Abstract
Doxorubicin (DOX) is an anticancer drug with cardiotoxic side effects mostly caused by iron homeostasis dysregulation. Mitochondria are involved in iron trafficking and mitochondrial ferritin (FtMt) was shown to provide protection against cellular iron imbalance. Therefore, we hypothesized that FtMt overexpression could limit DOX effects on iron homeostasis. Heart’s homogenates of DOX-treated C57BL/6 mice were analyzed for cytosolic and mitochondrial iron-related proteins’ expression and activity, revealing high cytosolic ferritin and ferritin-bound iron, low transferrin-receptor 1 and a strong hepcidin upregulation. Mitochondrial iron-related proteins (aconitase, succinate-dehydrogenase, frataxin) seemed, however, unaffected, although a partial inactivation of superoxide dismutase 2 was detected. Importantly, the ectopic expression of FtMt in human HeLa cells partially reverted DOX-induced iron imbalance. Our results, while confirming DOX effects on iron homeostasis, demonstrate that DOX affects more cytosolic than mitochondrial iron metabolism both in murine hearts and human HeLa cells and that FtMt overexpression is able to prevent most of these effects in HeLa cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Doxorubicin (DOX) is an effective anthracycline, widely used in the treatment of several cancers. Nevertheless, its use is limited by cardiotoxic side effects. Among the hypotheses advanced to explain DOX cardiotoxicity, the onset of cardiac oxidative stress is the most commonly accepted. This occurs through the formation of reactive oxygen species (ROS) resulting from DOX redox-cycling and DOX direct interaction with free reactive iron [1]. Iron involvement in DOX cardiotoxicity is supported by the evidence that only iron chelators (i.e. dexrazoxane) give cardioprotection, while iron excess potentiates the side effect [2–6]. However, although the overexpression of antioxidant proteins and the administration of antioxidant drugs were shown to reduce DOX cardiotoxicity in mice, human clinical trials did not give encouraging results [2, 7, 8]. Thus, the understanding of the mechanisms by which iron contributes to DOX cardiotoxicity is still of crucial importance and may suggest alternative approaches to limit DOX cardiac side effects.
Iron trafficking is intense in mitochondria, the site of heme and iron sulphur clusters’ (ISCs) synthesis [9]. Importantly, mitochondria constitute up to 50 % of cardiomyocytes’ mass and anthracyclines are known to be able to enter mitochondria and inhibit the respiratory chain [10]. Moreover, cardiac tissue expresses moderate levels of mitochondrial ferritin (FtMt), a protein shown to prevent iron imbalance in cellular models, probably because of its ability in masking free reactive iron and making iron bioavailable for cellular functions. Interestingly, FtMt was also reported to protect HeLa cells against oxidative insults reducing cytosolic and mitochondrial free iron level and ROS formation [11–16].
Therefore in this study we carefully evaluated changes in cytosolic and mitochondrial iron homeostasis in the heart of mice injected with a single dose of DOX and tested the hypothesis that FtMt could rescue these effects by overexpressing the protein in HeLa cells.
Materials and methods
Animals
Male C57BL/6 mice of 8 weeks (Charles River Italia, Calco, Italy) were divided in four experimental groups. Control group (n = 19) received one i.p. saline injection. DOX-treated group (n = 19) received a single i.p. DOX dose (20 mg/kg, Sigma-Aldrich, St. Louis, MO, USA). Sub-chronic iron loading was obtained in the iron-treated group (n = 6) by 15 daily i.p. iron-dextran injections (a total of 20 mg, Sigma-Aldrich). At day 16, mice were injected with saline. The iron plus DOX-treated group (n = 6) received iron as above and, at day 16, a single DOX dose. 4 days after treatments, animals were sacrificed and hearts were collected. Animal care and experimental procedures complied with EU Directive 2010/63/EU.
Cells
HeLa Tet-off cells (Clontech, Mountain View, CA, USA) were cultured in DMEM (Gibco Life Technologies, Paisley, UK) supplemented with 10 % FBS (Gibco Life Technologies), 40 μg/ml gentamicin, 150 μg/ml hygromicin. HeLa cells expressing human FtMt (MT53 cell line) [11] were cultured with tetracycline-free FBS (Clontech) to induce FtMt expression. Cells were treated for 18 h with DOX. Viability was assessed by MTT assay (Sigma-Aldrich) [13]. To assess ferric ammonium-citrate (FAC) or H2O2 sensitivity, after DOX exposure for 18 h cells were treated with FAC for 18 h or with H2O2 without FBS for 2 h prior to MTT assay.
Biochemical methods
Hearts, homogenized on ice, were immediately analyzed for enzyme activities or frozen for further analyses. For mitochondrial enrichment, hearts were homogenized with 220 mM d-mannitol, 70 mM sucrose, 2 mM HEPES pH 7.4 buffer and centrifuged for 1 min at 5,000 g to remove debris. Supernatants were centrifuged for 5 min at 11,000 g to collect cells. Cellular pellets were treated as described [13]. Mitochondria-enriched lysates were immediately analyzed for enzyme activities. HeLa total lysates and mitochondrial enrichment were obtained as previously described [13]. For immunoblot experiments, equal protein amounts, separated by SDS- or native-PAGE, were transferred to PVDF membranes. Filters were incubated with primary and then with peroxidase-labeled secondary antibodies (Dako, Glostrup, Denmark). Bound activity was revealed by chemiluminescence (ECL Advance, GE Healthcare, Uppsala, Sweden). Primary antibodies were: rabbit anti-murine ferritin heavy (FTH) and light (FTL) chains, kindly provided by Sonia Levi, rabbit anti-ferritin (Sigma-Aldrich), mouse anti-transferrin receptor 1 (TfR1) (Zymed, South San Francisco, CA, USA), rabbit anti-superoxide dismutase 2 (SOD2) (Upstate, Billerica, MA, USA), rabbit anti-frataxin, kindly provided by Franco Taroni, rabbit anti-iron regulatory protein (IRP) 1 produced in our laboratory and mouse anti-GAPDH or rabbit anti-voltage-dependent anion channel (VDAC)1/porin used as housekeeping genes (Sigma-Aldrich). For aconitase, succinate dehydrogenase (SDH), citrate synthase (CS) and SOD2 activity evaluations we followed described methods [13, 14]. For ferritin-bound iron estimation, native-PAGE separated proteins were revealed in-gel by the enhanced Perls’ DAB staining. Briefly, gels were treated with 2 % K4Fe(CN)6, 1 % HCl, rinsed with water and stained with 0.5 mg/ml DAB, 0.15 % H2O2 in Tris-buffered saline pH 7.4. Protein concentrations were determined by the BCA method (Pierce, Rockford, IL, USA). Densitometric analyses were performed with Kodak Image Station 440 CF and Kodak 1D 3.6 program (Kodak, Rochester, NY, USA).
RNA
For RNA extraction, hearts were homogenized in TRI-Reagent Solution (Ambion, Austin, TX, USA). cDNA synthesis was obtained with 1 μg of DNase-treated RNA using ImPromII reverse-transcriptase (Promega, Madison, WI, USA). Quantifications were performed by semi-quantitative RT-PCR with Xtra-Taq Pol (Genespin, Milan, Italy) and primers specific for FTH, TfR1 and hepcidin, with HPRT1 used as normalizing gene (Online Resource 1). Densitometric analysis was obtained with Kodak 1D 3.6 program.
Statistical analysis
Statistical analysis was performed using Student’s t test. Differences were defined as significant for p < 0.05.
Results
DOX effects on cardiac iron homeostasis in mice
Doxorubicin (DOX) was shown to alter iron homeostasis in cellular and animal models [17–19]. To assess DOX effects on cardiac iron metabolism in our murine model, we evaluated in heart lysates extracted from DOX-treated mice the expression of the proteins considered as the main indices of cellular iron homeostasis and involved in cellular iron uptake (TfR1) and storage (FTH and FTL). DOX treatment induced a significant increase of FTH and FTL and a decrease of TfR1 levels (Fig. 1a–c, p < 0.01 DOX group vs. control group, and Fig. 1f lanes 1–3 for representative analyses). Interestingly, although RT-PCR analysis did not give suggestions of a significant DOX-induced modulation of cardiac FtMt (not shown), FTH and TfR1 mRNA expression correlated with protein levels (Fig. 1d).
DOX effects on cytosolic and mitochondrial cardiac iron homeostasis in mice. a–c Heart total homogenates were analyzed by western-blot for FTH, FTL and TfR1, with GAPDH used as loading control. d FTH, TfR1 and hepcidin mRNA abundances were determined by RT-PCR and normalized by HPRT1 mRNA amount. e Ferritin-bound iron was determined by native-PAGE/Perls’ DAB staining, with Coomassie-blue staining used as loading control. All reported values were expressed as percentage relative to control group. g Heart total homogenates were analyzed for aconitase (ACO) activity and mitochondria-enriched lysates for SDH and CS activities. Enzymatic activities were expressed as percentage of mU/mg total proteins relative to control group. Aconitase activity was also analyzed in gel as in (i). h SOD2 activity was determined in gel with Coomassie-blue staining used as loading control and expressed as percentage relative to control group. f Heart homogenates were analyzed by western-blot for frataxin and SOD2, with GAPDH and VDAC1/porin used as loading control. Representative analyses of all above reported assays are also shown. i Heart total homogenates from saline (S) or DOX-treated mice, kidney (KT) and liver (LT) total homogenates and kidney mitochondrial fraction (KMF) from saline-treated animals were separated on native-PAGE and aconitase activity was revealed in-gel (c-aco, cytosolic aconitase, m-aco, mitochondrial aconitase). Data are expressed as mean and SD of values for each group (*p < 0.05, **p < 0.01 experimental groups vs. control group, #p < 0.05, ##p < 0.01 iron plus DOX group vs. DOX group, §p < 0.05, §§p < 0.01 iron plus DOX group vs. iron group)
Since DOX cardiotoxicity is potentiated by iron excess [3–6], we also examined the effects of the combined treatment of iron and DOX on iron homeostasis. As expected, cardiac FTH and FTL expression was increased in iron-treated mice, but, interestingly, iron and DOX together induced a greater increase (Fig. 1a, b, f lanes 1–2). Although not significant in immunoblot experiments, the trend toward a greater increase resulted significant when evaluated by a quantitative ELISA (Online Resource 2; p < 0.05 iron plus DOX group vs. iron group). No additional decrease in TfR1 expression was reported after the combined treatment (Fig. 1c and f lane 3).
In cellular models, DOX-induced ferritin upregulation was shown to be accompanied with an increased iron accumulation in this protein [18, 19]. In our mouse model we interestingly confirmed this finding, further showing that ferritin upregulation also reflected in a higher ferritin iron load after the combined treatment (Fig. 1e and f lane 4; p < 0.05 DOX group vs. control group). We then evaluated the mRNA expression of the iron regulatory peptide hepcidin, known to be transcriptionally regulated [20] and expressed in the heart [21]. Using RT-PCR, we found a strong hepcidin mRNA increase in DOX-treated mice compared to untreated controls (Fig. 1d; p < 0.05 DOX group vs. control group). DOX effect on hepcidin transcript was similar to the one obtained after treatment with iron alone or with the combination of iron and the drug (Fig. 1d).
In cellular models, DOX-induced ferritin iron storage was shown to prevent iron release from ferritin, suggesting apparent cellular iron depletion [19]. Mitochondria have a central role in iron metabolism and iron dysregulation is often accompanied with the inactivation of ISC-containing enzymes [9, 13, 14]. Therefore, we measured cardiac aconitase and SDH activities, with CS activity used as control, after the single (DOX or iron alone) or the combined (iron plus DOX) treatments. We found a similar decrease in all enzymes’ activities after iron or iron plus DOX treatments, while DOX alone did not cause any changes in their function (Fig. 1g and f lane 5). To further exclude an effect on ISC biogenesis, we evaluated frataxin expression, a protein involved in mitochondrial iron handling and ISC synthesis [13, 22], finding its expression levels tested by immunoblot to remain unmodified after DOX, iron or iron plus DOX treatments (Fig. 1f lane 6). Although these evidences suggested that just the cytosolic compartment is affected by DOX, we found a slight but significant decrease in the activity of SOD2, a mitochondrial enzyme with antioxidant function (Fig. 1h and f lane 7; p < 0.05 DOX group vs. control group). No changes in protein expression were detected (Fig. 1f lane 8), indicating that the decrease of activity was not caused by a decrease in the enzyme synthesis. Of interest, while the treatment with iron alone resembled the inhibiting effect on SOD2 activity found in DOX-treated mice, the combination of iron and DOX had a synergistic effect on SOD2 inactivation (Fig. 1h, f lane 7; p < 0.01 iron plus DOX group vs. DOX group and p < 0.01 iron plus DOX group vs. iron group).
DOX treatment of HeLa cells and the effects of FtMt expression
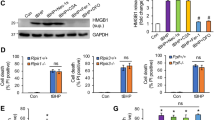
DOX was reported to induce iron imbalance in cultured cells [18, 19]. In our experiments, we used HeLa cells as cellular model, since overexpression of FtMt in these cells (MT53 cell line) was previously shown by our as well as other groups to rescue iron homeostasis dysregulation [13, 14, 16]. To determine whether FtMt overexpression could prevent DOX-induced iron imbalance, we studied the main indices of iron homeostasis after exposure of cells to 5 μM DOX, dose found to be clinically relevant [1]. We report that, although FtMt overexpression was insufficient to contrast cytosolic ferritin upregulation, however, it completely reverted the increase of cytosolic ferritin-bound iron observed in parental HeLa cells after DOX treatment, notably without a significant rise of FtMt iron uptake (Fig. 2a, b, d lanes 1–2 and Online Resource 3). Importantly, TfR1 downregulation induced by DOX in HeLa cells was not observed in MT53 cells (Fig. 2c, d lane 3). These evidences suggest that FtMt expression can partially rescue iron dysregulation caused by DOX in vitro.
DOX effects on HeLa cells and the influence of FtMt overexpression (MT53 cells). Cells were treated for 18 h with 5 μM DOX. Total lysates were analyzed by western-blot for cytosolic ferritin (FT) (a) and TfR1 (c), with GAPDH used as loading control, and by native-PAGE/Perls’ DAB staining for cytosolic (c-FT) bound iron (b), with Coomassie-blue staining used as loading control. Values were expressed as percentage relative to untreated cells. Representative analyses of all above reported assays are shown in (d). e Dose-dependent DOX effects on cell viability. f Dose-dependent DOX and H2O2 effects on cell viability. g DOX and FAC effects on cell viability. In all experiments cell viability was expressed as percentage relative to untreated cells. Data are presented as mean and SD of at least three independent experiments (*p < 0.05, **p < 0.01 treated vs. untreated cells, #p < 0.05, ##p < 0.01 MT53 vs. HeLa treated cells)
To test whether ectopic FtMt expression was also sufficient to protect cells against DOX-induced cytotoxicity, we measured cell viability after DOX exposure and found that MT53 cells were more resistant than control HeLa cells to the drug cytotoxic effect (Fig. 2e). These data clearly indicate that FtMt overexpression protects cells from DOX-induced toxicity in vitro.
FtMt has antioxidant properties and DOX is known to induce oxidative stress [1, 16]. To assess whether FtMt overexpression could protect cells against DOX-induced oxidative damage, we exposed cells to different H2O2 concentrations after treatment with different doses of DOX and then measured cell viability. Our results showed that FtMt expression increased cell resistance to H2O2 also in the presence of high DOX concentrations (Fig. 2f). Of interest, when we measured the activity of the mitochondrial antioxidant enzyme SOD2, we found that while DOX exposure induced a partial inactivation in parental cells, it surprisingly caused a significant increase of activity in FtMt overexpressing cells (Fig. 3a, c lane 1; p < 0.05 MT53 untreated cells vs. MT53 DOX-treated cells and p < 0.01 MT53 DOX-treated cells vs. HeLa DOX-treated cells). Consistently with results obtained in our mouse model, no significant changes in SOD2 protein levels were reported after DOX treatment of HeLa or MT53 cells (Fig. 3c lane 2). These evidences suggest that FtMt may at least in part exploit its antioxidant activity by inducing SOD2 iperactivation.
DOX effects on HeLa cells and the influence of FtMt overexpression (MT53 cells). Cells were treated for 18 h with 5 μM DOX. Total lysates were analyzed for SOD2 activity, expressed as percentage relative to untreated cells (a, c). Aconitase activity was analyzed in total lysates (t-ACO) and in mitochondrial (m-ACO) and post-mitochondrial (c-ACO) fractions, while mitochondrial fractions were analyzed for SDH and CS activities (a). Activities were expressed as percentage of mU/mg total proteins relative to untreated cells. b, c Total lysates were analyzed by western-blot for c-ACO/IRP1, SOD2 and frataxin, with GAPDH used as loading control. Protein abundance was expressed as percentage relative to untreated cells. Data are presented as mean and SD of at least three independent experiments (*p < 0.05, **p < 0.01 treated vs. untreated cells, #p < 0.05, ##p < 0.01 MT53 vs. HeLa treated cells)
To test the potential protective effect of FtMt in the presence of iron excess, we exposed cells to FAC alone or after DOX treatment and evaluated the effect of the single or the combined treatment on cell viability. While HeLa cells were slightly affected by FAC, the combination of FAC and DOX significantly decreased their viability. Conversely, FtMt overexpressing cells were found to be protected against either FAC used alone or in combination with DOX, indicating once again a protective role of FtMt in condition of cellular iron imbalance (Fig. 2g).
While cardiac aconitase is mostly in the mitochondria (Fig. 1i), cytosolic and mitochondrial aconitases are similarly expressed in HeLa cells [14]. Enzyme activity was reduced after DOX exposure both in HeLa and MT53 cells. However, only cytosolic activity was affected (Fig. 3a). Interestingly, when we analyzed cytosolic aconitase/IRP1 protein level by immunoblot, we found its expression decreased only in control cells (Fig. 3b, c lane 3). Finally, consistent with data obtained in our mouse model, SDH activity and frataxin expression were unmodified by DOX treatment both in HeLa and MT53 cells (Fig. 3a, with CS activity used as control, and 3c lane 4), ruling out once again a direct effect of DOX on mitochondrial iron handling.
Discussion
The first major finding of our study was that, although DOX had an evident effect on murine cardiac iron homeostasis, the dysregulation was mainly detectable in the cytosol while barely in mitochondria. DOX induced cardiac hepcidin mRNA, increased cytosolic ferritin, its iron load and downregulated TfR1 protein expression levels. Surprisingly, although mitochondrial iron-related proteins are known to be extremely sensitive to iron homeostasis dysregulation [9, 13], nevertheless a partial inactivation of the antioxidant enzyme SOD2 by DOX exposure was the only effect reported. Importantly, we confirmed these findings in HeLa cells, further showing a decrease in the expression and enzymatic activity of cytosolic aconitase/IRP1. Finally, we demonstrated that the ectopic expression of the mitochondrial protein FtMt in HeLa cells significantly attenuated most DOX effects, preserving TfR1 expression and ferritin iron load and preventing cytosolic aconitase/IRP1 protein decrease and SOD2 inactivation. Moreover, FtMt overexpression counteracted DOX and DOX plus iron citotoxicity and reduced H2O2 cell sensitivity after DOX treatment.
Iron is an essential cellular element as it serves as a cofactor for several proteins involved in important biological processes. However, free iron excess can produce tissue damage due to the generation of ROS. Cardiac damage mediated by ROS is one of the most thoroughly studied mechanisms proposed to explain DOX cardiotoxicity. Cardiac oxidative stress may be promoted by DOX through its redox-cycling, that results in the formation of superoxide free radicals. The increase of cellular free reactive iron induced by DOX can in turn result in the acceleration of the Haber–Weiss reaction, with the production of dangerous hydroxyl radicals. Alternatively, DOX can promote oxidative stress through its direct interaction with iron [1, 2].
Several studies however indicate a DOX direct effect on cardiac iron homeostasis [2, 17–19]. Consistent with this hypothesis, our in vivo results showed a significant DOX-induced ferritin upregulation and TfR1 downregulation, supporting previous evidences suggesting a post-transcriptional control of iron regulatory protein 2 (IRP2) through its downmodulation [17], mechanism possibly meant to counteract the rise of free reactive cellular iron pool. Alternatively, ferritin mRNA increase could be explained as an attempt to limit ROS generation and consequent oxidative stress [23]. We reported a strong cardiac hepcidin upregulation induced by DOX. Although mainly produced by hepatocytes and macrophages, the iron regulator hepcidin is expressed in the heart [20], where it was indicated to act as an autocrine/paracrine hormone. Cardiac hepcidin upregulation was suggested to upregulate cardiac ferritin as a protective mechanism against ROS [21]. Therefore, we can speculate that hepcidin upregulation in the heart of DOX-treated mice could be an attempt to reduce ROS levels through ferritin induction.
In cellular models ferritin increase is accompanied by its iron load [18, 19]. Consistently, we confirmed this drug effect in the heart’s lysates of DOX-treated mice. Since mitochondria are a main iron trafficking site, we focused our attention on mitochondrial iron-related proteins. The ISC-synthesis pathway and possibly other iron-related pathways were, however, unaffected by DOX, since we did not observe mitochondrial ISC-containing enzymes’ inactivation or modulation of frataxin, considered the iron chaperone in ISC assembly, heme synthesis and mitochondrial aconitase activity regulation and modulated by iron cellular status [22]. A limited mitochondrial iron imbalance cannot, however, be excluded, since we observed the inactivation of SOD2, an anti-oxidant mitochondrial enzyme, whose activity was found to be related to mitochondrial iron bioavailability [13, 14].
When mice were treated with the combination of iron plus DOX, we observed a greater cytosolic ferritin upregulation and a trend towards a higher ferritin iron uptake compared to iron alone treatment, suggesting an enhanced inhibition of iron mobilization with possible influence on mitochondria. Nonetheless, while iron alone partially inactivated aconitase and SDH, the ISC-synthesis pathway and frataxin synthesis seemed again unimpaired by DOX even with iron load. Although mitochondrial iron-related functions were mainly preserved, however, DOX-induced SOD2 inactivation was enhanced by iron excess.
FtMt was shown to prevent iron dysregulation in cellular models [13–16]. We demonstrated that DOX cytotoxicity in HeLa cells was reduced by FtMt expression, strongly suggesting an iron role in DOX effects. Consistent with our in vivo studies as well as with observations in other cells [18, 19], DOX affected HeLa cytosolic iron homeostasis. Nevertheless, although FtMt overexpression did not counteract ferritin upregulation, it was sufficient to prevent cytosolic or mitochondrial ferritin iron overload and TfR1 downregulation, suggesting that FtMt could maintain cellular iron bioavailability. This hypothesis is supported by the observation that, while DOX inactivated SOD2 in HeLa cells, FtMt expression rescued this deficiency, possibly also protecting cells from DOX-induced oxidative stress. Consistent with our in vivo data, mitochondrial iron homeostasis involvement in DOX-treated HeLa cells was limited to SOD2 inactivation. However, DOX reduced enzymatic activity of cytosolic aconitase both in HeLa and MT53 cells, possibly as a consequence of the release of iron from the ISC, due to the redox cycling of the drug [1] or alternatively to the suggested apparent DOX-induced cytosolic iron starvation [19]. In both cases, the release of iron from the cluster would modulate the expression of ferritin and TfR1, converting the cytosolic enzyme into an iron regulatory protein (IRP1). Increased IRP1 RNA-binding activity would then downregulate ferritin and upregulate TfR1 [24]. However, DOX led exactly to the opposite effect, suggesting that the enzyme inactivation could instead arise from its conversion into a null-protein, lacking of both aconitase and RNA-binding activities [1, 19]. In this condition, cells could be unable to properly sense cellular iron level and adapt response to cellular iron status changes. IRP1 null-protein has been shown to be susceptible to degradation by the ubiquitin–proteasome pathway as an iron dependent mechanism to control accumulation of IRP1 RNA binding activity [24, 25]. Consistently, we found a DOX-induced IRP1 decrease in HeLa cells, while its expression was preserved in MT53 cells. It is tempting to speculate that DOX could induce IRP1 degradation with consequent RNA-binding activity decrease, ferritin upregulation and TfR1 downregulation. FtMt expression may prevent IRP1 degradation, therefore at least partially preserving cellular iron sensing.
It has been previously shown that FtMt gives protection against H2O2 exposure in HeLa cells [16]. While confirming this finding, we further indicated that FtMt increased HeLa resistance to H2O2 even in the presence of DOX. This effect could be explained with the SOD2 iperactivation observed in MT53 cells or alternatively with a more controlled iron handling in the presence of FtMt, which could in turn influence SOD2 activity [13].
Finally, we showed that, while DOX cytotoxic effect was exacerbated by FAC in HeLa cells, FtMt overexpression preserved cells from DOX plus iron cytotoxicity, likely due to its ability to control cellular iron handling.
In conclusion, our results in mice confirmed DOX effects on cytosolic iron homeostasis, further revealing cardiac ferritin iron overload and hepcidin upregulation and demonstrated for the first time that mitochondrial iron homeostasis is, however, poorly involved, although the established central role of mitochondria in iron metabolism regulation. Our observations in HeLa cells, consistent with the in vivo data, confirmed that cytosolic iron homeostasis is the main target of DOX. Interestingly, the overexpression of the mitochondrial protein FtMt seemed sufficient to limit these effects, possibly making cellular iron bioavailable for essential functions. Our results could have important clinical implications, suggesting the modulation of the cardiac FtMt or alternatively of the cardiac hepcidin as potential therapeutic tools to avoid DOX cardiotoxicity.
References
Minotti G, Menna P, Salvatorelli E, Cairo G, Gianni L (2004) Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol Rev 56:185–229
Simůnek T, Stérba M, Popelová O, Adamcová M, Hrdina R, Gersl V (2009) Anthracycline-induced cardiotoxicity: overview of studies examining the roles of oxidative stress and free cellular iron. Pharmacol Rep 61:154–171
Hershko C, Link G, Tzahor M, Kaltwasser JP, Athias P, Grynberg A, Pinson A (1993) Anthracycline toxicity is potentiated by iron and inhibited by deferoxamine: studies in rat heart cells in culture. J Lab Clin Med 122:245–251
Panjrath GS, Patel V, Valdiviezo CI, Narula N, Narula J, Jain D (2007) Potentiation of doxorubicin cardiotoxicity by iron loading in a rodent model. J Am Coll Cardiol 49:2457–2464
Miranda CJ, Makui H, Soares RJ, Bilodeau M, Mui J, Vali H, Bertrand R, Andrews NC, Santos MM (2003) Hfe deficiency increases susceptibility to cardiotoxicity and exacerbates changes in iron metabolism induced by doxorubicin. Blood 102:2574–2580
Cascales A, Sánchez-Vega B, Navarro N, Pastor-Quirante F, Corral J, Vicente V, de la Peña FA (2012) Clinical and genetic determinants of anthracycline-induced cardiac iron accumulation. Int J Cardiol 154:282–286
Kang YJ, Chen Y, Epstein PN (1996) Suppression of doxorubicin cardiotoxicity by overexpression of catalase in the heart of transgenic mice. J Biol Chem 271:12610–12616
Yen HC, Oberley TD, Vichitbandha S, Ho YS, St Clair DK (1996) The protective role of manganese superoxide dismutase against adriamycin-induced acute cardiac toxicity in transgenic mice. J Clin Invest 98:1253–1260
Richardson DR, Lane DJ, Becker EM, Huang ML, Whitnall M, Rahmanto YS, Sheftel AD, Ponka P (2010) Mitochondrial iron trafficking and the integration of iron metabolism between the mitochondrion and cytosol. Proc Natl Acad Sci USA 107:10775–10782
Goormaghtigh E, Huart P, Praet M, Brasseur R, Ruysschaert JM (1990) Structure of the adriamycin-cardiolipin complex. Role in mitochondrial toxicity. Biophys Chem 35:247–257
Corsi B, Cozzi A, Arosio P, Drysdale J, Santambrogio P, Campanella A, Biasiotto G, Albertini A, Levi S (2002) Human mitochondrial ferritin expressed in HeLa cells incorporates iron and affects cellular iron metabolism. J Biol Chem 277:22430–22437
Santambrogio P, Biasiotto G, Sancito F, Olivieri S, Arosio P, Levi S (2007) Mitochondrial ferritin expression in adult mouse tissues. J Histochem Cytochem 55:1129–1137
Zanella I, Derosas M, Corrado M, Cocco E, Cavadini P, Biasiotto G, Poli M, Verardi R, Arosio P (2008) The effects of frataxin silencing in HeLa cells are rescued by the expression of human mitochondrial ferritin. Biochim Biophys Acta 1782:90–98
Cavadini P, Biasiotto G, Poli M, Levi S, Verardi R, Zanella I, Derosas M, Ingrassia R, Corrado M, Arosio P (2007) RNA silencing of the mitochondrial ABCB7 transporter in HeLa cells causes an iron-deficient phenotype with mitochondrial iron overload. Blood 109:3552–3559
Shi ZH, Nie G, Duan XL, Rouault T, Wu WS, Ning B, Zhang N, Chang YZ, Zhao BL (2010) Neuroprotective mechanism of mitochondrial ferritin on 6-hydroxydopamine-induced dopaminergic cell damage: implication for neuroprotection in Parkinson’s disease. Antioxid Redox Signal 13:783–796
Campanella A, Rovelli E, Santambrogio P, Cozzi A, Taroni F, Levi S (2009) Mitochondrial ferritin limits oxidative damage regulating mitochondrial iron availability: hypothesis for a protective role in Friedreich ataxia. Hum Mol Genet 18:1–11
Corna G, Galy B, Hentze MW, Cairo G (2006) IRP1-independent alterations of cardiac iron metabolism in doxorubicin-treated mice. J Mol Med 84:551–560
Corna G, Santambrogio P, Minotti G, Cairo G (2004) Doxorubicin paradoxically protects cardiomyocytes against iron-mediated toxicity: role of reactive oxygen species and ferritin. J Biol Chem 279:13738–13745
Xu X, Persson HL, Richardson DR (2005) Molecular pharmacology of the interaction of anthracyclines with iron. Mol Pharmacol 68:261–271
Ganz T (2011) Hepcidin and iron regulation, 10 years later. Blood 117:4425–4433
Merle U, Fein E, Gehrke SG, Stremmel W, Kulaksiz H (2007) The iron regulatory peptide hepcidin is expressed in the heart and regulated by hypoxia and inflammation. Endocrinology 148:2663–2668
Li K, Besse EK, Ha D, Kovtunovych G, Rouault TA (2008) Iron-dependent regulation of frataxin expression: implications for treatment of Friedreich ataxia. Hum Mol Genet 17:2265–2273
Torti FM, Torti SV (2002) Regulation of ferritin genes and protein. Blood 99:3505–3516
Anderson CP, Shen M, Eisenstein RS, Leibold EA (2012) Mammalian iron metabolism and its control by iron regulatory proteins. Biochim Biophys Acta 1823:1468–1483
Wang J, Fillebeen C, Chen G, Biederbick A, Lill R, Pantopoulos K (2007) Iron-dependent degradation of apo-IRP1 by the ubiquitin-proteasome pathway. Mol Cell Biol 27:2423–2430
Acknowledgments
Funded by University of Brescia (Fondi ex 60 % to I.Z.). We thank Dr. Sonia Levi (San Raffaele Scientific Institute, Milan, Italy) and Dr. Franco Taroni (Istituto Neurologico Carlo Besta, Milan, Italy) for supplying MT53 cells and antibodies to murine FTH and FTL and to frataxin.
Author information
Authors and Affiliations
Corresponding author
Additional information
Emiliano Cocco and Vanessa Porrini have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cocco, E., Porrini, V., Derosas, M. et al. Protective effect of mitochondrial ferritin on cytosolic iron dysregulation induced by doxorubicin in HeLa cells. Mol Biol Rep 40, 6757–6764 (2013). https://doi.org/10.1007/s11033-013-2792-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-013-2792-z