Abstract
Mucopolysaccharidosis type I is one of the most frequent lysosomal storage diseases. It has a high morbidity and mortality, causing in many cases severe neurological and somatic damage in the first years of life. Although the clinical phenotypes have been described for decades, and the enzymatic deficiency and many of the mutations that cause this disease are well known, the underlying pathophysiological mechanisms that lead to its development are not completely understood. In this review we describe and discuss the different pathogenic mechanisms currently proposed for this disease regarding its neurological damage. Deficiency in the lysosomal degradation of heparan sulfate and dermatan sulfate, as well as its primary accumulation, may disrupt a variety of physiological and biochemical processes: the intracellular and extracellular homeostasis of these macromolecules, the pathways related to gangliosides metabolism, mechanisms related to the activation of inflammation, receptor-mediated signaling, oxidative stress and permeability of the lysosomal membrane, as well as alterations in intracellular ionic homeostasis and the endosomal pathway. Many of the pathogenic mechanisms proposed for mucopolysaccharidosis type I are also present in other lysosomal storage diseases with neurological implications. Results from the use of methods that allow the analysis of multiple genes and proteins, in both patients and animal models, will shed light on the role of each of these mechanisms and their combination in the development of different phenotypes due to the same deficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucopolysaccharidosis type I (MPS I) is a lysosomal storage disease (LSD) included within the genetically heterogeneous group of mucopolysaccharidoses (MPSs). These diseases are caused by enzyme deficiencies in the catabolism of mucopolysaccharides or glycosaminoglycans (GAGs) (Neufeld and Muenzer 2001). MPS I is the type that contributes the largest number of diagnoses worldwide (Malm et al. 2008; Baehner et al. 2005; Ben Turkia et al. 2009; Meikle et al. 1999; Lowry et al. 1990; Menéndez-Sainz et al. 2009). It has an autosomal recessive inheritance pattern, and is due to a deficiency in enzyme activity alpha-L-iduronidase (IDUA) (Neufeld and Muenzer 2001).
The IDUA enzyme (EC. 3.2.1.76) is involved in the degradation of the GAGs heparan sulfate (HS) and dermatan sulfate (DS). These molecules can be found in free form in the extracellular matrix or as part of the structure of different types of proteoglycans, with important functions both in the structure of tissues and in intercellular communication. Intralysosomal accumulation of these substrates results in pathological processes that produce a chronic and progressive dysfunction in cells, tissues and organs of many systems (Clarke 2008).
MPS I exhibits considerable clinical heterogeneity with varying degrees of skeletal, cardiac, digestive, respiratory and central nervous system (CNS) commitment caused by the same enzyme deficiency (Neufeld and Muenzer 2001; Terlato and Cox 2003). Hurler syndrome represents the most severe phenotype. The disease progresses rapidly from six to 24 months, resulting in significant developmental delay, macrocephaly, coarse facies, hernias, skeletal changes (multiple dysostosis), stiffness and contracture of joints, hepatosplenomegaly, corneal opacity, deafness and intellectual disability. Death occurs in its natural evolution before the age of 10 due to respiratory complications or cardiomyopathy (Neufeld and Muenzer 2001; Moore et al. 2008).
Since the introduction of treatments capable of checking the course of the disease, including hematopoietic stem cell transplantation and enzyme replacement therapy (Aldenhoven et al. 2008; de Ru et al. 2011); there is a growing interest in identifying new biomarkers and methods for a rapid early diagnosis, as well as new therapeutic approaches. This requires a thorough understanding of the pathogenesis of the disease. The present review explores recent observations regarding potential mechanisms that may explain the pathophysiological development of MPS I.
Tissular storage of GAGs
GAG storage by itself seems to be the primary cause of the enlargement of various organs in patients with MPS I. Cytological analysis of murine models show the presence of large amounts of HS and DS in the liver, kidneys, spleen, heart, and to a lesser extent in the CNS, ever since the fetal period (Wang et al. 2010). Microscopic analysis of bone has shown retention of GAGs in the trabecular matrix and the bone cortex (Liu et al. 2005).
Lysosomal volume in tissues with an extensive intercellular compartment, of which GAGs are a major constituent, such as cornea, cartilage, bone and the connective tissue of skin, fasciae, heart valves and blood vessels, is 30-77 times higher in MPS I patients than in controls, and represents about 20% of cell volume (Resnick et al. 1994). Excess HS and DS is also seen in the urine and plasma, indicating a notable increase in extracellular molecules. Their structure differs from that present in proteoglycans, for they are partially depolymerized (Tomatsu et al. 2005; Tomatsu et al. 2010).
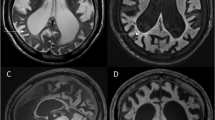
In relation to neurological manifestations due to an extensive storage of GAG, even in patients with the mild phenotype of the disease, cranial magnetic resonance images has shown signal abnormalities predominantly in the periventricular white matter. In addition, cerebral atrophy and ventriculomegaly (2/3 of the non-shunt patients) have been reported (Matheus et al. 2004). Hydrocephalus is frequently observed in patients with severe phenotype. It has been shown to be caused by a lack of reabsorption of cerebrospinal fluid in the arachnoid granulations due to thickening of the meninges by an extensive lysosomal storage. This also increases intracranial pressure and may contribute to intellectual disability (Gabrielli et al. 2004; Giussani et al. 2010). GAG deposition in the connective tissue of the brain causes narrowing of the dura, which leads to compressive myelopathy. Storage within the meninges can also cause spinal cord compression at cervical level (Boor et al. 2000). Many patients have carpal tunnel syndrome. Lysosomal storage was observed in fibroblasts obtained from biopsies of the synovial thickening causing compression of the median nerve (Yuen et al. 2007).
Other clinical manifestations that may be directly caused by the accumulation of GAGs are ocular. Histopathology studies have documented an increasing accumulation of these macromolecules in the iris, cornea and sclera, as well as structural periocular changes in the eyelids and the orbit (Ashworth et al. 2006). The ocular features include corneal clouding, optic nerve swelling, optic atrophy, glaucoma, and retinal pigment epithelium degeneration. Optic atrophy may be caused by increased intracranial pressure, by thickening of the sclera or the optic nerve outside the balloon, storage within the nerve or involvement of the meninges (Schumacher et al. 2008).
The deposit of GAGs in the spiral ganglion and vestibular-cochlear nerve may be responsible for the conductive and sensory hearing loss that occurs during the first year of life in many patients with MPS I (Hoffmann and Mayatepek 2005). The combination of chronic hearing loss, developmental delay and enlarged tongue may result in poor language skills (Neufeld and Muenzer 2001).
Analysis of HS levels in IDUA deficient mice tissues, report a noticeably less storage in the brain compared with the liver (Holley et al. 2011). Brain pathology is notoriously difficult to correct in MPS I patients because of the blood-brain barrier preventing entry of corrective enzymes except via bone marrow-derived microglia following hematopoietic stem cell transplantation. Thus, this difference suggests that brain GAG storage may occur later or more slowly than in other tissues, improving the outlook for therapeutic intervention following early diagnosis. It may also suggest a different pathological threshold for storage in neuronal tissue, suggesting the possibility of highly GAG-sensitive pathological cascades that may, in turn, inform therapeutic targets (Holley et al. 2011).
Altered metabolism of gangliosides
Lysosomal storage in the CNS of patients with MPS I results in significant neuronal loss and gliosis. It is heterogeneous, both in the type of compound accumulated and its location. GAGs are a majority in perivascular regions, connective tissue, meninges, microglial cells and neurons; whereas a significant accumulation of GM2 and GM3 gangliosides is observed principally in neurons (Walkley 2004a). Accumulation of unesterified cholesterol in neurons that store gangliosides has also been demonstrated (McGlynn et al. 2004). Storage of these macromolecules is also found in other MPSs (Walkley 2004a). Ganglioside storage occurs very early in the course of the disease and may constitute a causal factor determining the progress of CNS dysfunction (Desmaris et al. 2004).
The changes in axonal and dendritic morphology observed both in patients and in animal MPS I models might be the result of such accumulation, particularly of GM2, since this ganglioside has been linked to the dendritogenesis process in the developing brain (Walkley et al. 2000). These alterations may lead to the resumption of dendritic growth and the occurrence of altered synapses leading to neuro-synaptic dysfunction. For example, storage disease-affected neurons may undergo the formation of huge axon hillock enlargements (termed meganeurites) containing typical storage bodies, which often exceed the volume of adjacent perikarya. Cortical pyramidal neurons also exhibit abnormal sprouting of new dendrites at the axon hillock (termed ectopic dendritogenesis). These new dendrites are, in turn, contacted by axons that form new excitatory synaptic connections (Walkley et al. 2000; Walkley 2004b). Purkinje cells show marked distension of the fusiform perikarya with an expansion of their dendrites (Walkley 2009).
It is suggested that the alteration in the metabolism of gangliosides may be given by the direct action of GAGs in the enzymes involved in their degradation, since HS molecules can bind selectively to different hydrolases and reduce their activity towards their natural substrates (Clarke 2008). For example, in fibroblasts obtained from patients with different types of MPSs a marked decrease has been noted in neuraminidase activity towards gangliosides GM2 and GM3. This effect, tested in vitro, has been ascribed to the presence of a diffusible factor, presumably one or more of the sulfated GAGs accumulated or their incomplete degradation products (Baumkötter and Cantz 1983; Liour et al. 2001).
Both GM2 and GM3 are degraded to simpler components in late endosomes/lysosomes. Given the close sequential relationship of these degradative steps (GM1→GM2→GM3), it most probably takes place in the same late endosomal-lysosomal compartment. Furthermore, in neurons affected by MPS disease this compartment would presumably also contain detectable quantities of nondegraded HS, because GAGs-degradative enzymes would in all likelihood occupy this same cellular compartment (Parkinson-Lawrence et al. 2010). Surprisingly, studies of MPS III murine models indicate that although GM2 and GM3 molecules accumulate within the same neuron, they are consistently located in separate populations of cytoplasmic vesicles. Additionally, GM3 ganglioside only partially co-localized with the primary storage material (HS) within endosomal-lysosomal compartments (McGlynn et al. 2004). This finding is interesting, for the enzymes participating in the sequential degradation of gangliosides and GAGs are located in the same cellular compartment.
These results can not be explained only as a simple inhibition of degradative enzymes due to the accumulation of GAGs, thus suggesting the presence of complex deficiencies in gangliosides trafficking and/or homeostatic control mechanisms (Fig. 1).
Secondary gangliosides accumulation following primary GAGs storage in MPSs. An accompanying storage of GM2 (red circle) and GM3 (yellow multipoint star) gangliosides as well as free cholesterol (blue hexagon) has been documented to occur in neurons of patients and animal models of MPS I and others types of MPSs. Intracellular GAGs (three wavy black lines) accumulation may secondarily inhibit the activity of ganglioside-degradative lysosomal enzymes (green diamond) such as sialidase. GM2 and GM3 are localized to different populations of vesicles and only partially co-localized with the primary storage material, while cholesterol only had partial overlap with GM3. This suggests that independent/physically separate mechanisms are responsible for their sequestration. Given that gangliosides and cholesterol are both constituents of membrane rafts; their abnormal sequestration on the lysosomal-endosomal system due to a potential altered synthesis, trafficking and/or recycling of gangliosides simple products induced by an increase in intracellular GAGs could severely impact neuronal function
The studies also report the novel finding that free cholesterol is sequestered in conjunction with GM3 in many neurons from mice with MPS I and MPS III disease in a manner parallel to that observed in primary glycosphingolipidoses (McGlynn et al. 2004). Given that cholesterol and gangliosides are normally co-localized to specialized membrane microdomains known as rafts, which are believed to be important for signaling events in cells, their co-sequestration in both types of MPSs could be an additional element contributing to disease pathogenesis.
The accumulation of GM3 in late endosomes and lysosomes could cause a blockage in the retrograde transport of simple gangliosides breakdown products from lysosomes to the Golgi for use as precursors. This could lead to differential changes in the ganglioside synthetic routes. This sequestration mechanism of precursors has also been proposed for primary ganglioside storage diseases like GM1 and GM2 gangliosidoses, as well as others that occur with secondary accumulation, such as Niemann-Pick disease types A and C and α-mannosidosis (Walkley 2003; Walkley 2007; Prinetti et al. 2011). In all these cases, as in MPSs, there is evidence of the growth of ectopic dendrites on susceptible neuron populations.
Inflammatory response
Activation of immune effectors triggering inflammatory processes in the brain has been found in several LSDs with CNS pathology (Castaneda et al. 2008). Even in Gaucher disease type I, in which there is no CNS involvement, accumulation of substrates in the macrophages of the liver, spleen and bone marrow produces activation and the release of multiple inflammatory cytokines (Jmoudiak and Futerman 2005).
In the brain, macrophage lineage cells are represented by microglia, which respond to trauma and disease by activating the inflammatory response. In healthy individuals, microglia cells are in a resting state, but if infection or trauma is sensed, they undergo a wave of self-limiting activation until the disease/damage episode is resolved (Walkley 2007). Upon substrate accumulation in LSDs, an inflammatory response is triggered that is not self-limiting, and once triggered it progressively increases in parallel with the storage burden (Vitner et al. 2010).
Studies of murine models of MPS I show a perineuronal microglia activation within the CNS, as well as an increase in transcript levels for CD 38, lysozyme M, cathepsins S and Z, cytochrome b558, DAP12 and complements C1q and C4, all of which relate to macrophage/monocyte activation (Ohmi et al. 2003) (Fig. 2). Inside these cells there is abundant GAG, GM2 and GM3 lysosomal deposition, which can be either endogenous or caused by phagocytosis of the extracellular milieu and damaged or dead cells. However, these studies do not distinguish between activation of microglia resident within the brain and/or recruitment of activated monocytes from the circulation. The observation that activation of macrophages within the CNS occurs before evidence of significant CNS pathology would indicate that this phenomenon is not primarily related to neuronal cell loss.
Inflammation as a pathological mechanism in MPS I and other LSDs. Studies of murine models of MPS I and other LSDs with neurologic pathology revealed perineuronal microglial activation within the CNS and increased transcripts for genes related to macrophage/monocyte activation which contributes to pathogenesis. In addition, a chronic and unresolved inflammation state could produce an oxidative imbalance through the enhanced liberation of reactive oxygen and nitrogen species (ROS, RNS) by phagocytes. This in turn, may contribute to inflammation by a misidentification and autoimmune response to proteins damaged by oxidation. Evidence is also emerging for the involvement of inflammation in the pathophysiology of bone and joint disease in MPSs (Simonaro et al. 2005). One possible effector of triggering the inflammation response could be through the activation of TLR4 by HS incomplete degradation products accumulated in MPS I. This has also been associated to the pathogenesis of aortic dilatation and cartilage degeneration in MPSs
Although the precise mediators of the inflammatory response are still unknown, it is known that GAGs have proinflammatory properties related to the stabilization and release of cytokines and their oligomerization to achieve their biological action, as well as to cellular signaling processes (Mulloy and Rider 2006; Parish 2006). One mechanism proposed for triggering the inflammatory response in MPS diseases is through activation of the TLR4 receptor (Fig. 2).
The non-physiological activation of the TLR4 receptor resulting from its union with the lipopolysaccharide (LPS) causes the secretion of pro-inflammatory cytokines that trigger an innate immune response. Incomplete GAG degradation products such as HS resemble the LPS, thus its accumulation in the extracellular fluid could activate this receptor (Johnson et al. 2002). Animal models of various MPSs exhibiting accumulation of HS show an increase in the expression of several genes involved in signaling through TLR4. Among these are the genes encoding for TLR4 itself, the LPS binding protein and MyD88 (Simonaro et al. 2005).
In particular, mice with MPS IIIB show an increase in the expression of macrophage inflammatory protein-1 alpha chemokine and CD11b+ microglial cells in the cerebral cortex in relation to MPS IIIB mice deficient for TLR4 and MyD88 genes (Ausseil et al. 2008). This suggests an activation of microglia through this signaling pathway as a result of the accumulation of incomplete degradation products of HS.
Oxidative stress
Since lysosomes are highly susceptible to oxidative stress, alterations that occur in this organelle due to the accumulation of GAGs in MPS I could increase their susceptibility to an oxidative imbalance (Terman et al. 2006). It has been reported that mice lacking the gene for IDUA show an increase in superoxide dismutase and catalase in the cerebellum and peripheral organs, suggesting the presence of an oxidative stress in these cells (Reolon et al. 2009).
As we have previously discussed, in MPS I and other neurodegenerative LSDs, an inflammatory process on the CNS is believed to be involved in neuronal death through the pathological activation of microglia. This activation might trigger the release of neurotoxic substances such as reactive species from oxygen and nitrogen (Fig. 2). MPS I and MPS IIIB mice models have shown an increased expression of cytochrome b558 that is part of the NADPH oxidase complex, which is responsible for the oxidative burst of phagocytes (Simonaro et al. 2008). In MPS IIIB mice, an increased expression of components of the phagocyte NADPH oxidase was also observed in the brain and cerebellum (Villani et al. 2007).
The cerebellum, spleen and heart of IDUA knockout mice also presented a high formation of carbonyl groups on proteins, which were formed after reactive species attacked the protein backbone, compared to control mice (Reolon et al. 2009). This indication of protein damage was obtained despite the observed increase in antioxidant defense mentioned earlier. It is known that this effect can cause an autoimmune response through misidentification of those damaged proteins as exogenous ones, which in turn might trigger and/or enhance inflammation (Surh and Packer 2005).
Studies of MPS I patients have shown an increase in glutathione levels, responsible for the elimination of toxic peroxides, and malondialdehyde, an indicator of lipid peroxidation, compared with control subjects (Pereira et al. 2008).
These findings suggest the possibility that antioxidants might be included as part as current therapies for MPSs.
Lysosomal membrane permeabilization: change in intracellular ionic homeostasis and apoptosis
Studies of mice with MPS I show an alteration in the homeostasis of intracellular Ca2+ and H+ ions as well as an increase in the release into the cytoplasm of lysosomal cysteine-proteases and in the rate of cell death apoptosis (Pereira et al. 2010). Spleen cells of these animals were shown to release more Ca2+ from the lysosomes and endoplasmic reticulum than control mice, suggesting a higher intraorganelle store of this ion. Besides, a lower content of H+ in the lysosomes and in the cytosol was found in cells from diseased mice (Pereira et al. 2010).
Accumulation of undegraded or partially degraded substrates in the lysosomes of MPS I mice may lead to damage in the membrane of this organelle, leading to lysosomal membrane permeabilization. These alterations lead to an elevation of the pH in the organelle, which in turn may severely compromise the activity of other lysosomal hydrolases and vesicle trafficking mechanisms (Jentsch 2007) (Fig. 3). As a side effect, substrates and molecules not directly related to the primary enzyme deficiency may accumulate, as is the case with most LSDs.
Potential pathogenetic effects of lysosomal membrane permeabilization in MPS I cells. The increase in GAG (three wavy black lines) concentration inside the lysosomes could severely affect the integrity of its membrane. This has been demonstrated by a release of lysosomal proteases to the cytosol and the elevation of the organelle acidic pH. In addition, there is an increase in the release of Ca2+ from the endoplasmic reticulum that could represent a compensatory ion accumulation, as a result of compromised lysosome physiology and consequent cytosolic ionic alterations. Although these alterations and its negative effects have only been detected to date in IDUA deficient splenic cells, they could be contributing to diseases pathology in other tissues
Considering the higher release of Ca2+ and the lower concentration of H+ in the lysosomes of MPS I mice, it is possible that an impairment in the endocytic pathway may occur in these cells, contributing to the disease physiopathology, since both factors inhibit the fusion between early endosomes and late endosomes, and between late endosomes and lysosomes (Pryor et al. 2000) (Fig. 3). These alterations could also lead to a dysregulation of autophagy, probably caused by an impairment of autophagosome-lysosome fusion which requires lysosomal membrane integrity and ion homeostasis for vesicle transport, and thus increase autophagic substrates such as poly-ubiquitinated proteins and dysfunctional mitochondrias with high pathogenic potential (Pryor et al. 2000).
Blocking of autophagosome maturation has also been observed in MPS IIIA and other LSDs such as Danon’s disease, mucolipidosis type IV and multiple sulphatase deficiency (Ballabio and Gieselmann 2009).
Release of cysteine-proteases, such as cathepsins, to the cytosol due to lysosomal membrane permeabilization, leads to cleavage of a number of substrates which may trigger apoptotic signaling pathways, such as caspases and mitochondria-dependent processes, and may be the cause of the increased apoptotic activity observed in lymphocytes of IDUA-deficient mice (Boya and Kroemer 2008).
Storage of non-natural HS: alteration of cell signaling pathways
Besides its structural roles, HS and the proteoglycans they form at the cell surface and within the extracellular matrix are essential for cell signaling and distribution of growth factors, cytokines and morphogens (Bishop et al. 2007). HS molecules influence ligand-receptor interaction by stabilizing receptors at the cell surface and by direct binding and presentation of ligands to their respective receptor. Free HS within the extracellular matrix can also sequester humoral factors, thus modulating their biological effects (Clarke 2008). The growth factor/morphogen binding is determined by the degree and pattern of post-translational modifications of HS, particularly O-sulfation (Pye et al. 1998; Forsten-Williams et al. 2008).
GAGs that accumulate in a tissue-specific manner in MPS I patients consist of a combination of large, normally sized GAGs and partially degraded, smaller chains oligosaccharides (Ballabio and Gieselmann 2009; Hochuli et al. 2003). In addition, studies made in IDUA-deficient mice as well as in serum samples taken from untreated MPS I patients show that accumulated HS molecules are also structurally different in relation to its post-translational modifications (Holley et al. 2011).
These authors found that HS chains were shown to contain significantly increased N-, 2-O-, and 6-O-sulfation. Disaccharide analysis identified the presence of a non-reducing end disaccharide uniquely elevated in IDUA-deficient mice and MPS I patients. Different relative contributions of this disaccharide were seen between the liver and brain mice tissues, suggesting that it may represent a disease-specific disaccharide that accumulates at varying amounts in different tissues (Holley et al. 2011). Significantly, excess HS were also noted within the Golgi apparatus where it can influence HS biosynthesis directly. In deep, tissue extracts from IDUA deficient mice shown significantly increased N-deacetylase/N-sulfotransferase enzymatic activity, responsible for the first step in the HS modification pathway and ultimately defining the position of sulfate groups in clusters along the HS chain (Holley et al. 2011). So, excess HS acts as a positive regulator of HS-sulfation with the consequent accumulation of abnormal HS molecules at non-lysosomal sites. This has the potential to impact on HS-dependent signaling, dramatically altering cell functions (Fig. 4).
Alteration of cell signaling pathways due to modified HS storage in MPS I. Accumulation of GAGs and its incomplete degradation oligosaccharides products in MPS I cells is not restricted to the lysosomes, but also occurs in the extracellular matrix. In addition, HS storage (three wavy black lines) is also detected in the Golgi secretory pathway, and acts as a positive regulator of HS-sulfation (red circle), increasing the N-sulfotransferase activity of HS-modifying N-deacetylase/N-sulfotransferase enzymes (yellow diamond). HS molecules with increased sulfation in the extracellular matrix and the proteoglycans they form (HSPG) could impair cell response to different growth factor/cytokines. This is the case for FGF-2 (blue pentagon) and BMP-4 (dark green triangle superimposed on the left side of a light green triangle). Highly sulfated HSPG can not associate with FGF-2 and its receptor for proper signaling complex formation while its association with BMP-4 diminishes the union of this cytokine with its cell receptor. Impairment of activation of these receptors and the consecutive intracellular transduction pathways alters the cell response. This could contribute to neurodegeneration, defects in neurogenesis, axonal guidance and synapse as well as alterations in bone and cartilage tissues found in MPS I patients
-
1.
Impairment of signaling by FGF-2
The fibroblast growth factor (FGF) cytokine family affects cell growth, migration, differentiation, and neuroectodermal development. FGF-2, a prototypical member involved in tissue morphogenesis and neurogenesis, has two kinds of cell-surface receptors. Specific, high-affinity FGF receptors (FGFRs) possessing intrinsic tyrosine kinase activity mediate cellular responses, while low affinity receptors composed of HS proteoglycans (HSPGs) act as extracellular FGF-2 reservoirs and coreceptors (Powell et al. 2002). Although its mechanism of formation is unclear, the FGF-2-FGFR-HSPG complex is necessary for mitogenesis and optimal biologic response to FGF-2 (Krufka et al. 1996; Gallagher 2006).
Analyses made in multipotent adult progenitor cells (MAPCs) obtained from MPS I patients show that the structurally and functionally abnormal HS that accumulates in these patients perturbs critical FGF-2-FGFR1-HS interactions. Furthermore, FGF-2-induced proliferation and survival of MPS I MAPCs is defective (Pan et al. 2005) (Fig. 4).
Impairment of FGF-2 binding to Hurler MAPCs was also associated with defective mitogenic activity and survival-promoting activities of FGF-2 (Pan et al. 2005). Since FGF-2 acts as a proliferative agent and protector of several cell types, including neurons and their precursor cells (Alzheimer and Werner 2002), the deficiency in this signaling pathway may contribute to neurodegeneration of the disease and explain the increased rate of apoptosis seen in cells from patients (Ballabio and Gieselmann 2009). Proliferation of neural progenitor cells dependent on FGF-2 is also reduced in animal models of MPS IIIB and MPS VII, where partially degraded HS accumulate (Li et al. 2002; Walton and Wolfe 2007).
-
2.
Impairment of signaling by BMP-4
Bone morphogenetic proteins (BMPs) are a group of growth factors that regulate proliferation, differentiation and apoptosis in several tissues, including the nervous and skeletal (Kuo et al. 2010). BMP signaling is initiated by binding to specific type I and type II transmembrane serine/threonine kinase receptors. Type I receptors, activated by ligand-bound type II receptors, phosphorylate R-Smads proteins anchored to the cell membrane, which then complex with Co-Smads, translocate to the nucleus, and regulate gene expression in cooperation with other transcription factors (Miyazono et al. 2001).
It is recognized that the biological activities of bone morphogenetic proteins as well as their endogenous antagonists are regulated by extracellular matrix and cell surface HS proteoglycans. It is believed that specific sulfated residues in the GAG side chains bind to BMPs and their antagonists and thereby modulate receptor-mediated signaling, diffusion, and localization of these molecules (Takada et al. 2003).
Comparable to FGF-2; studies of MAPCs obtained from patients with severe MPS I phenotype indicate that abnormally accumulated GAGs impair BMP-4 signaling, which can be restored by enzymatic removal of these GAGs (Khan et al. 2008). Therefore, the alteration in this pathway probably contributes to the common joint and skeletal abnormalities as well as neurological abnormalities seen in patients with MPS I and other MPSs (Fig. 4).
Taken together, these studies suggest that impairment of cytokine/morphogen signaling and activity may be a common thread that contributes to the pathophysiology of the MPSs and has important implications for developing novel therapeutic agents.
Conclusions
In MPS I, a wide range of alterations in cell and tissue homeostasis occur secondary to the accumulation of GAGs due to its abnormal degradation. From current studies it is not yet possible to define a single pathological mechanism to integrate and explain the different findings observed in both animal models and patients with MPS I. However, the different mechanisms proposed independently may interact with each other and are not mutually exclusive. The complexity of defining a single pathological mechanism is understandable if one takes into account the wide variety of metabolic pathways and physiological processes involving GAGs and their related proteoglycans whose structures change with the accumulation of GAGs.
Pathological processes such as an impaired autophagy, activation of inflammation and alteration in ion homeostasis are not only linked to the development of MPS I, but also to other types of MPSs and even other LSDs in which there occurs a primary accumulation of other kind of macromolecules, such as complex lipids, oligosaccharides or glycopeptides, and not precisely GAGs. It seems that accumulation of undegraded substrates, regardless of their chemical nature, may lead to destabilization of the lysosome as a cellular organelle and produce deficiencies in different pathways such as: endosomal-lysosomal, retrosomal-lysosomal and lysosomal-autophagosomal. These are significantly involved in a wide range of cellular processes from signal transduction to synaptic plasticity and gene expression. In addition, lysosomes allow recycling of key molecules in synthetic and/or regulatory processes. Greater individual involvement of one of these pathways combined with the pathological effects caused by the presence of undegraded and altered substrates in the intracellular and extracellular environment, may define common pathogenic features and differences between various LSDs.
Other important thing to notice is the difficulty in translating in vitro and in vivo results to what could be truly happening in the human system as well as the limitations in the use of animal models. For example, the results obtained by Holley et al. (Holley et al. 2011), regarding an up-regulation of HS-sulfation in MPS I mice and patients directly contradict findings by Pan et al. (Pan et al. 2005) using MAPC cells. The fact that these cells were adapted to tissue culture prior analysis of HS chain composition could suggest that this analysis may not accurately reflect GAG structure in vivo.
Undoubtedly, understanding the precise pathogenic pathways involved in the development of MPS I and other LSDs would allow identification of new therapeutic targets to increase the efficiency of existing treatments and define novel ones.
References
Aldenhoven M, Boelens JJ, de Koning TJ (2008) The clinical outcome of Hurler syndrome after stem cell transplantation. Biol Blood Marrow Transplant 14:485–498
Alzheimer C, Werner S (2002) Fibroblast growth factors and neuroprotection. Adv Exp Med Biol 513:335–351
Ashworth JL, Biswas S, Wraith E, Lloyd IC (2006) Mucopolysaccharidoses and the eye. Surv Ophthalmol 51:1–17
Ausseil J, Desmaris N, Bigou S, Attali R, Corbineau S, Vitry S, Parent M, Cheillan D, Fuller M, Maire I, Vanier MT, Heard JM (2008) Early neurodegeneration progresses independently of microglial activation by heparan sulfate in the brain of mucopolysaccharidosis IIIB mice. PLoS One 3:e2296
Baehner F, Schmiedeskamp C, Krummenauer F, Miebach E, Bajbouj M, Whybra C, Kohlschütter A, Kampmann C, Beck M (2005) Cumulative incidence rates of the mucopolysaccharidoses in Germany. J Inherit Metab Dis 28:1011–1017
Ballabio A, Gieselmann V (2009) Lysosomal disorders: from storage to cellular damage. Biochim Biophys Acta 1793:684–696
Baumkötter J, Cantz M (1983) Decreased ganglioside neuraminidase activity in fibroblasts from mucopolysaccharidosis patients. Inhibition of the activity in vitro by sulfated glycosaminoglycans and other compounds. Biochim Biophys Acta 761:163–170
Ben Turkia H, Tebib N, Azzouz H, Abdelmoula MS, Ben Chehida A, Chemli J, Monastiri K, Chaabouni M, Sanhagi H, Zouari B, Kaabachi N, Ben Dridi MF (2009) Incidence of mucopolysaccharidoses in Tunisia. Tunis Med 87:782–785
Bishop JR, Schuksz M, Esko JD (2007) Heparan sulphate proteoglycans fine-tune mammalian physiology. Nature 446:1030–1037
Boor R, Miebach E, Brühl K, Beck M (2000) Abnormal somatosensory evoked potentials indicate compressive cervical myelopathy in mucopolysaccharidoses. Neuropediatrics 31:122–127
Boya P, Kroemer G (2008) Lysosomal membrane permeabilization in cell death. Oncogene 27:6434–6451
Castaneda JA, Lim MJ, Cooper JD, Pearce DA (2008) Immune system irregularities in lysosomal storage disorders. Acta Neuropathol 115:159–174
Clarke LA (2008) The mucopolysaccharidoses: a success of molecular medicine. Expert Rev Mol Med 10:1–18
de Ru MH, Boelens JJ, Das AM, Jones SA, van der Lee JH, Mahlaoui N, Mengel E, Offringa M, O’Meara A, Parini R, Rovelli A, Sykora KW, Valayannopoulos V, Vellodi A, Wynn RF, Wijburg FA (2011) Enzyme replacement therapy and/or hematopoietic stem cell transplantation at diagnosis in patients with mucopolysaccharidosis type I: results of a European consensus procedure. Orphanet J Rare Dis 6:55
Desmaris N, Verot L, Puech JP, Caillaud C, Vanier MT, Heard JM (2004) Prevention of neuropathology in the mouse model of Hurler syndrome. Ann Neurol 56:68–76
Forsten-Williams K, Chu CL, Fannon M, Buczek-Thomas JA, Nugent MA (2008) Control of growth factor networks by heparan sulfate proteoglycans. Ann Biomed Eng 36:2134–2148
Gabrielli O, Polonara G, Regnicolo L, Petroni V, Scarabino T, Coppa GV, Salvolini U (2004) Correlation between cerebral MRI abnormalities and mental retardation in patients with mucopolysaccharidoses. Am J Med Genet A 125A:224–231
Gallagher JT (2006) Multiprotein signalling complexes: regional assembly on heparin sulphate. Biochem Soc Trans 34:438–441
Giussani C, Miori S, Sganzerla EP (2010) Neurological complications and their management in Mucopolysaccharidosis. In: Parini R, Andria G (eds) Lysosomal storage diseases: early diagnosis and new treatments. John Libbey Eurotext, Montrouge (France), pp 107–120
Hochuli M, Wüthrich K, Steinmann B (2003) Two-dimensional NMR spectroscopy of urinary glycosaminoglycans from patients with different mucopolysaccharidoses. NMR Biomed 16:224–236
Hoffmann B, Mayatepek E (2005) Neurological manifestations in lysosomal storage disorders-from pathology to first therapeutic possibilities. Neuropediatrics 36:285–289
Holley RJ, Deligny A, Wei W, Watson HA, Niñonuevo MR, Dagälv A, Leary JA, Bigger BW, Kjellén L, Merry CL (2011) Mucopolysaccharidosis type I, unique structure of accumulated heparan sulfate and increased N-sulfotransferase activity in mice lacking α-l-iduronidase. J Biol Chem 286:37515–37524
Jentsch TJ (2007) Chloride and the endosomal-lysosomal pathway: emerging roles of CLC chloride transporters. J Physiol 578:633–640
Jmoudiak M, Futerman AH (2005) Gaucher disease: pathological mechanisms and modern management. Br J Haematol 129:178–188
Johnson GB, Brunn GJ, Kodaira Y, Platt JL (2002) Receptor-mediated monitoring of tissue well-being via detection of soluble heparan sulfate by Toll-like receptor 4. J Immunol 168:5233–5239
Khan SA, Nelson MS, Pan C, Gaffney PM, Gupta P (2008) Endogenous heparan sulphate and heparin modulate bone morphogenetic protein-4 (BMP-4) signalling and activity. Am J Physiol Cell Physiol 294:C1387–C1397
Krufka A, Guimond S, Rapraeger AC (1996) Two hierarchies of FGF-2 signaling in heparin: mitogenic stimulation and high-affinity binding/receptor transphosphorylation. Biochemistry 35:11131–11141
Kuo WJ, Digman MA, Lander AD (2010) Heparan sulfate acts as a bone morphogenetic protein coreceptor by facilitating ligand-induced receptor hetero-oligomerization. Mol Biol Cell 21:4028–4041
Li HH, Zhao HZ, Neufeld EF, Cai Y, Gómez-Pinilla F (2002) Attenuated plasticity in neurons and astrocytes in the mouse model of Sanfilippo syndrome type B. J Neurosci Res 69:30–38
Liour SS, Jones MZ, Suzuki M, Bieberich E, Yu RK (2001) Metabolic studies of glycosphingolipid accumulation in mucopolysaccharidosis IIID. Mol Genet Metab 72:239–247
Liu Y, Xu L, Hennig AK, Kovacs A, Fu A, Chung S, Lee D, Wang B, Herati RS, Mosinger Ogilvie J, Cai SR, Parker Ponder K (2005) Liver-directed neonatal gene therapy prevents cardiac, bone, ear, and eye disease in mucopolysaccharidosis I mice. Mol Ther 11:35–47
Lowry RB, Applegarth DA, Toone JR, MacDonald E, Thunem NY (1990) An update on the frequency of mucopolysaccharide syndromes in British Columbia. Hum Genet 85:389–390
Malm G, Lund AM, Månsson JE, Heiberg A (2008) Mucopolysaccharidoses in the Scandinavian countries: incidence and prevalence. Acta Paediatr 97:1577–1581
Matheus MG, Castillo M, Smith JK, Armao D, Towle D, Muenzer J (2004) Brain MRI findings in patients with mucopolysaccharidosis types I and II and mild clinical presentation. Neuroradiology 46:666–672
McGlynn R, Dobrenis K, Walkley SU (2004) Differential subcellular localization of cholesterol, gangliosides, and glycosaminoglycans in murine models of mucopolysaccharide storage disorders. J Comp Neurol 480:415–426
Meikle PJ, Hopwood JJ, Clague AE, Carey WF (1999) Prevalence of lysosomal storage disorders. JAMA 281:249–254
Menéndez-Sainz C, González-García S, Peña-Sánchez M, Zaldívar-Muñoz C, González-Quevedo A (2009) Mucopolisacaridosis: diagnóstico enzimático de 20 años en Cuba. Rev Neurol 49:458–462
Miyazono K, Kusanagi K, Inoue H (2001) Divergence and convergence of TGF-beta/BMP signaling. J Cell Physiol 187:265–276
Moore D, Connock MJ, Wraith E, Lavery C (2008) The prevalence of and survival in Mucopolysaccharidosis I: Hurler, Hurler-Scheie and Scheie syndromes in the UK. Orphanet J Rare Dis 3:24
Mulloy B, Rider CC (2006) Cytokines and proteoglycans: an introductory overview. Biochem Soc Trans 34:409–413
Neufeld EF, Muenzer J (2001) The mucopolysaccharidoses. In: Scriver C, Beaudet A, Sly WS, Valle D (eds) The metabolic and molecular bases of inherited disease, 8th edn. McGraw Hill, New York, pp 3421–3452
Ohmi K, Greenberg DS, Rajavel KS, Ryazantsev S, Li HH, Neufeld EF (2003) Activated microglia in cortex of mouse models of mucopolysaccharidoses I and IIIB. Proc Natl Acad Sci U S A 100:1902–1907
Pan C, Nelson MS, Reyes M, Koodie L, Brazil JJ, Stephenson EJ, Zhao RC, Peters C, Selleck SB, Stringer SE, Gupta P (2005) Functional abnormalities of heparan sulfate in mucopolysaccharidosis-I are associated with defective biologic activity of FGF-2 on human multipotent progenitor cells. Blood 106:1956–1964
Parish CR (2006) The role of heparan sulphate in inflammation. Nat Rev Immunol 6:633–643
Parkinson-Lawrence EJ, Shandala T, Prodoehl M, Plew R, Borlace GN, Brooks DA (2010) Lysosomal storage disease: revealing lysosomal function and physiology. Physiology (Bethesda) 25:102–115
Pereira VG, Martins AM, Micheletti C, D’Almeida V (2008) Mutational and oxidative stress analysis in patients with mucopolysaccharidosis type I undergoing enzyme replacement therapy. Clin Chim Acta 387:75–79
Pereira VG, Gazarini ML, Rodrigues LC, da Silva FH, Han SW, Martins AM, Tersariol IL, D’Almeida V (2010) Evidence of lysosomal membrane permeabilization in mucopolysaccharidosis type I: rupture of calcium and proton homeostasis. J Cell Physiol 223:335–342
Powell AK, Fernig DG, Turnbull JE (2002) Fibroblast growth factor receptors 1 and 2 interact differently with heparin/heparan sulfate. Implications for dynamic assembly of a ternary signaling complex. J Biol Chem 277:28554–28563
Prinetti A, Prioni S, Chiricozzi E, Schuchman EH, Chigorno V, Sonnino S (2011) Secondary alterations of sphingolipid metabolism in lysosomal storage diseases. Neurochem Res 36:1654–1668
Pryor PR, Mullock BM, Bright NA, Gray SR, Luzio JP (2000) The role of intraorganellar Ca(2+) in late endosome-lysosome heterotypic fusion and in the reformation of lysosomes from hybrid organelles. J Cell Biol 149:1053–1062
Pye DA, Vives RR, Turnbull JE, Hyde P, Gallagher JT (1998) Heparan sulfate oligosaccharides require 6-O-sulfation for promotion of basic fibroblast growth factor mitogenic activity. J Biol Chem 273:22936–22942
Reolon GK, Reinke A, de Oliveira MR, Braga LM, Camassola M, Andrades ME, Moreira JC, Nardi NB, Roesler R, Dal-Pizzol F (2009) Alterations in oxidative markers in the cerebellum and peripheral organs in MPS I mice. Cell Mol Neurobiol 29:443–448
Resnick JM, Whitley CB, Leonard AS, Krivit W, Snover DC (1994) Light and electron microscopic features of the liver in mucopolysaccharidosis. Hum Pathol 25:276–286
Schumacher RG, Brzezinska R, Schulze-Frenking G, Pitz S (2008) Sonographic ocular findings in patients with mucopolysaccharidoses I, II and VI. Pediatr Radiol 38:543–550
Simonaro CM, D’Angelo M, Haskins ME, Schuchman EH (2005) Joint and bone disease in mucopolysaccharidoses VI and VII: identification of new therapeutic targets and biomarkers using animal models. Pediatr Res 57:701–707
Simonaro CM, D’Angelo M, He X, Eliyahu E, Shtraizent N, Haskins ME, Schuchman EH (2008) Mechanism of glycosaminoglycan-mediated bone and joint disease: implications for the mucopolysaccharidoses and other connective tissue diseases. Am J Pathol 172:112–122
Surh YJ, Packer L (2005) Oxidative stress, inflammation, and health. Taylor and Francis, London
Takada T, Katagiri T, Ifuku M, Morimura N, Kobayashi M, Hasegawa K, Ogamo A, Kamijo R (2003) Sulfated polysaccharides enhance the biological activities of bone morphogenetic proteins. J Biol Chem 278:43229–43235
Terlato NJ, Cox GF (2003) Can mucopolysaccharidosis type I disease severity be predicted based on a patient’s genotype? A comprehensive review of the literature. Genet Med 5:286–294
Terman A, Kurz T, Gustafsson B, Brunk UT (2006) Lysosomal labilization. IUBMB Life 58:531–539
Tomatsu S, Gutierrez MA, Ishimaru T, Peña OM, Montaño AM, Maeda H, Velez-Castrillon S, Nishioka T, Fachel AA, Cooper A, Thornley M, Wraith E, Barrera LA, Laybauer LS, Giugliani R, Schwartz IV, Frenking GS, Beck M, Kircher SG, Paschke E, Yamaguchi S, Ullrich K, Isogai K, Suzuki Y, Orii T, Noguchi A (2005) Heparan sulfate levels in mucopolysaccharidoses and mucolipidoses. J Inherit Metab Dis 28:743–757
Tomatsu S, Montaño AM, Oguma T, Dung VC, Oikawa H, Gutiérrez ML, Yamaguchi S, Suzuki Y, Fukushi M, Barrera LA, Kida K, Kubota M, Orii T (2010) Validation of disaccharide compositions derived from dermatan sulfate and heparan sulfate in mucopolysaccharidoses and mucolipidoses II and III by tandem mass spectrometry. Mol Genet Metab 99:124–131
Villani GR, Gargiulo N, Faraonio R, Castaldo S, Gonzalez Y, Reyero E, Di Natale P (2007) Cytokines, neurotrophins, and oxidative stress in brain disease from mucopolysaccharidosis IIIB. J Neurosci Res 85:612–622
Vitner EB, Platt FM, Futerman AH (2010) Common and uncommon pathogenic cascades in lysosomal storage diseases. J Biol Chem 285:20423–20427
Walkley SU (2003) Neurobiology and cellular pathogenesis of glycolipid storage diseases. Philos Trans R Soc Lond B 358:893–904
Walkley SU (2004a) Secondary accumulation of gangliosides in lysosomal storage disorders. Semin Cell Dev Biol 15:433–444
Walkley SU (2004b) Pathogenic cascades and brain dysfunction. In: Platt FM, Walkley SU (eds) Lysosomal disorders of the brain. Oxford University Press, Oxford, pp 32–49
Walkley SU (2009) Pathogenic cascades in lysosomal disease-Why so complex? J Inherit Metab Dis 32:181–189
Walkley SU (2007) Pathogenic mechanisms in lysosomal disease: a reappraisal of the role of the lysosome. Acta Paediatr Suppl 96:26–32
Walkley SU, Zervas M, Wiseman S (2000) Gangliosides as modulators of dendritogenesis in normal and storage disease-affected pyramidal neurons. Cereb Cortex 10:1028–1037
Walton RM, Wolfe JH (2007) Abnormalities in neural progenitor cells in a dog model of lysosomal storage disease. J Neuropathol Exp Neurol 66:760–769
Wang D, Shukla C, Liu X, Schoeb TR, Clarke LA, Bedwell DM, Keeling KM (2010) Characterization of an MPS I-H knock-in mouse that carries a nonsense mutation analogous to the human IDUA-W402X mutation. Mol Genet Metab 99:62–71
Yuen A, Dowling G, Johnstone B, Kornberg A, Coombs C (2007) Carpal tunnel syndrome in children with mucopolysaccharidoses. J Child Neurol 22:260–263
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Campos, D., Monaga, M. Mucopolysaccharidosis type I: current knowledge on its pathophysiological mechanisms. Metab Brain Dis 27, 121–129 (2012). https://doi.org/10.1007/s11011-012-9302-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-012-9302-1