Abstract
Polymorphisms in the human dopamine transporter (DAT) are associated with bipolar endophenotype. Based on this, the acute inhibition of DAT using GBR12909 causes behavioral alterations that are prevented by valproate (VAL), being related to a mania-like model. Herein our first aim was to analyze behavioral and brain oxidative alterations during a 24 h period post-GBR12909 to better characterize this model. Our second aim was to determine the preventive effects of lithium (Li) or VAL 2 h post-GBR12909. For this, adult male mice received GBR12909 or saline being evaluated at 2, 4, 8, 12 or 24 h post-administration. Hyperlocomotion, levels of reduced glutathione (GSH) and lipid peroxidation in brain areas were assessed at all these time-points. GBR12909 caused hyperlocomotion at 2 and 24 h. Rearing behavior increased only at 2 h. GSH levels decreased in the hippocampus and striatum at the time points of 2, 4, 8 and 12 h. Increased lipid peroxidation was detected at the time-points of 2 and 12 h in all brain areas studied. At the time-point of 2 h post-GBR12909 Li prevented the hyperlocomotion and rearing alterations, while VAL prevented only rearing alterations. Both drugs prevented pro-oxidative changes. In conclusion, we observed that the main behavioral and oxidative alterations took place at the time-period of 2 h post-GBR12909, what points to this time-period as the best for the assessment of alterations in this model. Furthermore, the present study expands the predictive validity of the model by the determination of the preventive effects of Li.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent episodes of disturbed affect including mania and depression are core features of bipolar disorder (BD). Brain functions, such as cognition, seems to be impaired during the acute phases of BD, especially during manic states (Morice 1990; Martinez-Aran 2004).
Manic episodes include a variety of complex and multifaceted symptoms that challenges the clinician’s diagnosis. These symptoms include hyperactivity, euphoric or irritable mood, psychotic symptoms, decreased need for sleep, hyperverbosity and hypersexuality among others (Goodwin and Jamison 2007). Despite the aetiology and pathophysiology of mania remain unclear, one core neurobiological alteration of this mood state is the increased dopaminergic drive (Berk et al. 2007). The changes in dopaminergic drive between BD mania and depression are described as dopamine (DA) dysregulation syndrome (Berk et al. 2007).
Based on the hyperdopaminergic state underlying mania some animal models were developed. One example is the d-amphetamine model that is acknowledged as the “gold standard” model of mania (Young et al. 2011a). This model brought important evidences regarding the implication of DA, oxidative stress, neurotrophins and mitochondrial alterations in the neurobiology of mania (Frey et al. 2006b; Valvassori et al. 2010). Remarkably, oxidative stress is being implicated in the pathophysiology as well as neuroprogression of BD (Berk et al. 2011).
D-amphetamine-induced mania was first proposed by the co-administration of chlordiazepoxide-dexamphetamine (Davies et al. 1974) and thereafter by the administration 1.5 mg/kg d-amphetamine (Cappeliez and Moore 1990). Recently, this model is facing restrictions due to the high potential for abuse of d-amphetamine (Rush et al. 2001) which is limiting the acquisition of this drug for research purposes. As an attempt to ensure the maintenance of this model we recently proposed the use of lisdexamfetamine dimesylate (LDX), a prodrug of d-amphetamine (Macedo et al. 2013).
Earlier this decade, the model of mania induced by the acute administration of GBR12909 [1-{2-[bis-(4-fluorophenyl)methoxy]-ethyl}-4-(3-phenylpropyl)piperazine] was proposed (Young et al. 2010). To date, the face validity of this mania model was evaluated by the determination of hyperlocomotion immediately after GBR12909 administration (Young et al. 2010). The predictive validity of the model was determined by the use of the mood stabilizing drug valproate (VAL) (van Enkhuizen et al. 2013a).
GBR 12909 is a high affinity, long-acting DA transporter (DAT) inhibitor with a rapid onset of action. This drug is metabolically converted in humans to its close related analog GBR 12935 (Brown and Chand 2010), a drug also known as a DAT inhibitor (Andersen 1987). Importantly, the GBR12909-induced model of mania is based on the putative aetiology of BD, in which polymorphisms in the human DAT have been associated with the bipolar endophenotype (Greenwood et al. 2006; Pinsonneault et al. 2011). Conversely, mice generated through genetic deletion of DAT (DAT-KO) (Barr et al. 2004) or with reduced DAT functioning (DAT-KD) (Young et al. 2011b) exhibit hyperdopaminergic tone and hyperlocomotion resembling BD mania.
As previously mentioned, insights from the preclinical model of mania induced by amphetamine points to an important role of oxidative stress in this phenomenon. In fact decreased levels of the antioxidant glutathione (GSH) and increased lipid peroxidation were previously observed in putative brain areas related to mania, i.e. prefrontal cortex, hippocampus and striatum (Frey et al. 2006a, b; Macedo et al. 2013). Furthermore, prevention and treatment of the behavioral alterations induced by d-amphetamine by antioxidant drugs, such as alpha-lipoic acid, were demonstrated (Macêdo et al. 2012).
To date, as far as we know, no study was performed in order to determine the time course of behavioral and brain oxidative alterations induced by the acute administration of GBR12909. Thus, our main goal was to determine the time-related, within 24 h, behavioral and brain oxidative alterations induced by GBR12909. This will contribute to a further characterization of this animal model bringing new evidences to its face and construct validity. Our second aim was to determine the preventive effect of the mood stabilizing drug lithium (Li) in this model, since no previous study was conducted with the end.
Methods
Drugs
GBR12909 dihydrochloride (Sigma, St. Louis, USA), sodium valproate (VAL; Life Pharmaceutical Company) and lithium carbonate (Li; Sigma, St Louis, USA) were used. The drugs were made up freshly within 1–2 h of dosing. All other chemicals used were of analytical grade.
Animals
The experiments were performed in adult male Swiss mice (weighting: 20–25 g) obtained from the Animal House of Federal University of Ceará. The animals were group-housed maximum of 8 per cage in standard polycarbonate cages (42 × 20.5 × 20 cm) and standard environmental conditions (22 ± 1 °C; humidity 60 ± 5 %; 12-h light/dark cycle with lights on at 7:00 am) with access to food (Laboratory Rodent Diet - LabDiet®) and water ad libitum. All experimental procedures were conducted between 8:00 and 14:00 h by raters blinded to the experimental groups. The methods were carried out in accordance with the NIH Guide for the Care and Use of Laboratory Animals (NIH 1996) and the Brazilian College of Animal Experimentation (COBEA). The local ethical committee of Federal University of Ceará approved this research protocol.
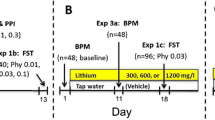
Study design
The mice were randomly divided into experimental groups (8–15 animals/group). The first experiment consisted in determining the time-related locomotor and oxidative alterations induced by GBR12909. To do this, distinct animals received a single intraperitoneal (i.p.) injection of GBR12909 (10 mg/kg) or saline (controls) and were evaluated at different time-points after administration i.e. 2, 4, 8, 12 or 24 h. The dose of GBR12909 was adopted from previous studies showing hyperlocomotion and a mania-like behavioral phenotype (van Enkhuizen et al. 2013a).
After the behavioral determinations the animals were decapitated and the brain areas prefrontal cortex (PFC), hippocampus (HC) and striatum (ST) dissected for neurochemical determinations of oxidative stress parameters.
In the second experiment the mood stabilizing drugs Li (47.5 mg/kg, i.p., twice a day) or VAL (200 mg/kg, i.p.) were administered to determine the predictive validity of the model. In this protocol each group of animals received Li, VAL or saline during 3 days and 30 min after received GBR12909. Two hours after GBR12909 administration the behavioral and oxidative alterations were evaluated. Controls received only saline.
In the case of Li and VAL the decision of using only one dose of each drug was based on: previous preclinical reports showing antimanic effect of these drugs in the model of mania induced by d-amphetamine (da-Rosa et al. 2012) and the need to reduce the use of laboratory animals.
In the present study our primary outcome was to determine the time-course of behavioral and oxidative changes induced by GBR12909. The secondary outcome was to determine the effects of the mood stabilizing drugs, Li or VAL in the prevention of GBR12909-induced alterations.
Behavioral determinations
Open-field test
The locomotor activity was assessed using the open-field test (Archer 1973). This test was performed in a 30 × 30 cm open field surrounded by 50 cm high walls made of acrylic. The floor of the open field was divided into nine equal parts by black lines. The apparatus was placed in a red light room. The animals were gently placed on the center of the field and allowed to freely explore the arena for 5 min. Crossings of the black lines (used to determine horizontal activity) and rearing behavior (used to determine vertical activity) were counted, during the 5 min period, by experienced raters who were blinded to treatment.
Neurochemical determinations
Tissue preparation
Brain tissue samples were homogenized (10 times (w/v) with ice-cold 0.1 M phosphate buffer (pH 7.4). The homogenates were centrifuged at 10,000 rpm for 15 min, and aliquots of supernatants were separated and used for determination of oxidative stress parameters.
Reduced glutathione (GSH) levels
Reduced glutathione levels were evaluated to estimate endogenous defenses against oxidative stress. The method was based on Ellman’s reagent (DTNB) reaction with free thiol groups (Ellman 1959). The brain areas were diluted in EDTA 0.02 M buffer (10 % w/v) and added to a 50 % trichloroacetic acid solution. After centrifugation (3000 rpm/15 min), the supernatant of the homogenate was collected and mixed with 0.4 M tris–HCl buffer, pH 8.9 and 0.01 M 5,5-dithiobis (2-nitrobenzoic acid (DTNB). The yellow color product was read immediately at 412 nm using a spectrophotometer (Beckman coulter UV/Visible). Results were calculated based on a standard glutathione curve and are expressed as μg of GSH/g wet tissue.
Lipid peroxidation
Lipid peroxides formation was analyzed by measuring the thiobarbituric-acid reacting substances (TBARS) in the homogenates (Ohkawa et al. 1979) as an index of reactive oxygen species (ROS) production. The samples were mixed with 1 mL of trichloroacetic acid 10 % (TCA) and 1 mL of thiobarbituric acid 0.67 % (TBA), then heated in a boiling water bath for 15 min and immediately kept cold in a bath of ice. Lipid peroxidation was determined by the absorbance at 532 nm. Results are expressed as μmol of malonaldehyde (MDA)/g tissue.
Statistical analysis
Statistical analysis was performed with GraphPad Prism 6.0 for Mac, GraphPad Software (San Diego, CA, USA). The results of the time related behavioral and neurochemical alterations induced by GBR12909 were analyzed by regular two-way ANOVA with “time” and “group” as factors. Two-way ANOVA followed by Sidak’s multiple comparison test was used for comparisons between control and GBR12909 groups at different time points whereas Tukey’s multiple comparisons test was used for comparisons between different time-points inside each respective group (control or GBR12909). The behavioral and neurochemical effects of Li and VAL were evaluated by one-way ANOVA followed by Tukey’s multiple comparisons test. All results are expressed as means ± S.E.M (standard errors of the mean). Before ANOVA, D’Agostino-Pearson omnibus test was conducted to verify the normal distribution of the data. For all analyses, the significance level was set at α = 0.05.
Results
Time course of behavioral and oxidative alterations induced by GBR 12909
Hyperlocomotion associated with increased rearing are important behavioral phenotypic alterations frequently evaluated in animal models of mania (Macedo et al. 2013). In this context, herein, two-way ANOVA of the number of crossings (Fig. 1, top panel) revealed a significant “time” × “group” interaction [F (4, 83) = 6.755, P < 0.0001] with significant main effects of “time” [F (4, 83) = 7.214, P < 0.0001] and “group” [F (1, 83) = 50.83, P < 0.0001]. Post hoc tests showed that the animals submitted to a single administration of GBR12909 presented a significant increase in the number of crossings at the time points of 2 (P < 0.0001) and 24 h (P < 0.0001) post-GBR12909 when compared to each respective control. The increase in the number of crossings at the time points of 2 and 24 h was also confirmed by its statistical significance when compared to the time points of 4 (P < 0.01), 8 (P < 0.05) and 12 h (P < 0.01) post-GBR 12909.
Number of crossings (top panel) and rearings (bottom panel) in the open field test of the animals administered 10 mg/kg GBR 12909 and evaluated at the time points of 2, 4, 8, 12 and 24 h post drug administration. Bars represent mean ± SEM of the number of crossings or rearings (n = 8–12 animals per group for each time point). * P ≤ 0.05 versus control at each respective time point according to two-way ANOVA followed by Sidak’s multiple comparisons test, $, &,+ P ≤ 0.05 versus GBR12909 group at the time points of 4, 8 and 12 h, respectively, according to two-way ANOVA followed by Tukey’s multiple comparisons test
In the evaluation of rearing behavior (Fig. 1, bottom panel) two-way ANOVA revealed a significant “time” × “group” interaction [F (4, 83) = 4.999, P = 0.0012] with significant main effects of “time” [F (4, 83) = 3.774, P = 0.072] and “group” [F (1, 83) = 24.82, P < 0.0001]. Post hoc analysis showed that the animals subjected to a single administration of GBR12909 presented a significant increase in the number of rearings at the time points of 2 (P < 0.0001) and 24 h (P < 0.05) when compared to control. The greater increase in rearing behavior was observed at the time point of 2 h post-GBR12909 since this result was significant when compared to the time points of 4 (P < 0.01) and 8 (P < 0.01) and 12 h (P < 0.05) post-GBR12909.
Regarding GSH levels in the PFC (Fig. 2 top panel) two-way ANOVA revealed significant main effects of “time” [F (4, 52) = 3.782, P = 0.0090] and “group” [F (1, 52) = 42.36, P < 0.0001]. Post hoc tests showed that in this brain area the levels of GSH significantly decreased at the time points of 8 (P < 0.05), 12 (P < 0.0001) and 24 h (P < 0.01) post-GBR12909 when compared to each respective control. The greater decrease in GSH in the PFC was observed at the time point of 12 h (2 × 12 h - P < 0.01; 4 × 12 h - P < 0.01). In the HC a significant “time” × “group” interaction [F (4, 62) = 4.000, P = 0.0060] with significant main effect of “group” was observed [F (1, 62) = 187.6, P < 0.0001]. In this brain area a reduction in GSH levels was observed at all-time points post-GBR12909 when compared to their respective controls (P < 0.0001). The greater decrease was observed at the time point of 12 h (8 × 12 h – P < 0.01; 12 × 24 h – P < 0.01). In the ST we also observed a significant “time” × “group” interaction [F (4, 60) = 9.371, P < 0.0001] with significant main effects of “time” [F (4, 60) = 13.12, P < 0.0001] and “group” [F (1, 60) = 288.8, P < 0.0001]. Post hoc tests showed that the levels of GSH significantly decreased at the time points of 2, 4, 8 and 12 h post-GBR12909 in respect to the control at each respective time point (P < 0.0001). Similarly to PFC and HC the decrease in GSH levels in the ST was greater at the time point of 12 h post-GBR12909 (2 × 12 h – P < 0.0001; 4 × 12 h – P < 0.05; 8 × 12 h – P < 0.05).
Reduced glutathione (GSH) levels in the prefrontal cortex (top panel), hippocampus (middle panel) and striatum (bottom panel) of control and GBR 12909 treated mice evaluated at the time points of 2, 4, 8, 12 and 24 h post drug administration. Bars represent mean ± SEM of GSH levels (controls n = 6–8 animals for each time point; GBR 12909 n = 8 animals for each time point). * P ≤ 0.05 versus control at each respective time point according to two-way ANOVA followed by Sidak’s multiple comparisons test, #,$,&,% P ≤ 0.05 versus GBR 12909 group at the time points of 2, 4, 8 and 24 h, respectively, according to two-way ANOVA followed by Tukey’s multiple comparisons test
In relation to lipid peroxidation, in the PFC, two-way ANOVA revealed a significant “time” × “group” interaction [F (4, 71) = 21.47, P < 0.0001] with main effects of “time” [F (4, 71) = 20.08, P < 0.0001] and “group” [F (1, 71) = 13.67, P = 0.0004]. Post hoc tests demonstrated significant increases in MDA levels at the time points of 2 (P < 0.0001) and 12 h (P < 0.0001) post-GBR12909 when compared to each respective control. In both time points (2 and 12 h) the increase in lipid peroxidation was significant when compared to the time points of 4, 8 and 24 h (P < 0.0001). A similar situation was observed in the HC and ST. In these brain areas a significant “time” × “group” interaction was observed (HC – [F (4, 62) = 7.245, P < 0.0001], ST – [F (4, 62) = 5.432, P = 0.0008]), with main effects of “time” and “group”. Post hoc analysis revealed significant increases in lipid peroxidation at the time points of 2 (P < 0.01) and 12 h (P < 0.05) in the HC and ST. At the time point of 2 h in both HC and ST the increment in lipid peroxidation was significant when compared to the time points of 4, 8 and 24 h (P < 0.001). At the time point of 12 h the increase was significant when compared to 8 and 24 h (P < 0.01) (Fig. 3).
Lipid peroxidation (determined by MDA equivalents) in the prefrontal cortex (top panel), hippocampus (middle panel) and striatum (bottom panel) of control and GBR 12909 treated mice evaluated at the time points of 2, 4, 8, 12 and 24 h post drug administration. Bars represent mean ± SEM of MDA levels (controls n = 6–8 animals for each time point; GBR 12909 n = 8 animals for each time point). * P ≤ 0.05 versus control at each respective time point according to two-way ANOVA followed by Sidak’s multiple comparisons test, #,$,&,% P ≤ 0.05 versus GBR 12909 group at the time points of 2, 4, 8 and 24 h, respectively, according to two-way ANOVA followed by Tukey’s multiple comparisons test
Prevention of GBR 12909-induced behavioral and pro-oxidative alterations by Li and VAL
The administration of Li significantly prevented the hyperlocomotion observed at the time point of 2 h post GBR 12909 [F(3, 35) = 16.84, P < 0.01]. Nevertheless, VAL did not prevent this behavioral alteration maintaining thus the number of crossings significantly increased when compared to control animals (P < 0.01). The increase in the number of rearings observed 2 h post GBR 12909 was prevented by both mood stabilizing drugs, Li and VAL [F(3, 36) = 8.734, P < 0.01] (Fig. 4).
Number of crossings (a) and rearings (b) of the animals pretreated for 3 days with lithium (Li) or valproate (VAL), administered 10 mg/kg GBR 12909 and evaluated at the time point of 2 h post-GBR12909. Bars represent mean ± SEM of the number of crossings or rearings (n = 6–8 animals/group). a P ≤ 0.05 versus control and b P ≤ 0.05 versus GBR 12909 according to one-way ANOVA followed by Tukey’s multiple comparisons test
Relative to the pro-oxidant alterations induced by GBR 12909 we observed that Li prevented the decrease in GSH levels observed 2 h after GBR 12909 in the HC [F(3, 28) = 8.327, P < 0.05] and ST [F(3, 25) = 6.076, P < 0.05]. The same preventive effect was observed by the preadministration of VAL only in the ST (P < 0.01). Both mood stabilizers significantly prevented the increase in lipid peroxidation observed 2 h after GBR 12909 in the PFC [F(3, 43) = 11.55, P < 0.001], HC [F(3, 30) = 6.176, P < 0.01] and ST [F(3, 34) = 8.764, P < 0.01] (Fig. 5).
Reduced glutathione (GSH) levels (a), and MDA equivalents levels (b) in the prefrontal cortex, hippocampus, and striatum of the animals pretreated for 3 days with lithium (Li) or valproate (VAL), administered 10 mg/kg GBR 12909 and evaluated at the time point of 2 h post GBR 12909. Bars represent mean ± standard error of the mean GSH or MDA levels (n = 6–8 animals/group). a P ≤ 0.05 versus control and b P ≤ 0.05 versus GBR 12909 according to one-way ANOVA followed by Tukey’s multiple comparisons test
Discussion
The data presented here point towards to time related behavioral and brain oxidative alterations induced by the DAT inhibitor GBR 12909. The behavioral alterations were more evident at the time points of 2 and 24 h post-GBR12909. Nevertheless, the oxidative changes were not closely related to the behavioral alterations. In this regard, we observed decreased levels of GSH from the time period of 2 to 24 h post-GBR12909 in some brain areas. On the other hand, increments in lipid peroxidation were observed at the time points of 2 and 12 h post-GBR12909. In the evaluation of the animals pretreated with the mood stabilizing drugs we observed that only Li prevented both the alterations in the number of crossings and rearings. The pretreatment with VAL prevented only the alterations in rearing behavior. Both mood-stabilizing drugs prevented the increase in lipid peroxidation induced by GBR12909, while alterations in HC GSH levels were prevented only by Li administration. Taken together, our results showed that the administration of the DAT inhibitor, GBR12909, is accompanied by brain oxidative alterations, giving, thus, the first evidences for the construct validity of the model. Furthermore, we expanded the predictive validity of the model by the determination of Li preventive effects.
Numerous findings from clinical studies highlight the importance of DAT in BD pathophysiology: i) a single-nucleotide polymorphism (SNP) in the rs27072 affecting DAT mRNA expression and translation was significantly associated with BD (Pinsonneault et al. 2011) as well as the presence of multiple variants in DAT1 was noticed to convey susceptibility to BD (Greenwood et al. 2006); ii) a decrease in DAT mRNA levels was demonstrated in the postmortem frontal cortex of BD patients as compared to healthy controls (Rao et al. 2012) and iii) significant lower DAT availability relative to healthy controls was observed in the bilateral dorsal caudate of unmedicated BD patients that underwent PET imaging with the DAT-selective radiotracer [(11) C]CFT and a structural magnetic resonance imaging (MRI) scan (Anand et al. 2011).
In line with the clinical evidences aforementioned, the DAT-KO mice exhibit hyperdopaminergic tone, increased levels of locomotor activity and highly linearized movement in a novel environment, as well as reduced prepulse inhibition (PPI) of acoustic startle, compared to wild-type littermates (Barr et al. 2004). Additionally, DAT-KD mice exhibit a behavioral profile in the behavioral pattern monitor (BPM) and an increased risk-taking that resembles BD mania when compared to wild-type mice (Young et al. 2011b). The mood-stabilizing drugs VAL (Ralph-Williams et al. 2003) and Li (Beaulieu et al. 2004) attenuated the alterations in locomotor activity observed in DAT-KD animals.
Time–related behavioral and brain oxidative alterations induced by GBR 12909
To date, only a few studies were based on the administration of the DAT inhibitor GBR12909 to induce a mania-like phenotype. In the first study different strains (C57BL/6J and 129/SvJ) of mice were examined during 3 h in a BPM. The results of this study showed that GBR12909 increased the animals’ activity at various doses tested, only 16 and 28.5 mg/kg initially, but also 9 mg/kg throughout the 3 h period of observation. This effect was strain independent (Young et al. 2010). In the second study GBR12909 administration increased motor impulsivity, motivation significantly, and risk preference subtly (van Enkhuizen et al. 2013b). Looking at these studies we can observe that the behavioral alterations induced by GBR12909 were evaluated only within 3 h postadministration (Young et al. 2010).
In our study we tried to expand this time of observation for a 24 h time period. Our results showed that the number of crossings and rearings significantly increased post-GBR12909 at two time points, 2 and 24 h. Noteworthy, the model of mania induced by the repeated administration of d-amphetamine uses the time point of 2 h post d-amphetamine for the conduction of behavioral and neurochemical evaluations (Frey et al. 2006a; Macêdo et al. 2012).
GBR12909 induces a hyperdopaminergic state that results in hyperlocomotion. Indeed, the oxidation of DA by enzymatic or non-enzymatic pathways generates compounds such as superoxide radical anions and quinones. Both ROS and quinones can react unspecifically with many cellular components altering their functionality and, thus, being potentially neurotoxic (Miyazaki and Asanuma 2008; Meiser et al. 2013). Therefore, we can conclude that the increased dopaminergic drive seen in mania causes oxidative imbalance. In line with this evidence, a large body of preclinical (Frey et al. 2006a; Macedo et al. 2013) and clinical studies (Andreazza et al. 2008) supports the role of oxidative stress in BD neurobiology. In this context, in animal models of mania induced by amphetamines, decreases in the antioxidant GSH and increases in lipid peroxidation in brain areas such as PFC, HC and ST are reported (Macêdo et al. 2012; Macedo et al. 2013). Oxidative imbalance is also observed in clinical studies with BD patients (Kuloglu et al. 2002; Raffa et al. 2012). Thus, knowing that DA metabolism itself is strongly linked to oxidative stress (Meiser et al. 2013) and on the importance of oxidative stress to BD (Andreazza et al. 2008) we decided to evaluate the levels of oxidative stress parameters, i.e. GSH and lipid peroxidation. In the present study, the levels of DA itself were not evaluated since DAT inhibition with GBR12909 causes obvious increases in DA levels and oxidative stress is one of the biomarkers of BD staging and neuroprogression (Berk et al. 2011). These oxidative parameters were evaluated in different time points post-GBR12909 and in brain areas related to mood disorders namely PFC, HC and ST (Drevets et al. 2008) aiming to contribute to the construct validity of this mania-like model.
We observed that GBR12909 caused long-term alterations in GSH since decreased levels of this parameter were observed up to 24 h post-GBR12909 in the HC and PFC. Hippocampus and ST were more susceptible to the effects of GBR12909 in reducing GSH levels, because this decrease was observed since the time-point of 2 h post-GBR12909. Regarding lipid peroxidation we observed increased levels of this parameter at the time points of 2 and 12 h post-GBR12909.
Interestingly, in the present study, a relation between increased oxidative imbalance and behavioral alterations was observed only at the time point of 2 h post-GBR12909. Thus, we can suggest that GBR12909 at the dose of 10 mg/kg causes oxidative imbalance, a core alteration observed in BD patients (Frey et al. 2013) and in animal models of mania (Frey et al. 2006a; Macedo et al. 2013), although this imbalance showed no direct relationship with the behavioral alterations induced by the drug (with the exception of 2 h time period post-GBR12909). This hypothesis is strengthened by the results obtained 12 h post-GBR12909. At this time point (12 h) we observed the greater decreases in GSH levels followed by increases in lipid peroxidation, but the absence of locomotor alterations.
As previously mentioned, at the time point of 24 h after GBR12909 we did not observe a direct relation between oxidative stress and hyperlocomotion. Indeed, locomotion is a multifaceted process that cannot be explained by the analysis of one parameter such as oxidative stress. It is possible that the decreases in GSH levels observed along time (from the time-point of 2 to 24 h), mainly in the HC, may cause dysfunction of dopaminergic neurons (Miyazaki and Asanuma 2008), changing the pattern of DA release (phasic and/or tonic) (Goto and Grace 2005) resulting, thus, in the hyperlocomotion observed at 24 h post-GBR12909.
Prevention of GBR 12909-induced behavioral and pro-oxidative alterations by Li and VAL
Overall, as previously showed, we observed a relation between oxidative and behavioral alterations only at 2 h post-GBR12909. Thus, we chose this time point for the evaluation of the animals submitted to pretreatments with the mood-stabilizing drugs, Li and VAL.
It is important to highlight that the predictive validity of GBR 12909-induced model of mania was only recently evaluated by the administration of VAL for 28 days followed by a single administration of 9 mg/kg GBR 12909 and behavioral evaluation during 60 min (van Enkhuizen et al. 2013a). This previous study showed that chronic VAL treatment attenuated GBR 12909-induced hyperactivity, without affecting other behavioral parameters such as specific exploration or sequential organization. In their conclusion these authors called attention to the need for studies using Li as mood stabilizing drug in this model because VAL was not able to attenuate all aspects of GBR 12909-induced mania (van Enkhuizen et al. 2013a). The signaling mechanisms mediating the action of DA on hyperactivity are still not fully understood. For instance, acute administration of lithium salts is known to antagonize the hyperactivity induced by various dopaminergic agonists. Nevertheless, the mechanism by which lithium interferes with DA-associated behavior remains uncharacterized. One putative physiological target of Li, glycogen synthase kinase 3 (GSK−3), is activated in response to sustained stimulation of DA receptors and its inhibition interferes with the expression of DA-dependent behaviors. However, it is important to keep in mind that inhibition of GSK−3 either by lithium, GSK−3 inhibitors, or a gene-targeting approach cannot completely abolish DA-mediated behavior in mice (Beaulieu et al. 2004).
Considering the brain oxidative alterations observed in the present study both mood stabilizing drugs showed an antioxidant profile. The only situation in which Li was superior to VAL was in the HC where only Li increased GSH levels. Of note, it was recently suggested that glutathione is essential for lithium’s ability to ameliorate rotenone-induced protein carbonylation, but not nitration (Nascimento et al. 2014). Furthermore, the production of oxidative stress through mitochondrial complex I aberrations including decreased mRNA expression, activity, and protein levels has been strongly implicated in BD (Andreazza et al. 2010; Moretti et al. 2011).
In line with the importance of oxidative stress in BD it was previously demonstrated that the increase in antioxidant defenses is important for the mechanism of mood stabilizing drugs (Cui et al. 2007).
Strengths and limitations
The strength of the present study was the determination of the time course of behavioral and oxidative alterations induced by GBR12909 during a 24 h time period. Furthermore, the determination of the predictive validity with Li was likewise important, since this drug is the most prescribed mood stabilizing drug.
Limitation: determination of other parameters related to BD neurobiology, such as neurotrophins and inflammatory alterations.
Conclusion
The results presented in this study point to the time period of 2 h after GBR12909 as the most evident for the evaluation of behavioral and neurochemical alterations related to a mania-like phenotype. Another important observation was that Li as well as VAL were effective in the prevention of the behavioral alterations induced by this DAT inhibitor. Overall our results contribute to the construct validity (by the determination of oxidative imbalance) as well as expand the predictive validity of the GBR12909-induced model of mania (by the determination of Li preventive effects).
References
Anand A, Barkay G, Dzemidzic M et al (2011) Striatal dopamine transporter availability in unmedicated bipolar disorder. Bipolar Disord 13:406–413. doi:10.1111/j.1399-5618.2011.00936.x
Andersen PH (1987) Biochemical and pharmacological characterization of [3 H]GBR 12935 binding in vitro to rat striatal membranes: labeling of the dopamine uptake complex. J Neurochem 48:1887–1896. doi:10.1111/j.1471-4159.1987.tb05752.x
Andreazza AC, Kauer-Sant’anna M, Frey BN et al (2008) Oxidative stress markers in bipolar disorder: a meta-analysis. J Affect Disord 111:135–144
Andreazza AC, Shao L, Wang J-F, Young LT (2010) Mitochondrial complex I activity and oxidative damage to mitochondrial proteins in the prefrontal cortex of patients with bipolar disorder. Arch Gen Psychiatry 67:360–368. doi:10.1001/archgenpsychiatry.2010.22
Archer J (1973) Tests for emotionality in rats and mice: a review. Anim Behav 21:205–235
Barr AM, Lehmann-Masten V, Paulus M et al (2004) The selective serotonin-2A receptor antagonist M100907 reverses behavioral deficits in dopamine transporter knockout mice. Neuropsychopharmacology 29:221–228. doi:10.1038/sj.npp.1300343
Beaulieu J-M, Sotnikova TD, Yao W-D et al (2004) Lithium antagonizes dopamine-dependent behaviors mediated by an AKT/glycogen synthase kinase 3 signaling cascade. Proc Natl Acad Sci U S A 101:5099–5104. doi:10.1073/pnas.0307921101
Berk M, Dodd S, Kauer-Sant’anna M et al (2007) Dopamine dysregulation syndrome: implications for a dopamine hypothesis of bipolar disorder. Acta Psychiatr Scand Suppl 41–49. doi:10.1111/j.1600-0447.2007.01058.x
Berk M, Kapczinski F, Andreazza AC et al (2011) Pathways underlying neuroprogression in bipolar disorder: focus on inflammation, oxidative stress and neurotrophic factors. Neurosci Biobehav Rev 35:804–817
Brown AM, Chand N (2010) Using vanoxerine type medicant; blocking calcium channel current
Cappeliez P, Moore E (1990) Effects of lithium on an amphetamine animal model of bipolar disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 14:347–358
Cui J, Shao L, Young LT, Wang J-F (2007) Role of glutathione in neuroprotective effects of mood stabilizing drugs lithium and valproate. Neuroscience 144:1447–1453. doi:10.1016/j.neuroscience.2006.11.010
da-Rosa DD, Valvassori SS, Steckert AV et al (2012) Effects of lithium and valproate on oxidative stress and behavioral changes induced by administration of m-AMPH. Psychiatry Res 198:521–526. doi:10.1016/j.psychres.2012.01.019
Davies C, Sanger DJ, Steinberg H et al (1974) Lithium and alpha-methyl-p-tyrosine prevent “manic” activity in rodents. Psychopharmacologia 36:263–274
Drevets WC, Price JL, Furey ML (2008) Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct 213:93–118. doi:10.1007/s00429-008-0189-x
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Frey BN, Martins MR, Petronilho FC et al (2006a) Increased oxidative stress after repeated amphetamine exposure: possible relevance as a model of mania. Bipolar Disord 8:275–280. doi:10.1111/j.1399-5618.2006.00318.x
Frey BN, Valvassori SS, Reus GZ et al (2006b) Effects of lithium and valproate on amphetamine-induced oxidative stress generation in an animal model of mania. J Psychiatry Neurosci 31:326–332
Frey BN, Andreazza AC, Houenou J et al (2013) Biomarkers in bipolar disorder: a positional paper from the International Society for Bipolar Disorders Biomarkers Task Force. Aust N Z J Psychiatry 47:321–332
Goodwin FK, Jamison KR (2007) Manic-depressive illness: bipolar disorders and recurrent depression
Goto Y, Grace AA (2005) Dopaminergic modulation of limbic and cortical drive of nucleus accumbens in goal-directed behavior. Nat Neurosci 8:805–812. doi:10.1038/nn1471
Greenwood TA, Schork NJ, Eskin E, Kelsoe JR (2006) Identification of additional variants within the human dopamine transporter gene provides further evidence for an association with bipolar disorder in two independent samples. Mol Psychiatry 11:125–133, 115. doi:10.1038/sj.mp.4001764
Kuloglu M, Ustundag B, Atmaca M et al (2002) Lipid peroxidation and antioxidant enzyme levels in patients with schizophrenia and bipolar disorder. Cell Biochem Funct 20:171–175. doi:10.1002/cbf.940
Macêdo DS, Medeiros CD, Cordeiro RC, et al (2012) Effects of alpha-lipoic acid in an animal model of mania induced by D-amphetamine. Bipolar Disord 14:707–718. doi:10.1111/j.1399-5618.2012.01046.x
Macedo DS, de Lucena DF, Queiroz AI et al (2013) Effects of lithium on oxidative stress and behavioral alterations induced by lisdexamfetamine dimesylate: relevance as an animal model of mania. Prog Neuro-Psychopharmacol Biol Psychiatry 43:230–237
Martinez-Aran A (2004) Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry 161:262–270. doi:10.1176/appi.ajp.161.2.262
Meiser J, Weindl D, Hiller K (2013) Complexity of dopamine metabolism. Cell Commun Signal 11:34. doi:10.1186/1478-811X-11-34
Miyazaki I, Asanuma M (2008) Dopaminergic neuron-specific oxidative stress caused by dopamine itself. Acta Med Okayama 62:141–150
Moretti M, Valvassori SS, Steckert AV et al (2011) Tamoxifen effects on respiratory chain complexes and creatine kinase activities in an animal model of mania. Pharmacol Biochem Behav 98:304–310. doi:10.1016/j.pbb.2011.01.017
Morice R (1990) Cognitive inflexibility and pre-frontal dysfunction in schizophrenia and mania. Br J Psychiatry 157:50–54
Nascimento C, Kyunghee H, Trevor KL, Andreazza AC (2014) Glutathione-mediated effects of lithium in decreasing protein oxidation induced by mitochondrial complex I dysfunction. doi:10.1007/s00702-014-1318-8
NIH (1996) Guide for the care and use of laboratory animals- Institute of Laboratory Animal Research- National Research Council. Natl. Acad. Press
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Pinsonneault JK, Han DD, Burdick KE et al (2011) Dopamine transporter gene variant affecting expression in human brain is associated with bipolar disorder. Neuropsychopharmacology 36:1644–1655. doi:10.1038/npp.2011.45
Raffa M, Barhoumi S, Atig F et al (2012) Reduced antioxidant defense systems in schizophrenia and bipolar I disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 39:371–375. doi:10.1016/j.pnpbp.2012.07.013
Ralph-Williams RJ, Paulus MP, Zhuang X et al (2003) Valproate attenuates hyperactive and perseverative behaviors in mutant mice with a dysregulated dopamine system. Biol Psychiatry 53:352–359
Rao JS, Kellom M, Reese EA, et al (2012) Dysregulated glutamate and dopamine transporters in postmortem frontal cortex from bipolar and schizophrenic patients. J Affect Disord 136:63–71. doi:10.1016/j.jad.2011.08.017
Rush CR, Essman WD, Simpson CA, Baker RW (2001) Reinforcing and subject-rated effects of methylphenidate and d-amphetamine in non-drug-abusing humans. J Clin Psychopharmacol 21:273–286
Valvassori SS, Rezin GT, Ferreira CL et al (2010) Effects of mood stabilizers on mitochondrial respiratory chain activity in brain of rats treated with d-amphetamine. J Psychiatr Res 44:903–909. doi:10.1016/j.jpsychires.2010.02.009
Van Enkhuizen J, Geyer MA, Kooistra K, Young JW (2013a) Chronic valproate attenuates some, but not all, facets of mania-like behaviour in mice. Int J Neuropsychopharmacol 16:1021–1031. doi:10.1017/S1461145712001198
Van Enkhuizen J, Geyer MA, Young JW (2013b) Differential effects of dopamine transporter inhibitors in the rodent Iowa gambling task: relevance to mania. Psychopharmacology 225:661–674. doi:10.1007/s00213-012-2854-2
Young JW, Goey AKL, Minassian A et al (2010) GBR 12909 administration as a mouse model of bipolar disorder mania: mimicking quantitative assessment of manic behavior. Psychopharmacology 208:443–454. doi:10.1007/s00213-009-1744-8
Young JW, Henry BL, Geyer MA (2011a) Predictive animal models of mania: hits, misses and future directions. Br J Pharmacol 164:1263–1284
Young JW, van Enkhuizen J, Winstanley CA, Geyer MA (2011b) Increased risk-taking behavior in dopamine transporter knockdown mice: further support for a mouse model of mania. J Psychopharmacol 25:934–943. doi:10.1177/0269881111400646
Acknowledgments
The authors thank Mrs. Vilani Bastos for technical support. We thank CNPq, CAPES and FUNCAP for the financial support.
Conflict of interest
The authors have nothing to disclosure.
Financial support
Brazilian Institutions, CNPq grant number 484509/2012-8, CAPES and FUNCAP partially funded this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Queiroz, A.I.G., de Araújo, M.M., da Silva Araújo, T. et al. GBR 12909 administration as an animal model of bipolar mania: time course of behavioral, brain oxidative alterations and effect of mood stabilizing drugs. Metab Brain Dis 30, 1207–1215 (2015). https://doi.org/10.1007/s11011-015-9697-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-015-9697-6