Abstract
Dependence of plasma total homocysteine (tHcy) and DNA damage profiles on melanodialdehyde (MDA), oxidative stress, liver function tests (LFT), and lipids was studied in non-obese and obese subjects in the Pakistani population. Development of obesity is influenced by both genetic, biochemical and environmental factors. Plasma homocysteine (Hcy) and DNA damage profiles play a pivotal role in its progression. We studied 160 obesity patients and 160 lean subjects. Leukocytes were evaluated for DNA damage by comet assay and blood plasma for biochemical properties using commercial kits. Plasma Hcy level and DNA damage were strongly correlated with triglycerides (P < 0.000), LDL-cholesterol (P < 0.001), systolic blood pressure (P < 0.001), cholesterol (P < 0.004), MDA (P < 0.004) and total oxygen stress (P < 0.004) in obese individuals. Both Hyc and DNA damage were negatively associated with total anti-oxidant response and globulin. Both Hcy profile and DNA damage may have a role in the endothelium damage even in the normal range and are related to triglycerides, ALT, MDA, TOS, HDL- and LDL-cholesterol in the Pakistani population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is wide-spread in both developed and developing countries and is due to deposition of fat in the fat compartments of body [1, 2]. It is due to the growing trend of sedentary lifestyle and increased consumption of high caloric diet [3, 4]. It is linked with metabolic complications, namely, hypercholesterolemia, hyper-insulinemia and dyslipidemia [5]. A BMI cut-off point for overweight and obesity is 25 and 30 kg/m2 [5, 6]. High lipid profile of the blood serum is considered as one of the factors that may develop obesity in diabetes mellitus and thus the progression of diabetes in a population. Knowledge of adipocyte biology is essential for understanding the patho-physiological basis of obesity and metabolic disorders. High levels of homocysteine are linked with obesity and the early development of heart and blood vessel disease. Its high level is considered an independent risk factor for heart disease. There is a link between high homocysteine level and damage to the arteries, causing atherosclerosis and the formation of blood clots [6, 7].
The possible risk factors for elevated levels of tHcy may include BMI, excessive use of pesticide, low consumption of folate and vitamins [7], which lower down recycling of homocysteine and methionine in blood plasma. A man’s risk of having higher tHcy level (hyperhomocysteinemia) is influenced by genetic, metabolic errors and environmental factors [8–10].
Excess homocysteine (>12 μmol/l) has a toxic effect on the endothelium, promotes thrombosis via platelet activation, causes oxidation of LDL-cholesterol and increases smooth muscle proliferation [11]. Oxidative stress causes oxidation of membrane lipoproteins and oxidation of DNA leading to tissue damage [12–15]. The liver function test may be a marker in monitoring the development and progression of the disease and documentation of the clinical evidence of this disease [16], since abnormal serum levels of hepatic enzymes are frequently found in subjects with obesity or hyperlipidemia [16]. In this investigation, we have observed the plasma levels of tHcy, and DNA damage and to establish their correlation with total oxidants, antioxidants, MDA, LFT, and lipids (triglycerides and cholesterols) in obese subjects and control individuals.
Materials and methods
Subjects
This case-controlled investigation included a total of 320 subjects, consisting 160 obese patients and 160 healthy volunteers as controls, who visited Government hospital. All cases and controls were recruited in this study under informed consent. University ethical committee approved the study and work was performed in accordance with the Declaration of Helsinki.
A complete physical examination of each individual was performed by one of the physicians attending the controls and patients. Following factors were recorded: (1) Hypertension indicated by a systolic blood pressure ≥140 mm Hg, a diastolic blood pressure of ≥90 mm Hg or anti-hypertensive medication; (2) diabetes requiring medical or dietary treatment; (3) body mass index (BMI; kg/m2) was calculated by using the following formula: BMI = weight (kg)/height (m)2; (4) body temperature (°F) was recorded by using thermometer; (5) HDL-cholesterol; (6) triglycerides; (7) blood glucose; and (8) low LDL-cholesterol were measured in the analytical laboratory using commercial kits.
Design
Risk factors for obesity include age, total cholesterol, HDL, BMI, glucose and cholesterol. Subjects were considered to have high cholesterol level if they had a value of 5.69 mmol/l (220 mg/dl) or more. Subjects were considered to be diabetic if they had a fasting blood glucose level of 7.77 mmol/l (140 mg/dl) or more. BP (cutoff values for systolic and diasystolic BP: ≥130 mm Hg or ≥85 mm Hg, respectively) was measured using manual sphygmomanometers after the controls and subjects had rested for 10 min in a quite room. Cut-off values of all risk factors were from published clinical values.
A total of 320 blood samples were collected from normal (n = 160) and obese (n = 160) patients. All subjects were asked to complete a questionnaire, which included standard demographic data (Table 1) as well as questions on their immunization status, history, fever, vomiting or medication as well as nutritional status. Normal and obese patients were not on any medication and were consuming routine diet. Efforts were made to match the patients and the controls for any potential confounding factors, namely age, gender, and socioeconomic condition. All of them belonged to urban area and were not exposed to any pesticide through out the study.
A sample of 10 ml of blood was collected from each individual using sterile disposable syringes and transferred to sterile heparin tubes. The tubes were kept cold and centrifuged to separate serum at 800g for 10 min. Later they were stored at −20°C till analysis.
Analytical methods
Serum glucose test was carried by commercially available kit (Biocon) through spectrophotometer. Total cholesterol (TC) and triglycerides (TG) were determined by using routine enzymatic methods. HDL- and LDL-cholesterols were determined by using commercially available kits per instructions of the manufacturers. Serum proteins, albumin and glubolin were also determined by using commercially available kit (Bio Rays). Plasma homocysteine (Hcy) was measured by homocysteine microtiter plate assay using enzyme-based kit (Diazyme). Plasma total oxidant status (TOS) and total antioxidants response (TAR) were measured colorimetrically as described previously [17, 18, respectively]. Malondialdehyde (MAD) levels were quantified by using thiobarbituric acid reactive species using spectrophotometer at 532 nm [19]. DNA damage was measured by performing comet assay by adopting the methods of Martin et al. [20]. Cells without DNA damage had an intact nucleus without a tail, whereas those cells having DNA damage had a comet-like look. The length of DNA migration in the comet tail was taken as an estimate of DNA damage and was measured with an ocular micrometer (μm). The laboratory performed strict external and internal quality control tests. Reagents for calibration of instruments were supplied by their manufacturers.
Statistical and sensitivity analyses
Data collected were subjected to calculations of mean ± SE. To calculate the differences between normal and obese (young male and female; old male and female subjects), data were analyzed by two way analysis of variance [21]. To evaluate the relationship between blood characteristics and DNA damage or homocysteine profile (μM/l), comparison of the correlation coefficients provided a feasible estimate of the strength of the association between different anthropometric data, and biochemical profiles.
Results
General and anthropometric characteristics of the subjects are shown in Table 1. In male and female, BMI was significantly higher in obese subjects as compared with their lean counterparts (16.75–22.98 kg/m2) and was an independent variable in both males and females, young and old (P ≤ 0.01). Overall mean systolic blood pressure increased significantly in old male and female while overall mean diastolic blood pressure was increased in female and decreased in males.
Mean serum glucose concentration was significantly low in old and in female obese cases (P ≤ 0.01) as compared to their control counterparts (young and male) respectively. However, young and the old obese individuals showed significantly higher value (P ≤ 0.01) in their serum glucose concentration. Mean serum cholesterol and triglyceride were significantly higher in old female and male obese cases than young male and female obese cases as compared to their normal individuals (Table 2). HDL-cholesterol was significantly higher in both old normal and obese males, followed by normal female and obese (P ≤ 0.01) cases (old ones). They were followed by normal male and female (young group). Young obese group (both male and female) had significantly lower values of this variable. However, LDL-cholesterol was significantly higher in old obese male and female, young obese females followed by normal individuals. Total proteins were significantly higher in normal male and female (both old and young), followed by obese cases. Almost similar trend was observed in the case of serum glubolin but albumin was non-significantly different in obese and normal cases.
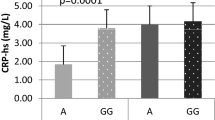
In the present study, alanine aminotransferase (ALT) and AST were significantly (P ≤ 0.01) higher in obese individuals (male and female). In the present study, we determined serum antioxidant response (TAR) to be significantly low while oxidant status was high in obese patients (young and old). Serum homocysteine was significantly high in obese patients as compared to healthy individuals. DNA damage level in obese patients was significantly higher (P ≤ 0.01) than their lean counterparts.
We performed the correlation analysis between Hcy and all studied parameters (Table 3) in obese and normal subjects. Serum homocysteine was positively correlated with all parameters (Table 3) in obese patients (P ≤ 0.000–0.006), except diastolic blood pressure, total proteins and AST. It was also observed that Hcy concentration in normal individuals was independent of BMI, triglycerides, glucose and cholesterol level, total proteins, glubolin, and AST. It was negatively correlated with glubolin and TOS in obese patients.
DNA damage in obese patients was strongly dependent (P ≤ 0.01) on all parameters studied (Table 4) except glubolin and TAR where it was negatively correlated. Correlation between Hcy and BMI, blood pressure, cholesterol, LDL-cholesterol, albumin, glubolin, TAR and TOS was not detected in normal subjects. In these subjects, it was strongly correlated to triglycerides, ALT and MDA (P ≤ 0.01).
Discussion
Homocysteine (Hcy) is an independent risk factor for development and progression of obesity. It may be related with several different anthropometric data, and biochemical profiles. Systolic and diastolic blood pressure were significantly and positively related to body mass index in obese and non-obese groups as also reported earlier [22]. In men and women both the prevalence of overweight and obesity increased with age and was evident between 30 and 40 years [23]. Previously, Grundy [7] used large samples of gender, a wide age range subjects and confirmed the notion that overweight and obese adolescents have higher glucose and insulin level as well as abnormal lipid profile relative to their lean peers. These results further elaborate that metabolic alteration caused by excess body fat are expressed in obesity and are of clinical importance [3, 4].
A quarter of the population of Pakistan would be classified as overweight or obese with the use of Indo-Asian specific BMI cutoff values [23]. Total cholesterol, LDL-cholesterol, triglycerides and HDL were significantly (P ≤ 0.01) higher in obese than in their lean counterparts. Increasing body fat will lead to significant changes in physiological function. It contributes towards the development of hypertension, increase in plasma insulin and insulin resistance, diabetes mellitus and hyper-lipidemia [6, 7]. In women with BMI of 25, 30 and 35, risk of diabetes increased 5-, 28- and 23-fold or greater as compared to women with BMI of 21 or less. ALT and AST were significantly (P ≤ 0.0000) higher in obese subjects than their normal leans. Burns et al. [24] reported that BMI is strongly associated with increased serum activities of ALT, AST and γ-glutamyl transferase (GGT). A significant change in serum ALT, AST and GGT has been linked with increased BMI [1–3]. Choi [25] also demonstrated that high body fatness exhibited significantly higher AST in men and GGT concentration in women compared to normal subjects with low fatness.
Again homocysteine was higher in obese subjects and was gender dependent. It was significantly high in old obese patients, followed by young obese patients. Its formation is regulated by mutations in its genes for related enzymes and by folic acid, B12 and B6 [7]. Serum homocysteine showed a positive correlation with glucose, cholesterol, triglycerides and LDL-cholesterol (Table 4) in obese individuals and corroborated the work of previous workers [10, 12]. Homocysteine is also known to mediate LDL-auto-oxidation in the presence of copper [20]. Higher homocysteine concentration was also observed in the hyperinsulinemic obese subjects and it is suggested to have its role in the high risk cardiovascular disease in obese patients [10]. Oxidative stress present in insulin resistant obese subjects may worsen the angiotoxicity of homocysteine thus increasing the risk of arteriosclerosis [8, 9].
Low plasma antioxidant status as observed in the present study have been linked to oxidative modification of LDL-cholesterol [9, 10]. It has been reported that aging develops reduced ability to response to stress as level of three critical repair proteins decrease as a result of oxidative stress response.
Obesity is the central and causal component in metabolic syndrome and adipocytes produce a variety of biologically active molecules [9]. These compounds are called adipocytokines or adipokines, part of total plasma proteins. Dys-regulation of these adipokines participates in the pathogenesis of obesity. A decrease in plasma adiponectin is causative for insulin resistance and atherosclerosis in obese subjects [2–4].
Conclusion
This study provides a positive correlation of homocysteine with triglycerides (P < 0.000), LDL-cholesterol (P < 0.001), BMI (P < 0.004), systolic blood pressure (P < 0.001, cholesterol (P < 0.004), ALT (P < 0.004), MDA (P < 0.004) and TOS (P < 0.004) in obese individuals. Correlation coefficient of Hyc and DNA damage indicated that both of them were negatively associated with TAR and globulin.
DNA damage was positively correlated with BMI, cholesterol, triglyceride, LDL-cholesterol, albumin, ALT, total oxidant status and MDA but negatively correlated with glubolin and TAR in obese subjects. In normal participants, it was not related to BMI, blood pressure, cholesterol, LDL-cholesterol, albumin, glubolin, TAR and TOS but was positively correlated to triglycerides, ALT and MDA. More comprehensive study for understanding the relationships between ROS in obesity to cause cell damage may greatly improve our ability to develop interventions in decreasing oxidative stress in obese individuals [19]. Nutritional strategies to improve total antioxidant response (TAR) may be effective in lowering risk of the toxic effect of ROS. Increase in homocysteine and DNA damage may lead to hyperglyceremia, hyperlipidemia, and hyper liver enzyme levels. We need to eradicate these adverse effects in our population in order to have healthy nation.
References
Kumar J, Sunkishala RR, Karthikeyan G, Sengupta S (2007) The common genetic variant upstream of INSIG2 gene is not associated with obesity in Indian population. Clin Genet 71:415–418
Bessesen DH (2008) Update on obesity. J Clin Endocrinol Metab 93:2027–2034
Hossain P, Bisher K, EI-Nahas M (2007) Obesity and diabetes in the developing world—a growing challenge. N Engl J Med 356:973
Haslam DW, James WP (2005) Obesity. Lancet 366:1197–1209
Anonymous (2006) Working together for health. World Health Organization, Geneva
Dudeja V, Misra A, Pandey RM, Devina G, Kumar G, Vikram NK (2001) BMI does not accurately predict overweight in Asian Indians in northern India. Brit J Nutr 86:105–112
Scott JM (2000) Homocysteine and cardiovascular risk. Am J Clin Nutr 72:333–334
Donald WJ (2000) Hyperhomocysteinemia and oxidative stress time for a reality check? Arterioscler Thromb Vasc Biol 20:1182–1184
Kanani PM, Sinkey CA, Browning RL, Allaman M, Knapp HR, Hayness WG (1999) Role of oxidant stress in endothelial dysfunction produced by experimental hyperhomocyst(e)inemia in humans. Circulation 100:1161–1168
Alla R, Friedrich I, Ben-Amotz A, Levy Y (2002) Low plasma antioxidants and normal plasma B vitamins and homocysteine in patients with severe obesity. IMAJ 4:590–593
Henning BF, Tepel M, Riezler R, Gillessen A, Doberauer C (1998) Vitamin supplementation during weight reduction—favourable effect on homocysteine metabolism. Res Exp Med 198:37–42
Dandona P, Mohanty P, Ghanim H, Aljada A, Browne R, Hamouda W, Prabhara A, Afzal A, Garg R (2001) The suppressive effect dietary restriction and weight loss in the obese on the generation of reactive oxygen species by leukocytes, lipid peroxidation, and protein carbonylation. J Clin Endocrinol Metab 86:355–362
Fridovich I (1998) Oxygen toxicity: a radical explanation. J Exp Biol 219:1203–1209
Sondike SB, Copperman N, Jacobson MS (2003) Effects of a low-carbohydrate diet on weight loss and cardiovascular risk factor in overweight adolescents. J Pediatr 142(3):253–258
Grundy SM (2007) Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 28:629–636
Bruckert E, Giral PRecziu V, Poynard T, Champan MJ, Opolon P, Turpin G (2002) A constellation of cardiovascular risk factors is associated with hepatic enzyme elevation in hyperlipidemic patients. Metabolism 51:1071–1076
Erel O (2005) A new automated colorimetric method for measuring total oxidant status. Clin Biochem 38:1103–1111
Erel O (2004) A novel automated method to measure total antioxidant response against potent free radical reactions. Clin Biochem 37:112–119
Prazny M, Skrha J, Hilgertova J (1999) Plasma malondialdehyde and obesity: is there a relationship? Clin Chem Lab Med 37:1129–1130
Martin FL, Cole KJ, Williams JA, Millar BC, Harvey D, Weaver G, Grover PL, Phillip PH (2000) Activation of genotoxins of DNA-damage species in exfoliated breast milk cells. Mutat Res 470:115–124
Steel RGD, Torrie JH, Dickey DA (1997) Principles and procedures of statistics, 3rd edn. McGraw Hill Book Co. Inc., New York
He Q, Ding ZY, Fong DYT, Karlberg J (2000) Blood pressure is associated with body mass index in both normal and obese children. Hypertension 36:165–170
Jafar TH, Chaturvedi N, Pappas G (2006) Prevalence of overweight and obesity and their association with hypertension and diabetes mellitus in an Indo-Asian population. Can Med Assoc J 175(9):1071–1077
Burns CJ, Boswell JM, Olsen GW (1996) Liver enzymes activity and body mass index. J Occup Environ Med 38:1248–1252
Choi JW (2003) Association between elevated serum hepatic enzyme activity and total body fat in obese humans. Ann Clin Lab Sci 33(3):256–264
Acknowledgments
These studies were supported by Higher Education Commission, Punjab Government and University of Agriculture, Faisalabad. Ethical Committee is thanked for permission to carry out this work. Lab staff and Departmental statistician are thanked for their assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bukhari, S.A., Rajoka, M.I., Nagra, S.A. et al. Plasma homocysteine and DNA damage profiles in normal and obese subjects in the Pakistani population. Mol Biol Rep 37, 289–295 (2010). https://doi.org/10.1007/s11033-009-9686-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-009-9686-0