Abstract
In the individual application of adriamycin, mitomycin, vindesine and their combined application with tamoxifen for the pre-treatment of the human cholangiocarcinoma cell line QBC939, QBC939 was determined by MTT assay to investigate the inhibitive effect and its initial mechanism of TAM on cell growth. Growth cycle and apoptosis of each group were determined by flow cytometry. Concentration of ADM in QBC939 was detected by flow cytometry. The levels of their P-glycoprotein were detected by immunohistochemistry. The mRNA and protein levels of apoptotic-associated genes Bcl-2 and Bax were determined by western blot and real-time PCR. The inhibitive rates of adriamycin, mitomycin, vindesine to QBC939 and the apoptosis rates of QBC939 were enhanced after the pre-treatment of tamoxifen. Influence of tamoxifen in their growth cycle was not so obvious except vindesine group because of the increasing cell numbers of G 2/M phase in which cells may be blocked. The contents of adriamycin in cells rose after the pre-treatment of tamoxifen. Expression level of the multi-drug resistant protein on cell surface was shown as (+). Furthermore, real-time PCR and Western blot analysis revealed an upregulation of Bcl-2 and a downregulation of Bax in QBC939 after the pre-treatment of tamoxifen. Therefore, tamoxifen may have the ability to enhance the relative sensitivity of QBC939 to chemotherapeutics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As one of the most common gastrointestinal neoplasms, cholangiocarcinoma is the second most common primary hepatobiliary cancer, after hepatocellular carcinoma [1]. The incidence of cholangiocarcinoma has been increasing persistently over the past decades. Surgery resection represents the only curative treatment for BDC [2]. However, because of its special biological behavior, the sensitivity of cholangiocarcinoma to chemotherapeutics remains rather low [3]. Fewer than 20% of cholangiocarcinomas are potentially resectable at the time of diagnosis [4]. Adjuvant radiotherapy [5–7] may not reduce the recurrence rate after resection; either may biliary drainage and palliative radiotherapy [8–10] prolong the survival rate [11–13]. Single-drug chemotherapy also has not been proven useful for prolonging life and relieving jaundice [14–18]. Therefore, the prognosis of conventional therapies for relieving unresectable cholangiocarcinoma, including chemotherapy, radiotherapy, endoscopic and percutaneous biliary drainage, may be very dismal. The overall 5-year survival rate, which is less than 5%, remains very low during the past 30 years [19].
The assay of the content of the multi-drug resistant (MDR) protein (P-glycoprotein, P-gp) in the normal bile duct and cholangiocarcinoma sample indicates that gallbladder is an organ of high level P-gp accumulation, which elucidates the mechanism of MDR at the molecular level [20]. Tamoxifen (TAM) has been primarily used to treat patients with breast cancer and nonbreast cancers, including hepatocellular, pancreatic, renal cell, ovarian and melanoma carcinomas, etc. [21–23].
The human cholangiocarcinoma cell line QBC939 was established from a Chinese patient with extrahepatic bile duct carcinoma in 1997 by the hepatobiliary surgery performed in the Southwest Hospital of the Third Military Medical University. In our study, we are trying to discuss the mechanism of MDR of the human cholangiocarcinoma in this experiment, in the hope of seeking a new approach to the use of chemotherapeutics in the treatment of the human cholangiocarcinoma.
Materials and methods
Cell culture
The human cholangiocarcinoma cell line QBC939 was obtained from the hepatobiliary surgery performed in the Southwest Hospital of the Third Military Medical University (Wang Shu-Guang, MD, China); Cells were cultured in 25 cm2 tissue culture flasks (Renner, Darmstadt, Germany) in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal calf serum, 100 units/ml penicillin and 100 mg/ml streptomycin (Invitrogen). The cultures were kept in a humidified atmosphere of 5% CO2 at 37°C. Cell passage was at preconfluent densities using 0.05% trypsin and 0.5 mm-EDTA (Invitrogen), when the density becomes 40–50%.
MTT activity measurement
The MTT (3-[4,5-dimethyl-2-thiazol-2-yl]-2,5-diphenyltetrazolium bromide) (Sigma Chemical Co., St. Louis, MO, USA) assay is a colorimetric measurement of MTT reduction to a blue formazan product by mitochondrial dehydrogenases of viable cells [24]. Cells were seeded in 96-well plate at the density of 2 × 103–3 × 103 per well and incubated for 24 h. Thereafter, the medium was replaced and incubation continued for another 48 h in the presence or absence of the test compounds (referred to as pre-exposure or pretreatment) of 25 μg/ml adriamycin (ADM, Farmitalia Carlo Erba, Milan, Italy), 2 μg/ml mitomycin (MMC, Kyowa Pharmaceutical Kogyo Co., Ltd, Tokyo, Japan), 0.5 μg/ml vindesine (VDS, Sanlian Pharmaceutical Co., Ltd, Harbin, China) with or without 10 μmol/l tamoxifen (TAM, First Pharmaceuticals Co., Ltd, Hangzhou, China). Then, the medium was replaced and 50 μl MTT working solution was added to each well at a final concentration of 0. 5 mg/ml. Cells were incubated for 4 h at 37°C and the medium was changed to 100 μl Dimethyl sulfoxide (DMSO) to dissolve the formazan. Optical density (A) was measured at 492 nm of the wave length using a Tecan SpectraFluor Plus microplate spectrophotometer (Esbe Scientific Industries Inc., Canada). Each experiment was performed in triplicate. A dose-response study was performed to calculate the 50% inhibiting concentration (IC50) for different chemotherapeutic agents: ADM 25 μg/ml, MMC 2 μg/ml, VDS 0.5 μg/ml. TAM (10 μmol/l) was selected as the sensitizer because its inhibition ratio was low within 2.92%, which did not show obvious inhibitory action on QBC939 when applied individually. The quantity of viable cells was reflected by cell growth inhibition rate calculated using the following formula:
Cell cycle and apoptosis analysis
Human cholangiocarcinoma QBC939 cells were seeded at a density of 50,000 onto the six-well culture flasks for 24 h and then incubated for another 24 h in the presence or absence of the test compounds. Cells were trypsinized, pelleted by centrifugation at 500g for 3 min, washed twice with PBS and adjusted to 1 × 106 cells/ml. Cells were then fixed by suspending the cells at 4°C in ethanol for 24 h. Thereafter, the suspension was centrifuged for 3 min at 500 g, and the pellet was washed twice in 38 mm-sodium citrate buffer (pH 7.4). After washing and centrifugation, cells were incubated with the dye solution containing 7-amino actin (1 mg/ml) and 1 U DNase-free RNase in sodium citrate buffer. Cell cycle and apoptosis analysis was performed using a FACScan (Becton Dickinson, San Jose, CA, USA) and the software BD CellQuest™ Pro version 1.41 for data analysis.
Assay of intra-cellular ADM concentration
Cells were cultured in 25 cm2 tissue culture flasks, digested into 2 × 106/l suspension, and then incubated for 30 min at 37°C in the presence of the test compounds (referred to as pre-exposure or pretreatment) of 5 μg/ml ADM with or without 2.5 μg/ml VER followed by a centrifugation step (15,000×g for 2 min). The medium was replaced and the precipitation was washed three times. Cells was incubated for another 10 min at 37°C and washed. Intra-cellular ADM concentration was performed with a FACScan.
Immunohistochemistry method
Streptavidin-biotin-peroxidase method was used for staining with the antibodies following manufacturer’s instructions. Positive reaction was defined as brown cellular staining. Leica RA2 microscope (Leica Microystems, Switzerland) was used for the analysis. The sections were evaluated by two independent observers. Negative, weak, median, and strong positive reactions were defined as: (−) positive cells <25%; (+) positive cells <50%, but >25%; (++) positive cells <75%, but >50%; and (+++) positive cells >75%, respectively. Each section was observed randomly for 10 high-power amplification fields and an average number was obtained. Primary antibody replaced by PBS was showed as the negative control.
Gel electrophoresis and western blotting
After different pretreatment, cells were homogenized in chilled RIPA buffer. After centrifugation at 10,000×g for 10 min at 4°C, the supernatant was recovered and assayed for protein content (DC protein assay; Bio-Rad, Hercules, CA, USA). Equal amounts of total protein were separated on 10% SDS–polyacrylamide gels and then transferred to a nitrocellulose membrane. After blocking overnight in Tris-buffered saline containing 0.05% Tween (TBS-T) and 5% dry powdered milk, membranes were washed three times for 5 min each with TBS-T and incubated for 2 h at room temperature in primary antibody (ab7973 and ab7977; abcam, Massachusetts, USA). After three washes with TBS-T, the membranes were incubated for 1 h with horseradish peroxidase-conjugated secondary antibody (abcam, Massachusetts, USA). Following two washes with TBS-T and one wash with TBS, the membranes were developed for visualization of protein by the enhanced chemiluminescence reagent (Amersham, Princeton, NJ, USA). Densitometric analysis was repeated (Alpha Imager 1220 system) for three times.
Quantitative real-time PCR
Total RNA was extracted by RNeasy Mini Kit (Qiagen, Hilden, Germany) from QBC939 and quantified spectrophotometrically (Gene Quant II; Amersham Pharmacia Biotech, Piscataway, NJ). First-strand cDNA was synthesized from 1 μg total RNA by reverse transcription using oligo-dT primers and reverse transcriptase (superscript II; Invitrogen) according to the manufacturer’s instructions. Real-time PCR reactions were performed in a 20 μl mixture, containing 1 μl of the cDNA preparation, 10× PCR mix (iQ SYBR Green Supermix; Bio-Rad, Hercules, CA) and 500 nm of each primer, in a thermocycler (iCycler iQ system; Bio-Rad) using the following PCR parameters: 95°C for 5 min followed by 50 cycles at 95°C for 15 s, 65°C for 15 s, and 72°C for 15 s. The fluorescence threshold (Ct) was calculated with the corresponding software. The absence of nonspecific products was confirmed by both the analysis of the melting-point curves and by electrophoresis in 3% agarose gels. GAPDH served as an internal standard of mRNA expression.
Statistical analysis
Data were evaluated by variance analysis of single factor, Mann–Whitney U-test and T-test. For each variable at least three independent experiments were carried out. Results are expressed as means and their standard errors. All analyses were done using the GraphPad Software Prism 5 (San Diego, CA, USA); differences were considered significant at P < 0.05.
Results
TAM may enhance the effect of chemotherapeutics
It is well-known that MTT reagent directly reacts with the mitochondria (mitochondrial dehydrogenase) of metabolically active cells. Therefore, the reaction of MTT reduction is directly proportional to the number of growing cells. The measured optical density, which could be recorded using ELISA microplate reader, is directly proportional to the number of viable cells in the culture medium. Therefore, MTT is regarded as a quantitative assay to determine the cytotoxicity of the materials, determined the viability/proliferation of the cells in solution in different groups. Table 1 and Fig. 1a plots the MTT assay results obtained using the human cholangiocarcinoma cell line QBC939. The inhibitive rates of ADM, MMC, VDS were 48.84, 44.19, 45.76%, respectively; while after the pre-treatment of TAM, the inhibitive rate went up to 64.37, 62.68, 65.90% with high inhibitive rates in each group (P < 0.05). These data indicate that the effects of combination chemotherapy with TAM may be enhanced, which shows a sensitization effect of TAM.
Assay of MTT and FCM to the effect of combination chemotherapeutics of TAM (%). a Assay of MTT to the effect of combination chemotherapeutics of TAM (%). After the pre-treatment of TAM, the inhibitive rate of ADM, MMC, VDS went up significantly (P < 0.05). These data indicate that the effects of combination chemotherapeutics with TAM may be enhanced, and TAM showed as a sensitization. b Assay of FCM on the effect of combination chemotherapeutics of TAM (%). Apoptosis rate of the control group and the group pretreated with TAM did not have significant difference (P < 0.05). The apoptosis rates after the pre-treatment of TAM were enhanced significantly (P < 0.05). * vs. ** group, P < 0.05. ** vs. *** group, P < 0.05. One-way ANOVA was performed with Tukey Kramer post-hoc comparison. Values were calculated by Student’s t-test. All data are given as means (SE)
Apoptosis promotion of TAM
The control group and the group of TAM did not have significant difference (P < 0.05) in the apoptosis rate. The apoptosis rates after the pre-treatment of TAM were enhanced apparently to 20.66, 14.18, 21.91% from 11.37, 7.25, 9.04%, as are shown in the Table 1, Fig. 1b (P < 0.05). An obvious apoptotic peak can be seen (Fig. 2a) compared to the control group (Fig. 2b).
Impact on the cell cycle analysis
Table 2 and Fig. 3 show the effect of TAM in the combination chemotherapy on the cell cycle. Cells blocked into the G 2/M phase increased significantly after the pre-treatment of TAM (P < 0.05) which led the cells in the G 0/G 1 and S phases to decrease. This may be due to the fact that TAM induces apoptosis by means of suppression of mitosis and extension of the mitosis phase. Because of the phase-nonspecific inhibitive character of ADM and MMC, cell cycle did not change significantly after the pre-treatment of TAM (P > 0.05). However, when it comes to VDS, the G 2/M phase-specific inhibitive drug, cells blocked into the G 2/M phase increased significantly (P < 0.05), as a result, cells were induced to death more easily.
Effect of combination chemotherapeutics of TAM on the cell cycle (%). Cells blocked into the G 2/M phase increased significantly after the pre-treatment of TAM (P < 0.05) which lead the cells in the G 0/G 1 and S phrase decreased. While cell cycle changed not significantly after the pre-treatment of TAM (P > 0.05). In the VDS group, cells blocked into the G 2/M phrase increased significantly (P < 0.05). * vs. ** group, P < 0.05. ** vs. *** group, P < 0.05. One-way ANOVA was performed with Tukey Kramer post-hoc comparison. Values were calculated by Student’s t-test. All data are given as means (SE)
The intra-cellular concentration of ADM enhanced by TAM
The intra-cellular concentration of ADM was enhanced to 298.91 from 260.48 after the pre-treatment of TAM (P < 0.05), which may indicate that combination chemotherapeutics with TAM increase the concentration of intra-cellular ADM, and promote the accumulation of the drug, thus enhancing the killing ability of the drug and causing the death of QBC939 (Fig. 4). (P < 0.05).
Increasement of ADM Concentration of intra-cellular after the pre-treatment of TAM. The intra-cellular Concentration of ADM was enhanced to 298.91 from 260.48 after the pre-treatment of TAM (P < 0.05), which may indicate that combination chemotherapeutics with TAM increase the concentration of intra-cellular antitumor drug. Values were calculated by Student’s t-test. All data are given as means (SE)
The positive expression level of P-gP
P-gP was stained to flavedo and buffy in the cellular cytoplasm and membrane; while only some caryons were stained. P-gP expression was shown as (+) in the QBC939, suggesting the insensitivity of QBC939 to those chemotherapeutics (Fig. 5).
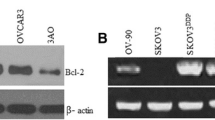
The expression levels of Blc2 and Bax enhanced by TAM in the combination chemotherapeutics
Western blot analyses were performed to determine the relative protein expression of Blc2 and Bax in different groups. The intensity measurements for whole-cell proteins were determined from the ratio of the integrated intensity of the Blc2 and Bax band to the integrated intensity of the β-actin band in the same sample. Western blotting showed that the expression level of Blc2 was enhanced; while Bax was inhibited when TAM was added in the combination chemotherapeutics (P < 0.05). There were no significant differences between the control group and the TAM group (P < 0.05, Fig. 6a, b).
Expression levels of Blc2 and Bax proteins were enhanced by TAM in the combination chemotherapeutics. a Western blotting analysis of Blc2 and Bax proteins. Expression was analysed in membrane fractions by immunoblotting and subsequent densitometry. b The statistical evaluation of densitometric data represented protein expression of the three separate experiments (in percentage of all controls on the same blot). * vs. ** group, P < 0.05. ** vs. *** group, P < 0.05. One-way ANOVA was performed with Tukey Kramer post-hoc comparison. Values were calculated by Student’s t-test. All data are given as means (SE)
Levels of Bcl-2 and Bax after the pretreatment of chemotherapeutic drugs
Real-time PCR was used to survey the changes in the mRNA expression of different groups of QBC939 after the pretreatment of chemotherapeutic drugs, involving the apoptotic-associated genes, Bcl-2 and Bax. A quantitative analysis showed that the mRNA level of Bcl-2 increased sharply at 2 h, and remained elevated even at 12 and 24 h, though gradually decreasing during the three time points (P < 0.05, Fig. 7a, b, c). However, the mRNA level of Bax was significantly downregulated from 2 h, and continued to decrease gradually at 12 and 24 h (P < 0.05, Fig. 7d, e, f).
Real-time PCR analysis of Bcl-2 and Bax after the pretreatment of chemotherapeutic drugs in QBC939 at different time points ranging from 2 to 24 h in different groups. a The Bcl-2 mRNA was upregulated as early as 2 h in the group of combination chemotherapeutics with TAM. b The Bcl-2 mRNA was upregulated at 12 h in the group of combination chemotherapeutics with TAM. c The Bcl-2 mRNA was upregulated at 24 h in the group of combination chemotherapeutics with TAM. d The Bax mRNA was upregulated as early as 2 h in the group of combination chemotherapeutics with TAM. e The Bax mRNA was upregulated at 12 h in the group of combination chemotherapeutics with TAM. f The Bax mRNA was upregulated at 24 h in the group of combination chemotherapeutics with TAM. The GAPDH served as the loading control. The mean ± SD of data from three independent experiments was shown. * vs. ** group, P < 0.05. ** vs. *** group, P < 0.05. One-way ANOVA was performed with Tukey Kramer post-hoc comparison. Values were calculated by Student’s t-test. All data are given as means (SE)
Discussion
The morbility of cholangiocarcinoma has been rising in recent years. Its special anatomy and occult invasion make its clinical diagnosis difficult, often depriving the patient of the opportunity of treatment after the definitive diagnosis. In addition, the special biological character of carcinoma in bile duct system makes cholangiocarcinoma refractory to radiotherapy and chemotherapy, leaving few tools in the surgeon’s hands. It has been reported that gallbladder itself is an organ rich in multidrug resistant (MDR) protein, P-gp. MDR gene is located on the 7th chromosome, which can be activated by related genes nearby, and then induce and enhance the translation and amplification of itself, followed by the over-expression of P-gp. P-gp has the ability to form the drug channel, acting as a drug pump, and detect drug concentration in cells. Therefore, if a drug enters into cells, P-gp will bind itself to drug molecules and induce a series of further reactions. Meanwhile, adenosine triphosphate (ATP) will bind itself to the corresponding receptors and release energy, leading to the transmission of drugs to the extracellular space in order to maintain a relatively low level of the intracellular drug concentration. Gradually (as time goes on), MDR to chemotherapeutic drugs was formed [25, 26]. This QBC939 cholangiocarcinoma cell line was showed to have (as) a relatively higher P-gp expression by immunohistochemistry, which, as one of the mechanisms, could make the cholangiocarcinoma less responsive to chemotherapy. Ferguson [27] reported that tamoxifen showed the ability to enhance the survival rate of advanced breast cancer patients treated by doxorubicin in phase III. And the pre-treatment of tamoxifen greatly enhanced cytotoxicity of docetaxel, paclitaxel, epirubicin, doxorubicin, and vinorelbine against MDR cells, by 50%. TAM, a cholangiocarcinoma sensitizer, could act as a P-gp substrate; by competing for the P-gp binding site with antineoplastic agents, it could inhibit the function of transmembrane transporter, and lower the velocity of drug efflux from within cells, leading to the enhancement of drug concentration and the effect of the chemotherapeutic drugs. The inhibitive rates of the human cholangiocarcinoma cell line QBC939 by ADM, MMC, VDS were 48.84, 44.19, and 45.76%, respectively; by comparison, after the pre-treatment of TAM, the inhibitive rates went up to 64.37, 62.68, and 65.90%, an indication that the effect of the chemotherapy drugs was enhanced by the added TAM. Apoptosis rate of the cells after the pre-treatment of TAM also increased significantly to 20.66, 14.18, and 21.91% from 11.37, 7.25, and 9.04%, indicating the added apoptosis induced by the cooperation of TAM and its corresponding chemotherapy drugs. In addition, mRNA and protein levels of apoptotic-associated genes Bcl-2 and Bax determined by western blot and real-time PCR revealed an upregulation of Bcl-2 and a downregulation of Bax in QBC939 after the pre-treatment of TAM.
As an estrogen receptor antagonist, TAM is extensively used in the treatment of mammary adenocarcinoma. The most common side-effect is vasomotor symptoms reported up to 1–4%. Toxicity and other side-effects were relatively uncommon during the clinical use of the TAM, which is 30 mg once daily for at least half a year for the breast cancer patients [28]. As far as our study was concerned, the total amount daily was 1.77 × 10−5 mg (10 μmol/l), and therefore, the side effect was insignificant. As was shown in the test, the inhibitive rate of TAM at 10 μmol/l was 0.15. This will make it unnecessary to limit its application for the possible cytotoxicity to normal cells, because the increased rate of cell inhibition and apoptosis was not due to the inhibitory effect of TAM itself, but by the enhanced effect of TAM on the chemotherapeutic agents. By comparing ADM and ADM when mixed with TAM, respectively for the treatment of cholangiocarcinoma cells, it is obvious that intensity of fluorescence which indicates the intracellular ADM measured by Flow cytometry was enhanced by the effect of TAM, resulting in the intracellular accumulation of ADM. It also proved that the extracellular to intracellular transportation of ADM was hindered by TAM, resulting in the relatively higher concentration of intracellular chemotherapy drugs, and this led to the enhancement of toxicity to cholangiocarcinoma cells. ADM and MMC are non-specific cycle inhibitors, because the cell cycles do not change so significantly after the pre-treatment of TAM (P > 0.05). However, VDS, a phrase-specific inhibitive drug which has effect on cells within mitosis period, may block cholangiocarcinoma cells in the G2/M phrase (P < 0.05), and lead to their death more easily. Adding TAM increased cholangiocarcinoma cells of G2/M phase from 16.44 to 29.47%. The combination chemotherapeutics of TAM with other three chemotherapeutic agents do not change the pharmacological characterization of the drugs, but enhance their anti-tumor effect.
Conclusion
In this study, it was indicated that TAM might compete for binding sites with other chemotherapy drug molecules and limit the extracellular transport of drugs from cholangiocarcinoma cells so as (not?) to induce their accumulation in the cells and lead to an increase of cell damage. In addition, the drug resistance of neuroblastoma, small cell lung cancer, gastric cancer, liver cancer, bladder cancer, ovarian cancer, and breast cancer to vincristine, vinblastine, cisplatin, and epirubicin can all be reversed by TAM and other simillimum, which is consistent with our experimental results [29].
Cancer cells could gradually develop their resistance to chemotherapeutic drugs in the course of chemotherapy, and there have been a lot of researches in the study of resistance mechanisms [30], among which the study of P-gp protein is considered as a classic one. Whether P-gp is the only passway in the formation of MDR of cholangiocarcinoma to chemotherapy drugs, or whether there are other ways involved, still requires further studies. Appropriate treatment strategies formulated according to mechanisms of drug resistance will be a guide in the fight against cancer, and for that reason, it is a subject worth exploring. Now the hyperthermic treatment and magnetic nano-target chemotherapy of cholangiocarcinoma [31, 32] have become a new research focus, with broad and bright prospects. Breakthroughs in new therapeutic approaches based on gene technology [33, 34] can be expected.
References
Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM (1999) Biliary tract cancers. N Engl J Med 18:1368–1378
Lazaridis KN, Gores GJ (2005) Cholangiocarcinoma. Gastroenterology 128:1655–1667
Hur H, Park IY, Sung GY et al (2009) Intrahepatic cholangiocarcinoma associated with intrahepatic duct stones. Asian J Surg 1:7–12
Jarnagin WR, Fong Y, DeMatteo RP et al (2001) Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234(4):507–517 (discussion 517–519)
Todoroki T, Kawamoto T, Koike N et al (2001) Treatment strategy for patients with middle and lower third bile duct cancer. Br J Surg 88(3):364–370
Sagawa N, Kondo S, Morikawa T et al (2005) Effectiveness of radiation therapy after surgery for hilar cholangiocarcinoma. Surg Today 35(7):548–552
Pitt HA, Nakeeb A, Abrams RA et al (1995) Perihilar cholangiocarcinoma postoperative radiotherapy does not improve survival. Ann Surg 221(6):788–797 (discussion 797–798)
Shinchi H, Takao S, Nishida H et al (2000) Length and quality of survival following external beam radiotherapy combined with expandable metallic stent for unresectable hilar cholangiocarcinoma. J Surg Oncol 75(2):89–94
Bowling TE, Galbraith SM, Hatfield AR et al (1996) A retrospective comparison of endoscopic stenting alone with stenting and radiotherapy in non-resectable cholangiocarcinoma. Gut 39(6):852–855
Sirica AE (2005) Cholangiocarcinoma: molecular targeting strategies for chemoprevention and therapy. Hepatology 41:5–15
Kaassis M, Boyer J, Dumas R et al (2003) Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. Gastrointest Endosc 57(2):178–182
Chang WH, Kortan P, Haber GB (1998) Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc 47(5):354–362
Prat F, Chapat O, Ducot B et al (1998) Predictive factors for survival of patients with inoperable malignant distal biliary strictures: a practical management guideline. Gut 42(1):76–80
Figueras J, Llado L, Valls C et al (2000) Changing strategies in diagnosis and management of hilar cholangiocarcinoma. Liver Transp l6(6):786–794
Takada T, Amano H, Yasuda H et al (2002) Is postoperative adjuvant chemotherapy useful for gallbladder carcinoma? A phase III multicenter prospective randomized controlled trial in patients with resected pancreaticobiliary carcinoma. Cancer 95(8):1685–1695
Todoroki T (2000) Chemotherapy for bile duct carcinoma in the light of adjuvant chemotherapy to surgery. Hepatogastroenterology 47(33):644–649
Rao S, Cunningham D, Hawkins RE et al (2005) Phase III study of 5FU, etoposide and leucovorin (FELV) compared to epirubicin, cisplatin and 5FU (ECF) in previously untreated patients with advanced biliary cancer. Br J Cancer 92(9):1650–1654
Glimelius B, Hoffman K, Sjödén PO et al (1996) Chemotherapy improves survival and quality of life in advanced pancreatic and biliary cancer. Ann Onco l7(6):593–600
Shaib Y, El-Serag HB (2004) The epidemiology of cholangiocarcinoma. Semin Liver Dis 24:115–125
Han P, Kang JH, Li HL et al (2009) Antiproliferation and apoptosis induced by tamoxifen in human bile duct carcinoma QBC939 cells via upregulated p53 expression. Biochem Biophys Res Commun 385(2):251–256
Tobias JS (2004) Endocrine approaches for the treatment of early and advanced breast cancer in postmenopausal women. Int J Biochem, Cell Biol 36:2112–2119
Grainger J, Metcalfe JC (1996) Tamoxifen: teaching an old drug new tricks? Nat Med 2:381–385
Mandlekar S, Kong AN (2001) Mechanisms of tamoxifen-induced apoptosis. Apoptosis 6:469–477
Carmichael J, DeGraff WG, Gazdar AF et al (1987) Evaluation of a tetrazolium-based semiautomated colorimetric assay: assessment of chemosensitivity testing. Cancer Res 47:936–942
Kerb R, Hoffmeyer S, Brinkmann U (2001) ABC drug tansporters: hereditary polymorphisms and pharmacological impact in MDR1, MRP1 and MRP2. Pharmacogenomics 1:51–64
Hooiveld GJ, Van Montfoort JE, Meijer DK et al (2001) Function and regulation of ATP-binding cassette transport proteins involved in hepatobiliary transport [J]. Eur J Pharm Sci 4:525–534
Ferguson PJ, Brisson AR, Koropatnick J et al (2009) Enhancement of cytotoxicity of natural product drugs against multidrug resistant variant cell lines of human head and neck squamous cell carcinoma and breast carcinoma by tesmilifene. Cancer Lett 2:279–289
Andersen J, Kamby C, Ejlertsen B et al (2008) Tamoxifen for one year versus two years versus 6 months of Tamoxifen and 6 months of megestrol acetate: a randomized comparison in postmenopausal patients with high-risk breast cancer (DBCG 89C). Acta Onco l4:718–724
Singh MN, Martin-Hirsch PL, Martin FL (2008) The multiple applications of tamoxifen: an example pointing to SERM modulation being the aspirin of the 21st century. Med Sci Monit 9:RA144–RA148
Incles CM, Schultes CM, Kelland LR et al (2003) Acquired cellular resistance to flavop iridol in a human colon carcinoma cell line involves up-regulation of the telomerase catalytic subunit and telomere elongation. Sensitivity of resistant cells to combination treatment with a telomerase inhibitor 1 [J]. Mol Pharmacol 5:1101–1108
Andrew DG, Giles R (2005) Mathematical modeling of magnetically targeted drug delivery. J Magn Magn Mater 5:455–463
Yoshino T, Hirabe H, Takahashi M et al (2008) Magnetic cell separation using nano-sized bacterial magnetic particles with reconstructed magnetosome membrane. Biotechnol Bioeng 101(3):470–477
Iain B, Kawan S, Sarahl M (2004) Reduced expression of p27 is a novel mechanism of docetaxel resistance in breast cancer cells [J]. Breast Cancer Res 56:601–607
Ghayad SE, Bieche I, Vendrell JA et al (2008) mTOR inhibition reverses acquired endocrine therapy resistance of breast cancer cells at the cell proliferation and gene-expression levels. Cancer Sci 10:1992–2003
Acknowledgments
The authors thank Shanghai Jiao Tong University Affiliated Sixth People’s Hospital for technical assistance during this study. This work was financially supported by National Natural Science Foundation of China (No. 30672044), and the National Basic Research Program of China (No. 2008CB517403).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, ZH., He, YP. & Qin, H. The growth-inhibition effect of tamoxifen in the combination chemotherapeutics on the human cholangiocarcinoma cell line QBC939. Mol Biol Rep 37, 2693–2701 (2010). https://doi.org/10.1007/s11033-009-9801-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-009-9801-2