Abstract
We investigated the therapeutic effect of zonisamide against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) neurotoxicity in mice, using Western blot analysis, immunohistochemistry and behavioral test. Our Western blot analysis and immunohistochemical study showed that the post-treatment with zonisamide prevented significantly dopaminergic cell damage, the depletion of tyrosine-hydroxylase (TH) protein levels and the proliferation of microglia in the striatum and/or substantia nigra 8 days after MPTP treatment. Furthermore, our behavioral study showed that the post-treatment with zonisamide attenuated significantly the motor deficits 7 days after MPTP treatment. These results show that zonisamide has the therapeutic effect in the MPTP model of Parkinson’s disease (PD) in mice. Our study also demonstrates the neuroprotective effect of zonisamide against dopaminergic cell damage after MPTP treatment in mice. Thus our present findings suggest that therapeutic strategies targeted to the activation of TH protein and/or the inhibition of microglial activation with zonisamide may offer a great potential for restoring the functional capacity of the surviving dopaminergic neurons in individuals affected with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Zonisamide (1,2-benzisoxazole-3-methanesulfonamide) was developed as an anti-convulsant drug and is used widely around the world, in countries such as Japan, Korea, USA and Europe. For proposed mechanisms of its anti-epileptic activity, it is thought to involve the antagonism of sodium (Rock et al. 1989; Schauf 1987) and T-type calcium channels (Suzuki et al. 1992). Furthermore, zonisamide has been shown to attenuate neonatal hypoxic-ischemic damage in experimental animals by a mechanism independent of its anti-convulsant properties (Hayakawa et al. 1994). Interestingly, a recent clinical study reports that zonisamide has clinical efficacy in the treatment of Parkinson’s disease (PD) by a randomized, double blind study (Murata et al. 2007). Furthermore, a recent experimental study suggests that zonisamide can exhibit preventing effects against dopamine quinone formation induced by excess amount of cytosolic dopamine outside the synaptic vesicles (Asanuma et al. 2008). We demonstrates recently that pre-treatment of zonisamide may attenuate MPTP-induced neurotoxicity by the elevation of TH on the dopaminergic system (Yano et al. 2009). Moreover, a recent study shows that zonisamide can increase dopaminergic turnover in the striatum of mice and common marmosets treated with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) (Yabe et al. 2009). From these observations, it is conceivable that zonisamide may be a novel drug for the treatment of PD.
MPTP is a neurotoxin that produces a parkinsonian syndrome in both humans and experimental animals (Bove et al. 2005; Dauer and Przedborski 2003). Its neurotoxic effects also appear to involve energy depletion and free radical generation. MPTP is converted to its metabolite 1-methyl-4-phenyl-pyridinium (MPP+) by monoamine oxidase B (MAO-B). MPP+ is selectively accumulated by high affinity dopamine transporters and taken up into the mitochondria of dopaminergic neurons, where it disrupts oxidative phosphorylation by inhibiting complex I of the mitochondrial electron transport chain (Gluck et al. 1994; Tipton and Singer 1993). This leads to impairment of ATP production, elevated intracellular calcium levels, and free radical generation, thereby exhibiting dopaminergic neurotoxicity (Hasegawa et al. 1990; Sriram et al. 1997). Therefore, MPTP treatments are known to cause a marked depletion of dopamine and nigrostriatal neuronal cell death in a wide variety of animal species, including mice, dogs and nonhuman primates (Zigmond and Stricker 1989). Especially, MPTP-treated mice are used worldwide as a good model of PD (Heikkila et al. 1984). However, little is known about the therapeutic (post-treatment) effect of zonisamide against MPTP neurotoxicity in mice. In the present study, therefore, we investigated the therapeutic effect of zonisamide against MPTP neurotoxicity in mice.
Materials and methods
Experimental animals
Male C57BL/6 mice (Nihon SLC Co., Shizuoka, Japan), 8-9 weeks of age, were used in the present study. The animals were housed in a controlled environment (23 ± 1°C, 50 ± 5% humidity) and were allowed food and tap water ad libitum. The room lights were on between 7:00 and 19:00. All experiments were performed in accordance with the Guidelines for Animal Experiments of the Tokushima University School of Medicine.
Experimental design
For Western blot analysis, immunohistochemical analysis and behavioral test, the animals were divided into four groups: (1) 1% Tween 80 (vehicle)-treated group; (2) Zonisamide (40 mg/kg)-treated group; (3) MPTP + vehicle-treated group; (4) MPTP + zonisamide (40 mg/kg)-treated group. The mice were injected intraperitoneally (ip.) four times with MPTP (20 mg/kg) at 2-h intervals. Zonisamide or vehicle was administered ip. once a day at 1, 2, 3, 4, 5, 6, and 7 days after MPTP treatment (Groups (3)-(4)). For groups (1) and (2), the vehicle-treated and zonisamide-treated animals were injected in the same manner with saline instead of MPTP. Zonisamide was generously provided by Dainippon-Sumitomo Pharmaceuticals (Osaka, Japan) and was suspended in 1% Tween 80.
Western blot analysis
The mice were killed by cervical dislocation 8 days after MPTP or saline treatment. The striatal tissues were homogenized in HEPES-buffered sucrose (0.32 M sucrose containing 4 g/ml pepstatin , 5 g/ml aprotinin, 20 g/ml trypsin inhibitor, 4 g/ml leupeptin, 0.2 mM phenylmethanesulfonyl fluoride, 2 mM EDTA, 2 mM EGTA, and 20 mM HEPES, pH 7.2) using a microtube homogenizer. Protein concentrations were determined using a BCA kit (PIERCE, IL, USA). The homogenates were solubilized in Laemmli’s sample buffer. Ten micrograms of protein from each sample were separated on 5–20% SDS-PAGE gel using constant current. Separated proteins were electrophoretically transferred to polyvinylidene difluoride (PVDF) membranes (ATTO, Tokyo, Japan) for 1 h with semi-dry blotting system. The PVDF membranes were incubated for 1 h at room temperature with Tris-buffered saline containing 0.1% Tween 20 (TBST) and 0.5% skim milk, followed by overnight incubation at 4°C with desired antibodies. The anti-tyrosine hydroxylase (TH) antibody (1:2,000, Chemicon International, Inc., Temecula, CA, USA) and anti-glial fibrillary acidic protein (GFAP) antibody (1:4,000, Sigma, Saint Louis, MO, USA) were diluted in TBST containing 0.5% skim milk. Membranes were washed six times for 5 min at room temperature and incubated with horseradish peroxidase-conjugated secondary antibody in TBST containing 0.5% skim milk for 1 h. Immunoreactive bands were visualized by enhanced chemiluminescent autoradiography (ECL Kit, Amersham, IL, USA), according to manufacturer’s instructions. Actin antibody (Sigma, Saint Louis, MO, USA) was used as a house keeping protein to confirm that equal amounts of protein were loaded in each line. Optical densities were determined using a computerized image analysis system (Dolphin-DOC, Kurabo, Osaka, Japan), as described previously (Yokoyama et al. 2008). Each group consisted of 3–5 mice.
Immunohistochemistry
For the immunohistochemical study, the mice were anesthetized with sodium pentobarbital (50 mg/kg, i.p.) 8 days after MPTP or saline treatment and the brains were perfusion-fixed with 4% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4) following a heparinized saline flush. The brains were removed 1 h after perfusion fixation at 4°C and were immersed in the same fixative until they were embedded in paraffin. Paraffin sections (5 µm) of the striatum and substantia nigra were used for immunohistochemistry. Each group contained of 4-5 mice.
The sections were stained immunohistochemically with anti-TH antibody (Chemicon International, Inc., Temecula, CA, USA, 1:200), anti-GFAP antibody (Chemicon International, Inc., Temecula, CA, USA, 1:200) and anti-ionized calcium-binding adaptor molecule 1 (Iba-1) (Wako Pure Chemicals, Osaka, Japan, 1:200) antibody using the ABC method (Vectastain elite ABC kit, Vector Laboratories., Burlingame, CA, USA), according to the supplier’s recommendations. In brief, after deparaffinization, the sections were incubated in phosphate buffered saline (PBS) containing 10% methanol and 0.3% H2O2 for 20 min for the blocking of endogenous peroxidase activity. The sections were pre-incubated with 10% normal serum in PBS for 30 min. They were then incubated with one of the primary antibodies in PBS containing 10% normal serum and 0.3% Triton X-100 overnight at 4°C. The sections were then incubated with biotinylated secondary antibody for 1 h, followed by avidin-biotin-peroxidase complex for 30 min at room temperature. Lastly, the sections were reacted with Vector DAB substrate kit (Vector Labs., Burlingame, CA, USA) for color development. Negative control study was performed using non-immuned IgG or by omission of the primary antibody, which showed no stable stainings.
For immunohistochemical stainings, changes of the densities of these immunostainings or changes in number of immunopositive cells in stained sections were evaluated with a light microscope at a magnification of X 200 without the examiner knowing the experimental protocols, using a computer-associated image analyzer software (WinRoof Version 5, Mitani Corporation, Fukui, Japan), as described previously (Aoki et al. 2009;Tanaka et al. 2007; Yokoyama et al. 2008).
Behavioral testing
Behavioral test was performed 2 h after final treatment with zonisamide or vehicle (7 days after MPTP or saline treatment). The Rota rod treadmill (Constant Speed Model, Ugo Basile, Varese, Italy) consists of a plastic rod, 6 cm in diameter and 36 cm long, with a non-slippery surface 20 cm above the base (trip plate). This rod is divided into five equal sections by six discs (25 cm in diameter), which enables five mice to walk on the rod at the same time. In the present study, rotor mode was used (28 rpm for 10 min). The time from when the animal was placed on the rod to when it fell off was recorded as the performance time, as described previously (Ookubo et al. 2009). Each group consisted of 9–17 mice.
Statistical analysis
For Western blot analysis and immunohistochemistry, all values were expressed as means±S.E.M. and statistical significance was evaluated by one-way analysis of variance (ANOVA) followed by Fisher’s PLSD multiple comparison test or Student’s t-test. The P values less than 0.05 was considered statistically significance.
Results
Therapeutic effects of post-treatment with zonisamide on the striatal TH protein levels by Western blot analysis 8 days after MPTP treatment
As shown in Fig. 1, zonisamide prevented a significant loss in TH protein levels in the striatum after MPTP treatment, as compared to MPTP-treated group. In addition, zonisamide only showed a significant increase in the striatal TH protein levels, as compared to vehicle-treated group.
Immunoblotting analysis of TH protein levels in the mouse striatum 8 days after MPTP treatment. a Western blot analysis. Actin protein was detected as a housekeeping protein to confirm that equal amounts of protein were loaded in each line. b TH protein levels were expressed as % of vehicle (means±S.E.M.) using ratios to actin protein levels. *p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). #P < 0.01 compared with vehicle-treated group (Student’s t-test). ZNS: zonisamide. n = 4-5
Therapeutic effects of post-treatment with zonisamide on the striatal GFAP protein levels by Western blot analysis 8 days after MPTP treatment
As shown in Fig. 2, zonisamide did not prevent a significant increase in GFAP protein levels in the striatum after MPTP treatment, as compared to MPTP-treated group. In addition, zonisamide only showed no significant change in the striatal GFAP protein levels, as compared to vehicle-treated group.
Immunoblotting analysis of GFAP protein levels in the mouse striatum 8 days after MPTP treatment. a Western blot analysis. Actin protein was detected as a housekeeping protein to confirm that equal amounts of protein were loaded in each line. b GFAP protein levels were expressed as % of vehicle (means±S.E.M.) using ratios to actin protein levels. *p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). ZNS: zonisamide. n = 3–5
Therapeutic effects of post-treatment with zonisamide on the dopaminergic neurons in the striatum and substantia nigra 8 days after MPTP treatment
Representative photographs of TH immunostaining in the striatum and substantia nigra are shown in Figs. 3 and 4. The striatal TH immunopositive fibers and nigral TH immunopositive neurons were easily detectable in vehicle-treated mice. A significant decrease in the density of TH immunopositive fibers was observed in the striatum after MPTP treatment. Zonisamide prevented a significant decrease in the density of TH immunopositive fibers in the striatum after MPTP treatment. On the other hand, a significant decrease in the number of TH immunopositive neurons was also found in the substantia nigra after MPTP treatment. Zonisamide prevented a significant decrease in the number of TH immunopositive neurons in the substantia nigra after MPTP treatment. In addition, zonisamide only showed no significant change in the density of TH immunopositive fibers in the striatum and in the number of TH immunopositive neurons in the substantia nigra, as compared to vehicle-treated group.
a Representative microphotographs of TH immunostaining in the striatum. a: Vehicle-treated group; b: ZNS-treated group; c: MPTP + vehicle-treated group; d: MPTP + ZNS-treated group. Bar = 100 μm. b TH immunostaining levels were expressed as density (means±S.E.M.). *p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). ZNS: zonisamide. n = 5
a Representative microphotographs of TH immunostaining in the substantia nigra. a: Vehicle-treated group; b: ZNS-treated group; c: MPTP + vehicle-treated group; d: MPTP + ZNS-treated group. Bar = 500 μm. b TH-immunopositive cells were expressed as cells/mm2 (means±S.E.M.). *p < 0.05, **p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). ZNS: zonisamide. n = 4-5
Therapeutic effects of post-treatment with zonisamide on GFAP immunopositive astrocytes in the striatum and substantia nigra 8 days after MPTP treatment
As shown in Figs. 5 and 6, astrocytes were slightly immunostained for GFAP in the striatum and substantia nigra of vehicle-treated mice. The number of GFAP immunoreactive astrocytes increased significantly in the striatum after MPTP treatment. Zonisamide attenuated a significant increase in the number of GFAP immunopositive astrocytes in the striatum after MPTP treatment. On the other hand, a significant increase in the number of GFAP immunopositive astrocytes was found in the substantia nigra after MPTP treatment. In contrast, zonisamide did not attenuate a significant increase in the number of GFAP immunopositive astrocytes in the substantia nigra after MPTP treatment. In addition, zonisamide only showed no significant change in the number of GFAP immunopositive astrocytes in the striatum and substantia nigra, as compared to vehicle-treated group.
a Representative microphotographs of GFAP immunostaining in the striatum. a: Vehicle-treated group; b: ZNS-treated group; c: MPTP + vehicle-treated group; d: MPTP + ZNS-treated group. Bar = 100 μm. b GFAP-immunopositive astrocytes were expressed as cells/mm2 (means±S.E.M.). *p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). ZNS: zonisamide. n = 4-5
a Representative microphotographs of GFAP immunostaining in the substantia nigra. a: Vehicle-treated group; b: ZNS-treated group; c: MPTP + vehicle-treated group; d: MPTP + ZNS-treated group. Bar = 50 μm. b GFAP immunopositive astrocytes were expressed as cells/mm2 (means±S.E.M.). *p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). ZNS: zonisamide. n = 4-5
Therapeutic effects of post-treatment with zonisamide on Iba-1 immunopositive microglia in the striatum and substantia nigra 8 days after MPTP treatment
As shown in Figs. 7 and 8, microglial cells were slightly immunostained for Iba-1 in the striatum and substantia nigra of vehicle-treated mice. The number of Iba-1 immunoreactive microglia increased significantly in the striatum after MPTP treatment. Zonisamide prevented a significant increase in the number of Iba-1 immunopositive microglia in the striatum after MPTP treatment. On the other hand, a significant increase in the number of Iba-1 immunopositive microglia was also found in the substantia nigra after MPTP treatment. Zonisamide prevented a significant increase in the number of Iba-1 immunopositive microglia in the substantia nigra after MPTP treatment. In addition, zonisamide only showed a significant decrease in the number of Iba-1 immunopositive microglia in the substantia nigra, as compared to vehicle-treated group.
a Representative microphotographs of Iba-1 immunostaining in the striatum. a: Vehicle-treated group; b: ZNS-treated group; c: MPTP + vehicle-treated group; d: MPTP + ZNS-treated group. Bar = 50 μm. b Iba 1 immunopositive microglia were expressed as cells/mm2 (means±S.E.M.). *p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). ZNS: zonisamide. n = 4-5
a Representative microphotographs of Iba-1 immunostaining in the substantia nigra. a: Vehicle-treated group; b: ZNS-treated group; c: MPTP + vehicle-treated group; d: MPTP + ZNS-treated group. Bar = 50 μm. b Iba-1-immunopositive microglia was expressed as cell/mm2 (means±S.E.M). *p < 0.05, **p < 0.01 compared with MPTP + vehicle-treated group (Fisher’s PLSD test). #p < 0.05 compared with each vehicle-treated group (Student’s t-test).ZNS: zonisamide. n = 5
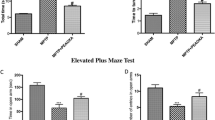
Therapeutic effects of post-treatment with zonisamide against motor deficits 7 days after MPTP treatment
Vehicle-treated mice usually remained on the Rota rod for 500–700 sec. As shown in Table 1, in Rota rod test, MPTP-treated mice exhibited a significant loss of motor activity after MPTP treatment as compared with each vehicle-treated group. In Rota rod test, zonisamide prevented a significant loss of motor activity after MPTP treatment. In Rota rod test, zonisamide only showed no significant change of motor activity, as compared to vehicle-treated group.
Discussion
It is known that anti-convulsant drug, zonisamide, has a wide clinical spectrum of use in both psychiatric and neurological disorders such as epilepsy, mood disorders and PD (Ito et al. 1982; McElroy et al. 2005; Murata et al. 2007). In patients with PD, in particular, several studies demonstrate that long-term treatment of levodopa causes various adverse side effects such as wearing-off phenomenon, dyskinesia and psychiatric symptom (Ahlskog and Munenter 2001; Ogawa et al. 2005). Furthermore, a recent double-blind controlled study in Japan reported that an adjunctive treatment with zonisamide to levodopa can improve all the cardinal symptoms of PD (Murata 2004; Murata et al. 2007). From these observations, it is suggested that zonisamide has a therapeutic effect in the treatment of PD particularly with regard to avoiding the adverse side effects of levodopa. However, little is known about the therapeutic effect of zonisamide against MPTP neurotoxicity in mice. In the present study, therefore, we investigated directly the therapeutic effect of zonisamide against MPTP neurotoxicity in mice.
Our Western blot analysis study showed that post-treatment with zonisamide can attenuate a significant decrease of TH protein levels in the striatum 8 days after MPTP treatment. Furthermore, zonisamide alone showed a significant increase of TH protein levels in the striatum, as compared to vehicle-treated group. In our immunohistochemical study, furthermore, post-treatment with zonisamide exhibited a protective effect against a significant decrease in the density of TH-immunopositive fibers in the striatum and a significant decrease in the number of TH-immunopositive neurons in the substantia nigra 8 days after MPTP treatment. A previous study reported that zonisamide increased dopaminergic synthesis by increasing TH activity and TH mRNA (Murata 2004). The findings are, at least in part, consistent with the results of our present Western blot analysis study. Interestingly, a previous study reported that dopaminergic neurons that survive the MPTP lesioning increase TH protein and may repopulate the striatum with axonal growth and branching, indicating neuroplasticity (Jakowec et al. 2004). Therefore, our present findings suggest that therapeutic strategies targeted to the activation of TH activity with zonisamide may offer a great potential for restoring the functional capacity of the surviving dopaminergic neurons in individuals affected with PD.
On the other hand, our Western blot analysis study showed a significant increase of GFAP protein levels in the striatum 8 days after MPTP treatment, as compared to vehicle-treated group. Post-treatment with zonisamide showed a tendency to attenuate a significant increase in GFAP protein levels in the striatum after MPTP treatment. Our immunohistochemical study demonstrated a significant increase in the number of GFAP immunopositive astrocytes in the striatum and substantia nigra 8 days after MPTP treatment. Although post-treatment with zonisamide attenuated a significant increase in the number of GFAP-immunopositive astrocytes in the striatum, this drug did not show a significant change in the number of GFAP-immunopositive astrocytes in the substantia nigra 8 days after MPTP treatment. GFAP immunopositive astrocytes are known to play a central role in the defense of brain and to exert a variety of neuroprotective functions (Morale et al. 2006). Thus, the astrocytes express crucial neurotrophic molecules, regulating growth, differentiation and survival of neurons (Dringen et al. 2000; Gallo et al. 2000). Furthermore, it is known that GFAP-null mice are highly susceptible to brain damage, such as cerebral ischemia (Nawashiro et al. 2000). These observations seem to suggest that GFAP immunopositive astrocytes may have a beneficial effect against MPTP neurotoxicity in mice. In the present study, the alteration of GFAP immunopositive astrocytes in the striatum was more pronounced than that of GFAP immunopositive astrocytes in the substantia nigra after MPTP treatment. The present results may suggest further evidence that the increase of the striatal GFAP immunopositive astrocytes does not always play an important role for neuroprotection against MPTP neurotoxicity in mice, although further studies are required to clarify our findings. In our preliminary study, in addition, post-treatment with zonisamide did not prevent the reductions of the striatal dopamine, DOPAC and HVA levels 8 days after MPTP treatment. Therefore, the exact mechanisms of zonisamide need to elucidate.
For the changes of microglia, post-treatment with zonisamide protected a significant increase in the number of Iba-1 immunopositive microglia in the striatum and substantia nigra 8 days after MPTP treatment. Microglial activation has been implicated as a common contributing component in numerous neurodegenerative diseases, such as PD, Alzheimer’s disease, multiple sclerosis, and amyotrophic lateral sclerosis (Beal 2003; Block and Hong 2005; McGeer et al. 1998). In MPTP experiments as the animal model of PD, in particular, massive microglial activation has been demonstrated in the striatum and substantia nigra (Czlonkowska et al. 1996; Kukowska-Jastrzebska et al. 1999; Sugama et al. 2003). Furthermore, a previous study has shown that blockade of microglial activation can protect against MPTP neurotoxicity in mice (Wu et al. 2002). Based on these observations, we speculate the possibility that zonisamide acts on microglia and its therapeutic effect may be partly mediated through the prevention of microglial activation. However, details of mechanisms of zonisamide against microglial activation need to elucidate.
In conclusion, we show that an anti-convulsant drug, zonisamide, has the therapeutic effect in the MPTP model of PD in mice. Our study also demonstrated that the neuroprotective effect of zonisamide against dopaminergic cell damage after MPTP treatment in mice. Furthermore, our present findings suggest that therapeutic strategies targeted to the activation of TH activity and/or the inhibition of microglial activation with zonisamide may offer a great potential for restoring the functional capacity of the surviving dopaminergic neurons in individuals affected with PD. These results demonstrate further evidence that zonisamide may offer a new approach for the treatment of PD.
References
Ahlskog JE, Munenter MD (2001) Frequency of levodopa-related dyskinesias and motor fluctuations as estimated from the cumulative literature. Mov Disord 16:448–458
Aoki E, Yano R, Yokoyama H, Kato H, Araki T (2009) Role of nuclear transcription factor kappa B (NF-kappaB) for MPTP (1-methyl-4-phenyl-1, 2, 3, 6-tetrahyropyridine)-induced apoptosis in nigral neurons of mice. Exp Mol Pathol 86:57–64
Asanuma M, Miyazaki I, Diaz-Corrales FJ, Miyoshi K, Ogawa N, Murata M (2008) Preventing effects of a novel anti-parkinsonian agent zonisamide on dopamine quinone formation. Neurosci Res 60:106–113
Beal MF (2003) Mitochondria, oxidative damage, and inflammation in Parkinson’s disease. Ann N Y Acad Sci 991:120–131
Block ML, Hong JS (2005) Microglia and inflammation-mediated neurodegeneration: multiple triggers with a common mechanism. Prog Neurobiol 76:77–98
Bové J, Prou D, Perier C, Przedborski S (2005) Toxin-induced models of Parkinson’s disease. NeuroRx 2:484–494
Członkowska A, Kohutnicka M, Kurkowska-Jastrzebska I, Członkowski A (1996) Microglial reaction in MPTP (1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine) induced Parkinson’s disease mice model. Neurodegeneration 5:137–143
Dauer W, Przedborski S (2003) Parkinson’s disease: mechanisms and models. Neuron 39:889–909
Dringen R, Gutterer JM, Hirrlinger J (2000) Glutathione metabolism in brain metabolic interaction between astrocytes and neurons in the defense against reactive oxygen species. Eur J Biochem 267:4912–4916
Gallo F, Morale MC, Spina-Purrello V, Tirolo C, Testa N, Farinella Z, Avola R, Beaudet A, Marchetti B (2000) Basic fibroblast growth factor (bFGF) acts on both neurons and glia to mediate the neurotrophic effects of astrocytes on LHRH neurons in culture. Synapse 36:233–253
Gluck MR, Youngster SK, Ramsay RR, Singer TP, Nicklas WJ (1994) Studies on the characterization of the inhibitory mechanism of 4'-alkylated 1-methyl-4-phenylpyridinium and phenylpyridine analogues in mitochondria and electron transport particles. J Neurochem 63:655–661
Hasegawa E, Takeshige K, Oishi T, Murai Y, Minakami S (1990) 1-Methyl-4-phenylpyridinium (MPP+) induces NADH-dependent superoxide formation and enhances NADH-dependent lipid peroxidation in bovine heart submitochondrial particles. Biochem Biophys Res Commun 170:1049–1055
Hayakawa T, Higuchi Y, Nigami H, Hattori H (1994) Zonisamide reduces hypoxic-ischemic brain damage in neonatal rats irrespective of its anticonvulsive effect. Eur J Pharmacol 257:131–136
Heikkila RE, Manzino L, Cabbat ES, Duvosion RC (1984) Protection against the dopaminergic neurotoxicity of 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydroxypyridine by monoamine oxidase inhibitors. Nature 311:467–469
Ito T, Yamaguchi T, Miyazaki H, Sekine Y, Shimizu M, Ishida S, Yagi K, Kakegawa N, Seino M, Wada T (1982) Pharmacokinetic studies of AD-810, a new antiepileptic compound. Phase I trials. Arzneimittelforschung 32:1581–1586
Jakowec MW, Nixon K, Hogg E, McNeill T, Petzinger GM (2004) Tyrosine hydroxylase and dopamine transporter expression following 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine-induced neurodegeneration of the mouse nigrostriatal pathway. J Neurosci Res 76:539–550
Kurkowska-Jastrzebska I, Wrońska A, Kohutnicka M, Członkowski A, Członkowska A (1999) The inflammatory reaction following 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine intoxication in mouse. Exp Neurol 156:50–61
McElroy SL, Suppes T, Keck PE Jr, Black D, Frye MA, Altshuler LL, Nolen WA, Kupka RW, Leverich GS, Walden J, Grunze H, Post RM (2005) Open-label adjunctive zonisamide in the treatment of bipolar disorders: a prospective trial. J Clin Psychiatry 66:617–624
McGeer PL, Itagaki S, Boyes BE, McGeer EG (1998) Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson's and Alzheimer's disease brains. Neurology 38:1285–1291
Morale MC, Serra PA, L'episcopo F, Tirolo C, Caniglia S, Testa N, Gennuso F, Giaquinta G, Rocchitta G, Desole MS, Miele E, Estrogen MB (2006) Estrogen, neuroinflammation and neuroprotection in Parkinson's disease: glia dictates resistance versus vulnerability to neurodegeneration. Neuroscience 138:869–878
Murata M (2004) Novel therapeutic effects of the anti-convulsant, zonisamide, on Parkinson’s disease. Curr Pharm Des 10:687–693
Murata M, Hasegawa K, Kanazawa I (2007) Zonisamide improves motor function in Parkinson’s disease: a randomized, double-blind study. Neurology 68:45–50
Nawashiro H, Brenner M, Fukui S, Shima K, Hallenbeck JM (2000) High susceptibility to cerebral ischemia in GFAP-null mice. J Cereb Blood Flow Metab 20:1040–1044
Ogawa N, Asanuma M, Miyazaki I, Diaz-Corrales F, Miyoshi K (2005) L-DOPA treatment from the viewpoint of neuroprotection: possible mechanism of specific and progressive dopaminergic neuronal death in Parkinson’s disease. J Neurol 252(suppl 4):iv23–iv31
Ookubo M, Yokoyama H, Kato H, Araki T (2009) Gender differences of MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) neurotoxicity in C57BL/6 mice. Mol Cell Endocrinol 311:62–68
Rock D, MacDonald R, Taylor C (1989) Blockade of sustained repetitive action potentials in cultured spinal cord neurons by zonisaimde (AD 810, CI 912), a novel anticonvulsant. Epilepsy Res 3:138–143
Schauf C (1987) Zonisamide enhances slow sodium inactivation in Myxicola. Brain Res 413:185–188
Sriram K, Pai KS, Boyd MR, Ravindranath V (1997) Evidence for generation of oxidative stress in brain by MPTP: in vitro and in vivo studies in mice. Brain Res 749:44–52
Sugama S, Yang L, Cho BP, DeGiorgio LA, Lorenzl S, Albers DS, Beal MF, Volpe BT, Joh TH (2003) Age-related microglial activation in 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine (MPTP)-induced dopaminergic neurodegeneration in C57BL/6 mice. Brain Res 964:288–294
Suzuki S, Kawakami K, Nishimura S, Watanabe Y, Yagi K, Seino M, Miyamoto K (1992) Zonisamide blocks T-type calcium channel in cultured neurons of rat cerebral cortex. Epilepsy Res 12:21–27
Tanaka A, Watanabe Y, Kato H, Araki T (2007) Immunohistochemical changes to related ageing in the mouse hippocampus and subventicular zone. Mech Ageing Dev 128:303–310
Tipton KF, Singer TP (1993) Advances in our understanding of the mechanisms of the neurotoxicity of MPTP and related compounds. J Neurochem 61:1191–1206
Wu DC, Jackson-Lewis V, Vila M, Tieu K, Teismann P, Vadseth C, Choi DK, Ischiropoulos H, Przedborski S (2002) Blockade of microglial activation is neuroprotective in the 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine mouse model of Parkinson disease. J Neurosci 22:1763–1771
Yabe H, Choudhury ME, Kubo M, Nishikawa N, Nagai M, Nomoto M (2009) Zonisamide Increases Dopamine Turnover in the Striatum of Mice and Common Marmosets Treated With MPTP. J Pharmacol Sci 110:64–68
Yano R, Yokoyama H, Kuroiwa H, Kato H, Araki T (2009) A novel anti-parkinsonian agent, zonisamide, attenuates MPTP-induced neurotoxicity in mice. J Mol Neurosci 39:211–219
Yokoyama H, Takagi S, Watanabe Y, Kato H, Araki T (2008) Role of reactive nitrogen and reactive oxygen species against MPTP neurotoxicity in mice. J Neural Transm 115:831–842
Zigmond MJ, Stricker EM (1989) Animals models of parkinsonism using selective neurotoxins: clinical and basic implications. Int Rev Neurobiol 31:1–79
Acknowledgements
This study was supported in part by Grant-in-Aid for Scientific Research (136700627 and 13671095) from the Ministry of Science and Education in Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yokoyama, H., Yano, R., Kuroiwa, H. et al. Therapeutic effect of a novel anti-parkinsonian agent zonisamide against MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine)neurotoxicity in mice. Metab Brain Dis 25, 135–143 (2010). https://doi.org/10.1007/s11011-010-9191-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-010-9191-0