Abstract
The aim of the present study was to assess the metabolic adjustments in adult rats with autonomic imbalance induced by hypercaloric diet. Male Wistar rats (4 weeks of age) were fed a chow diet (CD, n = 12) or hypercaloric diet (HD, n = 13) for 19 weeks. Body weight and dietary intake were measured every week and the basal metabolic rate was assessed. After 19 weeks of diet, six animals from each group were anesthetized with a lethal dose of barbital sodium (100 mg/Kg body weight, intraperitoneal; i.p.). Lee index was evaluated and adipose pads weighted. The remaining animals had a silastic cannula placed into the jugular vein for drug administration, blood collecting, and hemorrhage (1.2 mL/100 g bw/2 min). A polyethylene catheter (PE50) was inserted into the abdominal artery through the femoral artery for cardiovascular monitoring. The assessment of autonomic balance was done by evaluation of baroreflex sensitivity (intravenous (IV) injection of phenylephrine and sodium nitroprusside) and hemorrhage (1.2 mL/100 g bw/2 min). As expected, the HD induced obesity; increased weight gain (28%), adipose pads weight, and baroreflex dysfunction. The plasma level of free fatty acids and triacylglycerols were increased in HD rats by about 124% and 424%, respectively, as well as the basal metabolic rate measured at 19th weeks of diet (p < 0.01). We observed that baroreflex sensitivity to phenylephrine was reduced by about 50%, and the hyperglycemic response to hemorrhage hypotension was increased by 128% in HD rats. We found also a negative correlation between the alteration in baroreflex sensitivity and the increase in hyperglycemic response to hemorrhage in the obese rats (r = 0.72, p < 0.01) and a strong positive correlation between the increased Lee index and the hemorrhagic hyperglycemia (r = 0.93, p < 0.01). Our data demonstrate that obesity induced by hypercaloric diet in Wistar rats promotes an autonomic imbalance, which interferes with metabolic responses dependent on baroreflex sensitivity. In addition, we showed the existence of close correlation between the loss of baroreflex sensitivity and the degree of obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In addition to their role in ventilatory and cardiovascular control, reflexes from carotid receptors (baro- and chemoreceptors) also contribute to regulation of neuroendocrine responses to various physiological situations, such as exercise (Koyama et al. 2001), hypoxia (Zincker et al. 1994), hypoglycemia (Koyama et al. 2000) and hemorrhage hypotension (Silveira et al. 2003, 2005). It has been demonstrated that denervation of the carotid receptors reduces basal glucagon (Koyama et al. 2000) and arterial plasma glucagon concentration, as well as norepinephrine response to exercise and to mild hypoglycemia (Koyama et al. 2000, 2001). Previous studies have already shown that carotid baroreceptors are part of the major neuronal afferent pathway that activates metabolic adjustments induced by hemorrhagic hypotension (Silveira et al. 2003, 2005).
There are evidences of decreased baroreflex sensitivity in diet–induced obese rats (Bunag et al. 1996; Miller et al. 1999). Within this model, obesity also produces a change in the energy balance inducing both adipogenesis (Levin 1994) and increases in circulating leptin (Carroll et al. 2006), angiotensin II (Boustany et al. 2004), and insulin (Levin et al. 1997). Obesity also activates the sympathetic outflow, increasing oxygen consumption (Himms-Hagen et al. 1981; Himms-Hagen 1984) and free fatty acid mobilization from white adipose tissue (Park et al. 2000). Thus, we propose that the loss of baroreceptor sensitivity in obese rats may induce metabolic responses that are dependent on cardiovascular regulation.
Therefore, the present study was designed to investigate the relationship between reduction in baroreflex sensitivity and metabolic adjustments induced by hemorrhage hypotension in obese rats.
Materials and methods
Animals and diet
Weaning male Wistar rats (4 weeks of age) were housed in individual cages, under standard temperature conditions (22 ± 2°C) and light dark cycle (5:00 am–7:00 pm). Just after weaning, the animals were separated at random into two experimental groups: one group (CD group, n = 12) was fed a regular rat chow (NUVITAL, NUVILAB-CR, PR, Brazil) and the other was fed a hypercaloric diet (HD group, n = 13), made of chow (33%), sweetened condensed milk (33%), sugar (7%), and water (8.6%) for the next 19 weeks (Table 1). Body weight and calorie intake were measured once a week throughout the experimental period. The basal metabolic rate was determined at the end of the 19th week using individual open-circuit indirect calorimetry (Oxymax; Columbus Instruments, Columbus, OH).
The Lee index was used to evaluate the development of obesity. It was calculated as cubic root of body weight (gram) divided by the nasoanal length in millimeters × 10 (Lee 1929). The epididimal, retroperitoneal, inguinal white adipose tissues and interscapular brown adipose tissue were dissected and weighted.
The Ethics Committee for the Care and Use of Laboratory Animals of the Federal University of Minas Gerais approved all experimental procedures (Protocol n° 100/07).
Sample processing
After the 19th week, six animals in each group were anesthetized with lethal dose of pentabarbital sodium (100 mg/Kg body wt, i.p.). Blood samples were collected to assay plasma glucose, lactate, cholesterol, high density lipoprotein (HDL), triacylglycerols, free fatty acids, insulin, and leptin concentrations. The blood samples were transferred to microcentrifuge tubes containing trace amounts of heparin. Then, plasma was separated by centrifugation and kept frozen at −20°C until analysis.
Surgical procedures
The remaining animals (CD, n = 6; HD, n = 7) were submitted to arterial and vein catheter implantation for evaluation of the baroreflex sensitivity and the hyperglycemic response to hemorrhage. As described early (Silveira et al. 2003, 2005), under tribromoetanol anesthesia (1.0 mg/100 g body weight, i.p.) a silastic cannula was inserted into the jugular vein for drug administration, bleeding, and blood collecting, and a polyethylene catheter (PE10) was inserted into the abdominal aorta through the left femoral artery for cardiovascular monitoring. The outer ends of the cannulae were filled with heparinized saline solution and tunneled subcutaneously to exteriorize at the nape.
Following the surgical procedure, the rats received a single dose of analgesic (Flunixin 0.11 mg/100 g body weight; IM) and antibiotic (Pentabiotic R, Fort Dodge, Brazil, 0.2 mL; IM).
Autonomic balance assessment
Two different protocols were used to assess the autonomic balance. Firstly, we tested the baroreflex response to intravenous administration of phenylephrine and sodium nitroprusside (CD, n = 6; HD, n = 7). Secondly, we evaluated the integration of cardiovascular and metabolic responses during acute hemorrhage hypotension (CD, n = 6; HD, n = 6). Animals were allowed at least two days of recovery between the two experimental protocols.
Baroreflex sensitivity
Two days after the arterial and venous catheter implantation, mean arterial pressure and heart rate were recorded. This was accomplished by connecting the femoral cannula with heparinized saline to a pressure transducer, coupled to a MP100 system guide (Biopac systems, Santa Barbara, CA, model MP 100 CE series 198122765). After one hour of resting to adapt to this experimental environmental, the animals received doses of phenylephrine and sodium nitroprusside (1.0, 2.5, 5.0, 10.0 and 20.0 μg/mL) infused at random through the jugular catheter into the right atrium by bolus injections (0.1 mL).
The changes between basal and peak values of mean arterial pressure, and the change in heart rate reflex in response to phenylephrine and sodium nitroprusside injections were used to quantify baroreflex sensitivity. The changes in mean arterial pressure (Δ millimeters of mercury) and in heart rate expressed as pulse interval (60.000/ Δ bpm) were plotted to obtain regression lines.
Hemorrhage hypotension
In subsequent days following the baroreflex sensitivity procedure (with at least two days of recovery), the animals were submitted to the hemorrhage hypotension protocol (1.2 mL/100 g body wt/2 min). After the femoral catheter was connected to a pressure transducer and the mean arterial pressure was stabilized to resting levels (1 h of resting period), the animals were bled through the jugular catheter. Blood samples (0.2 mL) were collected immediately before hemorrhage and at 5, 10, 20 and 30 min after bleeding began (Silveira et al. 2003, 2005). The blood volume removed was replaced with saline solution following each sample collection.
Plasma samples were separated by centrifugation and stored in a freezer at −20°C until biochemical analyses of plasma glucose and lactate.
At the end of the experiment, the animals were anesthetized with a lethal dose of pentobarbital sodium (100 μg/Kg body weight, I.P.) and had Lee index values determined.
Biochemical analysis
Plasma cholesterol, HDL and triacylglycerols were determined by enzymatic method (KATAL-Kit, Belo Horizonte, Brazil). Plasma glucose and lactate were determined by the oxidase method using a glucose analyzer (2300 STATPLUS Yellow Springs Instruments, Yellow Springs, USA). Plasma free fatty acids were measured using a kit NEFA 30T (Randox Laboratories), insulin and leptin were determined by radioimmunoassay (Linco Research, St. Charles, MO, USA).
Statistical methods
The data were analyzed using two-way ANOVAs followed by Newman-Keuls’ Multiple range test. The differences between groups were analyzed by student’s t-tests. The regression lines of baroreflex sensitivity were calculated and the slopes of the curves were evaluated by Pearson correlation. Significance level was accepted at p < 0.05.
Results
Metabolic adjustments induced by the hypercaloric diet
As expected, the group fed the hypercaloric diet showed higher caloric intake (Fig. 1a) and greater body weight gain (Fig. 1b) than animals fed the chow diet (p < 0.01). Differences in body weight gain between groups were first observed at the 4th week of diet (p < 0.05), with this difference increasing through the end of the experiment. At the 19th week the HD group was 28% heavier than the CD group (p < 0.01, Fig. 1b). The HD group demonstrated an increased caloric intake and a greater Lee index at the 19th week than the CD group (Table 2).
As observed in Table 2, there were no statistical differences in plasma concentration of cholesterol HDL or glucose between HD and CD groups. However, the plasma levels of triacyglycerols, free fatty acids and insulin were 424%, 124% and 119%, respectively greater in the HD compared to CD group (p < 0.01). A significant increase in oxygen consumption (15%) was observed in the HD group compared to CD group (Table 2, p < 0.01).
Figure 2 shows the influence of hypercaloric diet on adipose pad weight. Comparing across groups, HD animals developed heavier white and brown adipose tissue pads than the CD group. In the HD group epididimal, retroperitoneal, and inguinal white pads, as well as interscapular brown pads weighed approximately 52%, 60%, 40% and 82%, respectively, more than in the CD group (p < 0.05).
Baroreflex sensitivity
Baroreceptor stimulation induced by the five levels of intravenous doses of phenylephrine and sodium nitroprusside produced a dose dependent response resulting in a positive correlation between changes in mean arterial pressure and heart rate expressed as pulse interval (ms) for both groups (Fig. 3a and c). Furthermore, as illustrated in Fig. 3b and d, baroreflex sensitivity induced by intravenous doses of pressor drugs showed a marked reduction on the bradycardic reflex of HD group compared to CD group during phenylephrine administrations (54%, p < 0.05) without any modification in tachycardia response during sodium nitroprusside.
Baroreflex sensitivity induced by intravenous doses of pressor and depressor drugs in CD and HD groups. a Change in mean arterial pressure (Δ MAP) and pulse interval (Δ PI) induced by phenylephrine; b The baroreflex gain of bradycardia reflex; c Change in mean arterial pressure (Δ MAP) and pulse interval (Δ PI) induced by sodium nitroprusside; d The baroreflex gain of tachycardia reflex. * p < 0.05
Effects of acute hemorrhage on blood pressure and heart rate in rats submitted to HD or CD
As observed in Fig. 4a, after 10 min of hemorrhage, the blood pressure of CD and HD rats fell acutely from resting values (62 mmHg and 57 mmHg, respectively, p < 0.05). For both group, the mean arterial pressure returned towards baseline levels within 30 min, stabilizing at approximately 27 mmHg below basal values in the CD group and 34 mmHg below basal values in the HD group. The effects of hemorrhage on mean arterial pressure did not differ significantly between groups.
Heart rate register during hemorrhage hypotension is showed in Fig. 4b. The heart rate of CD rats fell 184 beats/min from resting values after 10 min of hemorrhage (p < 0.05). The maximal value of bradycardia response in the HD group occurred 5 min latter than CD group, attaining 174 beats/min bellow basal values (p < 0.05). Following this bradycardia the heart rate of CD and HD groups started to increase towards the resting values stabilizing at about 22 beats/min and 55 beats/min below basal heart rate at 30 min, respectively. The changes in heart rate during bleeding were not significantly different between HD and CD groups.
Effects of acute hemorrhage on plasma glucose and plasma lactate levels CD and HD groups
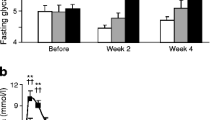
The plasma glucose levels increased immediately after hemorrhage in the CD group and the HD group, as showed in Fig. 5a. Hyperglycemia induced by hemorrhagic hypotension was observed beginning at 5 min after bleeding, reaching peak at 10 min. Plasma glucose levels increased by 37% in CD rats and 48% in HD rats, respectively. However, at 20 min post hemorrhage, plasma glucose in the CD group fell to 10.2 mM, while plasma glucose in the HD group remained high (13.1 mM). At this point, the hyperglycemia of the HD group was higher than the CD group (p < 0.05). The 128% increase in hyperglycemic response to hemorrhage hypotension shown by the HD animals over CD animals is best observed in Fig. 5b that illustrates the 30 min integrated area under the incremental glucose curve.
As illustrated in Fig. 5c, the plasma lactate levels also increased immediately after hemorrhage. This was observed during the first 10 min (p < 0.05) of the procedure, when plasma lactate increased 78% in the CD group and 76% in the HD group from resting values. After 30 min of hemorrhagic hypotension, the plasma lactate reduced 64% and 72% above baseline levels, respectively. However, this metabolic response to hemorrhage did not significantly differ between groups. The integrated area under the lactate curve after 30 min of hemorrhage further illustrates this result (Fig. 5d).
Correlation between Lee index, pulse interval (ms) and hemorrhagic hyperglycemia in HD group
As depicted in Fig. 6a, a negative correlation was observed between Lee index and pulse interval (r = 0.72; p < 0.01). Also, a strong positive correlation was observed between the increase in plasma glucose (Δ glucose) during hemorrhage hypotension and the increase in Lee index (r = 0.93; p < 0.01) in the HD group (Fig. 6b). In addition, a negative correlation was observed between the changes in plasma glucose levels after hemorrhage and pulse interval assessed with pressor doses of phenylephrine (r = 0.72; p < 0.01) in HD group.
Discussion
The results presented here clearly show that the hypercaloric diet induced a loss of baroreflex sensitivity that is closely related to degree of obesity. In addition, our data show an enhanced hyperglycemic response to hemorrhage hypotension in diet–induced obese rats that correlated positively to this loss in baroreflex sensitivity.
To the best of our knowledge, these are the first data in the literature reporting that obesity may interfere with metabolic adjustment dependent on increased peripheral sympathetic outflow due to a loss in baroreflex sensitivity. In fact, our data show an increased hyperglycemic response to hemorrhage demonstrating that hypercaloric diet produces autonomic imbalance beyond the loss of cardiovascular reflexes.
It has been shown that reflexes from carotid receptors (baro− and chemoreceptors) participate in neuroendocrine responses to various physiological situations, such as exercise (Koyama et al. 2001), hypoxia (Zincker et al. 1994), hypoglycemia (Koyama et al. 2000), and hemorrhage hypotension (Silveira et al. 2003, 2005). Previous studies have shown that hyperglycemic response to hemorrhage is modulated by baroreceptor unloading and cholinergic transmission into the paraventricular nucleus of the hypothalamus (PVN) (Silveira et al. 2003). This should be able to influence glucose output from the liver by several distinct reflex mechanisms, including adrenal catecholamine secretion, increased angiotensin II circulation and, hepatic sympathetic activation. There is anatomical and physiological evidence to support this idea (Strack et al. 1989; Machado 1995a, b; Palkovits et al. 1999; Silveira et al. 2003, 2005). Our data point to the possibility that hypercaloric diet promoting loss of sensitivity of baroreflex may alter the activity within this circuitry. It is interesting to point out that PVN neurons, in diet–induced obese dogs, are chronically activated, indicating a decrease in baroreflex sensitivity and a predominance of sympathoexcitatory input from RVLM neurons (Lohmeier et al. 2003). In fact, previous studies have already showed a reduction in baroreflex sensitivity after intravenous doses of phenylephrine in rats fed with hypercaloric diet (Bunag et al. 1990, 1996; Miller et al. 1999). These studies corroborate the hypothesis that changes in the metabolic regulation in obese rats may initially be mediated, at least in part, by desensitization of baroreflex, leading to an augmentation of sympathetic drive induced by hemorrhage hypotension.
In the present experiment, the increased white and brown adipose pads and metabolic rate associated with high triacylglycerol and free fatty acid plasma concentrations indicate a possible contribution of the peripheral rennin angiotensin system (RAS) to the autonomic imbalance in the diet of obese rats. It is important to point out that obesity is associated with an increased circulating concentration of angiotensin II (Boustany et al. 2004; Du Toit et al. 2005). Furthermore, there are studies showing that the hypercaloric diet intake produces overactivity in renal sympathetic nerve activity (Barnes et al. 2003). It raises the possibility that sympathetic outflow to the adipose tissue and liver induced by peripheral angiotensin II would contribute to metabolic disorder. Moreover, angiotensin II induces baroreflex dysfunction (Tan et al. 2007) and acts as an important hyperglycemic agent during hemorrhagic hypotension in rats (Machado et al. 1995a). In fact, angiotensin II has a direct hyperglycemic action through activation of hepatic glicogenolysis and gluconeogenesis (Coimbra et al. 1999) and exerts an indirect action by increasing peripheral sympathetic outflow (Machado et al. 1995a; Mihessen-Neto et al. 1996). These studies reinforce the possibility of the participation of peripherally circulating angiotensin II in the altered reflex response in the present study.
Our finding of increased leptin concentration in plasma simultaneous with elevated metabolic rate and plasma free fatty acid mobilization is consistent with the known action of this hormone in facilitating peripheral sympathetic outflow to the brown adipose tissue, kidney, and adrenal gland (Dunbar et al. 1997). Leptin, a protein hormone secreted by fat cells, crosses the blood–brain barrier (Schwartz et al. 1996; Hall et al. 2001) and activates neurons located in several hypothalamic areas, including the paraventricular nucleus (Van Dijk et al. 1996; Elmquist 2001). In addition to its role in the maintenance of energy balance, leptin also participates in the central regulation of cardiovascular functions (Dunbar et al. 1997; Correia et al. 2001). Central application of leptin augments sympathetic outflow resulting in an increase in systemic arterial pressure (Dunbar et al. 1997; Correia et al. 2001) that appears to be mediated by interaction with the arterial baroreflex system (Grassi 2004). It is important to point out that PVN is part of the neural circuitry involving modulation of baroreflex and activation of sympathetic outflow responsible for the hyperglycemic response to hemorrhage hypotension (Silveira et al. 2003). It has been shown that activation of PVN neurons by leptin result in increased neurogenic sympathetic vasomotor tone, tachycardia, and suppression of the baroreceptor reflex control (Shih et al. 2003). In addition, it was previously shown that baroreflex activation by phenylephrine completely suppressed the leptin–induced increase in renal nerve sympathetic activation (RNSA) (Hausberg et al. 2002). Thus, the loss of baroreflex sensitivity to phenylephrine, in obese rats observed in our experiment, may have facilitated the increase in RNSA (induced by leptin) leading to increased peripheral RAS activity. Therefore, the autonomic imbalance induced by hypercaloric diet seems to be due to multiple endocrine factors affecting metabolic and cardiovascular homeostasis that, in turn, contribute to the hyperglycemic reflex during hemorrhage hypotension.
In summary, our results demonstrated that the intake of hypercaloric diet by Wistar rats induced a loss in baroreflex sensitivity that was closely related to degree of obesity, and induced an increased hyperglycemic response to hypotension. In addition, obesity was also related to sympathetic tonus as revealed by high basal metabolic rate and free fatty acid mobilization. Therefore, our data demonstrated that diet induced obesity promotes an autonomic and metabolic imbalance that depends on peripheral sympathetic outflow due to the reduced baroreflex sensitivity.
References
Barnes MJ, Lapanowski K, Conley A, Rafols JA, Jen KL, Dunbar JC (2003) High fat feeding is associated with increased blood pressure, sympathetic nerve activity and hypothalamic mu opioid receptors. Brain Res Bull 61(5):511–519
Boustany CM, Bharadwaj K, Daugherty A, Brown DR, Randall DC, Cassis LA (2004) Activation of the systemic and adipose renin–angiotensin system in rats with diet–induced obesity and hypertension. Am J Physiol Regul Integr Comp Physiol 287(4):R943–R949
Bunag RD, Krizsan D, Itoh H (1990) Diminished cardiovascular responsiveness to vagal stimulation in obese rats. Am J Physiol Regul Integr Comp Physiol 259:R842–R848
Bunag RD, Meyer M, Vansell N, Kerecsen L (1996) Conscious obese rats have impaired reflex bradycardia and enhanced norepinephrine sensitivity. Am J Physiol Regul Integr Comp Physiol 271:R654–R660
Carroll JF, Zenebe WJ, Strange TB (2006) Cardiovascular function in a rat model of diet–induced obesity. Hypertension 48(1):65–72
Coimbra CC, Garófalo MAR, Fócolo DRC, Xavier AR, Migliorini RH (1999) Gluconeogenesis activation after intravenous angiotensin II in freely moving rats. Peptides 20:823–827
Correia ML, Morgan DA, Sivitz WI, Mark AL, Haynes WG (2001) Leptin acts in the central nervous system to produce dose–dependent changes in arterial pressure. Hypertension 37(3):936–942
Dunbar JC, Hu Y, Lu H (1997) Intracerebroventricular leptin increases lumbar and renal sympathetic nerve activity and blood pressure in normal rats. Diabetes 46:2040–2043
Du Toit EF, Nabben M, Lochner A (2005) A potential role for angiotensin II in obesity induced cardiac hypertrophy and ischaemic/reperfusion injury. Basic Res Cardiol 100(4):346–354
Elmquist JK (2001) Hypothalamic pathways underlying the endocrine, autonomic, and behavioral effects of leptin. Physiol Behav 7 4(4–5):703–708
Grassi G (2004) Leptin, sympathetic nervous system, and baroreflex function. Curr Hypertens Rep 6:236–240
Hall JE, Hildebrandt DA, Kuo J (2001) Obesity hypertension: role of leptin and sympathetic nervous system. Am J Hypertens 14(6 pt 2):103S–115S
Hausberg M, Morgan DA, Chapleau MA, Sivitz WI, Mark AL, Haynes WG (2002) Differential modulation of leptin–induced sympathoexcitation by baroflex activation. J Hypertension 20:1633–1641
Himms-Hagen J (1984) Nonshivering thermogenesis. Brain Res Bull 12:151–160
Himms-Hagen J, Triandafillou J, William GC (1981) Brown adipose tissue of cafeteria–fed rats. Am J Physiol Endocrinol Metab 241:E116–E120
Koyama Y, Coker RH, Stone EE, Lacy DB, Jabbour K, Williams PE, Wasserman DH (2000) Evidence that carotid bodies play an important role in glucoregulation in vivo. Diabetes 49:1434–1442
Koyama Y, Coker RH, Denny JC, Lacy DB, Jabbour K, Williams PE, Wasserman DH (2001) Role of carotid bodies in control of the neurendocrine response to exercise. Am J Physiol Endocrinol Metab 281:E742–E748
Lee MO (1929) Determination of the surface area of the white rat with its application to the expression of metabolic results. Am J Physiol 89:24–33
Levin BE (1994) Diet cycling age alters weight gain and insulin levels in rats. Am J Physiol Regul Integr Comp Physiol 267(2 pt 2):R527–R235
Levin BE, Dunn-Meynell AA, Balkan B, Keesey RE (1997) Selective breeding for diet induced obesity and resistance in Sprague Dawley rats. Am J Physiol Regul Integr Comp Physiol 273(2 pt 2):R725–R730
Lohmeier TE, Warren S, Cunningham JT (2003) Sustained activation of the central baroreceptor pathway in obesity hypertension. Hypertension 42(1):96–102
Machado LJ, Marubayashi U, Reis AM, Coimbra CC (1995a) Effect [1-sar, 8-thr]—angiotensin II on the hyperglycemic response to hemorrhage in adrenomedullated and guanethidine–treated rats. Regul Pep 60(1):69–77
Machado LJ, Mihessen-Neto I, Marubayashi U, Reis AM, Coimbra CC (1995b) Hyperglycemic action of angiotensin II in freely moving rats. Peptides 16(3):479–483
Mihessen-Neto I, Reis AM, Marubayashi U, Coimbra CC (1996) Effect of sympathoadrenal blockade on the hyperglycemic action of angiotensin II. Neuropeptides 30(3):303–308
Miller AW, Sims JJ, Canavan A, Hsu T, Ujhelyi MR (1999) Impaired vagal reflex activity in insulin–resistant rats. J Cardiovasc Pharmacol 33(5):698–702
Palkovits M, Baffi JS, Pacak K (1999) The role of ascending neuronal pathways in stress–induced release of noradrenaline in the hypothalamic paraventricular nucleus of rats. J Neuroendocrinol 11(7):529–539
Park SY, Lee YJ, Kim HJ, Doh KO, Lee MK, Kim JY, Lee SK (2000) Change in activity of the sympathetic nervous system in diet induced obese rats. J Korean Med Sci 15(6):635–640
Schwartz MW, See Ley RJ, Campfield LA, Burn P, Baskin DG (1996) Identification of targets of leptin action in rat hypothalamus. J Clin Invest 98(5):1101–1106
Shih CD, Au LC, Chan JYH (2003) Differential role of leptin receptors at the hypothalamic paraventricular nucleus in tonic regulation of food intake and cardiovascular functions. J Biol Sci 10:367–378
Silveira SA, Viana Lima NR, Haibara AS, Coimbra CC (2003) The hypothalamic paraventricular nucleus and carotid receptors modulate hyperglycemia induced by hemorrhage. Brain Res 993:183–191
Silveira SA, Haibara AS, Coimbra CC (2005) Hyperglycemic response to hemorrhage is modulated by baroreceptors unloading but not by peripheral chemoreceptors activation. Auton Neurosci. 123:36–43
Strack AM, Sawyer WB, Platt KB, Loewy AD (1989) CNS cell groups regulating the sympathetic outflow to adrenal gland as revealed by transneuronal cell body labeling with pseudorabies virus. Brain Res 491(2):274–296
Tan PS, Killinger S, Horiuchi J, Dampney RA (2007) Baroreceptor reflex modulation by circulating angiotensin II is mediated by AT1 receptors in the nucleus tractus solitarius. Am J Physiol Regul Integr Comp Physiol 293(6):R2267–R2278
Van Dijk G, Thiele TE, Donahey JC, Campfield LA, Smith FJ, Burn P, Bernstein IL, Woods SC, Seeley RJ (1996) Central infusions of leptin and GLP-1-(7–36) amide differentially stimulate c-FLI in the rat brain. Am J Physiol Regul Integr Comp Physiol 271(4 Pt 2):R1096–R1100
Zincker BA, Namdaran K, Wilson R, Lacy DB, Wasserman DH (1994) Acute adaptation of carbohydrate metabolism to decreased arterial PO2. Am J Physiol Endocrinol Metab 266:E921–E929
Acknowledgements
The authors thank CNPq, CAPES, FAPESP and FAPEMIG for financial support. The technical assistance of André Luis Pimenta de Faria, Janine Costa Ivo and Patrícia Andrade Guimarães Mitre are also acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Lima, D.C., Silveira, S.A., Haibara, A.S. et al. The enhanced hyperglycemic response to hemorrhage hypotension in obese rats is related to an impaired baroreflex. Metab Brain Dis 23, 361–373 (2008). https://doi.org/10.1007/s11011-008-9101-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-008-9101-x