malassezia strains were tested. As seen in Fig. 1, the first multiplex PCR tube identified and differentiated the DNAs of M. restricta, M. sympodialis, M. japonica, and M. globosa, but not the DNAs obtained from the other strains. The second multiplex PCR tube identified and differentiated the DNAs of M. pachydermaditis, M. obtusa, M. furfur, and M. dermatis individual DNAs, but not the DNAs obtained from the other strains, and the third multiplex PCR tube identified and differentiated the DNAs of M. slooffiae, M. nana, and M. yamatoensis, but not the DNAs obtained from the other strains.
In addition to DNAs of the Malassezia strains, DNAs of clinically isolated microorganisms, including Staphylococcus aureus, Escherichia coli, Candida albicans, Trichophyton rubrum, Microsporum canis, and Aspergillus fumigatus, and human DNA were tested with each of the multiplex PCR tubes for the specificity of technique. No PCR products were obtained with template DNAs used with each of the M-PCR tubes (Fig. 2).
Evalution of the specificity of the M-PCRs. M. molecular size marker, 1, 2, 3, and 4 are positive controls, for M-PCR tube 1: 1 M. restricta, 2 M. sympodialis, 3 M. japonica, and 4 M. globosa; for M-PCR tube 2: 1 M. pachydermaditis, 2 M. obtusa, 3 M. furfur, and 4 M. dermatis; for M-PCR tube 3: 1 M. slooffiae, 2 M. nana, 3 M. yamatoensis, 5 S. aureus, 6 E. coli, 7 C. albicans, 8 T. rubrum, 9 M. canis, 10 A. fumigatus, 11 human DNA, and 12 negative control
Comparison of Conventional Methods and Multiplex PCR for Identification and Differentiation of Malassezia Strains
Of 62 skin scrapings, 55 were microscopically positive for Malassezia elements. Fifty-five samples were tested with the M-PCR. M-PCR diagnosed and differentiated Malassezia strains in all 55 samples (Table 2). Fifty (90 %) of the microscopically positive specimens yielded Malassezia colony in the culture. Grown colonies were tested with conventional methods described in “Materials and Methods” section. DNAs were extracted from colonies grown in culture and used in multiplex PCR. Identical multiplex PCR results were obtained with DNA templates extracted from the colonies or skin samples obtained from the patients (Table 2). The conventional methods, however, led to different results for eight yeasts grown in culture. While three colonies were identified as M. obtusa with the conventional methods, multiplex PCR identified them as M. globosa. In addition to this, the conventional methods were unable to differentiate four Malassezia strains completely (Table 2). The PCR products of each of yeasts were sequenced. Sequences obtained were subjected to a BLAST search with registered sequences in the GenBank database. Results of sequence analysis with the BLAST program revealed that out of the examined yeasts, three were M. globosa and the remaining five were M. slooffiae, which is the same result obtained with multiplex PCR (Fig. 3; Table 2).
Results of multiplex PCRs using DNAs obtained from the skin of the patients. M, 1-kb-molecular-size marker: For the multiplex PCR tube 1, lanes 1 and 31 are positive control of M. restricta; lanes 2 and 32 are positive control of M. sympodialis; lanes 3 and 33 are positive control of M. japonica; and lanes 4 and 34 are positive control of M. globosa. For the multiplex PCR tube 2, lanes 1 and 31 are positive control of M. pachydermaditis; lanes 2 and 32 are positive control of M. obtusa; lanes 3 and 33 are positive control of M. furfur; and lanes 4 and 34 are positive control of M. dermatis. For the multiplex PCR tube 3, lanes 1 and 31 are positive control of M. slooffiae; lanes 2 and 32 are positive control of M. nana; and lanes 3 and 33 are positive control of M. yamatoensis. For the multiplex PCR tube 1 and tube 2, lanes 5–29, 35–59 are the results of the multiplex PCR performed for DNA templates obtained directly from the patients. For the multiplex PCR tube 3, lanes 4–28, 34–58 are the results of the multiplex PCR performed for DNA templates obtained directly from the patients
Discussion
A multiplex PCR-based diagnostic assay can use different primers specific to different species in a single test, which means that it can combine different diagnostic tests for different microorganisms into a single, comprehensive, all-encompassing test. However, using a large number of primers in a single PCR may increase the nonspecific background. An approach to decrease nonspecific background is using consensus forward and reverse primer pair [15]. In this study, a new multiplex PCR technique that can diagnose and differentiate 11 Malassezia species is developed. In this new technique, we divided the multiplex-PCR primer content into three parts to circumvent the problem of nonspecific background resulting from the use of a large number of primers in a single PCR. In addition to this, we used consensus forward primer, which could recognize all of Malassezia strains in the multiplex PCR, to decrease the primer numbers in each multiplex PCR tube. It is assumed that these approaches decrease nonspecific background and increase the sensitivity and specificity.
As culture-based methods do not always allow the species-specific identification, a range of molecular methods have been developed as tools to diagnose and differentiate Malassezia strains [5, 9]. Fingerprinting molecular methods such as DGGE, PFGE, RAPD, and AFLP have been employed to screen genomes for the identification and differentiation of Malassezia spp. In spite of their utility, each technique has its own limitation. Most of them are time-consuming to conduct and are thus less suited as a routine diagnostic tool. For example, although useful, DGGE and PFGE are time-consuming to perform and technically difficult, and PFGE requires large amounts of high molecular weight genomic DNA for analysis. RAPD has limited reproducibility of results. AFLP is relatively time-consuming to conduct (because of the digestion and ligation steps involved) [5]. Importantly, most of the methods mentioned above require cultivation to perform the test. Five studies have been reported to differentiate complex Malassezia strains from skin without cultivation [16, 17]. Four of them require either separate amplification with specific primer sets for each species or restriction digestion [16–18]. The other study used nested PCR which needed more than one PCR. In addition to time and technical requirements, the method was used for the detection of only six Malassezia species [17].
Therefore, in this study, the focus is placed on testing the multiplex PCR with the samples taken directly from the skin. Initially, the effectiveness of multiplex PCR is validated with DNA templates obtained from the skin and standard Malassezia strains using extraction method described by Harju et al. [14]. Since relatively low-yielding PCR products or no products were obtained from both samples, DNA extraction method is found to be ineffective. Hence, liquid nitrogen was used instead of the −80 °C freezer to break down the yeast membrane. This modification in DNA extraction increased sensitivity of the multiplex PCR dramatically in both samples obtained from the skin and the yeast grown in culture.
The samples from the 55 patients diagnosed with PV were tested with the multiplex PCR. The multiplex PCR identified and differentiated Malassezia species in all the 55 samples obtained directly from the skin. The isolation rate of Malassezia spp. was found to be 90 % similar to some other studies [19, 20]. In addition to low isolation rate of conventional method, eight samples were misdiagnosed or not completely differentiated with the conventional method. DNA sequence analysis of the seven strains confirmed that results of the multiplex PCR were correct. Similar to our results, most studies have shown some discrepancies between phenotypic and molecular-based identifications of Malassezia. In a study of 46 clinical isolates, identified using a conventional phenotypic approach as M. furfur, 22 were genetically identified as M. sympodialis and five as M. slooffiae by sequencing of the ITS-1 region [21]. In another study, an apparent misidentification rate of 13.8 % was recorded by comparing the results from AFLP as well as ITS sequencing with those based on the physiological identification of Malassezia spp. For example, one isolate identified previously as M. furfur was classified as M. sympodialis, and three isolates identified as M. globosa were categorized as M. sympodialis [22].
The multiplex PCR tests performed with templates obtained from the yeast–serum mixture showed that M-PCR can effectively identify Malassezia extracted from the serum. Therefore, one may conclude that the multiplex PCR can be used for the identification and differentiation of Malassezia that causes systemic infections [2].
In conclusion, a new multiplex PCR method is developed that can be applied for the identification of 11 Malassezia strains. This new method requires only PCR, therefore technically less demanding than most other molecular biological approaches and conventional methods. The method is capable of identifying species with high accuracy and reliability and would be simple, fast, and cost-effective for application. More importantly, the method works efficiently for the diagnosis of Malassezia species obtained directly from patient samples.
References
Chryssanthou E, Broberger U, Petrini B. Malassezia pachydermatis fungaemia in a neonatal intensive care unit. Acta Paediatr. 2001;90(3):323–7.
Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev. 2012;25(1):106–41.
Miranda KC, de Araujo CR, Costa CR, Passos XS, de Fernandes OFL, do Rosario Rodrigues Silva M. Antifungal activities of azole agents against the Malassezia species. Int J Antimicrob Agents. 2007;29(3):281–4.
Sugita T, Tajima M, Ito T, Saito M, Tsuboi R, Nishikawa A. Antifungal activities of tacrolimus and azole agents against the eleven currently accepted Malassezia species. J Clin Microbiol. 2005;43(6):2824–9.
Cafarchia C, Gasser RB, Figueredo LA, Latrofa MS, Otranto D. Advances in the identification of Malassezia. Mol Cell Probes. 2011;25(1):1–7.
Cabanes FJ, Theelen B, Castella G, Boekhout T. Two new lipid-dependent Malassezia species from domestic animals. FEMS Yeast Res. 2007;7(6):1064–76.
Gueho E, Midgley G, Guillot J. The genus Malassezia with description of four new species. Antonie Van Leeuwenhoek. 1996;69(4):337–55.
Sugita T, Takashima M, Shinoda T, Suto H, Unno T, Tsuboi R, et al. New yeast species, Malassezia dermatis, isolated from patients with atopic dermatitis. J Clin Microbiol. 2002;40(4):1363–7.
Gaitanis G, Bassukas ID, Velegraki A. The range of molecular methods for typing Malassezia. Curr opin infect dis. 2009;22(2):119–25.
Sugita T, Tajima M, Takashima M, Amaya M, Saito M, Tsuboi R, et al. A new yeast, Malassezia yamatoensis, isolated from a patient with seborrheic dermatitis, and its distribution in patients and healthy subjects. Microbiol Immunol. 2004;48(8):579–83.
Sugita T, Tajima M, Tsubuku H, Tsuboi R, Nishikawa A. Quantitative analysis of cutaneous malassezia in atopic dermatitis patients using real-time PCR. Microbiol Immunol. 2006;50(7):549–52.
Senczek D, Siesenop U, Bohm KH. Characterization of Malassezia species by means of phenotypic characteristics and detection of electrophoretic karyotypes by pulsed-field gel electrophoresis (PFGE). Mycoses. 1999;42(5–6):409–14.
Ayhan M, Sancak B, Karaduman A, Arikan S, Sahin S. Colonization of neonate skin by Malassezia species: relationship with neonatal cephalic pustulosis. J Am Acad Dermatol. 2007;57(6):1012–8.
Harju S, Fedosyuk H, Peterson KR. Rapid isolation of yeast genomic DNA: bust n’ Grab. BMC Biotechnol. 2004;4:8.
Sahin F, Gerceker D, Karasartova D, Ozsan TM. Detection of herpes simplex virus type 1 in addition to Epstein–Bar virus in tonsils using a new multiplex polymerase chain reaction assay. Diagn Microbiol Infect Dis. 2007;57(1):47–51.
Amaya M, Tajima M, Okubo Y, Sugita T, Nishikawa A, Tsuboi R. Molecular analysis of Malassezia microflora in the lesional skin of psoriasis patients. J Dermatol. 2007;34(9):619–24.
Gemmer CM, DeAngelis YM, Theelen B, Boekhout T, Dawson TL Jr. Fast, noninvasive method for molecular detection and differentiation of Malassezia yeast species on human skin and application of the method to dandruff microbiology. J Clin Microbiol. 2002;40(9):3350–7.
Zhang H, Ran Y, Xie Z, Zhang R. Identification of Malassezia species in patients with seborrheic dermatitis in China. Mycopathologia. 2013;175(1–2):83–9.
Shokohi T, Afshar P, Barzgar A. Distribution of Malassezia species in patients with pityriasis versicolor in Northern Iran. Int J Med Microbiol. 2009;27(4):321–4.
Nakabayashi A, Sei Y, Guillot J. Identification of Malassezia species isolated from patients with seborrhoeic dermatitis, atopic dermatitis, pityriasis versicolor and normal subjects. Med Mycol. 2000;38(5):337–41.
Makimura K, Tamura Y, Kudo M, Uchida K, Saito H, Yamaguchi H. Species identification and strain typing of Malassezia species stock strains and clinical isolates based on the DNA sequences of nuclear ribosomal internal transcribed spacer 1 regions. J Med Microbiol. 2000;49(1):29–35.
Gupta AK, Boekhout T, Theelen B, Summerbell R, Batra R. Identification and typing of Malassezia species by amplified fragment length polymorphism and sequence analyses of the internal transcribed spacer and large-subunit regions of ribosomal DNA. J Clin Microbiol. 2004;42(9):4253–60.
Acknowledgments
This work was supported by The Scientific and Technological Research Council of Turkey (TUBITAK) with project No. 111S037.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vuran, E., Karaarslan, A., Karasartova, D. et al. Identification of Malassezia Species from Pityriasis Versicolor Lesions with a New Multiplex PCR Method. Mycopathologia 177, 41–49 (2014). https://doi.org/10.1007/s11046-013-9704-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-013-9704-6