Abstract
In the past 50 years, an ethical-legal boundary has been drawn between treatment and research. It is based on the reasoning that the two activities pursue different purposes. Treatment is aimed at achieving optimal therapeutic benefits for the individual patient, whereas the goal of scientific research is to increase knowledge, in the public interest. From this viewpoint, the patient’s experience should be clearly distinguished from that of a participant in a clinical trial. On this premise, two parallel and mutually exclusive regimes have been established. Yet in the case of deep brain stimulation (DBS), this presentation is a poor fit, for both the patient’s lived experience and medical practice and research. The frictions may be explained by the specificities of the treatment (including surgery and medical devices) and of the pathologies concerned (chronic and evolutive), and by the characteristics of the medical team implementing the treatment. These particularities challenge the dominant frame of reference in medical bioethics and cause difficulties for the current legal framework in fulfilling its dual role: to protect patients while supporting the development of innovative treatments. The dominant model is still the clinical trial for medication safety and legal requirements of drug market regulation. However, DBS forces us to reflect on a medical device that is permanently implanted in the brain by highly specialized multi-disciplinary neurosurgical teams, for the treatment of chronic evolutive diseases. These devices demand fine-tuning on a case-by-case basis and there is still a lot to discover about why DBS is effective (or not). As a result, the wall between treatment and research is osmotic: many discoveries are made incidentally, in the course of treatment. The following study begins with these observations, and suggests that we review legal provisions (especially in French and United States law) so that they are better adapted to the first-person needs and experience of the patient undergoing brain stimulation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the late 1970s, the paradigm separating research and care has prevailed in ethics and biomedical law (US National Research Act 1974; Rapport Belmont 1979; French Loi Huriet-Sérusclat 1988; WMA Declaration of Helsinki 1964/2011). In order to better organize activities and protect persons, legislators acknowledged a need to distinguish between therapeutic actions aimed at relieving or treating the patient, taken as an individual, as opposed to research endeavors, which are mainly pursuing progress in knowledge about the body and its functions and dysfunctions, for the good of humanity as a whole (Thouvenin 2009, 2012; Largent et al. 2011; Kimmelman 2015). Separate legal regimes have been designed (French Loi Jardé 2012, 2016, US Code of Federal Regulations 2009). They enjoin health-care providers to inform patients likely to consent to treatment or to participate in a clinical trial in a clear and distinct manner. Yet studies of the perceptions and motivations of the participants in these trials showed that confusion persisted between research and treatment (Appelbaum et al. 2004). This is notably the case for deep brain stimulation (DBS). It was shown again recently, in exploring the reasons for consent of patients who participated in DBS trials (Leykin et al. 2011; Christopher and Dunn 2015). Even though the information they had received met the regulatory requirements for the expression of informed consent, many of them cited the direct benefits they expected from the procedure as their reason for participation. This finding might firstly be interpreted as an indication that they were not sufficiently informed. Indeed, there is room for improvement in this area: the hospital’s obligation to have the patient sign a consent form is sometimes disguised as an administrative injunction, to forestall the risk of legal proceedings. Forgetting the purpose of the legal provision, which is to ensure the full understanding of the patient, hospital routine sometimes turns into a pre-constitution of evidence (French Cour de cassation 2009; Vialla 2013). However, the case of DBS raises the possibility that the trial participants’ confusion may be the sign of something else.
In this regard, it should be noted that the patients’ mix-up reflects a certain reality of DBS practices. Examples can be found in the history of this high-tech innovation (Gardner 2013) as well as in its current development (Hariz 2012, 2014; Nicolaidis 2017). Is this an example of a dangerous “mixture of purposes,” which should be condemned as unethical? Might it not be the sign of a specificity, prompting us to reconsider the dynamics of the care and research regimes in a new light? In this article, we suggest exploring the second possibility. Such an approach is justified by several circumstances. Primarily, the characteristics of this treatment and the pathologies concerned deserve attention. As we will see in the first part of this paper, it is a highly complex, technological and invasive treatment, requiring two surgical procedures to position two kinds of implants (electrodes in the brain and a neurostimulator in the infraclavicular space, with wires to connect both of them) for the relief of symptoms of a chronic and evolutive disease (mainly neurological or psychiatric). In the unique context created by these features, DBS appears to be both an experimental tool and a treatment option, often of last resort. The second set of circumstances we would like to consider are those arising from more general changes in the context: a gradual recognition that medical devices must be differentiated from medications, on the one hand; and the rise of the “translational” and “personalized” medicine paradigms, on the other. In the second part of the article, we suggest that the confluence of these factors and tendencies should be examined carefully for the purpose of showing that the ethical and legal separation between research and care is deeply challenged. In this view, it might be useful to rethink the current legal framework to better adapt it to the particularities of the disease and the treatment, and especially to the patient’s needs and experience. The potential need to tailor regulations to patient experience is explored with caution, stressing the specificities of DBS, in the last part of the article.
DBS: a medical treatment device and an experimental tool
DBS is a complex therapeutic approach, involving medical and surgical procedures and active implantable medical devices. It is designed to stimulate areas at different depths in the brain with electrical current, using implanted electrodes which are connected to a device resembling a cardiac pacemaker via subcutaneous wires tunneling under the scalp and down the neck to the pulse generator (or “brain pacemaker”), surgically implanted in the infraclavicular pocket. As a result, DBS requires specialized medical skills: neurosurgical know-how supported by brain-imaging techniques and a stereotactical guidance system, and the use of active devices which exert a physical effect on the organism. A complex net of legal rules and technical standards is applied to this multi-faceted reality, to stipulate the obligations to be respected. The guidelines for performing the medical and surgical procedures mirror the provisions of medical and bioethical law (applied to both public hospitals and private clinics, implying guidelines for and justification of the medical prescription and the medical procedure performed, but also liability, etc.). Product safety and efficacy are regulated by the legislation on marketing medical devices. The first set of standards and rules is chiefly made up of deontological and legal norms, derived from national or state law (Code de la santé publique français), whereas standards and norms for product safety and efficacy are mainly technical and regulatory, and come from the supranational or federal level (the US Food and Drug Administration; European Union Directives and Regulations 1990, 2017). However, in addition to the problem of discriminating between factors related to the surgical procedure and those related to the medical device, defining a status to be conferred on implanted patients turns out to be especially delicate. There are many different types of reasons for this awkwardness. Essentially, they are connected to the characteristics of DBS which make it a “mosaic device” (Fins 2012): simultaneously a last-resort treatment and remarkable experimental instrument. The need to fine-tune the device and determine the best target for each symptom and each patient creates the potential to discover more about brain function. The fact that in most cases, patients are awake during surgery also makes it possible to perform “live testing” on the links between certain parts of the brain, certain motor actions and abilities, and certain emotional states (Mulroy et al. 2017). Secondly, distinctions are blurred due to the specificities of the pathologies concerned, combining neurology and psychiatry (Moutaud 2009). These are long-term, evolutive or degenerative, disabling illnesses, at an advanced stage or in a treatment-resistant form for which no safe and effective alternative really exists. Most of the time, unlike what occurs in clinical drug trials (especially in phase I), the only candidates for an implant trial are the patients themselves. Often, they have already experienced decades of suffering and treatment (Clausen 2010).
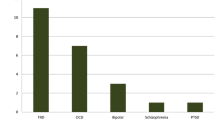
To complete the description of the peculiar situation of DBS, some important elements, regarding the development of this innovative treatment, shall be recalled. In general, the connection between research and treatment is often presented as a chronological continuum, starting with a period during which a concept is developed, and ending with the clinical routine, after going through market-approval process when a product undergoes trials to prove it is safe and effective (Unterrainer and Oduncu 2015). Yet, the history and recent developments in DBS tell a different story—although some introductions to scientific articles about DBS are misleading. True, if read superficially, the history of DBS may fit with the continuity narrative. Indeed, it is often said that a ground-breaking discovery occurred in 1987, thanks to the French neurosurgeon Alim-Louis Benabid, for the treatment of patients with Parkinson’s disease (Benabid 2003). This seems to have been followed by a series of studies that confirmed the effectiveness of DBS in PD. After that, DBS was considered for the treatment of other neurological disorders (essential tremor, dystonia, or Alzheimer’s, for example) and as a psychiatric treatment (especially for obsessive–compulsive disorder (OCD), resistant depression, and substance addiction). However, the sociohistorical facts are more complex than this linear outline indicates. As John Gardner shows, this medical and technological innovation draws on older sources (in particular, Wilder Penfield’s “Montreal procedure,” pioneered in the 1930s). Very early on, it was used as a psychiatric treatment (Gardner 2013; Gardner and Williams 2015). A variety of agents played roles: neurosurgeons, psychiatrists, neurologists, cardiac pacemaker manufacturers, etc. John Gardner is careful to point out that treatment advanced hand-in-hand with knowledge, and vice-versa. Just as with other active implantable devices, DBS development required an experiential learning process, as attested by the importance of “case reports” in the literature on the subject (Bell et al. 2009). Hence, incidental discoveries gave rise to the idea that DBS might be used to treat problems like OCD, addiction, or memory disorders (Bell et al. 2009; Clausen 2010; Hariz 2012; Moutaud 2009, 2014; Foley 2015). For this treatment, case reports played such a decisive role that a claim has been made to demand more systematic and centralized publication of findings, including findings on individual patients or on very small cohorts (Schlaepfer and Fins 2010). This key element is not only relevant to understand the past of DBS development. It still applies. Many case reports are still being published in professional journals; for example, to notify of an unexpected result of the treatment (Wolf et al. 2017). They can lead to a non-randomized clinical study on a small cohort to determine “proof of concept” (Deuschl et al. 2013; Morishita et al. 2014), and/or motivate the design of a randomized, controlled clinical trial. As Blank observes, “while the line dividing experimentation from therapy is often a fine one in medicine generally, it nearly disappears here” (Blank 2013). One important reason for this merger between treatment and experimentation is due to the fact that until recently, this type of brain surgery was perceived as being so risky and costly it could only be performed as a last resort. Moreover, as already mentioned, the characteristics of the DBS device make it “ideal for experimental purposes” (Hariz 2012; Foley 2015; Moutaud 2016). The best brain target, the best contact for the electrodes, and the best tuning are decided on a case-by-case basis, creating opportunities to discover more about the brain and its functioning with each patient. Finally, DBS does have the great virtue of being a “reversible” technology (Benabid 2003), although over the long term implantation and stimulation cause an adaptation of the brain, the consequences of which are still largely unknown. The “nature of the claimed reversibility” may be discussed, and long term effects of DBS may occur (Mundale 2016), but the stimulation can always be stopped, and the electrodes and neurostimulator can be explanted. From this standpoint, DBS is much safer and more reassuring than neuroablative lesion surgery, which has been and still is a competing treatment option (Lévêque 2013).
All these characteristic elements create a unique situation regarding the articulation between research and care. Besides, the atypicality of this situation has been acknowledged by official bioethics commissions (Comité consultatif national d’éthique 2002, 2013; Nuffield Council on Bioethics 2013). Nevertheless, few consequences have been drawn from this acknowledgement and little specific regulatory action has been taken as a result. For example, ethical papers often proceed as though there is a clear distinction between established DBS applications such as treating PD, and experimental applications focused on its use in psychiatric contexts. In this view, research on DBS is about resistant depression, cocaine addiction, or memory enhancement, whereas DBS for neurological diseases is only a daily routine clinical option. However, in addition to the fact that the opposition between neurology and psychiatry is debatable (Synofzik et al. 2011; Synofzik 2013), it is also problematic to neglect ongoing research in neurology, including research on treating Parkinson’s disease (Foley 2015). The fact that the authorities in charge of the medical-device approval process have recognized DBS as an effective treatment for certain neurological diseases (chiefly for Parkinson’s disease) leads to an interpretative bias. Although positive results from clinical trials (some of which involved large cohorts) made it possible for the US FDA to approve DBS medical devices as effective treatments for Parkinson’s disease, and for the European Union to define them as certified active medical devices, no explanation for this effectiveness has been provided. Much remains to be discovered about its causal mechanisms (Amadio et al. 2011; Kringelbach et al. 2011; Hariz 2012, 2014). Moreover, research continues, to determine the best targets in the brain, to shed light on problems related to undesirable side effects (speech difficulties, suicidal tendencies, behavioral disorders, etc.) or to improve the equipment (longer-lasting batteries, electrodes that could target zones more accurately, or closed-loop technology) (Hariz 2014; Rosin et al. 2011; Gunduz et al. 2017). Research also continues in an effort to better identify the patient population concerned. Currently, PD patients often undergo the implant when the disease is in its later stages and drugs are no longer effective in regulating dopamine levels and the motor disorders correlated to them. A European clinical study showed that it might be beneficial to apply DBS at an earlier stage of the disease, when the “honeymoon phase” of drug therapy is over and patients are again disturbed by motor dysfunction (Deuschl et al. 2013; Deuschl and Agid 2013). However, this study aroused real controversy (Azulay 2013; Hariz 2013; Mestre et al. 2014; Schüpbach et al. 2014). The debate reached a climax when a US team obtained approval to go even further, and initiate DBS treatment before medication-resistant motor fluctuations (“off times”) appear (Charles et al. 2014; Hacker et al. 2015; Hariz 2015). Clearly, neither experimental research nor ethical and scientific controversies are limited to the field of psychiatric treatment. Although the acquisition of official agency approval or notified body certification requires evidence from clinical trials and a regulatory evaluation of safety and effectiveness (with the exception of special situations, such as exemptions granted for humanitarian reasons: Fins et al. 2011), it does not mean that research ceases. Even if a device has been approved (US) or certified (EU), it may still be subjected to experimentation, research, and trials. In particular, this is likely to be the case if a device is used to treat a condition that is not specified by the agency authorization or certification (“off-label use”). In other words, randomized, controlled clinical trials do not account for all of the research conducted on human subjects, and psychiatry is not the only experimental field in DBS. This is why, in theory, the legal protection of the human subjects participating in medical experimentation is conceptually distinct from the laws governing regulatory clinical trials (phases I, II, III). Logically, the ethical or legal requirements that have been formulated to regulate research on human beings should apply to every situation in which new findings are likely to be drawn from the results observed. As for treatments, if deontological principles are applied strictly, only those that have been fully tested shall be administered (Déontologie des médecins et des infirmiers, Code de la santé publique français articles R.4312-10, R.4127-14, R.4127-39). In the case of DBS, it is clearly difficult to reconcile theoretical principles with practical realities. It would be inappropriate to classify all DBS patients as participants in research (Copeland 2013). The opposite attitude, to ignore the fact that research continues within the context of treatment, is also inappropriate. As a result, it seems to be advisable to question whether the separation between research and treatment, as conceptualized and established by regulation, makes sense for patients undergoing DBS.
Challenging the ethical and legal separation between treatment and research
Whereas the patient’s experience bridges care and research, the regulatory structure places law regulating research alongside the laws governing industrial innovation and commercial approval. Although they are conceptually separate, legislation aimed at protecting people participating in research and the regulations regarding commercialization of health care products are historically connected. The expressions “biomedical research” and “research involving human subjects” are broader than “clinical trials.” Nevertheless, “clinical trial” law is the standard used as a reference for regulating and implementing biomedical research and research involving human beings. This can be explained chiefly by the precision of the norms stipulated for clinical trials. They create an “already there” effect, as well as a benchmark for fields where standardization occurred later or less precisely. Moreover, the two legislations suffer from the same “original sin”: their strong ties to pharmaceutical industry interests and practices (Thouvenin 2009). Drug market regulation was used as a model for medical-device market regulation, despite the fact that the standards of reference for drugs did not necessarily fit medical devices (Gardner 2013; Adèle and Desmoulin-Canselier 2016). For example, the distinction between testing for safety and evaluating effectiveness raises some problems when the procedure involves implanting a medical device in a person’s brain. Likewise, the “gold standard” (Timmermans and Berg 2003) of the double-blind study is difficult to apply, because it involves performing sham surgery or sham stimulation; i.e., either in simulating a surgical procedure for some of the participants in the trial, or activating the device for only some of the participants. Certain specialists are convinced a double-blind study is needed to meet the requirements of evidence-based medicine and evaluate the extent of the placebo effect (Horng and Miller 2015). But they are opposed by others who are convinced that this methodological option is ethically unsound (Dekkers and Boer 2001) and, moreover, almost impossible to set up, because the patients would perceive the effect of the electricity, and the difference between ON and OFF states (Hariz 2013; Schüpbach et al. 2014). As a result, the US FDA and the European regulatory agencies elaborated more flexible evaluation criteria, based on the medical teams’ expertise and know-how (Gardner 2013). However, the problem raised by the drug clinical-trial model remains. In fact, some recent failures in attempts to treat resistant depression gave rise to intense debate over the possible need to abandon the “gold standard” and replace it with the “adaptive” clinical trial (Fins et al. 2017). This “alternative model” would make it possible to proceed by selecting patients who respond well to the treatment from the initial cohort, gathering them in a new cohort in order to shed light on the reasons why it was effective for them, and defining targets and adjustments more precisely. After that, it would be possible to re-test the experimental treatment on the rest of the original cohort.
The regulatory authorities might follow up on this proposal for future standards. However, at the moment, the clinical trial designed for marketing medication is still the prevailing reference. Yet it is not the majority practice. Several reasons may explain this. Firstly, device manufacturers obviously have an economic interest in organizing trials that will enable them to obtain certification or market approval for a new device or an already existing one for a new use. Conversely, it is substantially less advantageous for them to undertake an investigation to determine why a treatment is effective, or to identify the possible side effects of various adjustments. In the case of DBS, however, there is a significant need for knowledge about these questions. As a consequence, such studies are instigated either by a research institution in a clinical study on small cohorts with a more flexible design (an open-label trial), or they are carried out within the context of treatment. This is because the cost of organizing any research involving human subjects is burdensome, due to the clinical-trial model which dictates that the studies be structured in such a way as to meet evidence-based medicine criteria, and which implies multi-sites studies be organized, in order to gather a patient cohort large enough to withstand statistical analysis. By contrast, organizing smaller studies and, especially, publishing case reports, appears to be a simple and less restrictive way to produce more knowledge. As a result, case reports still have a long future ahead of them. Sometimes, they serve as a preliminary, spurring the organization of subsequent randomized tests. They may also stand on their own (although a case report meets only the lowest criteria as evidence, according to the French High Authority for Health). “Incidental discoveries” or “observations” described by case reports occurred within the context of treatment, even though in the field of DBS, case reports are one of the main motors driving knowledge. Case reports challenge the ethical and legal barrier between research and treatment. As we mentioned in the introduction to this paper, patients have trouble understanding this separation, probably because it does not fit their experience. The patient’s first-person experience, with DBS or waiting for it, is above all a treatment experience (the experimental nature of which is more or less clear depending on the situation): expecting relief, being admitted by a health care team, obtaining physical and financial access to treatment, etc. Even when patients are willing to submit to the constraints of the double blind and sham stimulation, studies show that they expect a treatment that will improve their condition, sooner or later (Strauss et al. 2014; Deuschl et al. 2014; Fins et al. 2014). Indeed, even in this context, where everything should make them aware that the purpose of the procedure is scientific/regulatory instead of medical, they are told that if they are part of the control group which does not receive the innovative treatment, they will receive DBS after the trial ends (Schüpbach et al. 2014). It is therefore understandable that DBS might serve as a topic example of “translational treatment.” Contrary to a certain usage of the “translational medicine” concept, let us make it clear that the point here is not to turn all patients and all physicians, regardless of pathology or specialty, into research subjects and researchers. When the “translational medicine” concept is not only used to support an overall program reinforcing the ties between research and care, but is also implemented to accelerate approval processes and invalidate current legislation, it is undoubtedly controversial (Canselier 2015). In the context of DBS, however, this nexus between research and treatment corresponds to realities experienced by patients. In that case, “translational medicine” is not a political platform, but a daily experience. This type of medical practice is already institutionalized to some extent in France, where a network of Centres d’Investigation Clinique has been organized. Unsurprisingly, the Institut du Cerveau et de la Moelle Epinière (Brain and Spinal Cord Institute), a key player in French DBS research, is one of the clinics engaged in “treatment and investigation” (Moutaud 2010). Conversely, the fact that this nexus has an impact on patient experience has not yet been sufficiently examined.
However, any change in this field would be illegitimate if it were not justified by ethical and/or practical considerations related to the protection of patient interests. In terms of ethics, objections seem to arise immediately. The ethical principles applied to research are supposed to be radically different from those governing treatment. Yet where DBS is concerned, an overview of the literature dedicated to applied ethics for the protection of people undergoing neurostimulation does not lead to such a conclusion. The same conceptual resources are present: the principles of non-malfeasance, of beneficence, of personal autonomy, and of benefit-vs-risk analysis (Bell et al. 2009, 2011; Clausen 2010; Kim 2013; Synofzik and Schlaepfer 2011; Cabrera et al. 2014; Synofzik 2013, 2015; Unterrainer and Oduncu 2015; Foley 2015). The authors admit that the persons to whom these principles are applied are themselves in a situation to be simultaneously patients and participants in research. As a result, the criteria of therapeutic value, of the absence of alternative treatment, or the “last-resort” option, classically associated with the field of medical ethics, are mobilized to support reflection on the ethics of DBS research. If the literature on neuroethics has trouble formulating distinct conceptual frameworks, does it fare any better with practical considerations? Does the reality of practice provide justification for maintaining the current framework, or on the contrary, for amending it, in this specific case?
Before going further with this reflection, we must point out that the purpose of this article is not to do away with the distinction between research and treatment as a whole. To rule out such an argument, one need only cite the well-known ethical catastrophes of World War Two. On principle and globally, the distinction remains fundamentally legitimate. In the field of DBS and elsewhere, it is undeniably valuable in that it causes (or is likely to cause) an increased awareness in practitioners. Likewise, the fact that the ethics of research protocol methods are subject to evaluation by an independent committee is another virtuous achievement of research law. Nevertheless, to serve the ultimate purpose of providing maximal protection for the rights and interests of the patient, it could be productive to consider the possibility that specific arrangements might be devised for certain situations. In this case, the point is to comply with the patients’ needs, experiences, and wishes as closely as possible, and to face up to the realities that resist regulatory injunctions.
DBS can be considered not only as a translational medical practice, but even a form of “personalized” medicine (Fins 2015). This expression refers mainly to individualized treatment, which is usually considered in terms of genomic medicine, in which patients would be treated according to their genetic particularities (OPECST 2014). There is no doubt, however, that DBS treatment is “tailored to the individual patient” (Strauss et al. 2014). It is also a “precision” treatment, because each disease, each stage of the disease, and each patient require specific device tuning and/or specific targets in the brain. The observation that each patient is his own reference point and that each treatment program can be adapted to individual needs, using the same technology, fits the criteria defining precision medicine. The concept of “personalized” medicine also appears to reflect a concern that the patient be placed at the center of medical attention (even if some thinkers see an opposition between patient-centered medicine, based on individualized treatment, and “personal medicine,” aimed at the patient-doctor relationship) (Guchet 2016). It is true that the care and coverage provided for patients who are either candidates for DBS or already implanted attests that efforts have been made to personalize the procedure. Health-care teams are now staffed differently: initially limited to the neurologist, neurosurgeon, and the nurses, the team has gradually expanded to integrate other skills, to some degree, depending on the country and the institution (Moutaud 2014, 2016; Gardner and Williams 2015). In France, patients are now systematically entitled to consult a psychiatrist prior to deciding to undergo the surgery, and often there is a psychologist on the staff of the healthcare team, to assess and follow up patients before and after surgery. Sometimes a specialist in nutrition or some other field the patient may feel is helpful in dealing with the disease is also part of the staff. Certain teams (for example, the University of Montreal Health Centre psychiatric unit neuromodulation team) provide counseling to find solutions to personal problems (financial aid, housing, driver’s license, etc.) which could be obstacles to an improvement in the patient’s condition. Therefore, in this case, the experimental nature of the treatment does not conflict in any way with the hospital’s mission to provide social assistance (as defined by the French national committee on bioethics, the Comité consultatif national d’éthique français: CCNE 2007).
Approaching DBS as a “personalized” treatment is also a way to acknowledge the fact that DBS research has evolved to integrate not only the individual specificities of the human brain, but also the complexity of the diseases treated, in terms of patient experience. Unexpected DBS side effects, whether they are judged interesting or disturbing, have contributed to revealing the osmosis between the neurological and psychiatric sides of the diseases. Even with Parkinson’s disease, it is becoming clear that each patient develops differently, and that the perception of the disease plays a role in its development (Hariz and Hamberg 2013; Hariz et al. 2016; Mathers et al. 2016; Sperens et al. 2017). Recent publications show that research success criteria are based primarily on considerations related above all to treatment. There is ample evidence that the perioperative period is decisive for the effectiveness of the treatment, but also for discovering ways to improve success rates; for example, for patient selection. The choice between sedation versus wakefulness during the surgical procedure can also be explored on the basis of patient experience (Mulroy et al. 2017). The next step that some doctors are ready to make is to redefine proof-of-effectiveness criteria based on patient satisfaction or feedback (Agid et al. 2006; Schüpbach et al. 2006; Hariz and Hamper 2013; Hariz et al. 2016). This highlights the active role of the patients, in research as well as in treatment. As John Gardner and Clare Williams sum it up, innovative and responsible research in the field “requires the generation of robust evidence, which depends upon the ability of clinicians and researchers to measure clinical improvements that patients themselves find meaningful” (Gardner and Williams 2015).
Should regulations be tailored to patient experience?
Will this new arrangement find an expression in the legal sphere, regarding legal status of patients or rules applying to them? A few recent general changes to French legislation may lead to this trend. For instance, a recent change in the title and wording of the law regarding biomedical research was interpreted as a sign that the legislation recognized the active role played by the participant. Indeed, the law no longer speaks of “research on human subjects,” but “with” them (Thouvenin 2012). The impact of such change on the legal framework, on the organization of research and on the protection of human rights is not yet clear. As regards DBS, recognizing a reconfiguration of the connection between treatment and research based on patient lived experience could be made even more imperative due to research currently underway and innovations that are in development. In fact, as was mentioned earlier, current research aims not only at investigating the effectiveness of DBS treatment for a wide spectrum of different disorders, but also at suggesting it could be prescribed for PD patients in earlier stages of the disease, or at implementing new devices allowing ongoing data-transmission and follow-up. In this new perspective, patients who receive implants earlier will be monitored for a longer time (Strauss et al. 2014). The closed-loop technology, thanks to connected electrodes, would allow healthcare teams to have a more complete collection of data about each patient brain and to modulate the treatment depending on his ou her specific needs (Rosin et al. 2011). But it would also make it possible to provide medical and research databases with ongoing brain-function data, to produce greater knowledge. Thus, patients would be called upon to play an active role in enriching research throughout their lives. The person with the DBS implant would still be a patient, but perhaps it is time to recognize that, in a variety of ways and even when he or she is not participating directly in a clinical trial, he or she is also contributing to a knowledge accretion process. From this perspective, the approach consisting in making informed consent to a medical procedure or for admission to a research protocol the decisive criterion for differentiated legal regimes seems especially reductive (Kim 2013; Unterrainer and Oduncu 2015).
At this point, we can wonder about the practical implications, for these patients, of the legal dichotomy between care and research. For example, is it so relevant to organize two different regimes regarding information? It is true that the double-blind trial situation presents significant particularities, in terms of the need to inform patients of the fact that some of them will not be receiving electrical stimulation. On the other hand, it would seem useful for all the patients to know that even when they are not participating in a clinical trial, the treatment being offered to them varies in effectiveness depending on the individual, and is still largely unexplained, and that each procedure is likely to give rise to incidental discoveries. Whether or not they are participants in a formal, regulated research trial, they are still patients, who need to be informed as thoroughly as possible about the unknowns of the treatment offered to them. The information content could therefore be adapted to a variety of situations, as long as it fulfills the requirement that it be complete and understandable. Instead of a standardized informed-consent form, drafted according to a general model, referring only to treatment or research, and responding to concerns that proof be easy to provide in case of lawsuit, wouldn’t it be more relevant to define a principle that patients be informed on a case-by-case basis, as part of the core of basic rights to which each patient is entitled? If a person receives a type of treatment that is likely to give rise to incidental discoveries, isn’t he or she also entitled to that information? French jurisprudence does not mention this last point, but it has already set stringent standards for informing patients who receive an innovative treatment. The French supreme administrative court has stated that “when healthcare providers prescribe an examination, treatment, or preventive procedure for which the risks cannot be fully evaluated on the date of the medical visit, in particular because the procedure is recent and has only been implemented with a limited number of patients, the patient is entitled to be informed both of any normally foreseeable frequent or serious risks that have already been identified, and of the fact that the existence of other risks cannot be ruled out, due to a lack of perspective” (Conseil d’État 4e et 5e chambres réunies, 10 mai 2017, requête no. 397840). Nevertheless, in French law today, there are textual differences regarding the way information is transmitted and the kind of proof needed to verify that it has been transmitted. The legal requirement for a signed form for risky interventional research alone has no clear grounds in the field of patient needs, or in that of de facto customs making the signature a systematic, non-individualized formality. Similarly, is it satisfactory to make consent (to a medical procedure or to admission to a research protocol) a formality that instantly sums up ethical and legal concerns, whereas patient consent is something that should be sought throughout the process, by a clear explanation that the patient can decide at any time to withdraw from the trial, to cease the treatment, to request an explantation of a device, or to refuse that data produced by his or her treatment be used in a scientific publication? Unlike the issues of insurance and liability, the specificity of the requirement for information cannot be cited to maintain a separation between the regime for research and the one for treatment.
According to current law in many Western countries, the separation between the legal regimes regulating treatment and research is also likely to create difficulties for a DBS patient. For example, a person who has had access to regular monitoring and attentive support while participating in research (Strauss et al. 2014) may feel a breach in the provision of care when the clinical trial ends. The principle in both France and the United States is that the proponent and sponsor of the research must guarantee long-term follow-up for participants. This is coherent with the overall goal of medical regulation to ensure continuity in care (Code de déontologie médicale, article R.4127-47 du Code de la santé publique français). Nevertheless, current organizational practices in both countries do not make it possible to ensure a smooth transition between the period of the clinical trial and its aftermath. Patients in the US expressed negative feelings about their experience during trials on DBS implants as treatment for resistant depression. According to accounts they published online (http://neurocritic.blogspot.fr/2014/01/broaden-trial-of-dbs-for-treatment.html; http://278-005.blogspot.fr/), certain patients were allegedly no longer monitored when the trial ended (prematurely). Patients may encounter the same difficulties with other types of treatment, but DBS raises specific complexities related to the need not only to provide a safe post-operative follow-up but also to tune and adapt the device (to avoid serious side effects) and to replace the battery (or to monitor the external charger). Generally speaking, an overly rigid administrative and legal division between research and treatment may hinder conditions ensuring treatment continuity and maintaining the regular service necessary for the proper and optimal operation of the medical device. One gets the impression that, for these patients, the transition from research to treatment (or even shuttling back and forth several times between the two) led to a breach in continuity, because the regulatory framework for research is not designed to guarantee continuity. The fact that financial coverage for the device differed depending on whether the patient undergoing the implant was a participant in a clinical trial sponsored by a manufacturer, a participant in a clinical study of an innovative procedure initiated by a hospital team, or a patient undergoing treatment is likely to present a serious obstacle to patients. Even within the French social system, known for the broad scope of the coverage it provides, expenses are not always optimally covered. Sometimes they are covered fully by the research proponent, sometimes they are covered totally or partially in a lump-sum payment by the national health insurance system (“Forfait innovation”: article L. 165-1-1 Code de la sécurité sociale: Mascret 2015; Paubel 2015), and sometimes they are covered by the national health insurance system as routine care. Obtaining EU certification, the end result of a lengthy procedure, does not automatically qualify a treatment for coverage by the healthcare insurance system. This coverage is contingent on an assessment of the service provided, carried out by other agencies (in France: CNEDIMTS or HAS, followed by registration on the hospital purchasing or reimbursement roster, qualifying the treatment for coverage on the basis of hospital services). In the United States, FDA approval for a product does not guarantee health insurance coverage for it (Doros 2010). It is only one of several necessary prerequisites. The Centers for Medicare and Medicaid Services independently determine whether a procedure or product qualifies for coverage and reimbursement, according to a non-uniform regional policy. In both legal systems, different regimes coexist, and their impermeability causes anxiety, delays, and bureaucratic obstacles. For patients, this is hard to understand. For DBS patients, it is even more abstruse. Why would there be any difference, since they themselves can see the device is the same, and the same teams perform the surgery? Indeed, a de facto limitation exists on the teams that are qualified to implement a high-tech treatment like DBS, due to the skills required to perform surgery, and also to the pluridisciplinarity needed for neuromodulated patient evaluation and follow-up. For PD patients, the development of DBS as routine clinical treatment enables the technology to spread beyond university hospitals, and it arouses concerns about the ability of smaller care facilities to provide the support necessary (Bell et al. 2011). However, in France, most of the time, patients are still implanted and followed-up in the same university hospital unit and by the same team. Moving means relocating in an area where a similar hospital team is at work.
Moreover, device manufacturers have blamed the complex patchwork of national health coverage regulations for being a factor in hindering patient access (in France, especially) to innovative medical devices (APIDIM/SNITEM 2016). Obviously, the claims of manufacturers, who are too often inclined to protest the supposed unfairness of regulations, must be taken with a grain of salt. The point of this paper is not to contest the fact that it is appropriate to make manufacturers bear the financial burden of clinical trials, nor is it to contest the need to have a different procedure for the evaluation of treatments and devices depending on the purpose of the evaluation (safety, social insurance coverage, etc.). However, it seems important to spare the patient any uncomfortable discontinuity in care, due to different organizational arrangements and divisions of responsibility for costs and coverage. Certain legal systems have made some changes to optimize coverage conditions (France has instituted the “Forfait Innovation,” as well as the “single agreement” in article L. 1121-6 du Code de la santé publique). Ideally, a patient should have only one insurance interlocutor. Although progress has been made, the efforts to achieve this goal have not sufficed, and coverage is still patchy. An optimal legal framework would organize rules in order to spare the patients the negative consequences of difference between the legal regimes—one for products and procedures that are undergoing clinical trials prior to licensing for sale, and one for those concerned by clinical studies aimed not at approval, but at treatment. Whether the patient is a participant in clinical research, or the beneficiary of an innovative medical device (certified as safe, but not yet listed as one of the products reimbursed by national health), or a patient undergoing “routine care” (likely to give frequent rise to incidental discoveries), his or her legal status and protection should ideally be the same. Similarly, better protection should be provided regarding liability suits. According to current laws in France and in the US, if the participant in a clinical trial wishes to file a lawsuit, he or she sues the legal proponent that sponsored the trial. In France, it is only when the trial proponent’s liability cannot be engaged that the plaintiff can file with the national medical accident compensation office [Office national d’indemnisation des accidents médicaux (ONIAM) (articles L.1121-10, L.1126-7 et L.1142-1 et L. 1142-3 du Code de la santé publique)]. Why not arrange for systematic compensation by the ONIAM, via a reserve fund managed by the ONIAM but financed by sponsors, in the case of damages caused by biomedical research?
The ideas developed in this article are aimed primarily at eliciting greater awareness and discussion. Unlike certain position papers (Sacristan 2015), we do not suggest a general reorganization. We only make comments and proposals based on findings and observations concerning DBS. Our assumption is that these suggestions may be sound for other similar situations, when patients suffering from a chronic, disabling and/or degenerative disease are treated thanks to an innovative technology which requires highly specialized teams ensuring the continuity between research and care, and between care and research. It might, for example, be applicable for diabetic patients treated with an implantable insulin pump. However, such similarities must still be investigated. For DBS-implanted patients, at least, and probably for other patients, there is a need for legal solutions that more convincingly account for the complicated nexus of medical practice and patient lived experience. The real issues at stake are notably: providing patients with the fullest and most understandable individual information about the treatment, its unknowns, and its risks, as well as the way medicine and the progress of medical knowledge function; acknowledging the patient’s active and decisive role in the success of both treatment and research, the certainty that the patient understands he or she is entitled to refuse a procedure or withdraw from a research program at any time; and the need for an effective principle of continuity of treatment for the patient, regardless of any kinks in the legal/bureaucratic machinery.
Conclusion
The characteristics of DBS make it an instrument of personalized and translational medicine. In patient lived experience, it means having access to an innovative technology, benefiting from care from a highly skilled, multidisciplinary team, with long-term, regular follow-up often in the same university hospital and by the same team. Even when this treatment has already been fully certified, approved for the market, and/or registered on the list of treatments that are covered by the national health insurance system, there is a room for discovery and innovation. Small clinical trials, incidental findings, and case reports may be valuable as a means of learning more about human brain, the effectivenesss of DBS, and how it can be fine-tuned for optimal results. Consequently, any patient receiving the treatment, even for a well-known indication like Parkinson’s disease, is likely to be a source of new findings that advance medical research. As for people who participate in clinical trials, they are all patients hoping that their symptoms will be relieved by DBS, in the short or medium term. A clinical trial is always limited by a time frame, whereas the chronic disease affecting these patients demands long-term care. Therefore, the temporality of clinical trials differs from that of both treatment and research. The opposition between research and care existing in current regulatory frameworks is a poor fit with patient experience. For the patient, the barriers built into these systems may even create hurdles that interfere with the continuity of care. Without claiming to contest the relevance and need for manufacturers sponsoring clinical trials to finance both the trials and to assume the liability for any harm to patients that may occur as a result, this study wonders about the possibility of designing solutions that are better fitted to the needs of DBS patients.
References
Adèle, Paul-Anthelme, and Sonia Desmoulin-Canselier. 2016. Droit des dispositifs médicaux: Vers une réforme ou un simple réaménagement? Revue de Droit Sanitaire et Social 5: 930–942.
Agid, Y., M. Schüpbach, M. Gargiulo, L. Mallet, I. L. Houeto, C. Behar, D. Maltete, V. Mesnage, and M.-L. Welter. 2006. Neurosurgery in Parkinson’s disease: The doctor is happy, the patient less so? Journal of Neural Transmission Supplementa 70: 409–414.
Amadio, Jordan P., and Nicholas M. Boulis. 2011. Practical considerations in the ethics of parkinsonian deep brain stimulation. AJOB Neuroscience 2: 24–26.
APIDIM/SNITEM. 2016. Faire de la France un modèle pour l’accès à l’innovation des dispositifs médicaux. Recommandations issues d’une analyse comparée des stratégies spécifiques de l’accès au marché des dispositifs médicaux innovants. http://www.snitem.fr/sites/default/files/snitem-apidim_recommandations-2016.pdf. Accessed 22 Dec 2017.
Appelbaum, P. S., C. W. Lidz, and T. Grisso. 2004. Therapeutic misconception in clinical research: Frequency and risk factors. IRB 26 (2): 1–8.
Azulay, J. P. 2013. Neurostimulation des noyaux sous-thalamiques: Mieux vaut tôt que jamais! Revue Neurologique 169: 283–284.
Bell, Emily, Racine Mathieu and Eric Ghislaine. 2009. Preparing the ethical future of deep brain stimulation. Surgical Neurology 72: 577–586.
Bell, Emily, Bruce Maxwell, Mary Oat McAndrews, Abbas Sadikot, and Eric Racine 2011. Deep brain stimulation and ethics: Perspectives from a Multisite qualitative study of Canadian neurosurgical centers. World Neurosurgery: December 76 (6): 537–547.
Belmont Report. 1979. The Belmont Report: Ethical principles and guidelines for the protection of human subjects of research. http://www.hhs.gov/ohrp/humansubjects/guidance/belmont.html. Accessed 22 Dec 2017.
Benabid, Alim-Louis. 2003. Deep brain stimulation for Parkinson’s Disease. Current Opinion in Neurobiology 13: 696–706.
Blank, Robert H. 2013. Intervention in the Brain. Politics, Policy, and Ethics. Cambridge: MIT Press.
Cabrera, Laura Y., Emily L. Evans, and Roy H. Hamilton. 2014. Ethics of the electrified mind: Defining issues and perspectives on the principled use of brain stimulation in medical research and clinical care. Brain Topography 27: 33–45.
Canselier (Desmoulin-Canselier), Sonia. 2015. Recherche et médecine “translationnelles”: Questions juridiques à propos d’un programme de politique scientifique. Cahiers Droit, Sciences et Technologies 5: 61–73.
Charles, D., P. E. Konrad, J. S. Neimat, A. L. Molinari, M. G. Tramontana, and S. G. Finder, et al. 2014. Subthalamic nucleus deep brain stimulation in early stage Parkinson’s disease. Parkinsonism and Related Disorders 20: 731–737.
Christopher, Paul P., and Laura B. Dunn. 2015. Risk and consent in neuropsychiatric deep brain stimulation: An exemplary analysis of treatment-resistant depression, obsessive-compulsive disorder, and dementia. In Handbook of Neuroethics, eds. J. Clausen, and N. Levy, 2, 589–605. Dordrecht: Springer.
Clausen, Jens. 2010. Ethical brain stimulation: Neuroethics of deep brain stimulation in research and clinical practice. European Journal of Neuroscience 32: 1152–1162.
Comité Consultatif National d’Éthique pour les Sciences de la Vie et de la Santé. 2002. Avis n° 71: La neurochirurgie fonctionnelle d’affections psychiatriques sévères. Paris. http://www.ccne-ethique.fr/fr/publications/avis-sur-la-neurochirurgie-fonctionnelle-daffections-psychiatriques-severes#.WftPn2jWw2w. Accessed 22 Dec 2017.
Comité Consultatif National d’Éthique pour les Sciences de la Vie et de la Santé. 2013. Avis n° 122: Recours aux techniques biomédicales en vue de « neuro-amélioration » chez la personne non malade: Enjeux éthique. Paris. http://www.ccne-ethique.fr/sites/default/files/publications/ccne.avis_ndeg122.pdf. Accessed 22 Dec 2017.
Comité Consultatif National d’Éthique pour les Sciences de la Vie et de la Santé (CCNE). 2007. Avis n° 101:Santé, éthique et argent: Les enjeux éthiques de la contrainte budgétaire sur les dépenses de santé en milieu hospitalier. Paris. http://www.ccne-ethique.fr/sites/default/files/publications/avis101.pdf. Accessed 22 Dec 2017.
Copeland Samantha, M. 2013. Problems with seeing Deep Brain Stimulation recipients primarily as research subjects. AJOB Neuroscience 4 (2): 50–52.
Dekkers, W., and G. Boer. 2001. Sham neurosurgery in patients with Parkinson’s disease: Is it morally acceptable? Journal of Medical Ethics 27: 151–156.
Deuschl, Günter, Yves Agid. 2013. Subthalamic neurostimulation for Parkinson’s disease with early fluctuations: Balancing the risks and benefits. The Lancet Neurology 12: 1025–1034.
Deuschl, Günter, Michael Schüpbach, Karina Knudsen, O. Marcus Pinsker, Philippe Cornu, JörnRau, Yves Agid, and Carmen Schade-Brittinger. 2013. Stimulation of the subthalamic nucleus at an earlier disease stage of Parkinson’s disease: Concept and standards of the EARLYSTIM-study. Parkinsonism and Related Disorders 19: 53–61.
Doros, Gerald. 2010. FDA approval does not mean what you think it does! Journal of Invasive Cardiology 22 (8): 382–384.
European Directive 90/385/EEC of 20 June 1990 on Active implantable medical devices. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A31990L0385. Accessed 31 July 2017.
European Regulation 2017/745 of 5 April 2017 on Medical devices. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32017R0745. Accessed 31 July 2017.
Fins, Joseph J. 2012. Deep brain stimulation as a probative biology: Scientific inquiry & the mosaic device. American Journal of Bioethics-Neuro Science 3 (1): 4–8.
Fins, Joseph J. 2015. Devices, drugs, and difference: Deep brain stimulation and the advent of personalized medicine. In Handbook of Neuroethics, eds. J. Clausen, and N. Levy, 2, 607–620. Dordrecht: Springer.
Fins, Joseph J., and Zachary E. Shapiro. 2014. Deep brain stimulation, brain maps and personalized medicine: Lessons from the human genome project. Brain Topography 27: 55–62.
Fins, J. J., H. S. Mayberg, B. Nuttin, C. S. Kubu, T. Galert, V. Strum, K. Stoppenbrink, R. Merkel, and T. E. Schlaepfer. 2011. Neuropsychiatric deep brain stimulation research and the misuse of the humanitarian device exemption. Health Affairs 30 (2): 302–311.
Fins, J. J, C. S. Kubu, H. S. Mayberg, Reinhard Merkel, Bart, Nuttin, and T. E. Schlaepfer. 2017. Being open minded about neuromodulation trials: Finding success in our “failures”. Brain Stimulation 10 (2): 181–186.
Foley, Paul. 2015. Deep brain stimulation for Parkinson’s disease: Historical and neuroethical aspects. In Handbook of Neuroethics, eds. J. Clausen, and N. Levy, 2, 561–587. Dordrecht: Springer.
French Cour de cassation. 2009. Chambre criminelle, 24 février 2009, pourvoi numéro 08-84.436. https://www.legifrance.gouv.fr/affichJuriJudi.do?idTexte=JURITEXT000020358473. Accessed 22 Dec 2017.
French Loi Huriet-Sérusclat. 1988. Loi n° 88-1138 du 20 décembre 1988 relative à la protection des personnes qui se prêtent à des recherches biomédicales. Journal officiel de la République Française. https://www.legifrance.gouv.fr/jo_pdf.do?id=JORFTEXT000000508831. Accessed 22 Dec 2017.
French Loi Jardé. 2012. Loi n° 2012-300 du 5 mars 2012 relative aux recherches impliquant la personne humaine. https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000025441587&categorieLien=id. Accessed 22 Dec 2017.
French Loi Jardé modifiée. 2016. Ordonnance n° 2016-800 du 16 juin 2016 relative aux recherches impliquant la personne humaine et décret n° 2016-1537 du 16 novembre 2016. https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000032719520&categorieLien=id. Accessed 22 Dec 2017.
Gardner, John. 2013. A history of deep brain stimulation: Technological innovation and the role of clinical assessment tools. Social Studies of Science 43 (5): 707–728.
Gardner, John, Clare Williams. 2015. Responsible research and innovation: A manifesto for empirical ethics? Clinical Ethics 10 (1–2): 5–12.
Guchet, Xavier. 2016. La Médecine personnalisée. Un essai philosophique. Paris: Les belles lettres/Médecine & sciences humaines.
Gunduz, Aysegul, K.D. Foote, and S. Okun Michael. 2017. Reengineering deep brain stimulation for movement disorders: Emerging technologies. Current Opinion in Biomedical Engineering. https://doi.org/10.1016/j.cobme.2017.09.001.
Hacker Mallory, L., James Tonascia, Maxim Turchan, Amanda Currie, Lauren Heusinkveld, Peter E. Konrad, Thomas L. Davis, Joseph S. Neimat, Fenna T. Phibbs, Peter Hedera, Lily Wang, Yaping Shi, David M. Shade, Alice L. Sternberg, Lea T. Drye, and David Charles. 2015. Deep brain stimulation may reduce the relative risk of clinically important worsening in early stage Parkinson’s disease. Parkinsonism and Related Disorders 21:1177–1183.
Hariz, Marwan. 2012. Twenty-five years of deep brain stimulation: Celebrations and apprehensions. Movement Disorders 27 (7):930–933.
Hariz, Marwan. 2013. Early surgery for Parkinson’s disease? Maybe, but not just yet. The Lancet Neurology 12:938–939.
Hariz, Marwan. 2014. Deep brain stimulation: New techniques. Parkinsonism and Related Disorders 20:S192–S196.
Hariz, Marwan. 2015. There is no credible rational for deep brain stimulation in very early Parkinson’s disease! Parkinsonism and Related Disorders 21: 345–346.
Hariz, G.-M., and K. Hamberg. 2013. Perceptions of living with a device-based treatment: An account of patients treated with deep brain stimulation for Parkinson’s disease. Neuromodulation. https://doi.org/10.1111/ner.12073.
Hariz, Gun-Marie, Patricia Limousin, Katarina Hamberg. 2016. “DBS means everything – for some time”. Patients’ perspectives on daily life with deep brain stimulation for Parkinson’s disease. Journal of Parkinson’s Disease. https://doi.org/10.3233/JPD-160799.
Horng, Sam, and Franklin G. Miller. 2015. Ethics of sham surgery in clinical trials for neurologic disease. In Handbook of Neuroethics, eds. J. Clausen, and N. Levy, 2, 1125–1138. Dordrecht: Springer.
Kim Scott, Y.H. 2013. Competence for informed treatment and research. In Neuroethics in Practice. Medicine, Mind, and Society, eds. A. Chatterjee, and M. J. Farah, 83–95. New-York: Oxford University Press.
Kimmelman, Jonathan, Spencer Philipps Hey. 2015. Clinical translation in central nervous system diseases: Ethical and social challenges. In Handbook of Neuroethics, eds. J. Clausen, and N. Levy, 2, 1107–1124. Dordrecht: Springer.
Kringelbach, Morten L., and Tipu Z. Aziz. 2011. Neuroethical principles of deep brain stimulation. (commentary). World Neurosurgery 76 (6): 518–519.
Largent, Emily, Steven Joffe, and Franklin Miller. 2011. Can research and care be ethically integrated? The Hastings Center Report 41 (4): 37–46.
Lévêque, Marc. 2013. Psychochirurgie. Paris: Springer.
Leykin, Y., P. P. Christopher, P. E. Holtzheimer, P. S. Appelbaum, H. S. Mayberg, and S. H. Lisanby, and L. B. Dunn. 2011. Participants’ perceptions of deep brain stimulation research for treatment-resistant depression: Risks, benefits, and therapeutic misconception. AJOB Primary Research 2:33–41.
Mascret, Caroline. 2015. Les nouvelles règles juridiques de la prise en charge de l’innovation des technologies en santé par l’assurance maladie. Petites Affiches 77 (17 avril 2015): 4–7.
Mathers, J., C. Rick, C. Jenkinson, R. Garside, H. Pall, R. Mitchell, S. Bayliss, and L. L. Jones. 2016. Patients’ experiences of deep brain stimulation for Parkinson’s disease: A qualitative systematic review and synthesis. BMJ Open. https://doi.org/10.1136/bmjopen-2016-011525.
Mestre, Tiago A., Alberto J. Espay, Connie Marras, Mark H. Eckman, Pierre Pollak, and Anthony E. Lang. 2014. Subthalamic nucleus-deep brain stimulation for early motor complications in Parkinson’s Disease: The EARLYSTIM Trial: Early is not always better. Movement Disorders 29 (14):1751–1756.
Morishita, Takashi, Sarah M. Fayad, Masa-aki Higuchi, Kelsey A. Nestor, and Kelly D. Foote. 2014. Deep brain stimulation for treatment-resistant depression: Systematic review of clinical outcomes. Neurotherapeutics 11 (3): 475–484.
Moutaud, Baptiste. 2009. C’est un problème neurologique ou psychiatrique ? Ethnologie de la stimulation cérébrale profonde appliquée au trouble obsessionnel compulsif. Université Paris Descartes.
Moutaud, Baptiste. 2010. L’implantation de la recherche clinique à l’hôpital en France. Histoire de la création des centres d’investigation clinique ». Médecines/Sciences 26 (7): 768–771.
Moutaud, Baptiste. 2014. Pour le bien de tous et l’intérêt de chacun. Essai clinique et innovation organisationnelle en psychochirurgie. Sciences Sociales et Santé 3 (32): 43–68.
Moutaud, Baptiste. 2016. Neuromodulation technologies and the regulation of forms of life: Exploring, treating, enhancing. Medical Anthropology: 35: 1–17.
Mulroy, Eoin, Nigel Robertson, Lorraine MacDonald, Arnold Bok and Simpson Mark. 2017. Patients’ perioperative experience of awake deep-brain stimulation for Parkinson disease. World Neurosurgery 105: 526–528.
Mundale, Jennifer. 2016. Reversibility and deep brain stimulation. Journal of Cognition and Neuroethics 3 (4): 97–111.
Nicolaidis, Stylianos. 2017. Neurosurgery of the future: Deep brain stimulations and manipulations. Metabolism Clinical and Experimental 69: 16–20.
Nuffield Council on Bioethics. 2013. Novel neurotechnologies: intervening in the brain. http://nuffieldbioethics.org/wp-content/uploads/2013/06/Novel_neurotechnologies_report_PDF_web_0.pdf. Accessed 22 Dec 2017.
Office parlementaire des choix scientifiques et techniques. 2014. Les progrès de la génétique: vers une médecine de précision ? Les enjeux scientifiques, technologiques, sociaux et éthiques de la médecine personnalisée. Paris. http://www.senat.fr/rap/r13-306/r13-306_mono.html. Accessed 22 Dec 2017.
Paubel, Pascal. 2015. Forfait innovation: Un dispositif de financement des dispositifs médicaux perfectible. Journal de Droit de la Santé et de l’Assurance Maladie 1: 62–65.
Rosin, Boris, Maya Slovik, Mitelman Rea, Michal Rivlin-Etzion, Suzanne Haber, Zvi Israel, Eilon Vaadia, and Hagai Bergman. 2011. Closed-loop deep brain stimulation is superior in ameliorating Parkinsonism. Neuron 72 (2): 370–384.
Sacristan, José. 2015. Clinical research and medical care: Towards effective and complete integration. BMC Medical Research Methodology 15: 53–65.
Schlaepfer, Thomas E., and Joseph.J. Fins. 2010. Deep brain stimulation and the neuroethics of responsible publishing: When one is not enough. Journal of the American Medical Association 303 (8): 775–776.
Schüpbach, M., M. Gargiulo, M.-L. Welter, L. Mallet, C. Béhar, I.-L. Houeto, D. Maltête, V. Mesnage, and Y. Agid. 2006. Neurosurgery in Parkinson disease: A distressed mind in a repaired body? Neurology 66: 1811–1816.
Schüpbach, Michael W.M., Jörn Rau, Jean-Luc Houeto, Paul Krack, Alfons Schnitzler, Carmen Schade-Brittinger, Lars Timmerman, and Günter Deuschl. 2014. Myths and facts about the EARLYSTIM Study. Movement Disorders 29 (14): 1742–1750.
Sperens, Maria, Katarina Hamberg, and Gun-Marie Hariz. 2017. Are patients ready for “EARLYSTIM”? Attitudes towards deep brain stimulation among female and male patients with moderately advanced Parkinson’s disease. Parkinson’s Disease. https://doi.org/10.1155/2017/1939831.
Strauss, Ido, Suneil Kalia, and Andres Lozano. 2014. Where are we with surgical therapies for Parkinson’s disease? Parkinsonism and Related Disorders 20S1: 187–191.
Synofzik, Matthis. 2013. Functional neurosurgery and deep brain stimulation. In Neuroethics in Practice. Medicine, Mind, and Society, eds. A. Chatterjee, and M. J. Farah, 189–208. New-York: Oxford University Press.
Synofzik, Matthis. 2015. Ethical implications of brain stimulation. In Handbook of Neuroethics, eds. J. Clausen, and N. Levy, 2. 553–560. Dordrecht: Springer.
Synofzik, Matthis, Thomas E. Schlaepfer. 2011. Electrodes in the brain-ethical criteria for research and treatment with deep brain stimulation for neuropsychiatric disorders. Brain Stimulation 4 (1): 7–16.
Thouvenin Dominique. 2009. Commentaire de l’article L. 1121-1 du code de la santé publique. In Code de la santé publique commenté, ed. F. Dreifuss-Netter, 43–55. Paris: Litec.
Thouvenin, Dominique. 2012. La loi n° 2012 – 300 du 5 mars 2012: Des recherches pratiquées sur la personne aux recherches avec la personne. Revue de Droit Sanitaire et Social 5: 787–799.
Timmermans, Stefan, Marc Berg. 2003. The Gold Standard: The Challenge of Evidence-Based Medicine and Standardization in Health Care. Philadelphia: Temple University Press.
Unterrainer, Marcus, Fuat S. Oduncu. 2015. The ethics of deep brain stimulation. Medicine Health Care and Philosophy 18: 475–485.
US Code of Federal regulations. 2009. Title 45: Public Welfare Department of Health and Human Services, Part 46: Protection of Human Subjects. Washington: US Department of Health and Human Subjects. Revised January 15, 2009 Effective July 14, 2009. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html. Accessed 22 Dec 2017.
USA National Research Act. 1974. Public Law 93–348 (July 12, 1974) To amend the Public Health Service Act to establish a program of National Research Service Awards to assure the continued excellence of biomedical and behavioral research and to provide for the protection of human subjects involved in biomedical and behavioral research and for other purposes. https://history.nih.gov/research/downloads/PL93-348.pdf. Accessed 15 Nov 2017.
Vialla, François. 2013. De quelques questions posées par l’administration de la preuve de l’information due au patient. Petites Affiches 112: 16–22.
Wolf, Marc E., Mahmoud Abdallat, Christian Blahak, and Joachim K. Krauss. 2017. Pathological crying induced by deep brain stimulation of the subthalamic nucleus in Parkinson’s disease. Journal of Clinical Neuroscience 45: 159–161.
Funding
This research was funded by the NormaStim ANR 14-CE30-0016-01 program with the support of the French National Research Agency (Agence Nationale de la Recherche).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Desmoulin-Canselier, S. Patient’s lived experience with DBS between medical research and care: some legal implications. Med Health Care and Philos 22, 375–386 (2019). https://doi.org/10.1007/s11019-018-9859-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11019-018-9859-5