Abstract
Diagnosis of deep-seated bacterial infection remains a serious medical challenge. The situation is becoming more severe with the increasing prevalence of bacteria that are resistant to multiple antibiotic classes. Early efforts to develop imaging agents for infection, such as technetium-99m (99mTc) labeled leukocytes, were encouraging, but they failed to differentiate between bacterial infection and sterile inflammation. Other diagnostic techniques, such as ultrasonography, magnetic resonance imaging, and computed tomography, also fail to distinguish between bacterial infection and sterile inflammation. In an attempt to bypass these problems, the potent, broad-spectrum antibiotic ciprofloxacin was labeled with 99mTc to image bacterial infection. Initial results were encouraging, but excitement declined when controversial results were reported. Subsequent radiolabeling of ciprofloxacin with 99mTc using tricarbonyl and nitrido core, fluorine and rhenium couldn’t produce robust infection imaging agent and remained in discussion. The issue of developing a robust probe can be approached by reviewing the broad-spectrum activity of ciprofloxacin, labeling strategies, potential for imaging infection, and structure–activity (specificity) relationships. In this review we discuss ways to accelerate efforts to improve the specificity of ciprofloxacin-based imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antibiotic research was highly praised from 1930 to 1970, as this time period was declared to be the golden age of antibiotic development. Indeed, most of the antibiotic classes in current use were developed then. However, the enormous consumption of antibacterial agents has driven the emergence of bacterial resistance to sulfonamides, β-lactams, and macrolides; resistance now limits the efficacy of antibiotics in general. For some indications, bacterial resistance threatens our ability to control infection. A new round of research is occurring to develop novel antibiotics and improve existing agents.
With the quinolone class, a significant advancement occurred in the late 1970s and early 1980s with the addition of a fluorine moiety to the C6 position, thereby producing norfloxacin. Soon after, the N1 ethyl was changed to cyclopropyl, giving rise to ciprofloxacin, a compound with greater activity and a broader spectrum. In subsequent years, a variety of quinolone derivatives have entered the clinical and veterinary markets [1] and it was identified as second largest antibacterial class which share 16.6% global antibacterial drugs market [2].
Ciprofloxacin and other fluoroquinolones share a common mechanism of action that begins with the trapping of gyrase and topoisomerase IV on DNA as a ternary complex. The targets of fluoroquinolones are widely distributed among bacterial species, which allows the fluoroquinolones to have broad-spectrum activity [3]. Ciprofloxacin and other fluoroquinolones are important for controlling infections of lungs, joints, bones, airways, and the urinary tract. Other chronic infections, such as infectious diarrhea, anthrax, and intra-abdominal infections are also being commonly addressed with ciprofloxacin. Broad-spectrum antibacterial potential of ciprofloxacin, later on in 1990s, were considered for bacterial infection imaging by labeling it with 99mTc.
Initial reports indicated that 99mTc labeled ciprofloxacin accumulates specifically at sites of bacterial infection rather than at inflammation lesions [2, 4,5,6,7,8,9], and for a decade (~ 1995–2005) the agent was marketed under the trade name Infecton®. The excitement disappeared when a lack of specificity toward bacterial infection was reported [4, 8, 9].
Recent excitement in the field of infection imaging has emerged from several technical developments. For example, a positron emission tomography/computed tomography (PET/CT) integrated technique is being developed for imaging a broad spectrum of infections, including fever of unknown origin (FUO), spondylitis, discitis or osteitis associated with metallic implants [10, 11]. Other examples include imaging infections caused by Mycobacterium tuberculosis, Staphylococcus aureus, and Escherichia coli using metabolic tracers, such as the glucose analogue, 2-[18F]-fluoro-2-deoxy-d-glucose (FDG) [12, 13], 18F-2-fluorodeoxy sorbitol (18F-FDS) [14, 15], para-mannitol, 6-18F-fluoromaltose, 18F-manitol and p-aminobenzoic acid (PABA) [16], and 99mTc labeled antimicrobial peptides such as 99mTc-Ubiquicidin 29–41 [17]. Nevertheless, work is continuing with 99mTc-fluoroquinolones [18, 19] because the agents are easy to prepare and they have high selectivity and specificity in some situations [20, 21]. Moreover high sensitivity is possible due to the high resolution of integrated SPECT/CT cameras and 99mTc labeling with a wide variety of available fluoroquinolone derivatives. To address the potential of ciprofloxacin, both as an imaging and a therapeutic agent, we discuss the quinolone mechanism of action, labeling strategies with various radionuclides, and infections imaging results both in animals and patients.
Overview of ciprofloxacin synthesis
Since their discovery in the early 1960s [22], the quinolone class of antibiotics has evoked considerable clinical and scientific interest. Nalidixic acid (Fig. 1), the first of the class to be used clinically, was discovered as an impurity during the synthesis of quinine. This agent was found to be bacteriostatic at low concentration and bactericidal at higher concentration [23]. The compound exhibited a narrow spectrum of clinical activity that focused on Gram-negative bacteria.
Structurally, the two rings of nalidixic acid each contain a nitrogen atom, which makes the compound a naphthyridone rather than a quinolone. From this progenitor compound two drug classes emerged, the quinolones and the naphthyridones. These classes were developed by stepwise modification in the basic structure, in many cases using the well-known Gould–Jacobs method [24], to improve efficiency and reduce cost [25, 26].
Ciprofloxacin, a member of the third generation quinolones (norfloxacin is a common representative of the second generation), was recognized as having particularly good activity against Gram-negative bacteria [27]. Although few of the fluoroquinolone substituents can be assigned unique functions, several dominant features have been identified in Fig. 2.
Clinical properties
Ciprofloxacin, launched into clinical practice in 1987, is listed as an essential medicine by the World Health Organization (WHO). Since its introduction to clinical practice, more than 250 million patients have been treated along with enormous research investigation—as reflected in more than 32,000 publications [28]. Ciprofloxacin is administrated both through intravenous and oral routes. Pharmacokinetic studies indicate that drug absorption from the gastrointestinal tract provides 70–85% bioavailability, reaches a peak plasma concentration within an hour [29,30,31,32,33,34,35], and shows low plasma protein binding (25–30%) [31]. The pharmacokinetic characteristics are rapid and effective distribution within patients, and significant concentration in infected tissues, which can exceed serum levels by several fold [31, 36]. Metabolic studies reveal that about 10% of the absorbed dose metabolizes via conjugation in the liver, while 30–50% is excreted unaltered via urine (when administered intravenously, the excreted value increases to > 57% and peak plasma concentration is reached within one minute [29]). Neutrophils may play a role in the distribution of ciprofloxacin by up-taking and releasing it at infection sites, thereby contributing to the therapeutic value of ciprofloxacin (some other antimicrobial agents, such as β-lactams, do not penetrate into neutrophils [36]).
Ciprofloxacin reaches infectious tissues directly through body fluids (Fig. 3a) or encapsulation by neutrophils (Fig. 3b). The later moieties phagocytose foreign particles and microorganisms (Fig. 3c) to deactivate or eradicate by killing [37]. However, some microorganisms resist to phagocytosis-mediated killing and damage neutrophils (Fig. 3e). That releases the fluoroquinolone into the intracellular matrix where the bactericidal agent (the second-line of defense) encounters the pathogen. The damaged neutrophils are then released into blood (Fig. 3f), recognized by the liver, and expelled as non-functional moieties. This release of damaged neutrophils is the basis of a biochemical test for infection. Ciprofloxacin-loaded neutrophils work efficiently to kill bacteria, and the dead-cell debris is expelled through an exocytosis process (Fig. 3d) [38].
Mechanism of action of ciprofloxacin (a) release of ciprofloxacin at infected tissues; (b) release of ciprofloxacin at infected tissues through neutrophil encapsulation; (c) engulfing of bacteria by ciprofloxacin loaded neutrophils; (d) release of dead bacteria by the action of neutrophil and ciprofloxacin loaded neutrophils; (e) release of live bacteria after killing neutrophils; (f) entrance of dead neutrophils into blood that make the bases for biochemically detection of infections through blood test; and (g) showing the binding of ciprofloxacin with bacterial DNA gyrase [39]
Mechanism of action
As with other fluoroquinolones, ciprofloxacin acts by trapping the type II topoisomerases, DNA gyrase and topoisomerase IV, on DNA. These enzymes solve topological problems associated with DNA biology, including chromosome replication [40]. The ternary drug–enzyme–DNA complexes (cleaved complexes) rapidly inhibit DNA synthesis but reversibly complexes (Fig. 3g) [39]. Cell death derives from chromosome breakage, in part from the accumulation of toxic reactive oxygen species [41,42,43,44].
Rationale for the use of technetium-99m-labeled ciprofloxacin
Radiolabeled (Indium-111 (111In) or 99mTc) white blood cell (WBC) imaging is successful for imaging a variety of infections, [45, 46] but, as pointed out above, it cannot be used to distinguish bacterial infection and inflammation [5, 45, 47,48,49]. Radiolabeled monoclonal and polyclonal antibodies were also tested to differentiate between infection and inflammation, but these also tend to localize at sites of inflammation. Moreover, 99mTc-antibodies were not better than tagged leukocytes in terms of specificity for bacterial infections [47]. In contrast, fine-needle aspiration appears to give a definitive diagnosis of infection; however, it is invasive and difficult to apply with critically ill patients [50].
99mTc-labeled ciprofloxacin has been observed to discriminate non-invasively between infection (a microbiological process) and sterile inflammation (a histological event) [51]. Sterile inflammation is a common histological event, which is triggered by physical, chemical or metabolic noxiae (in radiopharmaceutical development studies it is commonly induced using chemicals or heat-killed bacteria) [52]. There are several reasons to distinguish infection from inflammation, the most important of which is to make sure the presence of infection before starting antibiotic therapy which eliminate the chance of unnecessary use of antibacterial agents and consequently the appearance of microbial resistance [53, 54]. In case of deep-seated bacterial infections e.g. intra-abdominal abscesses, osteomyelitis, and endocarditis,most of the imaging methods show conflicting informations, whereas 99mTc-ciprofloxacin diagnose precisely [8]. In vitro experiments and infection induced animal model studies, 99mTc-ciprofloxacin showed promising accumulation at bacterial infection foci while at sterile inflammation only blood pool activity has been reported [2, 55]. The infection imaging specificity of 99mTc-ciprofloxacin in animal models is shown in Table 1 [56,57,58]. Below we review labeling strategies and investigations of imaging in patients that will helpful to conclude imaging specificity and validation of 99mTc-ciprofloxacin.
Methods for radiolabeling ciprofloxacin
With the encouraging development of 99mTc-ciprofloxacin as an imaging agent and the gradually increasing popularity of non-invasive methods of infection diagnosis [66], studies were carried out in variety of animal infection models using a variety of radiolabeling methods. These strategies have been included, labeling with 99mTc (using oxo, carbonyl, or nitrido cores), and fluorine-18/fluorine-19 (18F/19F). In addition, the ciprofloxacin was labeled with rhenium-188 (188Re) to elucidate the 99mTc-ciprofloxacin structural elucidation issue.
Ciprofloxacin labeling with technetium-99m
Labeling using technetium oxo core
Sodium pertechnetate (NaTcO4), eluted from a 99Mo/99mTc generator, is commonly used as a source of 99mTc for labeling ciprofloxacin. As pertechnetate, 99mTc exists in a high oxidation state (i.e. + 7), the principle factor controlling the chemistry of technetium. At this oxidation state, technetium is unable to form coordination complexes with ligands. However, at lower oxidation states, it complexes with variety of ligands. The reduction in oxidation state of 99mTcO4−1 is performed by using an appropriate reducing agent. However, from its discovery in 1943, many reducing agents have been tested for obtaining appropriate oxidation state to complex with ligand molecule. The selection of a suitable reducing agent is based on lack of toxicity, water solubility, and suppression of 99mTc-colloid formation [67]. In the early period of 99mTc radiopharmaceutical development, ferric chloride and ascorbic acid were used to prepare 99mTc-labeled albumin. Subsequently, sodium borohydride, cyanoborohydride, sodium nitrite, sodium amalgam, dithiothreitol, and propionaldehyde were also tested. Most of these agents failed to reduce 99mTcO4−1 to the required oxidation state; consequently, little 99mTc bound (Table 2) [68].
Later, formamidine sulfinic acid (FSA) and stannous(II) chloride di-hydrate (SnCl2·2H2O) showed promising reducing action during labeling of nicotinic acid. The development of 99mTc-ciprofloxacin, initially in 1993, was carried out using FSA as a reducing agent and it was favored due to its high reducing power, high radiochemical yield, and low free and hydrolyzed 99mTc. However, SnCl2·2H2O remained in use for the development of new tracer agents. In the same period, stannous(II) tartrate was reported to be a potentially useful reducing agent. In subsequent studies, a variety of other tin salts, such as stannous fluoride, stannous oxalate, and stannous phosphate, were tested [2] – out of these, however, SnCl2·2H2O and stannous tartrate were used frequently for the development of 99mTc-labeled radiopharmaceuticals. Both reducing agents showed excellent properties in terms of ease of preparation, high radiochemical purity, and biological stability of 99mTc-labeled compounds. Below we describe examples of infection imaging using FSA, SnCl2·2H2O, and stannous tartrate as reducing agents for preparing 99mTc-ciprofloxacin.
Labeling using FSA
In 1993, FSA became a prominent reducing agent for 99mTc-labeling of ciprofloxacin. Using FSA reducing agent, the labeling process required heating at 100 °C for 10 min. However, the agent showed incomplete reduction of 99m TcO4−1 which leave enough free 99mTcO4−1 that need an extra purification step (Sephadex chromatography) to obtain maximal radiochemical yield [2, 69]. The resulted radiochemical showed a specificity 71% in abdominal infection, 91% in skeletal infection, and 100% with infective endocarditis imaging [2]. In other studies, slightly different procedures were opted e.g. heating procedure, pH changes, and reducing agent concentration, to obtain a satisfactory radiochemical yield (~ 90%) without extra purification step and imaging specificity [63].
Labeling using SnCl2·2H2O
This reducing agent is a widely accepted agent for routine radio-synthesis of 99mTc-labeled compounds. It was preferred over FSA for a single-vial 99mTc-ciprofloxacin cold kit under mild reaction conditions, i.e. incubation of labeling mixture for 10 min at room temperature, thereby producing a promising radio-synthesis yield and shelf-life. 99mTc-ciprofloxacin prepared using SnCl2·2H2O showed encouraging infection imaging results. For example, in a murine infection model, 99mTc-ciprofloxacin clearly accumulated in infected tissues [70]; in a 16-patient scintigraphy study, one patient showed a false negative result while 15 showed true positive results. The work showed 88% sensitivity and 85% specificity for hip infection, while for knee infection the two parameters were 100 and 50%, respectively [2, 8, 58, 71, 72]. While labeling antibiotics of other classes, SnCl2·2H2O was also remained a first order choice [73,74,75,76,77,78,79].
Labeling using stannous tartrate
Stannous tartrate was frequently reported in clinical studies of 99mTc-ciprofloxacin soon after the development of 99mTc-ciprofloxacin. FSA was replaced with stannous salts due to multiple serious disadvantages (Table 3) [80]. In other studies, more than 1500 patients were examined using 99mTc-ciprofloxacin in which TcO4−1 was reduced using stannous tartrate; the overall sensitivity was 85.4% and specificity was 81.7% for detecting infective foci [58]. The chemistry of 99mTc reduction by the two stannous salts is similar, with the main difference being the production and elimination of counter ions. Tartrate and chloride ions are removed in different ways; tartrate is an organic moiety and offers no serious interference. However, with both reducing agents Sn(II) gets oxidized from [Sn(II) to Sn(IV)] during exposure to oxygen. That oxidation results in a decrease in Sn(II) ion concentration and therefore poor reduction of TcO4−1, loss of radiochemical yield, and low target specificity. A post-reduction step was introduced to fix this problem and obtain maximal reduction benefits [9, 81,82,83,84,85].
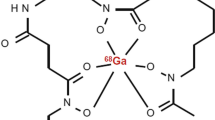
Labeling using technetium carbonyl core
To improve the infection imaging specificity, other 99mTc-labeling strategies were also introduced. One, was the use of 99mTc-tricarbonyl core [86], which does not require prior conventional 99mTcO4-reduction, labeling with fluorine-18, and labeling with galium-67 [18, 87, 88]. In recent years, many studies have been carried out to evaluate 99mTc-tricarbonyl-ciprofloxacin radiopharmaceuticals in vitro and in vivo [64]. For example, Halder et al. conducted a competitive study between 99mTc(CO)3-ciprofloxacin, 99mTc(CO)3-nitrofuryl thiosemicarbazide (NFT) and 99mTc(V)-ciprofloxacin. The mean ratios of uptake in infected/non-infected thighs were 3.87, 3.41 and 3.17, respectively. The advantages of the fac-[99mTc(OH2)3(CO)3]+ in labeling are ease of synthesis, the availability of three labile aqua groups, which ensure complex formation according to the number of electron donor moieties, small size, and inertness [64, 89, 90].
Labeling using technetium nitrido core
The [Tc≡N]2+ core, typically isoelectronic with [Tc=O]3+, exhibits a very high chemical stability toward basic 99mTc labeling reaction conditions such as oxidation–reduction reactions and pH variations. The labeling with technetium nitride core plays critical role in alteration of the biological behavior of a radiopharmaceutical as has been extensively investigated both in sterile and pyrogen free conditions [91]. Ciprofloxacin was labeled with 99mTc using [Tc≡N]2+ core with high yield and good accumulation potential at infection foci with 1.78 infected muscle-to-normal muscle ratio [65]. Thus technetium nitrido core also opens a new avenue for the exploration of infection imaging behavior of ciprofloxacin.
18F-labeled ciprofloxacin
Due to its promising sensitivity and specificity for bacterial infection, ciprofloxacin was labeled with the positron emitting radionuclide fluorine-18 as a positron-emission-tomographic (PET) agent for studies of drug pharmacokinetics and biodistribution in human tissues [28, 66]. Consequently, addition of 18F expanded the imaging and diagnostic potential of radiolabeled ciprofloxacin. Furthermore, 18F-ciprofloxacin can easily be prepared in two steps by a nucleophile substitution reaction, because ciprofloxacin contains a single exchangeable fluorine atom. This labeling is more difficult with trovafloxacin, fleroxacin, and lomefloxacin, which have also been labeled with F-18, because they contain two exchangeable fluorine atoms [92,93,94].
Ciprofloxacin labeling using rhenium
The structure of 99mTc-ciprofloxacin is still unknown; consequently, the 99mTc-ciprofloxacin structure was examined by labeling ciprofloxacin with rhenium (Re) to correlate the lack of infection imaging specificity of 99mTc-ciprofloxacin with structural information. Re is chemically similar to 99mTc, and complexing with ciprofloxacin was carried out to obtain 99mTc-ciprofloxacin structural information [95]. The study showed that ciprofloxacin forms a bi-dentate coordination with 99mTc, one interaction through the carboxyl oxygen atom and the other through the exocyclic carbonyl oxygen atom, as shown in Fig. 4.
99mTc-ciprofloxacin infection imaging
One clinical challenge has been to identify the cause of FUO. It has been thought that 20–30% might be due to infection. Although 67Ga-citrate, 99mTc-methylene diphosphonate (99mTc-MDP), 111In-oxine- and 99mTc-hexamethylpropyleneamine oxime (HMPAO)-labeled autologous leukocytes and 99mTc-labeled leukocyte are useful infection imaging agents, considerable effort has been carried out to determine whether 99mTc-ciprofloxacin can replace leukocyte-based imaging. In an early investigation, 56 patients were examined for possible infection of skin and soft tissue, respiratory tract, abdomen, and skeleton. Out of 56 cases, 39 were found to be in concordance with results found with radiolabeled leukocytes, while 18 cases were not. Out of these 18 patients 9 were clinically documented to have infections; 8 showed a positive 99mTc-ciprofloxacin image, while 9 showed a negative 99mTc-leukocyte image. The other 9 also showed a positive 99mTc-ciprofloxacin image. This early, direct comparative study between 99mTc-ciprofloxacin and 99mTc-leukocyte revealed sensitivity, specificity, and accuracy of ciprofloxacin as 84, 96 and 90%, respectively, while leukocytes showed 81, 77 and 79%, respectively [5]. In a subsequent study involving 99 patients, 56 were tested with 99mTc-leukocytes, and some were given with antibiotic therapy for 5–14 days. The latter were expected to give true-negative results. For imaging with 99mTc-ciprofloxacin, the results were 83% sensitivity and 91% specificity [2]. In another study, aimed to determine the sensitivity and specificity of 99mTc-ciprofloxacin, 90 patients were administrated with 300–400 MBq 99mTc-ciprofloxacin. Whole-body images were taken at 1 and 4 h post injection. The results showed the infection-imaging sensitivity of 70.3% and specificity of 93.1% [56]. The claim regarding the specificity for viable bacterial infection was further tested in three patients with axial skeleton infection; 99mTc-labeled leukocytes failed to show a hot spot at the infection site, while in all three patients 99mTc-ciprofloxacin revealed a hot spot [57]. The usefulness of 99mTc-ciprofloxacin was further tested in 51 patients with suspected bone or joint infection. 99mTc-ciprofloxacin identified 30 as having infections. Four false positive, 20 true negative, and 2 false negative results were obtained, which indicated sensitivity, specificity, and accuracy of 94, 83 and 89%. In contrast, labeled leukocytes showed values of 63, 96 and 77%, respectively. In same study 5 out of 6 hot spots of vertebral osteomyelitis infection were detected with 99mTc-ciprofloxacin, while with tagged-leukocytes 4 hot spots were seen with lower radioactive signal [47]. In the same year (2001), Yapra et al. compared 99mTc-ciprofloxacin with Ga-67 scintigraphy in 22 orthopedic infection patients—sensitivity, specificity, and accuracy were found 85, 92 and 88% for 99mTc-ciprofloxacin while for gallium-67 the values were 78, 100 and 90%, respectively. Although in this study specificity for 99mTc-ciprofloxacin was 8% lower than for Ga-67, the former was seen as an attractive agent due to ease preparation, short investigation time and body compatible biodistribution [7].
Enthusiasm for developing Infecton® as an infection-imaging agent was halted when Sarda et al., reported non-specific behavior in detecting prosthetic joint infection in a rabbit model. In this work, involving 6 prosthetic joint-infected rabbits, 3 of 5 rabbits showed uptake on day 5, and all 5 on days 12 to 19; however, one did not show a response to 99mTc-ciprofloxacin. The mean infected knee to non-infected knee uptake ratio was 1.8 ± 0.4 [96].
The validity in bacterial infection imaging of 99mTc-ciprofloxacin was further tested using 879 patients from a variety of countries (Argentina, Chile, Egypt, Greece, India, Indonesia, Singapore, and UK) having suspected bacterial infections, such as osteomyelitis, orthopaedic prosthesis, tuberculosis, soft tissue, abdominal, surgical wound, septic arthritis, endocarditis, primary bloodstream, ear, nose, and throat, genitourinary, lower respiratory, enteric, and intracranial (for data see Table 4).
It is obvious from the table that Infecton® showed specificity 91.6, 100 and 100%, for orthropaedic prosthesis, surgical wound and endocarditis infections, respectively and specificity for other infections remained between 72 and 77%. However, the overall sensitivity and specificity were 85.4 and 81.7, respectively. But in subsequent reports, the good sensitivity and specificity was sometimes supported and sometimes challenged. For example, when Larikka et al. studied 16 patients using 99mTc-ciprofloxacin, sensitivity was 85% and specificity was 78%; Malamitsi et al. studied 45 patients with suspected bone infection, reporting a sensitivity of 97.2% and specificity of 80% [97]; Sarda et al. reported the results of 37 patients studied in two groups, one having septic artiritis/osteomyelitis (n = 16) and the second (n = 11) having aseptic signs. This work indicated 100% sensitivity, 37.5% specificity and 63% accuracy [8]. Appelboom et al., while studying > 100 patients with arthritis, crystal arthropathy, osteoarthritis, or renal infection, reported that 99mTc-ciprofloxacin is not a specific infection-imaging agent, but it could be used to indicate inflammation within the joints [98].Gemmel et al. reported data for 22 spinal infection patients, including 9 with deep-seated infections—the planar and SPECT scan at 3 h post injection indicated sensitivity, specificity, and accuracy of 78, 69, 73% and 100, 54 and 73%, respectively [99]. De Winter et al. reported similar findings using planar and SPECT imaging of 48 patients to evaluate postoperative spinal infection. This study showed highly specific imaging in patients who had undergone a spinal operation more than 6 months previously [100]. Singh et al. reported a case that indicated better specificity of 99mTc-ciprofloxacin than the bone-seeking agent 99mTc-MDP at the point of a fixed screw following its removal [101].
99mTc-ciprofloxacin also showed good results with tubercular bone infection imaging (n = 14; specificity 71%) [102], cholecystitis (specificity 75%) [81], pelvic inflammatory disease (n = 2, case report) [103], pulmonary tuberculosis (n = 21; specificity 90.9%) [60], osteoarticular tuberculosis (n = 25; 100% positive response) [104] and pediatric osteomyelitis (n = 94; specificity 100%). 99mTc-ciprofloxacin was also implemented in assessing disease activity [105, 106]. Apart from the literature reported on patient study, a variety of infections induced in animal models were also applied (described above) to sort out the spectrum-of-infection-imaging potential and specificity of 99mTc-ciprofloxacin. The results indicated target to non-target ratios ranging from 3.23 ± 0.05 to 5.425 ± 0.17 [60].
Future perspectives
99mTc-ciprofloxacin, over the period of 10 years (1995–2005), showed potential for infection imaging, but in recent reports it is considered to be a controversial tracer agent. The molecular basis of the absence of specificity has not been addressed, nor has the relationship of 99mTc-ciprofloxacin structure to activity. Indeed, preclinical experience with this agent needs to be considered in much more detail to define the mechanism of action, which will be needed to design more specific derivatives, their labeling with 99mTc and detailed screening correspond to infection imaging specificity. One immediate approach is to perform a series labeling and imaging experiments with other existed antibiotics and quinolone derivatives starting from sitafloxacin [88, 107].
References
Takahashi H, Hayakawa I, Akimoto T (2002) The history of the development and changes of quinolone antibacterial agents. Yakushigaku Zasshi 38:161–179
Britton K, Vinjamuri S, Hall A, Solanki K, Siraj Q, Bomanji J, Das S (1997) Clinical evaluation of technetium-99m infecton for the localisation of bacterial infection. Eur J Nucl Med 24:553–556
LeBel M (1988) Ciprofloxacin: chemistry, mechanism of action, resistance, antimicrobial spectrum, pharmacokinetics, clinical trials, and adverse reactions. Pharmacother: J Hum Pharmacol Drug Ther 8:3–30
Palestro CJ, Love C, Miller TT (2007) Diagnostic imaging tests and microbial infections. Cell Microbiol 9:2323–2333
Vinjamuri S, Solanki K, Bomanji J, Siraj Q, Britton K, Hall A, O’Shaughnessy E, Das S (1996) Comparison of 99mTc infecton imaging with radiolabelled white-cell imaging in the evaluation of bacterial infection. Lancet 347:233–235
De Winter F, Van de Wiele C, Dumont F, Van Durme J, Solanki K, Britton K, Slegers G, Dierckx RA, Thierens H (2001) Biodistribution and dosimetry of 99mTc-ciprofloxacin, a promising agent for the diagnosis of bacterial infection. Eur J Nucl Med 28:570–574
Yapar Z, Kibar M, Yapar FA, Toğrul E, Kayaselçuk U, Sarpel Y (2001) The efficacy of technetium-99m ciprofloxacin (Infecton) imaging in suspected orthopaedic infection: a comparison with sequential bone/gallium imaging. Eur J Nucl Med 28:822–830
Sarda L, Crémieux A-C, Lebellec Y, Meulemans A, Lebtahi R, Hayem G, Génin R, Delahaye N, Huten D, Le Guludec D (2003) Inability of 99mTc-ciprofloxacin scintigraphy to discriminate between septic and sterile osteoarticular diseases. J Nucl Med 44:920–926
Siaens RH, Rennen HJ, Boerman OC, Dierckx R, Slegers G (2004) Synthesis and comparison of 99mTc-enrofloxacin and 99mTc-ciprofloxacin. J Nucl Med 45:2088–2094
Tokmak H, Ergonul O, Demirkol O, Cetiner M, Ferhanoglu B (2014) Diagnostic contribution of 18F-FDG-PET/CT in fever of unknown origin. Int J Infect Dis 19:53–58
Haroon A, Zumla A, Bomanji J (2012) Role of fluorine 18 fluorodeoxyglucose positron emission tomography–computed tomography in focal and generalized infectious and inflammatory disorders. Clin Infect Dis 54:1333–1341
Glaudemans AWJM, Signore A (2010) FDG-PET/CT in infections: the imaging method of choice? Eur J Nucl Med Mol Imaging 37:1986–1991. https://doi.org/10.1007/s00259-010-1587-x
Ankrah AO, van der Werf TS, de Vries EFJ, Dierckx RAJO, Sathekge MM, Glaudemans AWJM (2016) PET/CT imaging of Mycobacterium tuberculosis infection. Clin Transl Imaging 4:131–144. https://doi.org/10.1007/s40336-016-0164-0
Yao S, Xing H, Zhu W, Wu Z, Zhang Y, Ma Y, Liu Y, Huo L, Zhu Z, Li Z, Li F (2016) Infection imaging with (18)F-FDS and first-in-human evaluation. Nucl Med Biol 43:206–214. https://doi.org/10.1016/j.nucmedbio.2015.11.008
Weinstein EA, Ordonez AA, DeMarco VP, Murawski AM, Pokkali S, MacDonald EM, Klunk M, Mease RC, Pomper MG, Jain SK (2014) Imaging enterobacteriaceae infection in vivo with (18)F-fluorodeoxysorbitol positron emission tomography. Sci Transl Med 6:259ra146. https://doi.org/10.1126/scitranslmed.3009815
Ordonez AA, Weinstein EA, Bambarger LE, Saini V, Chang YS, DeMarco VP, Klunk MH, Urbanowski ME, Moulton KL, Murawski AM, Pokkali S, Kalinda AS, Jain SK (2017) A systematic approach for developing bacteria-specific imaging tracers. J Nucl Med 58:144–150. https://doi.org/10.2967/jnumed.116.181792
Akhtar M, Qaisar A, Irfanullah J, Iqbal J, Khan B, Jehangir M (2005) Antimicrobial peptide 99mTc-ubiquicidin 29–41 as human infection-imaging agent: clinical trial. J Nucl Med 46:567
Nayak DK, Baishya R, Halder KK, Sen T, Sarkar BR, Ganguly S, Das MK, Debnath MC (2012) Evaluation of 99mTc(i)-tricarbonyl complexes of fluoroquinolones for targeting bacterial infection. Metallomics 4:1197–1208. https://doi.org/10.1039/c2mt20132a
Qadir MA, Wattoo FH, Yaseen M, Atta S, Wattoo MHS, Ahmad SA, Gulzar A (2015) In-vitro binding assay study of 99mTc-flouroquinolones with E. coli, Salmonella and Ps. aeruginosa. Alex J Med 51:47–52
Auletta S, Galli F, Lauri C, Martinelli D, Santino I, Signore A (2016) Imaging bacteria with radiolabelled quinolones, cephalosporins and siderophores for imaging infection: a systematic review. Clin Transl Imaging 4:229–252. https://doi.org/10.1007/s40336-016-0185-8
Naqvi SAR, Drlica K (2017) Fluoroquinolones as imaging agents for bacterial infection. Dalton Trans 46:14452–14460
Reese L (1965) Nalidixic acid (Neggram) in the treatment of urinary infections. Can Med Assoc J 92:394
Mitscher LA (2005) Bacterial topoisomerase inhibitors: quinolone and pyridone antibacterial agents. Chem Rev 105:559–592
Gould RG, Jacobs WA (1939) The synthesis of certain substituted quinolines and 5, 6-benzoquinolines. J Am Chem Soc 61:2890–2895
Pintilie L, Negut C, Oniscu C, Caproiu M, Nechifor M, Iancu L, Ghiciuc C, Ursu R (2009) Synthesis and antibacterial activity of some novel quinolones. Rom Biotechnol Lett 14:4756–4767
Pintilie L, Nita S, Caproiu MT (2010) Synthesis of new 7-chloro-8-substituted-1, 4-dihydro-4-oxo-quinolin-3-carboxylic acids. Synthesis 792:544w
Grohe K, Zeiler H-J, Metzger KG (1987) 7-amino-1-cyclopropyl-4-oxo-1, 4-dihydro-quinoline-and naphthyridine-3-carboxylic acids and antibacterial agents containing these compounds. Google Patents
Brunner M, Langer O, Dobrozemsky G, Müller U, Zeitlinger M, Mitterhauser M, Wadsak W, Dudczak R, Kletter K, Müller M (2004) [18F] Ciprofloxacin, a new positron emission tomography tracer for noninvasive assessment of the tissue distribution and pharmacokinetics of ciprofloxacin in humans. Antimicrob Agents Chemother 48:3850–3857
Turnidge J (1999) Pharmacokinetics and pharmacodynamics of fluoroquinolones. Drugs 58:29–36
Lettieri J, Rogge M, Kaiser L, Echols R, Heller A (1992) Pharmacokinetic profiles of ciprofloxacin after single intravenous and oral doses. Antimicrob Agents Chemother 36:993–996
Davis R, Markham A, Balfour JA (1996) Ciprofloxacin. Drugs 51:1019–1074
Crump B, Wise R, Dent J (1983) Pharmacokinetics and tissue penetration of ciprofloxacin. Antimicrob Agents Chemother 24:784–786
Davis R, Koup JR, Williams-Warren J, Weber A, Smith AL (1985) Pharmacokinetics of three oral formulations of ciprofloxacin. Antimicrob Agents Chemother 28:74–77
Tartaglione T, Raffalovich A, Poynor W, Espinel-Ingroff A, Kerkering T (1986) Pharmacokinetics and tolerance of ciprofloxacin after sequential increasing oral doses. Antimicrob Agents Chemother 29:62–66
Vance-Bryan K, Guay DR, Rotschafer JC (1990) Clinical pharmacokinetics of ciprofloxacin. Clin Pharmacokinet 19:434–461
Walters JD, Zhang F, Nakkula RJ (1999) Mechanisms of fluoroquinolone transport by human neutrophils. Antimicrob Agents Chemother 43:2710–2715
Falkow S, Isberg R, Portnoy D (1992) The interaction of bacteria with mammalian cells. Annu Rev Cell Biol 8:333–363
Frank M, Sullivan G, Carper H, Mandell G (1992) In vitro demonstration of transport and delivery of antibiotics by polymorphonuclear leukocytes. Antimicrob Agents Chemother 36:2584–2588
Mustaev A, Malik M, Zhao X, Kurepina N, Luan G, Oppegard L, Hiasa H, Marks K, Kerns R, Berger J, Drlica K (2014) Fluoroquinolone-gyrase-DNA complexes: two modes of drug binding. J Biol Chem 289:12300–12312
Drlica K, Malik M (2003) Fluoroquinolones: action and resistance. Curr Top Med Chem 3:249–282
Chen C-R, Malik M, Snyder M, Drlica K (1996) DNA gyrase and topoisomerase IV on the bacterial chromosome: quinolone-induced DNA cleavage. J Mol Biol 258:627–637
Malik M, Zhao X, Drlica K (2006) Lethal fragmentation of bacterial chromosomes mediated by DNA gyrase and quinolones. Mol Microbiol 61:810–825
Zhao X, Drlica K (2014) Reactive oxygen species and the bacterial response to lethal stress. Curr Opin Microbiol 21:1–6
Dwyer D, Belenky P, Yang J, MacDonald I, Martell J, Takahashi N, Chan C, Lobritz M, Braff D, Schwarz E, Ye J, Pati M, Vercruysse M, Ralifo P, Allison K, Khalil A, Ting A, Walker G, Collins J (2014) Antibiotics induce redox-related physiological alterations as part of their lethality. Proc Natl Acad Sci USA 111:E2100–E2109
Wang J-H, Sun G-F, Zhang J, Shao C-W, Zuo C-J, Hao J, Zheng J-M, Feng X-Y (2013) Infective severe acute pancreatitis: a comparison of 99mTc-ciprofloxacin scintigraphy and computed tomography. World J Gastroenterol 19:4897
Hovi I, Taavitsainen M, Lantto T, Vorne M, Paul R, Remes K (1993) Technetium-99m-HMPAO-labeled leukocytes and technetium-99m-labeled human polyclonal immunoglobulin G in diagnosis of focal purulent disease. J Nucl Med 34:1428–1434
Sonmezoglu K, Sonmezoglu M, Halac M, Akgün I, Türkmen C, Önsel C, Kanmaz B, Solanki K, Britton KE, Uslu I (2001) Usefulness of 99mTc-ciprofloxacin (infecton) scan in diagnosis of chronic orthopedic infections: comparative study with 99mTc-HMPAO leukocyte scintigraphy. J Nucl Med 42:567–574
Yurt Lambrecht F, Yilmaz O, Unak P, Seyitoglu B, Durkan K, Baskan H (2008) Evaluation of 99mTc-Cefuroxime axetil for imaging of inflammation. J Radioanal Nucl Chem 277:491–494
El-Ghany E, El-Kolaly M, Amine A, El-Sayed A, Abdel-Gelil F (2005) Synthesis of 99mTc-pefloxacin: a new targeting agent for infectious foci. J Radioanal Nucl Chem 266:131–139
Isenmann R, Beger HG (1999) Natural history of acute pancreatitis and the role of infection. Best Pract Res Clin Gastroenterol 13:291–301
Kyprianidou P, Tsoukalas C, Chiotellis A, Papagiannopoulou D, Raptopoulou CP, Terzis A, Pelecanou M, Papadopoulos M, Pirmettis I (2011) First example of well-characterized Re and 99mTc tricarbonyl complexes of ciprofloxacin and norfloxacin in the development of infection-specific imaging agents. Inorg Chim Acta 370:236–242
Petruzzi N, Shanthly N, Thakur M (2009) Recent trends in soft-tissue infection imaging. In: Seminars in nuclear medicine, vol 2. Elsevier, Orlando, FL, pp 115–123. https://doi.org/10.1053/j.semnuclmed.2008.10.005
Babich JW, Fischman AJ (1999) Targeted imaging of infection. Adv Drug Deliv Rev 37:237–252
Laverman P, Bleeker-Rovers CP, Corstens FH, Boerman OC, Oyen WJ (2008) Development of infection and inflammation targeting compounds. Curr Radiopharm 1:42–48
Malamitsi J, Giamarellou H, Kanellakopoulou K, Dounis E, Grecka V, Christakopoulos J, Koratzanis G, Antoniadou A, Panoutsopoulos G, Batsakis C, Proukakis C (2003) Infecton: a 99mTc-ciprofloxacin radiopharmaceutical for the detection of bone infection. Clin Microbiol Infect 9:101–109. https://doi.org/10.1046/j.1469-0691.2003.00506.x
Hall A, Solanki K, Vinjamuri S, Britton K, Das S (1998) Evaluation of the efficacy of 99mTc-Infecton, a novel agent for detecting sites of infection. J Clin Pathol 51:215–219
Amaral H, Morales B, Pruzzo R, Britton KE (1999) Cold–hot mismatch between Tc-99m HMPAO–labeled Leukocytes and Tc-99m ciprofloxacin in axial skeleton infections: a report of three cases. Clin Nucl Med 24:855
Britton K, Wareham D, Das S, Solanki K, Amaral H, Bhatnagar A, Katamihardja A, Malamitsi J, Moustafa H, Soroa V (2002) Imaging bacterial infection with 99mTc-ciprofloxacin (Infecton). J Clin Pathol 55:817–823
Doroudi A, Erfani M, Kooshki F, Saadati SM, Ahmadi F, Kiasat A, Khodayar MJ, Etessami B, Meghdadi H (2014) Efficacy of 99mTc-Ciprofloxacin and 67 Ga-Citrate scintigraphy to discriminate infection foci induced by Staphylococcus aureus from sterile inflammation induced by Carrageenan in rat. Iran J Nucl Med 23:96–102
Lee M, Yoon M, Hwang KH, Choe W (2010) Tc-99m ciprofloxacin SPECT of pulmonary tuberculosis. Nucl Med Mol Imaging 44:116–122
Mirshojaei SF, Erfani M, Ebrahimi S, Esmaeil S, Talebi MH, Haj Hassan Abbasi F (2010) Freeze-dried cold kit for preparation of 99mTc-ciprofloxacin as an infection imaging agent. Iran J Nucl Med 18(2):45–51
Shahzad S, Qadir MA, Ahmed M (2015) Development of stable freeze dried kits of 99 m Tc-ciprofloxacin for infection imaging. J Chem Soc Pak 37:643
Oh SJ, Ryu J-S, Shin JW, Yoon EJ, Ha H-J, Cheon JH, Lee HK (2002) Synthesis of 99mTc-ciprofloxacin by different methods and its biodistribution. Appl Radiat Isot 57:193–200
Zhang J, Zhang S, Guo H, Wang X (2010) Synthesis and biological evaluation of a novel 99mTc(CO)3 complex of ciprofloxacin dithiocarbamate as a potential agent to target infection. Bioorg Med Chem Lett 20:3781–3784. https://doi.org/10.1016/j.bmcl.2010.04.057
Zhang J, Guo H, Zhang S, Lin Y, Wang X (2008) Synthesis and biodistribution of a novel 99mTcN complex of ciprofloxacin dithiocarbamate as a potential agent for infection imaging. Bioorg Med Chem Lett 18:5168–5170
Langer O, Mitterhauser M, Brunner M, Zeitlinger M, Wadsak W, Mayer BX, Kletter K, Müller M (2003) Synthesis of fluorine-18-labeled ciprofloxacin for PET studies in humans. Nucl Med Biol 30:285–291
Baldas J, Bonnyman J, Pojer P, Williams G (1982) The influence of reducing agents on the composition of 99Tc-complexes: Implications for 99mTc-radiopharmaceutical preparation. Eur J Nucl Med 7:187–189. https://doi.org/10.1007/bf00443930
Fritzberg A, Lyster D, Dolphin D (1977) Evaluation of formamidine sulfinic acid and other reducing agents for use in the preparation of Tc-99m labeled radiopharmaceuticals. J Nucl Med 18:553–557
Solanki K, Bomanji J, Siraj Q, Small M, Britton K (1993) Tc-99m Infecton-a new class of radiopharmaceutical for imaging infection. J Nucl Med 34:119A
Mirshojaei SF, Erfani M, Ebrahimi S, Esmaeil S, Talebi MH, Haj Hassan Abbasi F (2010) Freeze-dried cold kit for preparation of 99mTc-ciprofloxacin as an infection imaging agent. Iran J Nucl Med 18:45–51
Fuster D, Soriano A, Garcia S, Piera C, Suades J, Rodríguez D, Martinez JC, Mensa J, Campos F, Pons F (2011) Usefulness of 99mTc-ciprofloxacin scintigraphy in the diagnosis of prosthetic joint infections. Nucl Med Commun 32:44–51
Bhardwaj N, Bhatnagar A, Singh A (2005) Development and evaluation of a single vial cold kit for infection imaging: Tc-99m ciprofloxacin. World J Nucl Med 4:244–251
İlem-Özdemir D, Aşıkoğlu M, Özkılıç H (2013) Radiolabeling, quality control and kit formulation of a new 99mTc-labeled antibiotic: 99mTc-doxycycline hyclate. J Radioanal Nucl Ch 298:1635–1642
Javed M, Khan IU, Mobeen S, Dar U-K, Hyder SW (2012) Synthesis, characterization and biodistribution of novel amine thiophene 99mTc labeled complex. Pak J Pharm Sci 25:381–387
Naqvi SAR, Ishfaq MM, Khan ZA, Nagra SA, Bukhari IH, Hussain AI, Mahmood N, Shahzad SA, Haque A, Bokhari TH (2012) ^{99m} Tc labeled levofloxacin as an infection imaging agent: a novel method for labeling levofloxacin using cysteine\cdot HCl as co-ligand and in vivo study. Turk J Chem 36:267–277
Chattopadhyay S, Das SS, Chandra S, De K, Mishra M, Sarkar BR, Sinha S, Ganguly S (2010) Synthesis and evaluation of 99mTc-moxifloxacin, a potential infection specific imaging agent. Appl Radiant Isot 68:314–316
Roohi S, Mushtaq A, Malik SA (2005) Synthesis and biodistribution of 99mTc-Vancomycin in a model of bacterial infection. Radiochim Acta 93:415–418
Roohi S, Mushtaq A, Jehangir M, Malik S (2006) Synthesis, quality control and biodistribution of 99mTc-Kanamycin. J Radioanal Nucl Chem 267:561–566
Shah SQ, Khan MR (2013) Synthesis of (99 m)Tc labeled temafloxacin complex and biodistribution in male Wistar rats artificially infected with Streptococci pneumonia. Adv Clin Exp Med 22:319–325
Seung J, Jin S, Joong W, Eun J, Hyun J (2002) Synthesis of 99mTc-ciprofloxacin by different methods and its biodistribution. J Appl Radiat Isot 57:193–200
Choe Y-M, Choe W, Lee K-Y, Ahn S-I, Kim K, Cho YU, Choi SK, Hur Y-S, Kim S-J, Hong K-C (2007) Tc-99m ciprofloxacin imaging in acute cholecystitis. World J Gastroenterol 13:3249
Ryu J-K, Lee S-M, Seong D-W, Suh J-K, Kim S, Choe W, Moon Y, Pai S-H (2003) Tc-99m ciprofloxacin imaging in diagnosis of chronic bacterial prostatitis. Asian J Androl 5:179–184
Dahiya S, Chuttani K, Khar RK, Saluja D, Mishra AK, Chopra M (2009) Synthesis and evaluation of Ciprofloxacin derivatives as diagnostic tools for bacterial infection by Staphylococcus aureus. Metallomics 1:409–417
İlem-Özdemir D, Asikoglu M, Ozkilic H, Yilmaz F, Hosgor-Limoncu M, Ayhan S (2014) 99mTc-Doxycycline hyclate: a new radiolabeled antibiotic for bacterial infection imaging. J Label Compd Radiopharm 57:36–41
Rasheed R, Javed M, Ahmad F, Sohail A, Murad S, Masood M, Rasheed S (2013) Preparation of (99 m)Tc-labelled methotraxate by a direct labeling technique as a potential diagnostic agent for breast cancer and preliminary clinical results. Hell J Nucl Med 16:33–37. https://doi.org/10.1967/s002449910069
Alberto R, Schibli R, Egli A, Schubiger AP, Abram U, Kaden TA (1998) A novel organometallic aqua complex of technetium for the labeling of biomolecules: synthesis of [99mTc (OH2)3 (CO)3]+ from [99mTcO4]-in aqueous solution and its reaction with a bifunctional ligand. J Am Chem Soc 120:7987–7988
Lipowska M, He H, Malveaux E, Xu X, Marzilli LG, Taylor A (2006) First evaluation of a 99mTc-tricarbonyl complex, 99mTc(CO)3 (LAN), as a new renal radiopharmaceutical in humans. J Nucl Med 47:1032–1040
Shah SQ, Khan MR, Ali SM (2011) Radiosynthesis of 99mTc (CO)3-clinafloxacin dithiocarbamate and its biological evaluation as a potential Staphylococcus aureus infection radiotracer. Nucl Med Mol Imaging 45:248–254
Pietzsch H-J, Gupta A, Reisgys M, Drews A, Seifert S, Syhre R, Spies H, Alberto R, Abram U, Schubiger P (2000) Chemical and biological characterization of technetium (I) and rhenium (I) tricarbonyl complexes with dithioether ligands serving as linkers for coupling the Tc(CO)3 and Re(CO)3 moieties to biologically active molecules. Bioconjug Chem 11:414–424
Erfani M, Doroudi A, Hadisi L, Andishmand A, Mirshojaei SF, Shafiei M (2013) 99mTc-tricabonyl labeling of ofloxacin and its biological evaluation in Staphylococcus aureus as an infection imaging agent. J Label Compd Radiopharm 56:627–631
Zhang S, Zhang W, Wang Y, Jin Z, Wang X, Zhang J, Zhang Y (2011) Synthesis and biodistribution of a novel 99mTcN complex of norfloxacin dithiocarbamate as a potential agent for bacterial infection imaging. Bioconjug Chem 22:369–375
Babich JW, Rubin RH, Graham WA, Wilkinson RA, Vincent J, Fischman AJ (1996) 18F-labeling and biodistribution of the novel fluoro-quinolone antimicrobial agent, trovafloxacin (CP 99,219). Nucl Med Biol 23:995–998
Fischman AJ, Babich JW, Alpert NM, Vincent J, Wilkinson RA, Callahan RJ, Correia JA, Rubin RH (1997) Pharmacokinetics of 18F-labeled trovafloxacin in normal and Escherichia coli-infected rats and rabbits studied with positron emission tomography. Clin Microbiol Infect 3:63–72. https://doi.org/10.1111/j.1469-0691.1997.tb00253.x
Tewson T, Yang D, Wong G, Macy D, DeJesus O, Nickles R, Perlman S, Taylor M, Frank P (1996) The synthesis of fluorine-18 lomefloxacin and its preliminary use in human studies. Nucl Med Biol 23:767–772
Lecina J, Cortés MP, Martín MA, Piera C, Llagostera M, Suades J (2010) New rhenium complexes with ciprofloxacin. Nucl Med Biol 37:685
Sarda L, Saleh-Mghir A, Peker C, Meulemans A, Crémieux A-C, Le Guludec D (2002) Evaluation of 99mTc-ciprofloxacin scintigraphy in a rabbit model of Staphylococcus aureus prosthetic joint infection. J Nucl Med 43:239–245
Malamitsi J, Giamarellou H, Kanellakopoulou K, Dounis E, Grecka V, Christakopoulos J, Koratzanis G, Antoniadou A, Panoutsopoulos G, Batsakis C (2003) Infecton: a 99mTc-ciprofloxacin radiopharmaceutical for the detection of bone infection. Clin Microbiol Infect 9:101–109
Appelboom T, Emery P, Tant L, Dumarey N, Schoutens A (2003) Evaluation of technetium-99m-ciprofloxacin (Infecton) for detecting sites of inflammation in arthritis. Rheumatology 42:1179–1182
Daou D, Coaguila C, Benada A, Razzouk M, Haidar M, Colin P, Lebtahi R, Slama M, Le Guludec D (2004) The value of a completely automatic ECG gated blood pool SPECT processing method for the estimation of global systolic left ventricular function. Nucl Med Commun 25:271–276
De Winter F, Gemmel F, Van Laere K, De Winter O, Poffijn B, Dierckx RA, Van de Wiele C (2004) 99mTc-Ciprofloxacin planar and tomographic imaging for the diagnosis of infection in the postoperative spine: experience in 48 patients. Eur J Nucl Med Mol Imaging 31:233–239
Singh B, Mittal BR, Bhattacharya A, Aggarwal A, Nagi ON, Singh AK (2005) Technetium-99m ciprofloxacin imaging in the diagnosis of postsurgical bony infection and evaluation of the response to antibiotic therapy: a case report. J Orthop Surg (Hong Kong) 13:190–194
Sharma R, Tewari KN, Bhatnagar A, Mondal A, Mishra AK, Singh AK, Chopra MK, Rawat H, Kashyap R, Tripathi RP (2007) Tc-99m ciprofloxacin scans for detection of tubercular bone infection. Clin Nucl Med 32:367–370
Im MW, Choe W, Hwang SO, Song ES, Lee WY (2008) Pelvic inflammatory disease with Tc-99 m Ciprofloxacin imaging. J Obstet Gynaecol Res 34:754–758
Bhardwaj V, Agrawal M, Suri T, Sural S, Kashyap R, Dhal A (2011) Evaluation of adequacy of short-course chemotherapy for extraspinal osteoarticular tuberculosis using 99mTc ciprofloxacin scan. Int Orthop 35:1869–1874
Singh B, Prasad V, Bhattacharya A, Singh AK, Bhatnagar A, Mittal BR, Gupta KA (2008) Diagnosis of mandibular osteomyelitis in probable coexisting tumor recurrence: role of Tc-99m ciprofloxacin imaging. Clin Nucl Med 33:525–527
Agrawal M, Bhardwaj V, Tsering W, Sural S, Kashyap R, Dhal A (2012) Use of Technetium99m–ciprofloxacin scan in Pott’s spine to assess the disease activity. Int Orthop 36:271–276
Shah S, Khan A, Khan M (2011) Radiosynthesis and biological evolution of 99mTc(CO)3-sitafloxacin dithiocarbamate complex: a promising Staphylococcus aureus infection tracer. J Radioanal Nucl Chem 288:131–136
Funding
This study was funded by Higher Education Commission (HEC), Islamabad, Pakistan for (No. 5612/Punjab/NRPU/R&D/HEC/2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The article is in compliance with ethical standards.
Informed consent
Informed consent was taken from all co-authors before submission of manuscript.
Rights and permissions
About this article
Cite this article
Naqvi, S.A.R., Roohi, S., Iqbal, A. et al. Ciprofloxacin: from infection therapy to molecular imaging. Mol Biol Rep 45, 1457–1468 (2018). https://doi.org/10.1007/s11033-018-4220-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-018-4220-x