Abstract
Inflammatory cytokine, adipokine and adhesion molecules are known to play a key role in pathogenesis of diabetic kidney disease (DKD). In this study, our aim was to investigate the role of fetuin-A in relation with pro-inflammatory cytokines (IL-6, IL-18), adipokines (adiponectin, leptin), chemokine (MCP-1), and adhesion molecules (ICAM-1, VCAM-1) in control and DKD subjects. We recruited a total of 224 type 2 diabetic (T2D) subjects. The control subjects were T2D with a normal albumin excrete (albumin-to-creatinine ratio—ACR ≤ 30 mg/g creatinine) and estimated glomerular filtration rate (eGFR) ≥ 60 (ml/min/1.73 m2), while cases were T2D subjects with albumin excrete (ACR ≥ 30 mg/g creatinine) and eGFR ≤ 60 (ml/min/1.73 m2). FBS, HbA1c, lipid profile (TC, LDL, HDL, triglyceride), ALT, AST, GGT, serum creatinine, BMI, blood pressure was evaluated in all the study subjects. Randox evidence biochip analyzer was used for measuring inflammatory cytokines, adipokines, and adhesion molecules by chemiluminescent assay. Serum fetuin-A and IL-18 were measured by ELISA kits. Serum fetuin-A levels were significantly decreased in DKD cases compare to control group [456.8 (299.2–649.0) µg/ml versus 670.6 (573.0–726.1) µg/ml; p < 0.001)]. Serum fetuin-A levels correlates significantly with IL-6, IL-18, TNF-α, PAI-1, leptin, resistin and ACR (p < 0.001). This study concludes that serum fetuin-A and pro-inflammatory markers (IL-18, IL-6, IL-1α and TNF-α) might play an important role in the pathophysiology and inflammatory process of DKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus (DM) is a metabolic disease with an increasing global prevalence. According to the International Diabetes Federation (IDF), an estimated 425 million people worldwide had diabetes in 2017, while it is predicted that the number of cases will increase to 629 million by 2045. Diabetic kidney disease (DKD), a major microvascular complication of type 1 diabetes (T1D) and type 2 diabetes (T2D), remains the most common cause of end-stage kidney disease (ESKD) worldwide [1].
Poor glycemic control and uncontrolled diabetes lead to the generation of advanced glycation end products (AGEs) and oxidative stress, resulting in endothelial dysfunction via inflammation [2]. Several inflammatory pathways play a key role in the pathophysiology of DKD. Proinflammatory cytokines and signaling cascades that participate in the pathophysiology of DKD include pro-inflammatory molecules [interleukin-6 (IL-6), interleukin-18 (IL-18), interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α)], adhesion molecules [vascular cell adhesion molecule-1 (VCAM-1), intercellular cell adhesion molecule-1 (ICAM-1), E-Selectin], transcription factor (nuclear factor-kappa B [NFkB]), and chemokines [monocyte chemoattractant protein-1 (MCP-1), chemokine (C-X3-C motif) ligand 1 (CX3CL1 or fractalkine), C–C motif chemokine ligand 5 (CCL5 or RANTES) and their receptors (C–C chemokine receptor type 2 [CCR2], CX3C chemokine receptor 1 [CX3CR1], C-C chemokine receptor type 5 [CCR5])] [2]. All inflammatory signaling molecules are interconnected with kidney injury, and induce the activation of several signaling pathways in different renal cell types (mesangial, epithelial, tubular, endothelial, and podocytes) [3]. For instance, several studies reported that increased serum IL-18 and IL-6 expression levels are correlated with the progression of DKD [4, 5]. Furthermore, studies have also reported that the expression levels of cell adhesion molecule ICAM-1 and VCAM-1 increase in response to pro-inflammatory cytokines in DKD [6, 7].
Fetuin-A is an anti-inflammatory protein that can attenuate the inflammatory response, and is highly expressed in hepatocytes. It is negatively regulated by several pro-inflammatory cytokines, while its production is down-regulated by the inflammatory response. Hence, fetuin-A is regarded as a “negative acute phase reactant” [8]. Previously, it was reported that fetuin-A plays a substantial role in the pathogenesis of DKD by suppressing adiponectin [9].
In the current study, our aim was to understand the role of fetuin-A in DKD. Specifically, we evaluated the relationship between serum fetuin-A levels, and levels of pro-inflammatory cytokines (IL-18, IL-6, IL-1α TNF-α, resistin), adipokines (leptin, adiponectin), chemokine (MCP-1), and adhesion molecules (ICAM-1, VCAM-1), in DKD.
Methods
Study participants
In this case–control study, all the subjects were matched for age, sex, BMI, and diabetes duration. The study subjects were selected from Saudi Diabetes Kidney Disease (SAUDI-DKD) cohort. The exclusion and inclusion criteria were as previously reported [10]. This study was performed at the University Diabetes Center, King Saud University, Riyadh, during the period from April 2014 to June 2015.
In the present study, 224 T2D subjects aged 37–66 years were selected as participants according to American Diabetes Association criteria [11]. Patients were categorized and diagnosed in accordance with the Chronic Kidney Disease (CKD) nomenclature in Kidney Disease: Improving Global Outcomes (KDIGO) guidelines [12]. Patients were placed in one of two groups, followed by the assessment of albumin-to-creatinine ratio (ACR). Estimated glomerular filtration rate (eGFR) was measured using the CKD–Epidemiology Collaboration (EPI) equation [13]. Each subject was categorized as a ‘control’ or ‘case’ according to the subject’s ACR and eGFR. The control subjects were those with a normal albumin excrete (ACR ≤ 30 mg/g creatinine) as well as eGFR ≥ 60 (ml/min/1.73 m2), while cases were subjects with a greater than normal albumin excrete (ACR ≥ 30 mg/g creatinine) as well as eGFR ≤ 60 (ml/min/1.73 m2).
This study was approved by the institutional review committee of the College of Medicine (King Saud University, Riyadh). Written informed consent was obtained from each subject. We used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) case–control checklist for writing our report [14].
Subjects with a medical history were recruited to the study, and their demographic measurements were recorded, on the same day that they visited a physician. Body mass index (BMI) (kg/m2) was calculated by dividing weight (kg) by height squared (m2). In all the study subjects, sitting blood pressure was measured using a mercury sphygmomanometer. Information on smoking status was obtained from self-reported questionnaires and recorded as non-smokers or smokers.
Biochemical assessment
We obtained 10 ml of fasting venous blood in a plain tube from each subject at one time point. Blood samples were centrifuged and serum samples were stored at − 20 °C until analysis. The biochemical assessment for each patient included fasting blood sugar (FBS), HbA1c, serum creatinine, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglyceride, total cholesterol (TC), alanine transaminase (ALT), aspartate transaminase (AST), gamma glutamyl transferase (GGT), albumin, and total bilirubin, which were measured using established enzymatic methods (RX-Daytona chemistry analyzer, Randox, UK).
Measurement of serum biomarkers
Serum biomarker levels were measured using the Randox Evidence Biochip analyzer (Randox Laboratories Ltd., Crumlin, UK). Metabolic syndrome array I [IL-6, IL-1α, insulin, leptin, plasminogen activator inhibitor-1 (PAI-1), resistin, TNF-α] (Randox evidence, Catalog No. EV3754), metabolic syndrome array II (adiponectin) (Randox evidence, Catalog No. EV3758), and adhesion array (VCAM-1, ICAM-1) (Randox evidence, Catlog No. EV3572) were performed. IL-18 and MCP-1 levels were determined using ELISA kits (Abcam, Catalog Nos. ab100586 and ab100559, Cambridge, USA). Serum fetuin-A levels were measured using an ELISA kit (Biovendor, Catalog No: RD191037100, Czech Republic).
Statistical analysis
Statistical analysis was carried out using SPSS software version 21.0 (SPSS Inc., Chicago, USA). The results are presented as mean ± standard deviation for normally distributed variables and median (interquartile range) for skewed variables. The Chi-square test was performed to compare categorical data. We compared the correlation of serum fetuin-A, inflammatory markers, adipokines, and adhesion molecules using bivariate correlation analysis. A p value of ≤ 0.05 was considered to be statistically significant.
Results
Demographic information
The demographic and biochemical parameters of the study subjects are presented in Table 1. In this study, both the control and DKD case group were homogenous, and there was no statistically significant difference in their age, sex, smoking status, duration of diabetes, BMI and insulin (p > 0.05). DKD cases had higher systolic blood pressure (144.6 ± 23.8 mmHg; p = 0.001), diastolic blood pressure (75.4 ± 12.9 mmHg; p = 0.040), glycated hemoglobulin (HbA1c %) (10.7 ± 2.0; p = 0.002), FBS (243.4 ± 98.8 mg/dl; p = 0.001), triglyceride (209.6 ± 91.9 mg/dl, p = 0.001), total cholesterol (194.6 ± 46.7 mg/dl; p = 0.001), creatinine (1.32 ± 0.66 mg/dl; p = 0.001), albumin creatinine ratio (229.0 mg/g; p = 0.001) levels compared with control group. Patients with DKD cases also had lower eGFR (59.8 ± 31.0 ml/min/1.73 m2, p = 0.001).
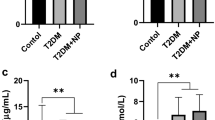
Serum level of fetuin-A, pro-inflammatory cytokines, adipokines, and adhesion molecules in control type 2 diabetes and DKD cases and its clinical significance
The serum biomarkers of the study subjects are presented in Table 2. Patients with DKD cases had higher levels of VCAM-1 (924.1 ng/ml; p = 0.038), ICAM-1 (339.9 ng/ml; p = 0.450), adiponectin (2152 ng/ml; p = 0.230), resistin (6.2 ng/ml; p = 0.001), TNF-α (8.8 pg/ml; p = 0.001), IL-1α (0.23 pg/ml; p = 0.009), IL-6 (3.05 pg/ml; p = 0.001), IL-18 (1755.8 pg/ml; p < 0.001) levels compared with control group. Patients with DKD cases also had lower fetuin-A (456.8 µg/ml; p = 0.001), PAI-1 (26.6 ng/ml; p = 0.002), MCP-1 (49.1 pg/ml; p = 0.007) and leptin (1.5 ng/ml; p = 0.343) levels compare with control group.
Association of fetuin-A, pro-inflammatory cytokines, adipokines, and adhesion molecules
Serum fetuin-A level negatively correlated with IL-6 (r = − 0.239, p = 0.001), IL-18 (r = − 0.198, p = 0.003), TNF-α (r = − 0.257, p = 0.001), leptin (r = − 0.198, p = 0.001), resistin (r = − 0.201, p = 0.004), and ACR (r = − 0.313, p = 0.001). However, no significant correlation was observed between serum fetuin-A level and adiponectin, IL-1α, ICAM-1, VCAM-1, MCP-1 and eGFR as shown in Table 3.
Discussion
This study showed that the levels of pro-inflammatory molecules (IL-18, IL-6, IL-1α and TNF-α) and the adhesion molecule VCAM-1 were higher, while that of the chemokine MCP-1, PAI-1 and fetuin-A were considerable lower, in subjects with DKD. Notably, ICAM-1, leptin and adiponectin levels did not differ considerably between control and DKD subjects.
Hyperglycemia is a leading driving force of diabetic nephropathy development, and its progression to ESKD [2]. Chronic hyperglycemia and oxidative stress cause the accumulation of AGEs, which activate macrophages and induce the impairment of glomerular cells. This causes glomerular cell injury and over-expression of adhesion molecules and cytokines, resulting in macrophage infiltration in kidney tissues, and progression of DKD to ESKD [2, 3].
In the current study, we found a decreased level of fetuin-A in cases when compared to control subjects, providing evidence for its role within the pathological process of DKD. Earlier, a study by Caglar et al. reported decreased concentrations of fetuin-A with decreased eGFR, and indicated fetuin-A as a “risk factor” for endothelial dysfunction in kidney disease [15]. However, another study demonstrated that severe proteinuria correlated with the decrease in fetuin-A concentration [16]. While confirmed in our study, a previous study by Lebreton et al. also suggested that the levels of fetuin-A, which is a “negative acute phase reactant,” are decreased during the inflammatory response [17]. Similar studies have demonstrated that chronic inflammation in hemodialysis subjects lead to lower serum fetuin-A levels [18]. Our understanding the role of fetuin-A is restricted to specific molecules and signaling pathways. The mechanism for negative regulation of fetuin-A induced by inflammation is examined in details by Gangneux et al., they reported that fetuin-A levels transiently decreases during pro-inflammatory cytokine stimulation. Fetuin-A expression is regulated by member of C/EBP transcription factor family. Pro-inflammatory cytokines (TNF-alpha, IL-1beta and IL-6) stimulate liver cells to expressed C/EBP isoform lacking transactivation domain resulting in decreased fetuin-A levels [19].
Consistent with previous studies, the current study also found increased levels of the inflammatory markers IL-6 and IL-18 in cases compared with control subjects [4, 5, 20], which is related to the DKD progression. A positive expression of IL-6 in interstitial, mesangial, and tubular infiltrating cells in kidney biopsies of DKD subjects has also been reported [21]. Furthermore, the over-expression of pro-inflammatory markers such as TNF-α, IL-1, and IL-6 in rat models of DKD showed a direct association with kidney damage, and was expressed as urinary-albumin excretion (UAE) [22].
Moreover, NFkB has long been studied as one of the most important transcription factors involved in the synchronization of pro-inflammatory cytokines, cell adhesion molecules, chemokines, and different signaling molecules. It is also involved in the pathological process of DKD [2, 3]. NF-kB is activated in hyperglycemic environments with appropriate stimuli, as well as in severe proteinuric conditions. It is hypothesized that several signaling molecules such as extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38 mitogen-activated protein kinase (MAPK) cascades are closely associated with pro-inflammatory cytokines, adiponectin, and chemokines to frame the network interrelated with the inflammatory process in DKD [23]. Previously, a leading role was reported for the inflammatory molecule IL-18 in DKD progression, than in other diabetic complications [24].
A study by Miyauchi et al. demonstrated the over-expression of IL-18 and its receptor in renal tissue, and showed the upregulation of IL-18 in proximal tubular epithelial cells of the kidney by the activation of MAPK/ERK pathway, and induction of TGF-β1 [25]. Further studies reported that IL-18 over-expression activates the secretion of various pro-inflammatory cytokines by TNF-α and IL-1 beta, as well as the over-expression of ICAM-1 and VCAM-1 by macrophages and endothelial cells. Similarly, studies on human monocytes showed that IL-18 upregulates ICAM-1, while the over-expression of ICAM-1 depended on TNF-α. Additionally, the initiation of ICAM-1 upregulation in human monocytes is suppressed by TNF-α or IL-18 blockage [26, 27]. The present study is consistent with a previous study by Moriwaki et al., where DKD subjects showed elevated levels of IL-18 with raised UAE and TNF-α [28, 29].
In DKD infiltration, the accumulation and activation of macrophages or monocytes in the glomerulus are involved in renal injury. The decreased level of the inflammatory marker MCP-1 in cases is consistent with results of the study by Amann et al., which showed that treatment with angiotensin-converting enzyme inhibitors (ACEIs) reduces MCP-1 levels in subjects with DKD. The mechanism by which ACEIs induce decreased MCP-1 in DKD is not clearly understood [30].
Furthermore, DKD subjects under intensive insulin therapy showed reduction in ICAM-1 and MCP-1 expression [31]. Supporting earlier studies, 81% of the cases in the current study were hypertensive and were receiving ACEIs. In patients with DKD, treatment with insulin and ACEIs leads to a reduction in soluble adhesion molecules via different signaling mechanisms. The present study demonstrates increased levels of adiponectin in cases compared to control subjects; however, the adiponectin levels were not significant confirming a previous study [32]. DKD subjects were under intensive hypertensive therapy (Beta-blockers, ACE inhibitors, angiotensin receptor blockers) and showed reduction in PAI-1 expression [33]. The current study shows increase level of resistin in DKD cases compare to control subjects, contrary to these findings increase resisting levels are associated with decreased glomerular filtration rate and increase in inflammation in chronic kidney disease and suggesting a vital role in the pathogenesis [34].
The current study demonstrated increased levels of adhesion molecules (VCAM-1 and ICAM-1) in cases compared to control subjects which confirms previous studies [6, 7]. It is proposed that increased levels of adhesion molecules may play a possible role in the development of DKD. This evidence revealed interrelationships existing within an inflammatory, cytokine, chemokine, fetuin-A, cell adhesion, and signaling molecules in DKD as shown in Fig. 1. We hypothesize that hyperglycemia results in accumulation of AGEs and endothelial dysfunction, via inflammation. Moreover, an increase in pro-inflammatory cytokines and adhesion molecules in DKD may further increase proteinuria and renal injury in DKD patients.
The present study has several strengths and is the first case–control study investigating baseline pro-inflammatory cytokine, adipokine, and adhesion molecule levels with incident albuminuria. In the present study, we also considered numerous potential confounders such as age, sex, BMI, and diabetes duration. The present study has few limitations. Firstly, biomarkers were measured at one time point of sample collection from each subject. Secondly, we lack information on various drug treatments, dosage and the duration of drug use. Hence, we were unable to see whether various drugs have any effects on biomarkers level. Data presented here demonstrate consistency in terms of metabolic parameters and biomarker measurements, thus providing validity in terms of procedures used in the study. To remove bias, specific assays that were validated earlier were carefully run with lab code by researchers.
This study concludes that serum fetuin-A levels were lower in DKD cases compare to control group. Serum fetuin-A levels are associated with IL-6, IL-18, TNF-α, PAI-1, leptin, resistin and ACR. There is a close relationship among pro-inflammatory molecules, chemokine, adipokines, and fetuin-A in DKD. We hypothesize that an increase in glycemia drives inflammatory mechanisms, which may lead to the development and progression of DKD. This study also provides new insights into the etiology of DKD, in which inflammatory cytokines, adipokines, adhesion molecules, and fetuin-A, are critically involved in the pathogenesis process.
References
International Diabetes Federation (IDF) (2017) http://www.diabetesatlas.org/resources/2017-atlas.html. Accessed 28 Jan 2018
Wada J, Makino H (2013) Inflammation and the pathogenesis of diabetic nephropathy. Clin Sci (Lond) 124:139–152. https://doi.org/10.1042/cs20120198
Navarro-Gonzalez JF, Mora-Fernandez C, Muros de Fuentes M, Garcia-Perez J (2011) Inflammatory molecules and pathways in the pathogenesis of diabetic nephropathy. Nat Rev Nephrol 7:327–340. https://doi.org/10.1038/nrneph.2011.51
Choudhary N, Ahlawat RS (2008) Interleukin-6 and C-reactive protein in pathogenesis of diabetic nephropathy: new evidence linking inflammation, glycemic control, and microalbuminuria. Iran J Kidney Dis 2:72–79
Nakamura A, Shikata K, Hiramatsu M, Nakatou T, Kitamura T, Wada J, Itoshima T, Makino H (2005) Serum interleukin-18 levels are associated with nephropathy and atherosclerosis in Japanese patients with type 2 diabetes. Diabetes Care 28:2890–2895
Clausen P, Jacobsen P, Rossing K, Jensen JS, Parving HH, Feldt-Rasmussen B (2000) Plasma concentrations of VCAM-1 and ICAM-1 are elevated in patients with Type 1 diabetes mellitus with microalbuminuria and overt nephropathy. Diabetes Med 17:644–649
Guler S, Cakir B, Demirbas B, Yonem A, Odabasi E, Onde U, Aykut O, Gursoy G (2002) Plasma soluble intercellular adhesion molecule 1 levels are increased in type 2 diabetic patients with nephropathy. Horm Res 58:67–70. https://doi.org/10.1159/000064664
Binkert C, Demetriou M, Sukhu B, Szweras M, Tenenbaum HC, Dennis JW (1999) Regulation of osteogenesis by fetuin. J Biol Chem 274:28514–28520
Ju H, Zhou Z, Sun M, Ji Y, Zhang J, Chen S, Ji J (2014) Association between serum fetuin A and diabetic nephropathy in patients with type 2 diabetes. Chin J Endocrinol Metab 30(7):592–594
Al-Rubeaan K, Siddiqui K, Alghonaim M, Youssef AM, AlNaqeb D (2018) The Saudi Diabetic Kidney Disease study (Saudi-DKD): clinical characteristics and biochemical parameters. Ann Saudi Med 38:46–56. https://doi.org/10.5144/0256-4947.2018.03.01.1010
American Diabetes Association (2014) Standards of medical care in diabetes—2014. Diabetes Care 37(Suppl 1):S14–S80. https://doi.org/10.2337/dc14-S014
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Caglar K, Yilmaz MI, Saglam M, Cakir E, Kilic S, Sonmez A, Eyileten T, Yenicesu M, Oguz Y, Tasar M, Vural A, Ikizler TA, Stenvinkel P, Lindholm B (2008) Serum fetuin-a concentration and endothelial dysfunction in chronic kidney disease. Nephron Clin Pract 108:c233–40. https://doi.org/10.1159/000120209
Yilmaz MI, Saglam M, Qureshi AR, Carrero JJ, Caglar K, Eyileten T, Sonmez A, Cakir E, Oguz Y, Vural A, Yenicesu M, Stenvinkel P, Lindholm B, Axelsson J (2008) Endothelial dysfunction in type-2 diabetics with early diabetic nephropathy is associated with low circulating adiponectin. Nephrol Dial Transplant 23:1621–1627. https://doi.org/10.1093/ndt/gfm828
Lebreton JP, Joisel F, Raoult JP, Lannuzel B, Rogez JP, Humbert G (1979) Serum concentration of human alpha 2 HS glycoprotein during the inflammatory process: evidence that alpha 2 HS glycoprotein is a negative acute-phase reactant. J Clin Invest 64:1118–1129. https://doi.org/10.1172/jci109551
Cozzolino M, Galassi A, Biondi ML, Turri O, Papagni S, Mongelli N, Civita L, Gallieni M, Brancaccio D (2006) Serum fetuin-A levels link inflammation and cardiovascular calcification in hemodialysis patients. Am J Nephrol 26:423–429
Gangneux C, Daveau M, Hiron M, Derambure C, Papaconstantinou J, Salier JP (2003) The inflammation-induced down-regulation of plasma Fetuin-A (α2HS-Glycoprotein) in liver results from the loss of interaction between long C/EBP isoforms at two neighbouring binding sites. Nucleic Acids Res 31:5957–5970
Wegner M, Araszkiewicz A, Piorunska-Stolzmann M, Wierusz-Wysocka B, Zozulinska-Ziolkiewicz D (2013) Association between IL-6 concentration and diabetes-related variables in DM1 patients with and without microvascular complications. Inflammation 36:723–728. https://doi.org/10.1007/s10753-013-9598-y
Suzuki D, Miyazaki M, Naka R, Koji T, Yagame M, Jinde K, Endoh M, Nomoto Y, Sakai H (1995) In situ hybridization of interleukin 6 in diabetic nephropathy. Diabetes 44:1233–1238
Navarro JF, Milena FJ, Mora C, Leon C, Garcia J (2006) Renal pro-inflammatory cytokine gene expression in diabetic nephropathy: effect of angiotensin-converting enzyme inhibition and pentoxifylline administration. Am J Nephrol 26:562–570. https://doi.org/10.1159/000098004
Wong CK, Ho AW, Tong PC, Yeung CY, Kong AP, Lun SW, Chan JC, Lam CW (2007) Aberrant activation profile of cytokines and mitogen-activated protein kinases in type 2 diabetic patients with nephropathy. Clin Exp Immunol 149:123–131. https://doi.org/10.1111/j.1365-2249.2007.03389.x
Fujita T, Ogihara N, Kamura Y, Satomura A, Fuke Y, Shimizu C, Wada Y, Matsumoto K (2012) Interleukin-18 contributes more closely to the progression of diabetic nephropathy than other diabetic complications. Acta Diabetol 49:111–117. https://doi.org/10.1007/s00592-010-0178-4
Miyauchi K, Takiyama Y, Honjyo J, Tateno M, Haneda M (2009) Upregulated IL-18 expression in type 2 diabetic subjects with nephropathy: TGF-beta1 enhanced IL-18 expression in human renal proximal tubular epithelial cells. Diabetes Res Clin Pract 83:190–199. https://doi.org/10.1016/j.diabres.2008.11.018
Marino E, Cardier JE (2003) Differential effect of IL-18 on endothelial cell apoptosis mediated by TNF-alpha and Fas (CD95). Cytokine 22:142–148
Stuyt RJ, Netea MG, Geijtenbeek TB, Kullberg BJ, Dinarello CA, van der Meer JW (2003) Selective regulation of intercellular adhesion molecule-1 expression by interleukin-18 and interleukin-12 on human monocytes. Immunology 110:329–334
Moriwaki Y, Yamamoto T, Shibutani Y, Aoki E, Tsutsumi Z, Takahashi S, Okamura H, Koga M, Fukuchi M, Hada T (2003) Elevated levels of interleukin-18 and tumor necrosis factor-alpha in serum of patients with type 2 diabetes mellitus: relationship with diabetic nephropathy. Metabolism 52:605–608. https://doi.org/10.1053/meta.2003.50096
Mahmoud RA, el-Ezz SA, Hegazy AS (2004) Increased serum levels of interleukin-18 in patients with diabetic nephropathy. Ital J Biochem 53:73–81
Amann B, Tinzmann R, Angelkort B (2003) ACE inhibitors improve diabetic nephropathy through suppression of renal MCP-1. Diabetes Care 26:2421–2425
Ye SD, Zheng M, Zhao LL, Qian Y, Yao XM, Ren A, Li SM, Jing CY (2009) Intensive insulin therapy decreases urinary MCP-1 and ICAM-1 excretions in incipient diabetic nephropathy. Eur J Clin Invest 39:980–985. https://doi.org/10.1111/j.1365-2362.2009.02203.x
Saito T, Saito O, Kawano T, Tamemoto H, Kusano E, Kawakami M, Ishikawa S-e (2007) Elevation of serum adiponectin and CD146 levels in diabetic nephropathy. Diabetes Res Clin Pract 78:85–92
D’Elia JA, Bayliss G, Gleason RE, Weinrauch LA (2016) Cardiovascular-renal complications and the possible role of plasminogen activator inhibitor: a review. Clin Kidney J 9:705–712
Axelsson J, Bergsten A, Qureshi AR, Heimbürger O, Barany P, Lönnqvist F, Lindholm B, Nordfors L, Alvestrand A, Stenvinkel P (2006) Elevated resistin levels in chronic kidney disease are associated with decreased glomerular filtration rate and inflammation, but not with insulin resistance. Kidney Int 69:596–604
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study has been carried out under compliance of ethical issues. The study was approved by the institutional Review Committee of College of Medicine, King Saud University Riyadh. We used the STROBE case–control checklist for writing our report.
Informed consent
Written informed consent was obtained from each subject.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nawaz, S.S., Joy, S.S., Al Farsi, Y. et al. Potential role of serum fetuin-A in relation with pro-inflammatory, chemokine and adhesion molecules in diabetic kidney disease: a case–control study. Mol Biol Rep 46, 1239–1246 (2019). https://doi.org/10.1007/s11033-019-04592-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-019-04592-2