Abstract
In the present study we investigated the effect of the non-alcoholic fatty liver disease (NAFLD) on the alterations in the activity of neurotransmitters catabolizing enzymes and energy catabolising enzymes, prooxidants, endogenous antioxidants and proinflammatory cytokines in brain tissue of NAFLD rats. Rats were intraperitonealy injected with CCl4 solution at a dose of (0.021 mole/Kg, 20 μL, body weight) three times weekly for four weeks. Acetylcholine esterase (AChE), monoamine oxidase (MAO), prooxidant/ antioxidants status, ATPase, lipid profile and glucose level were estimated spectrophotometrically while inflammatory markers; interleukin 6 and tumor necrosis factor alpha (IL6 and TNF-α) and insulin were assessed by ELISA technique. Our results showed that the induced NAFLD and insulin resistance (IR) were accompanied with hyperglycemia and hyperlipidemia and lowered brain glucose level with elevated ATPase activity, prooxidant status (TBARS level, xanthine oxidase and cytochrome 2E1 activities), and inflammatory markers. Through the induction period AChE activity was significantly increased compared to control in blood, liver and brain tissues. Also, MAO activity was significantly increased in both brain and liver tissue but decreased in serum compared with control. These biochemical data were supported with pathophysiological analysis that showed severe neurodegeneration, pyknosis acuolations and cavitations. These observations warrant the reassessment of the conventional concept that the NAFLD with IR progression may induce disturbances in activities of neurotransmitters catabolising enzymes and energy production accompanied with oxidative stress and metabolic disorders, acting as relative risk factors for brain dysfunction and damage with the development of age-associated neurodegenerative diseases such as Alzheimer's disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is ranging from simple steatosis (lipid accumulation in liver, mainly triglycerides) to steatohepatitis (NASH) accompanied with various metabolic syndromes inform of insulin resistance, increased risk of type 2 diabetes, and cardiovascular diseases due to lipoperoxidative stress pathway stimulation (Marchesini et al. 2003; Eckel et al. 2005; Musso et al. 2009).
Insulin plays an important role in brain functions through glucose uptake modulation in central nervous system (CNS) (Bingham et al. 2002). It also modulates levels of classic neurotransmitters such as acetylcholine (ACh) and affects membrane potentials, neuronal physiology, and long-term potential, all of which influences the synaptic remodelling processes thought to underlie memory formation (Craft and Watson 2004; Watson and Craft 2006; Angelini et al. 2010). Thus, insulin may modulate cognitive functions through effects on neurotransmission.
Moreover, insulin resistance and chronic hyperinsulinemia down-regulate the insulin transport to brain with brain insulin deficient state which associated with age related memory impairments and Alzheimer’s disease (AD) (Baura et al. 1996; McGarry and Dobbins 1999; Neuschwander-Tetri et al. 2003; Sanyal et al. 2001; Biessels and Kappalle 2005; Craft 2005). Defects in insulin signalling and peripheral insulin resistance have been linked to intrahepatocellular lipid accumulation (McGarry 2002). The oversupply of lipid to peripheral tissues might contribute to the development of insulin resistance through the increased availability of lipids (in form of free fatty acids and elevated intracellular lipids) to peripheral tissues induces insulin resistance by promoting the accumulation of one or more fat-derived metabolites capable of inhibiting insulin action (Chavez and Summers 2003; McGarry 2002).
Such mechanism had evidenced a particularly tight inverse correlation between intrahepatic triglyceride contents and insulin sensitivity measured by whole body glucose disposal during euglycemic-hyperinsulinemic clamp (Hwang et al. 2007; Korenblat et al. 2008). Consequently, reduction of intrahepatic lipid contents (80%) by a moderately hypocaloric very-low-fat diet (3%) in patients with obesity and T2DM enhanced insulin sensitivity by normalizing insulin suppression of hepatic glucose production but had no effects on peripheral insulin sensitivity (Petersen et al. 2005).
Insulin resistance and subsequent hyperinsulinemia may result in alterations in the hepatic pathways of uptake, synthesis, degradation, and secretion of free fatty acids (Browning and Horton 2004) This overloading of the liver with lipids is believed to render the liver more susceptible to a “second or multiple hits,’ which then results in liver damage and disease progression (Day and James 1998; Diehl 2002; McCullough 2004).
Moreover, TNF-α and other proinflammatory cytokines have central role in the development of obesity-associated insulin resistance and fatty liver by inhibition of insulin-stimulated glucose disposal, (Plomgaard et al. 2005) and certain TNF-α polymorphisms are associated with susceptibility to insulin resistance and NAFLD, (Valenti et al. 2002; Tokushige et al. 2007) supporting the importance of this cytokine in the interaction among inflammation, insulin signaling, and fat accumulation.
The molecular events resulting in intrahepatic lipid accumulation and growth of lipid droplets are poorly understood, but may arise from (1) increased uptake of lipids, (2) elevated de novo synthesis of fatty acids, (3) impaired lipoprotein synthesis or secretion, and/or (4) reduced fatty acid oxidation (Farrell and Larter 2006). Moreover, NAFLD is a very serious disorder leading to hepatic failure and encephalopathy due to increased ammonia production, false neurotransmitters, activation of benzodiazepine receptor and oxidative stress (Angulo 2007; Johansen et al. 2007).
Carbon tetrachloride (CCl4), tetrachloromethane, is a well-established hepatotoxin, which is widely used to study the mechanism of toxic liver injury such as acute necrosis and chronic fibrosis in laboratory animals (Yu et al. 2002). CCl4 is reductively bioactivated by cytochrome P450 2E1 into a trichloromethyl radical (•CCl3), which, in the presence of oxygen, is subsequently converted into a peroxyl radical (•OOCCl3) (Weber et al. 2003). Once the free radical is formed, it reacts with various biologically important substances such as amino acids, nucleic acids, and lipids then causes lipid peroxidation, membrane damage, and loss of hepatocellular calcium homeostasis. Oxidative stress induces tissue inflammation and necrosis which in turn alters cell membrane permeability, integrity and structure leading to cell membrane damage (Choudhary et al. 1996).
Our previous studies showed that the increase in brain oxidative stress status such as resulting from diabetes or long term lead exposure altered brain acetylcholine esterase (AChE) activity (Ghareeb and Hussein 2008; Ghareeb et al. 2010a). Furthermore, it was reported that oxidative damage to rat synapses contributes to cognitive deficits (Hsu and Guo 2002).
Monoamine oxidase (MAO), an enzyme that catalyzes the oxidation of monoamines, is vital to the inactivation of monoaminergic neurotransmitters such as dopamine, noradrenaline and serotonin (Hare 1928). It has been found an association between NAFLD progression and the increase in the activity of MAO. Furthermore, the MAO activity alteration is linked with increased reactive oxygen species (ROS) production. MAO dysfunction is thought to be responsible for a number of neurological disorders and have recently received attention with regard to aging and age-related diseases like AD and others. In addition, mitochondria are responsible for adenosine triphosphate (ATP) metabolism because it produces ATP through the oxidative phosphorylation, and degrades ATP through the ATPase action (Calabrese et al. 2001). Brain contains a large number of mitochondria. It is well demonstrated that mitochondria dysfunction is implicated in the pathogenesis of a number of diseases (Beal 2005).
In the present study we investigated the correlation between the induction and progression of NAFLD to insulin resistance and its subsequent risk factors for brain tissue dysfunction through studying oxidative stress incidence that could lead to alteration in the activity of proinflammatory molecules, energy levels and neurotransmitter catabolising enzymes.
Materials and methods
Materials
CCl4, NAD+, Dimethylaminobenzylaldehyde reagent, Inorganic pyrophosphatase (PPase), Tris–HCl, 2-(N-morpholino) ethane sulphonic acid (Mes), Pyrophosphate, Methyl green, triton X-305, Thiobarbituric acid (TBA), Cumene H2O2, Reduced glutathione (GSH), 5,5′-dithiobis 2-nitrobrnzoic acid (DTNB), p-Hydroxydiphenyl, Trichloroacetic acid, Acetaldehyde, Sodium tungstate, Foline reagent, Xanthine, Benzylamine, ATP, Acetylthiocholine iodide (ACTI) were purchased from Sigma Chemical Company (St. Louis, Mo, USA). Rat TNF-α, IL-6 and insulin kits were purchased from BioVision, USA. All the other reagents were of analytical grade and highest purity commercial kits (Diamon, Egypt).
Methods
Animals and experimental design
All animal procedures were performed according to the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (Institute of Laboratory Animal Resources 1996). Female Sprague–Dawley rats (weighed from 200 to 250 g) were obtained from the animal house of Faculty of Medicine, Alexandria University, Egypt. The rats were maintained at approximately 23–25°C with a 12-h light/dark cycle and received basal diet and tap water for 1 week (acclimation period).
CCl4 was mixed with a concentration of 1.6% (V/V) in olive oil for administration according to standard protocol. After a period of acclimation, 30 rats were housed in metal standard cages, and then divided into two experimental groups as follows: Group 1 (control): consisted of six rats which were intraperitonealy injected with olive oil as vehicle (1.2 mL/Kg) three times weekly for 4 weeks and served as untreated control group. Group 2 (NAFLD induced groups) which consisted of 24 rats; . This group was subdivided into four groups, first week group; was administered CCl4 for 1 week, second week group; received CCl4 for 2 weeks, third week group; injected with CCl4 for 3 weeks and finally fourth week group was intraperitonealy administered CCl4 for 4 weeks. The first and second week groups represented the NAFLD induction groups while the third and fourth week groups represented the NAFLD progression groups. By the end of each induction period rats were sacrificed after anesthesia with diethylether inhalation, blood was collected and sera were separated to measure the lipid profile, insulin resistance markers while brain and liver tissues were quickly removed and placed in chilled phosphate buffer, pH 7.4. The tissue was freed from adhering blood by repeated washing with the same buffer. Brain and liver tissues were subdivided into to longitude section one part was fixed in 10% formalin for histological study while the other part was frozen at −80°C until further investigations.
Preparation of lipid supernatant
0.1 g of brain tissue was homogenized with 1 mL of chloroform-methanol mixture (2:1, v/v) using polytron. The homogenate was centrifuged at 2500 rpm for 15 min then the supernatant was obtained. The residue was washed with 1 mL solvent mixture, vortexed, centrifuged and then the supernatants were combined, stored at −20°C.
Preparation of tissue supernatant
Brain and liver tissues were weighed and homogenized directly in nine volumes of cold phosphate buffer using Potter-Elvehjem type glass-Teflon homogenizer. To separate the nuclear debris, the tissue homogenates were centrifuged at 3000 rpm for 15 min at 4°C. Brain supernatant was used for determination of insulin, AChE, MAO, lipid peroxidation, GSH, GPx, XO, TNF-α, IL6, cytochrome 2E1, ATPase, Pi and PPi. Liver supernatant was used for determination of AChE and MAO activities.
Estimation of brain total lipid
Ten microlitre of lipid supernatant, standard solution or distilled water was added to 2 mL H2SO4 and mixed well. The tubes were covered with marble and let to stand in boiling water bath for 10 min then cooled. In another four test tubes, 50 μL of pervious solutions were mixed to 1.5 mL color reagent (phosphoric acid, 14 M and vaniline, 10 mM) and let to stand at room temperature for 30 min. The absorbance was measured at 530 nm against blank (Zollner and Kirsch 1962).
Determination of serum and brain triglycerides (TG) and cholesterol
Ten microlitre of serum or lipid supernatant or standard TG solution was added to 1 mL colour reagent and the tubes were incubated at 25°C for 10 min. The absorbance was measured at 500 nm against blank (Fossati and Prencipe 1982). While, estimation of serum and brain cholesterol was carried out as follow, 10 μL of serum or lipid supernatant or standard cholesterol solution was added to 1 mL color reagent, and then incubated at 25°C for 10 min. The absorbance was measured at 500 nm against blank reagent (Watson 1960).
Determination of serum and brain glucose level
In three test tubes, 10 μL serum or brain supernatant, 10 μL standard or 10 μL water was added to 1 mL working reagent and mixed well. All test tubes were incubated at 25°C for 20 min. The absorbances of standard (As) and test (At) were read against blank at 505 nm (Hjelm and De Verdier 1963).
Determination of brain total protein concentration
In two test tubes, 10 μL brain supernatant or water were added to 4 mL working biuret reagent and vortex for 1 min then incubated for 10 min at room temperature. Foline- Ciocalteau, 125 μL was added to the mixtures then all test tubes were incubated for 30 min at room temperature. The absorbance was read against blank at 759 nm (Plummer 1978).
Estimation of brain lipid peroxidation
The malondialdehyde content, a measure of lipid peroxidation, was assayed in the form of thiobarbituric acid-reactive substances by the method described by Wills (1965). Briefly, 500 μL of brain supernatant was added to 1 mL TCA and mixed well then the solutions were centrifuged at 3000 rpm for 10 min. One milliliter of the supernatant was added to 0.5 mL of TBA and boiled for 10 min in boiling water bath then cooled. The absorbance of serum or homogenate was read at 532 nm against blank.
For tissue TBARS level (nmol/g wet tissue) = at/0.156 × 10, Where; the sample dilution was ten.
Determination of endogenous antioxidants in brain such as, glutathione peroxidase (Gpx), reduced glutathione (GSH), xanthine oxidase (XO) activities: Glutathione peroxidase (Gpx)
Fifty microlitre brain supernatant was added to 100 μL GSH (GSH, 5 mg was dissolved in 10 mL Tris–HCl buffer, 50 mM, pH 7.6), 100 μL cumene H2O2 (cumene H2O2, 50 μL was mixed with 10 mL Tris–HCl buffer, 50 mM, pH 7.6) and 750 μL Tris–HCl and incubated at 37°C for 10 min. One mL TCA (15%) was added centrifuged at 3000 rpm for 20 min and then the supernatants were separated off. One mL supernatant was added to 2 mL Tris–HCl, 0.4 mM, pH 8.9 and 100 μL DTNB (DTNB, 0.0198 g was dissolved in 5 mL methanol) and incubated for 5 min. The absorbance was measured at 412 nm against distilled H2O. The activity of GPx was calculated according to Paglia and Valentine (1967) with the following equation: \( {\text{GPx activity}}\left( {{\text{U}}/{\text{g wet tissue}}} \right) = {\text{A}} \times {6}.{2} \times {1}00/{13}.{1} \times 0.0{5} \times {1}0 \). Reduced glutathione (GSH) was assayed by the method of Jollow et al. (1974). Briefly, 0.1 mL of brain supernatant (10%) was precipitated with 0.1 mL of 4% sulphosalicylic acid. The samples were kept at 4°C for at least 1 h and then subjected to centrifugation at 1200×g for 10 min at 4°C. The assay mixture contained 0.1 mL supernatant, 2.7 mL phosphate buffer (0.1 M, pH 7.4) and 0.2 mL DTNB (0.1 mM, pH 8) in a total volume of 3 mL. The yellow color developed was measured immediately at 412 nm. Xanthine oxidase (XO) activity: In two test tube, 30 μL buffer and 60 μL water (control) or stock solution (test) [Xanthine,0.038 M, dissolved in distilled water by adding alkali and gentle heating then 1: 125 dilution of stock is used] was added to 0.5 mL brain supernatant and incubated for 40 min at 37°C. 0.1 mL of this solution was mixed with 0.1 mL Na- tungstate, 0.5 mL water and 0.1 mL H2SO4 complete to 1 mL and incubated for 1 h at 37°C then centrifuged at 3000 rpm for 10 min. 0.15 mL of supernatant was mixed with 0.75 mL water and 0.3 mL Foline reagent and 1.5 mL Na-carbonate and absorbance was measured at 650 nm (Montgomery and Dymock 1961). Activity of xanthine oxidase was determined using the following equation; Concentration of xanthine in control or test = A/A s * concentration of standard*480
Xanthine oxidase activity (μmole/h/g tissue) = (Concentration of control-concentration of test)/0.284* xanthine M.Wt.
Determination of brain adenosine triphosphatase (ATPase) activity
Two hundred microlitre buffer (5 mM MgCl2, 80 mM NaCl, 20 mM KCl, 40 mM Tris–HCl buffer, pH 7.4) was added to 20 μL brain supernatant and preincubated for 5 min at 37°C. Then 20 μL ATP (10 mM) was added and incubated for 30 min. To the solution, 200 μL TCA (10%) was added and centrifuged at 3000 rpm, for 10 min. To 50 μL of supernatant, 5 mL ammonium molybdate- methyl green mixture (5.8 mL molybdate, 1.7 mL methyl green, and 1.3 triton X305/NaOH and 1 mL water) was added, mixed well and incubated for 10 min at room temperature. Absorbance of samples and standards were measured at 630 nm against blank (Litwack et al. 1953). Enzyme specific activities were expressed as nmol Pi released/min/mg protein.
Estimation of supernatant pyrophosphate (PPi)
One hundred microlitre of brain supernatant was added to 100 μL Mes [2-(N-morpholino) ethane sulphonic acid (Mes)/sodium fluoride (0.2 M/0.1 M), pH 5.8] and 5 μL PPase solution [Inorganic pyrophosphatase (PPase)/MgCL2/Tris–HCl (50 U/ml/40 mM/0.1 M), pH 7], mixed well and incubated for 15 min at 25°C (incubation mixture). Fifty microlitre of incubation mixtures were added to 5 mL solution 4 [Tris/MgCl2/pyrophosphate (0.05 M, pH 8.5/0.2 mM/0.5 mM)] and 5 mL ammonium molybdate- methyl green mixture (5.8 mL molybdate, 1.7 mL methyl green, and 1.3 triton ×305/NaOH and 1 mL water), mixed well and incubated for 10 min at room temperature. The absorbances of samples and standards were measured at 630 nm against blank (Candeiasa et al. 2009). The concentration of pyrophosphate was calculated with the following equation; \( {\text{PPi concentration}}\left( {{\text{mg}}/{\text{dl}}} \right) = {\text{At}}/{\text{As}} \times {\text{concentration of standard}} \).
Estimation of brain inorganic phosphate (Pi)
Eight hundred microlitre of blank reagent (sulphuric acid, 0.36 M and NaCl, 154 mM) was added to 40 μL brain supernatant. Then 400 μL of phosphorus reagent (ammonium molybdate, 3.5 mM, H2SO4, 0.36 mM and NaCl, 154 mM) was added and incubated for 5 min at 37°C. The absorbances of standard and test were measured at 340 nm against blank (Drake et al. 1979). The sample Pi level was calculated with the following equation; \( {\text{Sample Pi }}\left( {{\text{mg}}/{\text{dl}}} \right) = {\text{At}}/{\text{As}} \times {\text{concentration of standard}} \).
Determination of Cytochrome 2E1 (CYP2E1)
CYP2E1 activity was determined in brain supernatant by the hydroxylation of aniline into p-aminophenol (Srivastava et al. 2002; Robin et al. 2005). The p-aminophenol was converted into a blue complex with an absorption peak at 630 nm.
Estimation of AChE and MAO activities
AChE was measured according to Ellman et al. (1961). The assay system contained, in a final volume of 1 mL: 100 mM phosphate buffer, pH 8, 75 mM ACTI. The brain, liver supernatant or serum was pre-incubated with the assay medium for 15 min at 37°C, then added 0.32 mM DTNB as a second substrate. The reaction was started by the addition of DTNB then the increase in absorbance at 412 nm was recorded for 5 min at 37°C with 5 s intervals. While MAO activity: 667 μl of 500 μM p-tyramine and 133 μl potassium phosphate buffer pH 7.6 were added to 100 μl brain, liver supernatant or sreum. The absorbance was measured at 250 nm against air after 30 s and 90 s. The activity of MAO was calculated according to Sandler et al. (1981) with the following equation: \( {\text{MAO activity}}\left( {{\text{U}}/{\text{l}}} \right) = \Delta {\text{A}} \times {\text{total volume}} \times {1}000/{32}.{2} \times {\text{sample volume}} \times 0.{5} \).
Determination of TNF-α and IL-6 in brain supernatant
Assayed by the method described in the commercial TNF-α ELISA kit purchased from Ray Biotech, USA. The TNF-α level was carried out by the enzyme-linked immunosorbent assay (ELISA), using the anti-Rat TNF-α precoated microplates (12 × 8 microwell strips). Absorbance was measured immediately at 450 nm against blank using an ELISA reader (BioTek, USA). IL-6 in brain supernatant: Assayed by the method described in the commercial IL-6 ELISA kit purchased from RayBiotech, USA. The IL-6 was determined by ELISA using the anti-Rat IL-6 pre-coated microplates (12 × 8 microwell strips) following the above mentioned procedure in TNF- α.
Determination of insulin in serum and brain supernatant
Twenty five microlitre of standard, control, serum or brain supernatant was dispensed into appropriate wells, then 25 μl enzyme conjugate (mouse monoclonal anti- insulin conjugated to biotin) was dispensed into each well and incubated for 30 min at room temperature. The wells were rinsed three times with diluted wash solution. Fifty microlitre of enzyme complex (Streptavidin HRP Complex) was added to each well then were incubated for 30 min at room temperature. The wells were rinsed three times with diluted wash solution. Fifty microlitre of substrate solution (TMB) was added to each well then incubated for 15 min at room temperature. The enzymatic reaction was stopped by adding 50 μl of stop solution (0.5 M H2SO4) to each well. OD was read at 450 nm with a microtiter plate reader within 10 min after adding the stop solution.
Calculation of HOMA-IR and HOMA-β
The homeostatic model assessment (HOMA) was used to quantify insulin resistance and beta-cell function, this model was calculated by the following equation; \( {\text{HOMA}} - {\text{IR}} = \left( {{\text{Glucose}}\left( {{\text{mg}}/{\text{dL}}} \right)*{\text{Insulin}}\left( {{\text{pg}}/{\text{mL}}} \right)} \right)/{4}0{5} \) \( {\text{HOMA}} - \beta \% = \left( {{36}0*{\text{Insulin}}/{\text{Glucose}} - {63}} \right) \).
Histopathological examination
Hematoxylin-eosin stain was used for liver and brain cells: Portions of liver or brainwere fixed in 10% neutral buffered formalin for 48 h. Specimens were dehydrated and embedded in paraffin, sectioned and stained with hematoxylin and eosin (H&E) for histopathological examination.
Statistical analysis
Data are expressed as the mean ± S.D. One-way analysis of variance (ANOVA) followed by Student Newman-Keuls test, which was provided by Primer Biostatistics program (Version 5). The differences were considered statistically significant at P-value <0.05.
Results
In the present study, we investigated the complications of fatty liver during NAFLD stages in two forms of induction (during first and second weeks) and progression (through third and fourth weeks) on brain tissue to assess the relation between NAFLD development and brain damage/dysfunctions incidence through induced insulin resistance and deficiency of insulin signalling..
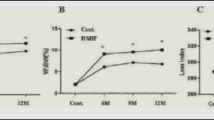
The insulin resistance markers, on the one hand, were firstly assessed during the induction and progression period and it was found that CCl4 administration increased blood glucose level, insulin level, and HOMA IR, on the other hand, HOMA- β started to decrease from the first weeks until reached the maximum reduction at fourth weeks. Moreover, Cholesterol and triglycerides levels were not altered at the first week then slightly increased at the second weeks and reached to the maximum levels at fourth weeks when compared to control levels, at p < 0.05 (Table 1).
The incidence of NAFLD proved with the histological investigation that represented in Fig. 1. After 1 week of CCl4 administration, fat droplets (steatosis) appeared intrahepatocytes, this case was accompanied with necrosis after 2 week of CCl4 administration and inflammation was detected in the third week. Finally, the severity of steatosis, necrosis, and inflammation were elevated in the fourth week of the progression stage.
Effect of the NAFLD induction and progression on liver histology. Hematoxylin-eosin staining showed the cells in a longitudinal section at magnification 400× of light microscope: (a) Control (b) first week (c) second week (d) third week (e) Fourth week. Solid arrow shows steatosis, dashed arrow shows necrosis and dotted arrow shows inflammation
Table 2 shows the alterations that took place in the levels of the brain glucose, protein and lipid profile (cholesterol, triglycerides and total lipid) due to NAFLD induction (first and second weeks) and progression (third and fourth weeks). On the one hand, during the induction and progression stages, the level of glucose was markedly decreased while protein content and lipid profile were significantly increased than those of control levels, at p < 0.05. On the other hand, brain insulin level did not affect through the induction stage but it significantly elevated through the progression period as shown in Table 2, at p < 0.05.
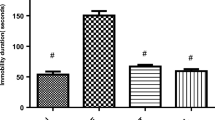
Brain prooxidants, described in terms of TBARS and the activity of xanthine oxidase, were significantly increased in a range of 2–7 and 5–14 folds though the induction and progression periods, respectively when compared to control level. On the other hand, the antioxidants parameters, GSH and GPx were markedly decreased through the disease induction and progression, as shown in Fig. 2.
TBARS, GSH, GPx and XO. Means with different letters (a, b, c, d or e) were significantly different at p < 0.05. Mean with letter (a) was significantly the lowest value while mean with the letter (e) was significantly the highest value. Letters b, c and d within a series are significantly different from a and e, as well as b letter is significantly lower than c and c lower than d letter at p < 0.05. Groups with the same letters are not significantly different at p < 0.05
The alteration in prooxidants/antioxidants status was linked with alteration in energy status where it was found that the brain ATPase gradually increased in the levels of 31% to 228% through the induction and progression period. This elevation associated with suddenly decrease in brain inorganic phosphate level from the first week. Otherwise, the level of inorganic pyrophosphate was unaffected by disease induction or progression (Fig. 3).
ATPase (nmol/min), PPi (mg/g) and Pi (mg/g*10−1). Means with different letters (a, b or c) were significantly different at p < 0.05. Mean with letter (a) was significantly the lowest value while mean with the letter (c) was significantly the highest value. Letter b is significantly lower than c at p < 0.05. If two or three groups within the same series have the same letters that means there is no significant difference detected at p < 0.05
The NAFLD induction and progression showed a progressive alteration in brain inflammatory markers as shown in Table 3. Cytochrome P450 (CYP 2E1) activity was strongly increased at all time intervals of studied stages where it was increased by 47, 46, 71 and 90% respectively from the first to the fourth weeks (Table 3).
TNF-α levels were potentially increased in brain by approximately 2 folds for the first week, 2.6 folds for the second week, 3.2 folds for the third week and 3.8 folds at the fourth week interval (Table 3). In the same manner, brain IL-6 levels were potentially heightened from the first to the fourth weeks, respectively by 1.8, 1.7, 2.5 and 3.1 folds in comparison to the control group at p < 0.05 (Table 3).
The levels of acetylcholine esterase (AChE) and monoamine oxidase (MAO) in serum, liver and brain tissues were shown in Table 4. NAFLD induction and progression increased AChE activity in brain, liver and serum. While, MAO activity was increased in brain and liver tissue and was decreased in serum along the induction and progression stages.
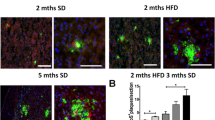
Finally the brain histopathological examination that is represented in Fig. 4 showed that normal cellular architecture in the control group (Fig. 4a). During the first week of NAFLD induction, severe neurodegenerative changes with pyknosis and vacuolations was observed (Fig. 4b) that associated with cavitations in the second week of induction period (Fig. 4c). Furthermore, during the third week (NAFLD progression, neurodegeneration with eosinophilic cells, pyknosis and vacuolations were shown in Fig. 4d. Finally, severe neurodegeneration, pyknosis acuolations and cavitations was observed during the fourth week (Fig. 4e).
Discussion
Non-alcoholic fatty liver disease (NAFLD) is being increasingly recognized as a common liver disorder that represents the hepatic manifestation of the metabolic syndrome related to obesity, insulin resistance, type II diabetes, hypertension and hyperlipidemia. NASH is the progressive form of liver injury that carries a risk for progressive fibrosis, cirrhosis, and end-stage liver disease. Indeed, hepatic lipid accumulation results from an imbalance between lipid availability (from circulating lipid uptake or de novo lipogenesis) and lipid disposal (via fatty acid oxidation or triglyceride-rich lipoprotein secretion) and eventually triggering lipoperoxidative stress and hepatic injury (Samuel et al. 2004; Shoelson et al. 2006; Samuel et al. 2007; De Luis et al. 2008; Musso et al. 2009). In our study, the increased insulin levels (hyperinsulinemia) with increased homeostatic model assessment of insulin resistance (HOMA-IR) and decreased homeostatic model assessment of beta cell function (HOMA-β) indices were matched with the significant increased levels of cholesterol and triglycerides in the progression state of NAFLD and owned to decrease in mitochondrial beta-oxidation of fatty acids and increased hepatic uptake of fatty acids. The significant increased insulin resistance favoured its role in accumulation of free fatty acids in the liver and predisposing oxidative stress through stimulating microsomal lipid peroxidases (Anania and Parekh 2007; Musso et al. 2009).
Moreover, our results revealed the role of lipid accumulation and lipid peroxidation in brain tissue accompanied with stimulating and induction of CYP 2E1 with sever oxidative stress status, which is characterized by high levels of thiobarbituric acid-reactive substances and xanthine oxidase, respectively (TBARS and XO) and low antioxidants levels reduced glutathione and glutathione peroxidise (GSH and GPx, respectively) in the progression stages of NAFLD. Moreover, the increased level of ROS effects on endogenous antioxidant system by reducing the intracellular concentration of GSH and decreases the activities of superoxide dismutase (SOD), catalase (CAT) and GPx (Halliwell and Gutteridge 2000). The mechanisms of oxidative stress in NAFLD have been focused on generation of prooxidants such as mitochondrial release of reactive oxygen species (Pessayre et al. 2002; Perez-Carreras et al. 2003), induction of microsomal cytochrome P450 (CYP) (Robertson et al. 2001), peroxisomal production of hydroperoxide (Perez-Carreras et al. 2003; Reddy 2001) or the inflammatory process itself. Cytochrome P450, in particular, CYP2E1, is characterized as a free enzyme with high pro-oxidant activity, with a potential source of oxidative stress in NASH (Macdonald et al. 2001; Robertson et al. 2001; Weltman et al. 1998; Seki et al. 2002; Emery et al. 2003; Videla et al. 2004). Furthermore, several in vitro and in vivo studies indicated that insulin resistance (IR) enhanced lipid peroxidation, reduced NADPH, CYP P450, and GSH level that mediated severe cellular damage in different tissues through metabolic activation to highly reactive substances such as free radicals (Marchesini et al. 2003). The increased hepatic activity of CYP P450 2E1 was reported in type 2 diabetes patients (Bosetti et al. 2002) and in patients with NASH (Hummel et al. 2006). Due to the remarkable increase in ketone bodies in patients with type II diabetes is considered CYP 2E1 inducers which could be an important source for ROS in hepatocytes, in the cytosol and mitochondria. So increased mitochondrial expression of CYP 2E1 could play a pivotal role in ROS generation and augment lipid peroxidation to release more reactive aldehydes that exert further mtDNA oxidation and respiratory chain polypeptides reduction (Aleynik et al. 1997).
Furthermore, the increased CYP2E1 and produced reactive oxygen species accompanied with oxidative stress cause nuclear factor kappa (NF-кβ) activation which induces the synthesis of tumor necrosis factor-α (TNF- α) (Eckel et al. 2005, Qi Cao et al. 2005). The intracellular and molecular mechanisms responsible for TNF-α-induced insulin resistance and lipid overloading of liver cells have been increasingly elucidated and appear to involve both activation of stress-related protein kinases, such as Jun N-terminal kinase (JNK), as well as the inhibitor kappa beta kinase beta (IKKβ)/NF-κB pathway. Furthermore, selective low-grade activation of the IKKβ/NF-κB pathway in liver cells results in a state of subacute chronic inflammation with increased production of cytokines, such as TNF-α and interleukin (IL)-6, and both hepatic and systemic insulin resistance (Cai et al. 2005).
The remarkable increased lipid peroxidation products and cytokines involved in the progression of NAFLD through activity of apoptosis and necrosis leading to cell death and supporting the importance of this cytokines in the interaction among inflammation, decreased insulin signaling and sensitivity with fat accumulation in liver (Angulo 2007). This overloading of liver with lipids is believed to render the liver more susceptible to a second hits which results in liver damage and disease progression (Ahboucha and Butterworth 2008). The increased cytokine IL-6 have played a significant role in the development of insulin resistance and fatty liver. Serum IL-6 levels were elevated in animal models with NAFLD, as well as alcoholic liver disease (Plummer 1978; Paglia and Valentine 1967). Moreover, IL-6 has recently been shown to be unregulated in the liver of NAFLD and positively correlated with both the inflammatory activity and the stage of fibrosis (Hjelm and De Verdier 1963; Jollow et al. 1974). Furthermore, several in vitro and in vivo studies have shown that the liver is the major target for IL-6 actions where it inhibits insulin signaling, resulting in increased hepatic gluconeogenesis, subsequent hyperglycemia, and compensatory hyperinsulinemia (Zhao and Alkon 2001).
Our brain tissue data showed that through disease induction and progression; brain glucose level was decreased while cholesterol, triglycerides, total lipid and total protein were increased. Several studies reported that high serum and brain cholesterol levels enhance amyloid β-peptide (Aβ) formation and facilitated its deposition into plaques. Therefore, NASH indicated to be a significant role for cholesterol in pathophysiology of AD (Cibickova et al. 2009). Furthermore, cholesterol influences the activity of the enzymes involved in the metabolism of the amyloid precursor protein and in the production of Aβ but the mechanism by which cholesterol affects Aβ production and metabolism is not fully understood (Rojo et al. 2006).
Furthermore, the disruptions of the neurotransmitter acetylcholine were recorded in the progression stage of NAFLD and were parallel with the observed inhibition of AChE activity (Bardov et al. 1990). Accordingly, the decreased GSH is obviously related to the reduction of AChE due to oxidative inactivation of the enzyme thiols and formation of disulfide bonds resulting in reduction in ACh (Zheng et al. 1988). So, insulin resistance, subsequent hyperinsulinemia, and hyperlipidemia are associated with increased oxidative stress, elevated inflammatory markers and increased risk for AD and other neurodegenerative disease (Watson and Craft 2006).
Lam et al. (2008) proved the direct relationship between liver disorder and nerve impulse alterations; they found that CCl4-induced fibrosis in rat increased AChE-positive nerve fibers three fold than that of control. Moreover, several investigators proved that personality changes and memory deficits are largely attributed to deficiency in cholinergic neurotransmission which returns to AChE hyperactivity (Hu et al. 2003). Thereby our animal model could be had memory deficit due to the apparently AChE hyperactivity showed in serum, liver and brain tissues especially at the third week in the stage of NAFLD progression and NASH development. Thus, to some extent, insulin acts as its own counter-regulatory hormone, with CNS insulin producing features of insulin resistance (Banks 2004). Thus, in the CNS, insulin participates in the regulation of feeding behavior and energy homeostasis, neuronal maintenance, neurogenesis, and neurotransmitter regulation. In addition, it has a role on cognitive functions as supported by neuronal activity, and in the control of aging-related processes (Craft and Watson 2004).
On the one hand, chronic hyperinsulinemia has a negative influence on memory, since type II Diabetes Mellitus has been associated with long-term impairment in cognitive function in humans and animal model studies. On the other hand, acute hyperinsulinemia increases of peripheral or brain insulin have an enhanced memory performance effect (Craft et al. 1999; Ott et al. 1999; Reger et al. 2008).
Monoamine oxidase (MAOs) play a vital role in the inactivation of neurotransmitters, MAO dysfunction (too much or too little MAO activity) is thought to be responsible for a number of neurological disorders, depression (Meyer et al. 2006), schizophrenia (Schildkraut et al. 1976), substance abuse, attention deficit disorder, migraines, and irregular sexual maturation.
Our results revealed a significant increase in MAO activity in brain tissue along induction and progression periods of NAFLD. In spite of brain enzyme activity positive increment, the activity of the enzyme was progressively decreased serum along the induction period. As we measured the total enzyme activity, we postulated that this discrepancy is due to enzyme isoforms, where there are two types of MAO, MAO-A and MAO-B. Both of MAO-A and MAO-B are found in neurons and astroglia. While outside the central nervous system; MAO-A is found in the liver, gastrointestinal tract, and placenta and MAO-B is mostly found in blood platelets (Fowler et al. 1998).
The fluctuations in the present study for the amount of MAO concentration and per se activity is mainly affected by the steatosis in the stages of NAFLD induction and increased in the progression stage of the NAFLD as the biochemical activity of monoamine oxidase generates hydroxyl radicals, very toxic members of the oxygen free radical group, that may be involved in neurodegenerative disorders such as Parkinson’s disease. Monoamine oxidase inhibitors are one of the major classes of drug prescribed for the treatment of depression, although they are last-line treatment due to risk of the drug’s interaction with diet or other drugs. Excessive levels of catecholamines (epinephrine, norepinephrine, and dopamine) may lead to a hypertensive crisis, and excessive levels of serotonin may lead to serotonin syndrome. Inhibiting monoamine oxidase with selegiline (1-deprenyl) seems to have neuroprotective actions but this may be due to inducing the release of neuronal growth factors rather than by preventing the formation of free radicals (Ghareeb et al. 2010b).
Furthermore, ATPase activity showed a surprising and interesting positive increment along the induction period. In disagreement with our results, several investigators revealed that insulin-amyloid protein directly inhibits Cl- ATPase, Na-K ATPase and Ca ATPase (Vives-Bauza et al. 2006).
In addition, Caro et al. (2009) reported that overexpression of CYP2E1 inhibited microsomal Ca2+-ATPase. However, it was (Hattori et al. 1998) reported that Mg ATPase was increased by 25% in AD patients than control subjects. We speculated that IR is the key factor in this unexpected increment, as long as it shifts the metabolic pathways toward gluconeogenesis and lipolysis both of which uses cellular storage energy (ATP) by the action of ATPase. However, an increased sensitivity of NASH livers to stressors was demonstrated in animal models of NASH, which displayed significantly increased mitochondrial ROS production and impaired ATPase activity in response to ischemia-reperfusion injury (Serviddio et al. 2008).
Finally our histopathological study (Fig. 4) supported our biochemical parameters where the brain tissue damage was associated with NAFLD/IR induction and progression took place and characterized by severe neurodegenerative changes with pyknosis and vacuolations, cavitations, accumulation of eosinophilic cells and acuolations. So, we tried to speculate the mechanism of NASH as risk factor for AD (Scheme 1) through the progression of NAFLD and its accompanied alterations in the activities of neurotransmitters catabolizing enzymes and energy depletion due to the oxidative stress and inflammation induction, all, these factors may induce brain dysfunction with increased brain damage. All, these factors may induce brain dysfunction with increased brain damage. In conclusion, we tried to establish the polygenic and interrelated pathways elucidated the link between obesity, insulin resistance, hepatic steatosis, and the progression to parenchymal necroinflammation and fibrosis through the hypothesis that, insulin may modulate cognitive functions through effects on neurotransmission and acetylcholine function and memory formation and cholinergic blockade impairs memory.
References
Ahboucha S, Butterworth R (2008) The neurosteriod system: implication in the pathophysiology of hepatic eccephalopathy. Neurochem Int 52:575–585
Aleynik S, Leo M, Aleynik M, Leiber C (1997) Polyenyphosphatidylcholine prevents carbon tetrachloride induced lipid peroxidation while it attenuates liver fibrosis. J Hepatol 27:554–556
Anania FA, Parekh S (2007) Abnormal lipid and glucose metabolism in obesity: implications for nonalcoholic fatty liver disease. Gastroenterology 132:2191–2207
Angelini N, Rafacho A, Boschero AC, Bosqueiro JR (2010) Involvement of the cholinergic pathway in glucocorticoid-induced hyperinsulinemia in rats. Diabetes Res Clin Pract 87:184–191
Angulo P (2007) GI epidemiology: nonalcoholic fatty liver disease: incidence and prevalence. Aliment Pharmacol Ther 25(8):883–889
Banks WA (2004) The source of cerebral insulin. Eur J Pharmacol 490:5–12
Bardov VG, Shmuter GM, Suchkov BP, Stepanenko GA, Khalavchuk IV, Gerashchenko SK, Kapelist VA (1990) The effect of a complex of preventive agents on the level of radioactive cesium and strontium in the bodies of laboratory animals (white rats). Gig Sanit 10:51–52
Baura GD, Foster DM, Kaiyala K, Porte D, Kahn E, Schwartz W (1996) Insulin transport from plasma into the central nervous system is inhibited by dexamethasone in dogs. Diabetes 45(1):86–90
Beal M (2005) Mitochondria take centre stage in aging and neurodegeneration. Ann Neurol 58:495–505
Biessels GJ, Kappalle LJ (2005) Uhrecht Diabetic Encephalopathy Study Group: Increased risk of Alzheimer’s disease in Type II diabetes: insulin resistance of the brain or insulin-induced amyloid pathology? Biochem Soc Trans 33:1041–1044
Bingham E, Hopkins D, Smith D, Pernet A, Hallett W, Reed L (2002) The role of insulin in human brain glucose metabolism: an fluoro-deoxyglucose positron emission tomography study. Diabetes 51(12):3384–3390
Bosetti F, Brizzi F, Barogia S, Mancuso M, Siciliano G, Tendi E, Murric L, Rapoport S, Solaini G (2002) Cytochrome c oxidase and mitochondrial F1F0-ATPase (ATP synthase) activities in platelets and brain from patients with Alzheimer’s disease. Neurobiol Aging 23:371–376
Browning JD, Horton JD (2004) Molecular mediators of hepatic steatosis and liver injury. J Clin Invest 114:147–152
Cai D, Yuan M, Frantz DF et al (2005) Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med 11:183–190
Calabrese V, Scapagnini G, Giuffrida-Stella A, Bates T, Clark J (2001) Mitochondrial involvement in brain function and dysfunction: relevance to aging, neurodegenerative disorders and longevity. Neurochem Res 26:739–764
Candeiasa F, Abreub P, Pereiraa A, Cruz-Morais J (2009) Effects of strictosamide on mouse brain and kidney Na+, K+−ATPase and Mg2+−ATPase activities. J Ethnopharmacology 121:117–122
Cao Q, Mak KM, Lieber CS (2005) Cytochrome P4502E1 primes macrophages to increase TNF-_ production in response to lipopolysaccharide. Am J Physiol Gastrointest Liver Physiol 289:G95–G107
Caro A, Evans L, Cederbaum I (2009) CYP2E1 overexpression inhibits microsomal Ca2+−ATPase activity in HepG2 cells. Toxicology 255:171–176
Chavez JA, Summers SA (2003) Characterizing the effects of saturated fatty acids on insulin signaling and ceramide and diacylglycerol accumulation in 3T3-L1 adipocytes and C2C12 myotubes. Arch Biochem Biophys 419:101–109
Choudhary P, Malik V, Puri S, Ahluwalia P (1996) Studies on the effects of monosodium glutamate on hepatic microsomal lipid peroxidation, calcium, ascorbic acid and glutathione and its dependent enzymes in adult male mice. Toxicol Lett 89:71–76
Cibickova L, Hyspler R, Micuda S, Cibicek N, Jun D, Ticha A, Brcakova E, Palicka V, Zivna H (2009) The influence of simvastatin, atorvastatin and high-cholesterol diet on acetylcholinesterase activity, amyloid beta and cholesterol synthesis in rat brain. Steroids 74:13–19
Craft S (2005) Insulin resistance syndrome and Alzheimer’s disease: age- and obesity-related effects on memory, amyloid, and inflammation. Neurobiol Aging 26:65–69
Craft S, Watson G (2004) Insulin and neurodegenerative disease: shared and specific mechanisms. Lancet Neurol 3(3):169–178
Craft S, Asthana S, Newcomer JW, Wilkinson CW, Matos IT, Baker LD et al (1999) Enhancement of memory in Alzheimer’s disease with insulin and somatostatin, but not glucose. Arch Gen Psychiatry 56:1135–1140
Day CP, James OF (1998) Steatohepatitis: a tale of two “hits”? Gastroenterology 114:842–845
De Luis DA, Aller R, Izaola O et al (2008) Effect of a hypocaloric diet in transaminases in nonalcoholic fatty liver disease and obese patients, relation with insulin resistance. Diabetes Res Clin Pract 79:74–78
Diehl AM (2002) Nonalcoholic steatosis and steatohepatitis IV. Nonalcoholic fatty liver disease abnormalities in macrophage function and cytokines. Am J Physiol Gastrointest Liver Physiol 282:G1–G5
Drake H, Goss H, Wood G (1979) New convenient method for the rapid analysis of inorganic pyrophosphate. Anal Biochem 94:117–120
Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365:1415–1428
Ellman G, Courtney K, Andres V, Featherstone R (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 7:88–95
Emery MG, Fisher JM, Chien JY et al (2003) CYP2E1 activity before and after weight loss in morbidly obese subjects with nonalcoholic fatty liver disease. Hepatology 38:428–435
Farrell GC, Larter CZ (2006) Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology 43:S99–S112
Fossati P, Prencipe L (1982) Triglyceride determination calorimetrically with an enzyme that produces hydrogen peroxide. Clin Chem 28:2077–2080
Fowler J, Volkow N, Wang G, Pappas N, Logan J, Mac Gregor R, Alexoff D, Wolf A, Warner D, Cilento R, Zezulkova I (1998) Neuropharmacological action of cigarette smoke: brain monoamine oxidase B (MAOB) inhibition. J Addict Dis 17:23–34
Ghareeb D, Hussein H (2008) Vanadium improves brain acetylcholinesterase activity on early stage alloxan-diabetic rats. Neurosci Lett 436:44–47
Ghareeb D, Hussein H, Khalil A, El-Saadani M, Ali A (2010a) Toxic effects of lead exposure on the brain of rats: Involvement of oxidative stress, inflammation, acetylcholinesterase, and the beneficial role of flaxseed extract. Toxicol Environ Chem 92(1):187–195
Ghareeb D, Khalil A, Elbassoumy A, Hussien H, Abo-Sraiaa M (2010b) Ameliorated effects of garlic (Allium sativum) on biomarkers of subchronic acrylamide hepatotoxicity and brain toxicity in rats. Toxicol Environ Chem 92(7):1357–1372
Halliwell B, Gutteridge J (2000) Free radicals in biology and medicine. In: (ed) Oxford University Press, pp 148–149
Hare M (1928) Tyramine oxidase. I. A new enzyme system in liver. Biochem J 22(4):968–979
Hattori N, Kitagawa K, Higashida K, Yagyu K, Shimoham S, Watay T, Perry G, Smith M, Inagaki C (1998) Cl-ATPase and Na/K-ATPase activities in Alzheimer’s disease brains. Neurosci Lett 254:141–144
Hjelm M, De Verdier C (1963) Determination of serum glucose by glucose oxidase method. Scand J Clin Lab Invest 15:415–428
Hsu C, Guo L (2002) Antioxidant nutrients and lead toxicity. Toxicology 180(1):33–44
Hu W, Gray NW, Brimijoin S (2003) Amyloid-beta increases acetylcholinesterase expression in neuroblastoma cells by reducing enzyme degradation. J Neurochem 86:470–478
Hummel S, Fischer A, Martin S, Schafer F, Buettner G (2006) Nitric oxide as a cellular antioxidant: a little goes a long way. Free Radic Biol Med 40:501–506
Hwang JH, Stein DT, Barzilai N, Cui MH, Tonelli J, Kishore P, Hawkins M (2007) Increased intrahepatic triglyceride is associated with peripheral insulin resistance: in vivo MR imaging and spectroscopy studies. Am J Physiol Endocrinol Metab 293:E1663–E1669
Institute of Laboratory Animal Resources (1996) Guide for the care and use of laboratory animals. Commission on life sciences, national research council. National Academy, Washington, DC
Johansen M, Bak L, Schousboe A, Iversen P, Keiding S, Sorensen M, Vilstrup H, Gjedde A, Ott P, Waagepetersen H (2007) The metabolic role of isoleucine in detoxification of ammonia in cultured mouse neurons and astrocytes. Neurochem Int 50:1042–1051
Jollow D, Mitchell J, Zampaglione N, Gillette J (1974) Bromobenze induced liver necrosis: protective role of glutathione and evidence for 3, 4-bromobenzenoxide as the hepatotoxic intermediate. Pharmacology 11:151–169
Korenblat KM, Fabbrini E, Mohammed BS, Klein S (2008) Liver, muscle, and adipose tissue insulin action is directly related to intrahepatic triglyceride content in obese subjects. Gastroenterology 134:1369–1375
Lam H, Yeh C, Cheng K, Hus C, Cheng J (2008) Effect of cholinergic denervation on hepatic fibrosis induced by carbon tetrachloride in rats. Neuroscience Lett 438:90–95
Litwack G, Bothwell JW, Williams JN, Elvehjem J (1953) A colorimetric assay for xanthine oxidase in rat liver homogenates. J Biol Chem 200:303–310
Macdonald GA, Bridle KR, Ward PJ et al (2001) Lipid peroxidation in hepatic steatosis is associated with hepatic fibrosis and occurs predominantly in acinar zone 3. J Gastroenterol Hepatol 16:599–606
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, Natale S, Vanni E, Villanova N, Melchionda N, Rizzetto M (2003) Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 37:917–923
McCullough AJ (2004) The clinical features, diagnosis and natural history of nonalcoholic fatty liver disease. Clin Liver Dis 8:VIII521–VIII533
McGarry JD (2002) Dys-regulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes 51:7–18
McGarry JD, Dobbins RL (1999) Fatty acids, lipotoxicity and insulin secretion. Diabetologia 42:128–138
Meyer JH, Ginovart N, Boovariwala A, Sagrati S, Hussey D, Garcia A, Young T, Praschak-Rieder N, Wilson AA, Houle S (2006) Elevated monoamine oxidase a levels in the brain: an explanation for the monoamine imbalance of major depression. Arch Gen Psychiatry 63(11):1209–1216
Montgomery H, Dymock J (1961) The determination of nitrite in water. Analyst 35:414–416
Musso G, Gambino R, Cassader M (2009) Recent insights into hepatic lipid metabolism in non-alcoholic fatty liver disease (NAFLD). Prog Lipid Res 48:1–26
Neuschwander-Tetri BA, Brunt EM, Wehmeier KR et al (2003) Interim results of a pilot study demonstrating the early effects of the PPAR-g ligand rosiglitazone on insulin sensitivity, aminotransferases, hepatic steatosis and body weight in patients with non-alcoholic steatohepatitis. J Hepatol 38:434–440
Ott A, Stolk RP, Hofman A, van Harskamp F, Grobbee DE, Breteler MM (1999) Association of diabetes mellitus and dementia: The Rotterdam study. Diabetologia 39:1392–1397
Paglia E, Valentine N (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med 70:158–169
Perez-Carreras M, Del Hoyo P, Martin MA et al (2003) Defective hepatic mitochondrial respiratory chain in patients with nonalcoholic steatohepatitis. Hepatology 38:999–1007
Pessayre D, Mansouri A, Fromenty B (2002) Nonalcoholic steatosis and steatohepatitis: mitochondrial dysfunction in steatohepatitis. Am J Physiol Gastrointest Liver Physiol 282:G193–G199
Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI (2005) Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 54:603–608
Plomgaard P, Bouzakri K, Krogh-Madsen R et al (2005) Tumor necrosis factor-alpha induces skeletal muscle insulin resistance in healthy human subjects via inhibition of Akt substrate 160 phosphorylation. Diabetes 54:2939–2945
Plummer D (1978) Amino acids and proteins. In: (ed) An introduction to practical biochemistry. UK, McGraw- Hill Book Co, pp 145–146
Reddy JK (2001) Nonalcoholic steatosis and steatohepatitis: peroxisomal β-oxidation, PPAR-α and steatohepatitis. Am J Physiol Gastrointest Liver Physiol 281:G1333–G1339
Reger MA, Watson GS, Green PS, Wilkinson CW, Baker LD, Cholerton B et al (2008) Intranasal insulin improves cognition and modulates β-amyloid in early AD. Neurology 70(6):440–448
Robertson GR, Leclercq I, Farrell GC (2001) Nonalcoholic steatosis and steatohepatitis: cytochrome P-450 enzymes and oxidative stress. Am J Physiol Gastrointest Liver Physiol 281:G1135–G1139
Robin M, Sauvage I, Grandperret T, Descatoire V, Pessayre D, Fromenty B (2005) Ethanol increases mitochondrial cytochrome P450 2E1 in mouse liver and rat hepatocytes. FESB Lett 579:6895–6902
Rojo L, Sjöberg MK, Hernández P, Zambrano C, Maccioni RB (2006) Roles of cholesterol and lipids in the etiopathogenesis of Alzheimer’s disease. J Biomed Biotechnol 3:73–90
Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D, Romanelli AJ, Shulman GI (2004) Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem 279:32345–32353
Samuel VT, Liu ZX, Wang A, Beddow SA, Geisler JG, Kahn M, Zhang XM, Monia BP, Bhanot S, Shulman GI (2007) Inhibition of protein kinase Cepsilon prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J Clin Invest 117:739–745
Sandler M, Reveley M, Glover V (1981) Human platelet monoamine oxidase activity in health and disease: a review. J Clin Pathol 34:292–302
Sanyal AJ, Campbell-Sargent C, Mirshahi F et al (2001) Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology 120:1183–1192
Schildkraut JJ, Herzog JM, Orsulak PJ, Edelman SE, Shein HM, Frazier SHSH (1976) Reduced platelet monoamine oxidase activity in a subgroup of schizophrenic patients. Am J Psychiatry 133(4):438–440
Seki S, Kitada T, Yamada T, Sakagushi H, Nakatani K, Wakasa K (2002) In situ detection of lipid peroxidation and oxidative DNA damage in non-alcoholic fatty liver diseases. J Hepatol 37:56–62
Serviddio G, Sastre J, Bellanti F, Vina J, Vendemiale G, Altomare E (2008) Mitochondrial involvement in non-alcoholic steatohepatitis. Mol Aspects Med 29:22–35
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Srivastava L, Das N, Sinha S (2002) Quantitative estimation of analytes in blood. In: Srivastava L, Das N, Sinha S (eds) Essential of practical biochemistry. CBS publishers and distributors, New Delhi, pp 91–94
Tokushige K, Takakura M, Tsuchiya-Matsushita N et al (2007) Influence of TNF gene polymorphisms in Japanese patients with NASH and simple steatosis. J Hepatol 46:1104–1110
Valenti L, Fracanzani AL, Dongiovanni P et al (2002) Tumor necrosis factor-alpha promoter polymorphisms and insulin resistance in nonalcoholic fatty liver disease. Gastroenterology 122:274–280
Videla LA, Rodrigo R, Orellana M et al (2004) Oxidative stress-related parameters in the liver of nonalcoholic fatty liver disease patients. Clin Sci 106:261–268
Vives-Bauza C, Gonzalo R, Manfredi G, Garcia-Arumi E, Andreu A (2006) Enhanced ROS production and antioxidant defenses in cybrids harbouring mutations in mtDNA. Neurosci Lett 391:136–141
Watson D (1960) A simple method for the determination of serum cholesterol. Clinica Chemica Acta 5:637–643
Watson GS, Craft S (2006) Insulin resistance, inflammation, and cognition in Alzheimer’s Disease:Lessons for multiple sclerosis. J Neurol Sci 245:21–33
Weber L, Boll M, Stampfl A (2003) Hepatotoxicity and mechanism of action of haloalkanes: carbon tetrachloride as a toxicological model. Crit Rev Toxicol 33:105–136
Weltman MD, Farrell GC, Hall P, Ingelman-Sundberg M, Liddle C (1998) Hepatic cytochrome P450 2E1 is increased in patients with non alcoholic steatohepatitis. Hepatology 28:128–133
Wills ED (1965) Mechanisms of lipid peroxide formation in animal tissues. Biochem J 99(3):667–676
Yu C, Wang F, Jin C, Wu X, Chan W, McKeehan W (2002) Increased carbon tetrachloride-induced liver injury and fibrosis in FGFR4-deficient mice. Am J Pathol 161:2003–2010
Zhao WQ, Alkon DL (2001) Role of insulin and insulin receptor in learning and memory. Mol Cell Endocrinol 177(1–2):125–134
Zheng S, Newton GL, Gonick G, Fahey RC, Ward JF (1988) Radioprotection of DNA by thiols: relationship between the net charge on a thiol and its ability to protect DNA. Radiat Res 114:11–27
Zollner N, Kirsch K (1962) Absorptimetric determination of total lipids in serum. Z Ges Exp Med 135:544–549
Acknowledgements
Special thanks for Prof Dr. Ashraf A. Khalil, protein technology department, the city of scientific research and Application technology, who gave us several advises through the work design.
Competing interests
There is neither financial competing interest (political, personal, religious, ideological, academic, intellectual, commercial or any other) to declare in relation to this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Doaa A. Ghareeb and Hani S. Hafez contributed equally to this work
Rights and permissions
About this article
Cite this article
Ghareeb, D.A., Hafez, H.S., Hussien, H.M. et al. Non-alcoholic fatty liver induces insulin resistance and metabolic disorders with development of brain damage and dysfunction. Metab Brain Dis 26, 253–267 (2011). https://doi.org/10.1007/s11011-011-9261-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-011-9261-y