Abstract
Near infrared radiation (NIR) is known to penetrate and affect biological systems in multiple ways. Recently, a series of experimental studies suggested that low intensity NIR may protect neuronal cells against a wide range of insults that mimic diseases such as stroke, brain trauma and neurodegeneration. However, the potential molecular mechanisms of neuroprotection with NIR remain poorly defined. In this study, we tested the hypothesis that low intensity NIR may attenuate hypoxia/ischemia-induced mitochondrial dysfunction in neurons. Primary cortical mouse neuronal cultures were subjected to 4 h oxygen-glucose deprivation followed by reoxygenation for 2 h, neurons were then treated with a 2 min exposure to 810-nm NIR. Mitochondrial function markers including MTT reduction and mitochondria membrane potential were measured at 2 h after treatment. Neurotoxicity was quantified 20 h later. Our results showed that 4 h oxygen-glucose deprivation plus 20 h reoxygenation caused 33.8 ± 3.4 % of neuron death, while NIR exposure significantly reduced neuronal death to 23.6 ± 2.9 %. MTT reduction rate was reduced to 75.9 ± 2.7 % by oxygen-glucose deprivation compared to normoxic controls, but NIR exposure significantly rescued MTT reduction to 87.6 ± 4.5 %. Furthermore, after oxygen-glucose deprivation, mitochondria membrane potential was reduced to 48.9 ± 4.39 % of normoxic control, while NIR exposure significantly ameliorated this reduction to 89.6 ± 13.9 % of normoxic control. Finally, NIR significantly rescued OGD-induced ATP production decline at 20 min after NIR. These findings suggest that low intensity NIR can protect neurons against oxygen-glucose deprivation by rescuing mitochondrial function and restoring neuronal energetics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Near infrared radiation (NIR) can penetrate biological tissue, and low intensity lasers that emit at or close to the NIR range (600 to 1,000 nm) have been applied as a noninvasive technology to modulate intracellular biochemistry and metabolism in many model systems (Karu 1999). Clinically, low intensity NIR lasers have been used as a potential therapy for a variety of conditions including pain relief (Brosseau et al. 2005; Morimoto et al. 2013), treatment of inflammation (Wang et al. 2013; Xavier et al. 2010), and wound healing (Peplow et al. 2010).
Emerging experimental evidence suggest that NIR may also interact with the central nervous system in potentially beneficial ways. NIR may promote axonal growth and nerve regeneration (Anders et al. 2004; Byrnes et al. 2005). In vitro studies suggest that exposure to NIR may defend against excitotoxicity and oxidative stress in cultured neurons (Huang et al. 2013a; Huang et al. 2013b). However, the underlying molecular and cellular mechanisms of these putative neuroprotective phenomenon remain poorly understood. Because eukaryotic mitochondria may be evolutionarily descended from photosynthetic endosynbiotic bacteria (Cavalier-Smith 2006; Karu 1999), it is possible that mitochondrial responses may be involved in NIR neuroprotection. In this study, we tested the hypothesis that NIR’s ability to protect neurons against substrate deprivation may be related to improvements in mitochondrial function and energetic rescue.
Methods
Animals
All animal experiments were performed following protocols approved by the Massachusetts General Hospital Institutional Animal Care and Use Committee in compliance with the NIH Guide for the Care and Use of Laboratory Animals.
Primary mouse cortical neuron culture
Primary mouse cortical neuron culture was performed as previously described (Liu et al. 2009). Briefly, primary mouse cortical neurons were isolated from 15 days embryonic cortex obtained from the pregnant C57 BL/6 female mouse. Neurons from each embryo cortex were isolated and seeded into multiple well plates separately with equal cell amounts (1.5 × 105 cells/well in 24-well plates, 6 × 105 cells/well in 6-well plate). The neurons were maintained in Neurobasal medium (NBM) with 3 % B27 and 0.3 mM glutamine (Invitrogene). Medium was half changed in each 3 days.
Oxygen-glucose deprivation (OGD) and reoxygenation
OGD was performed following the method as previous described (Yu et al. 2009) . Briefly, at day 8–9 of primary neuron culture, NBM was replaced with deoxygenated, glucose-free extracellular solution–Locke’s medium (154 mM NaCl, 5.6 mM KCl, 2.3 mM CaCl2, 1.0 mM MgCl2, 3.6 mM NaHCO3, 5 mM Hepes, pH 7.2), the cells were then put in a specialized, humidified chamber (Heidolph, incubator 1,000, Brinkmann Instruments, Westbury, NY, USA) at 37 °C, which contained an anaerobic gas mixture (90 % N2, 5 % H2, and 5 % CO2). Four hour OGD was performed in this study, which is our previously established and routinely used OGD model (Yu et al 2009). Four hour OGD followed by 20 h reoxygenation caused ~40 % neuronal cell death, which is a moderate injury for cell viability and neuroprotection study. After 4 h incubation, the cultures were removed from the anaerobic chamber, and the OGD solution was replaced with maintenance medium. Cells were then allowed to recover for 20 h (for neurotoxicity assay) or 4 h (for MMP and ATP measurements) in a regular incubator. Unless otherwise specified, the “OGD” in the text refers to 4 h OGD plus 4 h reoxygenation.
Near infrared Radiation
Near infrared radiation was obtained using a 810 nm diode laser (Photothera, Inc., Carlsbad, CA). The cells were irradiated in continuous wave mode with a power density of 25 mW/cm2 for 2 min, and then returned to normal incubation condition before being measured for neurotoxicity or mitochondrial function markers.
Neurotoxicity measurement
Neurotoxicity was measured by lactate dehydrogenase (LDH) release. LDH release is an indicator of plasma membrane damage and commonly used for the determination of neurotoxicity as we previously described (Wang et al. 2002). Primary cortical neurons were cultured in 24-well plates for 8 − 9 days. LDH release was measured after OGD.
MTT reduction
(3-(4, 5-dimethylthiazolyl-2)-2, 5-diphenyltetrazolium bromide) (MTT) reduction by viable mitochondria was used as an indicator of neuronal viability and mitochondria function, as previously described (Wang et al. 2002). MTT reduction was measured after 4 h OGD followed by 4 h reoxygenation. Percentages of live cell counts were used for assay normalization.
Mitochondrial membrane potential measurement
JC-1 (5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylbenzimi-dazolylcarbocyanine iodide) is a cationic carbocyanine dye that exists as a monomer at low concentrations with green fluorescence, and forms aggregates at higher concentrations with red fluorescence. JC-1 accumulates in mitochondria. This accumulation is dependent on the membrane potential and indicated by a fluorescence emission shift from green (~525 nm) to red (~590 nm). Consequently, mitochondrial depolarization is indicated by a decrease in the red/green fluorescence intensity ratio. After 20 min of incubation with JC-1 (Invitrogen) and Hoechst-33342 (final concentrations, 5 μg/ml) at 37 °C, the cells were irradiated with the 810-nm laser. The cells were washed twice with the PBS and fluorescence was either measured by fluorescence plate reader (green fluorescence, excitation 485-nm and emission 535-nm; red fluorescence, excitation 590-nm and emission 610-nm) and imaged with a confocal microscope.
ATP production assay
After 5 min of NIR, the cells were lysed with 50 μl cell lysis buffer and the plate was placed on shaker for 2 min to ensure completely release of ATP. Five microliters lysate was then transferred to 96-well plates for BCA assay for protein concentration measurement, while the rest of the cell lysates were transferred to 96-well plates with black walls for ATP measurement. One hundred microliters of Cell-Titer Glo Assay (Promega, Madison, WI) was added into each sample and after about 5 min, the luminescence signal was measure by a luminescence plate reader (Wallac Tri-Lux beta, PerkinElmer Life and Analytical Sciences, Waltham, MA).
Statistical analysis
Results were expressed as mean ± SEM. Multiple comparisons were evaluated by one-way ANOVA followed by Tukey–Kramer’s tests between all groups. P < 0.05 was considered statistically significant.
Results
-
1.
Effect of NIR on OGD-induced neuronal cell death
After 8 days in culture, primary mouse cortical neurons were transiently subjected to 4 h OGD followed by reoxygenation with normal glucose conditions. Low intensity NIR was applied after 2 h reoxygenation. Cell death was measured by LDH release at 4 h (O4/R4) and 20 h (O4/R20) reoxygenation. Our results showed that after 4 h reoxygenation (2 h post-NIR), there was no significant difference in cell death between NIR-treated neurons and the control group. However, neuronal cell death continued to increase over the course of reoxygenation in untreated controls but not in NIR-treated neurons. At 20 h reoxygenation, cell death was 33.8 ± 3.4 % in the control group, while NIR treatment significantly reduced neuronal death to 23.6 ± 2.9 % (30.2 % reduction, n = 6, p < 0.05) (Fig. 1).
Fig. 1 Effect of NIR on OGD-induced neuronal cell death in primary cultured mouse cortical neurons. Primary culture mouse cortical neurons were subjected to 4 h OGD and reoxygenation. NIR was applied at 2 h reoxygenation. Neurotoxicity was measured by LDH release at 4 h reoxygeneration (O4/R4) or 20 h reoxygenation (O4/R20) (n = 6, * p < 0.05)
-
2.
Effect of NIR on OGD-induced alterations in MTT reduction
Next, we asked whether NIR neuroprotection was accompanied by detectable changes in mitochondrial function. MTT reduction was quantified as a functional marker after 4 h OGD plus 4 h rexoygenation (2 h post-NIR). MTT reduction was significantly decreased to 75.9 ± 2.68 % by OGD compared to normal undamaged neurons. But this mitochondrial disturbance was significantly rescued by NIR back to 87.6 ± 4.55 % (15.4 % improvement, n = 6, p < 0.05) (Fig. 2).
-
3.
Effect of NIR on OGD-induced alterations in mitochondrial membrane potential
Mitochondrial membrane potential was measured using JC-1 reagents in neurons after 4 h OGD plus 4 h rexoygenation (2 h post-NIR). Spectrophotometer readings showed that membrane potentials were reduced by OGD to 48.9 ± 4.39 % compared to normal undamaged neurons, while NIR significantly ameliorated this reduction to 89.6 ± 13.9 % (83 % improvement, n = 4, p < 0.05) (Fig. 3a). Furthermore, fluorescence microscopy of JC-1 aggregates also showed that mitochondrial membrane potential was significantly decreased by OGD, while NIR appeared to rescue these OGD-induced reductions in membrane potential (Fig. 3b).
Fig. 3 Effect of NIR on OGD-caused alterations in mitochondrial membrane potential (MMP). Primary cultured neurons were subjected to 4 h OGD and reoxygenation. NIR was applied at 2 h reoxygenation. a MMP measured by spectrophotometer reading at 4 h reoxygeneration (O4/R4) (2 h post-NIR) compared with untreated control group (n = 4, * p < 0.05). b MMP measured by fluorescence microscopic imaging of JC-1 aggregates at 4 h reoxygeneration (O4/R4) (2 h post-NIR) (Scale bar = 50 μm)
-
4.
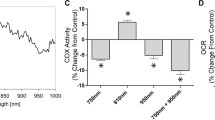
Effect of NIR on OGD-caused alterations in ATP production
Finally, we asked whether neuroprotective rescue of mitochondrial function was accompanied with restoration of energetics. After 4 h OGD and 2 h reoxygenation, the total intracellular ATP levels in neurons were measured at 5 min, 20 min, 40 min, 60 min and 120 min post-NIR and compared with untreated neurons. Our results showed that intracellular ATP levels were significantly reduced by OGD compared to undamaged normal conditions. NIR treatment significantly rescued ATP levels to 88.7 ± 7.8 % (30 % improvement, n = 6, p < 0.05) at 20 min post-treatment compared to untreated controls (68.6 ± 5.2 %) at the same time point (Fig. 4).
Fig. 4 Effect of NIR on ATP production in primary neurons after OGD. Primary cultured neurons were subjected to 4 h OGD and reoxygenation, and treated with NIR at 2 h reoxygenation. The total intracellular ATP levels were measured at 5 min, 20 min, 40 min, 60 min and 120 min post-NIR and compared with normal condition (n = 6, * p < 0.05 vs non-treated control at the same time point)
Discussion
Low intensity lasers at or near the infrared range are well known to possess many biological effects (Karu 1999). In the context of the CNS, NIR lasers have been proposed to protect neurons against a wide spectrum of insults that may mimic many disorders including stroke, brain trauma and neurodegeneration. Low intensity NIR lasers may reduce amyloid-beta induced neurotoxicity in mice (De Taboada et al. 2011), and may reduce injury and improve outcomes in animal models of traumatic brain injury (Oron et al. 2007; Xuan et al. 2013) and cerebral ischemia (Lapchak et al. 2004; Oron et al. 2006). However, in spite of promising experimental results, recent clinical trials testing NIR lasers in acute ischemic stroke have failed to reach positive outcomes. Of course, many complex reasons can contribute to any failed clinical trial. However, these findings also suggest that further basic investigations into the mechanisms of putative neuroprotection are needed. In the present study, we tested the hypothesis that the ability of NIR to protect neurons against OGD may be due to its ability to modify mitochondrial dysfunction and rescue energetics. Our data show that very brief exposure to a low intensity 810 nm NIR laser significantly improved MTT reduction, mitochondrial membrane potential and ATP levels in neurons that were damaged by oxygen-glucose deprivation. In concert with mitochondrial rescue, NIR prevented the accumulation of cell death over the course of reoxygenation. Taken together, these findings support the notion that NIR’s ability to modify mitochondria may underlie its neuroprotective properties.
Mitochondria may represent a reasonable target for NIR because they may be evolutionarily descended from photosynthetic endosynbiotic bacteria (Cavalier-Smith 2006; Karu 1999). Extensive studies have demonstrated that cytochrome c oxidase (mitochondrial complex IV) is a primary photoacceptor (Eells et al. 2003; Karu 1999). As a component of the mitochondrial respiration chain, cytochrome c oxidase contains four redox active metal centers and has a strong absorbency in the far-red to near-infrared spectral range, thus the biological roles of NIR at the cellular level can be ascribed to the activation of mitochondrial respiratory chain. This mechanism might be at least partially responsible for the restoration of general mitochondrial function, as measured by MTT reduction in our study, since MTT reduction reflects the cellular metabolic activity via NAD(P)H-dependent cellular oxidoreductase enzymes (Berridge et al. 2005).
Our results also showed that NIR can rescue OGD-impaired mitochondrial membrane potentials. Mitochondrial membrane potential is a critical feature of mitochondrial function, as it reflects the pumping of hydrogen ions across the mitochondrial inner membrane during the process of electron transport and oxidative phosphorylation, all key events in mitochondrial respiration (Chen 1988). Thus NIR may influence mitochondrial membrane potential through its absorption by cytochrome c oxidase. Furthermore, we also observed an increased ATP level at 20 min post-NIR, which may also be attributable to preserved mitochondria respiration and membrane potentials. This result is consistent with other studies showing that NIR can enhance ATP production in primary neurons under normal conditions (Sharma et al. 2011). However, the increase of ATP by NIR in our study is transient, detectable only at 20 min post-treatment, which may be due to the rapid ATP consumption in cells under injury conditions. How a relatively brief effect on ATP contributes to the overall neuroprotection effect of NIR is unclear and awaits further investigation.
There are a few caveats in this study. First, we only tested the effects of NIR treatment after OGD at limited time points. Our data suggest that NIR improves mitochondrial function, briefly rescues ATP levels, then prevents further development of neuronal death during reoxygenation. However, more detailed time course studies will be required to dissect how mitochondrial rescue can be linked to neuroprotection as a causal mechanism. Second, we only tested NIR treatments at a single time point. Whether multiple NIR exposures may offer more pronounced neuroprotective effects remain to be assessed. Additionally, in this study we conducted a 2 min laser exposure, but this may not be the optimal therapeutic regimen, in terms of power and exposure. The optimal therapeutic regimen with maximal efficacy and safety should be defined in pre-clinical study before moving this therapy into clinical investigation (Khuman et al. 2012; Wu et al. 2012). Finally, our focus on selected markers of mitochondrial function does not preclude the possibility of other cellular targets being involved. For instance, NADPH-oxidase is an enzyme capable of a non-mitochondrial respiratory burst, and might be activated by NIR (Duan et al. 2001). Furthermore, certain molecules with visible absorption bands, like porphyrins lacking transition metal coordination centers (Friedmann et al. 1991), can be converted into a long-lived triplet state by photon absorption. This triplet state can interact with ground-state oxygen with energy transfer leading to production of a reactive species, singlet oxygen, which at very low doses can cause cell proliferation and tissue stimulation (Plaetzer et al. 2002). Moreover, experimental evidence has shown that nitric oxide might be involved in the cellular response to photons (Majem et al. 2006), as NIR is associated with reduced NO production in either rat stroke model (Leung et al. 2002) or arthritis model (Moriyama et al. 2005). Thus NIR may also play a role in inhibiting NO neurotoxicity. All these other possible mechanisms should be addressed in future studies.
In conclusion, this study for the first time demonstrated the protective effect of NIR against OGD-induced neurotoxicity in primary mouse cortical neurons, and suggested that this effect might be mediated via a preservation of mitochondrial functions. More detailed investigations into NIR molecular mechanisms may be warranted before any further attempts at clinical translation are re-initiated.
References
Anders JJ et al (2004) Phototherapy promotes regeneration and functional recovery of injured peripheral nerve. Neurol Res 26:233–239
Berridge MV et al (2005) Tetrazolium dyes as tools in cell biology: new insights into their cellular reduction. Biotechnol Annu Rev 11:127–152
Brosseau, L., et al., 2005. Low level laser therapy (Classes I, II and III) for treating rheumatoid arthritis. Cochrane Database Syst Rev. CD002049
Byrnes KR et al (2005) Light promotes regeneration and functional recovery and alters the immune response after spinal cord injury. Lasers Surg Med 36:171–185
Cavalier-Smith T (2006) Origin of mitochondria by intracellular enslavement of a photosynthetic purple bacterium. Proc Biol Sci 273:1943–1952
Chen LB (1988) Mitochondrial membrane potential in living cells. Annu Rev Cell Biol 4:155–181
De Taboada L et al (2011) Transcranial laser therapy attenuates amyloid-beta peptide neuropathology in amyloid-beta protein precursor transgenic mice. J Alzheimers Dis 23:521–535
Duan R et al (2001) Signal transduction pathways involved in low intensity He-Ne laser-induced respiratory burst in bovine neutrophils: a potential mechanism of low intensity laser biostimulation. Lasers Surg Med 29:174–178
Eells JT et al (2003) Therapeutic photobiomodulation for methanol-induced retinal toxicity. Proc Natl Acad Sci USA 100:3439–3444
Friedmann H et al (1991) A possible explanation of laser-induced stimulation and damage of cell cultures. J Photochem Photobiol B 11:87–91
Huang, Y. Y., et al., 2013a. Low-level laser therapy (810 nm) protects primary cortical neurons against excitotoxicity in vitro. J Biophotonics
Huang YY et al (2013b) Low-level laser therapy (LLLT) reduces oxidative stress in primary cortical neurons in vitro. J Biophotonics 6:829–838
Karu T (1999) Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B 49:1–17
Khuman J et al (2012) Low-level laser light therapy improves cognitive deficits and inhibits microglial activation after controlled cortical impact in mice. J Neurotrauma 29:408–417
Lapchak PA et al (2004) Transcranial infrared laser therapy improves clinical rating scores after embolic strokes in rabbits. Stroke 35:1985–1988
Leung MC et al (2002) Treatment of experimentally induced transient cerebral ischemia with low energy laser inhibits nitric oxide synthase activity and up-regulates the expression of transforming growth factor-beta 1. Lasers Surg Med 31:283–288
Liu J et al (2009) Effects of neuroglobin overexpression on mitochondrial function and oxidative stress following hypoxia/reoxygenation in cultured neurons. J Neurosci Res 87:164–170
Majem M et al (2006) Does induction chemotherapy still have a role in larynx preservation strategies? The experience of Institut Catala d’Oncologia in stage III larynx carcinoma. Laryngoscope 116:1651–1656
Morimoto Y et al (2013) Low level laser therapy for sports injuries. Laser Ther 22:17–20
Moriyama Y et al (2005) In vivo study of the inflammatory modulating effects of low-level laser therapy on iNOS expression using bioluminescence imaging. Photochem Photobiol 81:1351–1355
Oron A et al (2006) Low-level laser therapy applied transcranially to rats after induction of stroke significantly reduces long-term neurological deficits. Stroke 37:2620–2624
Oron A et al (2007) low-level laser therapy applied transcranially to mice following traumatic brain injury significantly reduces long-term neurological deficits. J Neurotrauma 24:651–656
Peplow PV et al (2010) Laser photobiomodulation of wound healing: a review of experimental studies in mouse and rat animal models. Photomed Laser Surg 28:291–325
Plaetzer K et al (2002) Characterization of the cell death modes and the associated changes in cellular energy supply in response to AlPcS4-PDT. Photochem Photobiol Sci 1:172–177
Sharma SK et al (2011) Dose response effects of 810 nm laser light on mouse primary cortical neurons. Lasers Surg Med 43:851–859
Wang X et al (2002) Hemoglobin-induced cytotoxicity in rat cerebral cortical neurons: caspase activation and oxidative stress. Stroke 33:1882–1888
Wang, X. Y., et al., 2013. Effect of low-level laser therapy on allergic asthma in rats. Lasers Med Sci
Wu Q et al (2012) Low-level laser therapy for closed-head traumatic brain injury in mice: effect of different wavelengths. Lasers Surg Med 44:218–226
Xavier M et al (2010) Anti-inflammatory effects of low-level light emitting diode therapy on Achilles tendinitis in rats. Lasers Surg Med 42:553–558
Xuan W et al (2013) Transcranial low-level laser therapy improves neurological performance in traumatic brain injury in mice: effect of treatment repetition regimen. PLoS One 8:e53454
Yu Z et al (2009) Neuroglobin-overexpression alters hypoxic response gene expression in primary neuron culture following oxygen glucose deprivation. Neuroscience 162:396–403
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yu, Z., Liu, N., Zhao, J. et al. Near infrared radiation rescues mitochondrial dysfunction in cortical neurons after oxygen-glucose deprivation. Metab Brain Dis 30, 491–496 (2015). https://doi.org/10.1007/s11011-014-9515-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-014-9515-6