Abstract
Heat shock protein B8 (HSPB8) impacts on tumor proliferation and migration of malignancy. However, the role of HSPB8 in lung adenocarcinoma (LUAC) remains unclear. The aim of this study, therefore, was to clarify whether HSPB8 could bring benefits to proliferation and migration of LUAC and its underlying mechanisms. The expression of HSPB8 was first evaluated by immunohistochemistry in 35 LUAC samples. Then, A549 lung adenocarcinoma cells were transfected with pcDNA-HSPB8 or si-HSPB8 to induce HSPB8 overexpression and silence. Cellular activity was evaluated with a Cell Counting Kit-8 (CCK-8) assay. Cell proliferation and migration were observed by EdU assay and scratch assay. Mitochondria-specific reactive oxygen species (mtROS) and membrane potential were measured using MitoSOX Red probe and JC-1 staining. Superoxide dismutase (SOD) activities and malondialdehyde (MDA) level were measured using commercial kits, respectively. HSPB8 protein, mitochondrial fusion protein MFN2 and mitochondrial fission protein p-Drp1/Drp1 were measured using western blot. Compared with the normal tissues, the expression of HSPB8 protein was higher in LUAC tissues and upregulation of HSPB8 protein was related to tumor size and tumor location. Furthermore, HSPB8 overexpression aggravated cell proliferation and migration of A549 cells. Mechanistically, HSPB8 suppressed mitochondrial impairment, leading to promoting the progress of A549 lung adenocarcinoma cells. These data demonstrate that HSPB8 plays an important role in progression of LUAC and may be a new target to treat LUAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the most commonly malignancy and the leading cause of death among all types of cancer worldwide [1]. Small cell lung cancer (SCLC) and non-small lung cancer (NSCLC) are two histological types of lung cancer. Furthermore, NSCLC accounts for 85% of all lung cancer cases and contains various subtypes, including large cell carcinoma, squamous cell carcinoma, and lung adenocarcinoma (LUAC) which is the most prevalent type [2, 3]. Despite advanced interventions, such as surgery, chemotherapy and radiotherapy, tumor treatment is still facing challenges for the delayed diagnosis, recurrence or metastasis [4]. Exploring the mechanism of progress of tumor cells, therefore, necessary to find effective therapies to improve the survival rate of LUAC.
Mitochondria is dynamic organelle and the balance of mitochondrial fusion and fission is benefit to maintaining mitochondrial morphology and function, contributing to biological process, including cell proliferation, migration, invasion, apoptosis, and tumor growth [5,6,7,8,9]. Increasing evidence indicated that mitochondrial dysfunction is closely related to tumorigenesis and chemotherapy resistance of multiple tumors, including lung cancer [6, 10]. Recent study found that reactive oxygen species (ROS) mainly from mitochondria disturbed mitochondrial homeostasis and induced mitochondrial damage, subsequently leading to cell growth inhibition and apoptosis [11,12,13]. Indeed, various anticancer agents effectively eliminated lung cancer cells and limited the cancer progression via promoting ROS generation [11, 14, 15]. It is therefore of great significant to further exploring the molecular mechanism of cellular processes of lung cancer cells based on ROS production and mitochondrial function.
Heat shock protein B8 (HSPB8) is a stress-related protein which was first identified as a H11 protein kinase in human melanoma cells [16]. Research suggested that HSPB8 has been participated multiple cellular functions, such as cytoskeleton stabilization, autophagy, oxidative stress, apoptosis, aging, differentiation, and proliferation [13, 17,18,19]. Furthermore, an increasing number of studies found that HSPB8 was associated with tumor proliferation, invasion and apoptosis [19,20,21,22,23,24,25]. However, the role of HSPB8 in solid tumors is divergent. For example, HSPB8 is overexpressed in breast cancer, glioblastoma, gastrointestinal carcinoma and ovarian cancer, in which it promotes proliferation and/or suppresses apoptosis [19, 21,22,23]. But for other tumors, including melanoma, prostatic cancer, hepatocellular carcinoma, Ewing’s sarcoma and hematopoietic malignancy, the expression of HSPB8 is poor and methylated [20, 24,25,26,27]. HSPB8 has been reported to inhibition of lung ischemia–reperfusion injury by inhibiting lipid peroxidation and apoptosis, however, the role of HSPB8 expression in lung cancer remains unclear [28]. Our previous study observed that HSPB8 protected vascular endothelial cell from diabetes-induced injury by inhibition of mitochondrial reactive oxygen species (mtROS) formation [18]. Hence, we will explore the role of HSPB8 and its potential molecular mechanism in LUAC.
In this study, we hypothesize that HSPB8 promotes lung cancer cells proliferation and migration. We initially collected patients’ tissue samples to determine the expression of HSPB8 in LUAC. Overexpression and silencing of HSPB8 were then generated to confirm our hypothesis in A549 lung carcinoma cells, respectively. Our results show that HSPB8 decreased mitochondrial oxidative stress and protected mitochondrial function, ultimately promoting tumor cells proliferation and migration. Our findings may provide a novel basis for the development of therapies targeting lung cancer.
Materials and methods
Patients and samples
Thirty-five patients (11 women, 24 men) diagnosed with LUAC who underwent surgical resection were recruited from Jiangxi Provincial People’s Hospital Affiliated to Nanchang University between April 2018 and April 2019. Patients’ detailed clinical information were collected retrospectively, including age, gender, tumor location, tumor size, histological differentiation grade, lymph node metastasis, and tumor node metastasis (TNM) stage. The research was approved by the Ethical Committee of Jiangxi Provincial People’s Hospital Affiliated to Nanchang University Hospital, and the informed consent was provided from the clinicians and patients.
Histological assay
Immunohistochemistry (IHC) was used to evaluate the expression of HSPB8 protein according to previous experience [29]. Briefly, tissue specimens were cut into 5 μm serial sections, deparaffinized, rehydrated, blocked and incubated with HSPB8 antibody (Abcam, ab151552, USA).The immunohistochemical results were calculated as described previously [30]. For hematoxylin and eosin staining (H&E), 5 µm sections from the paraffin blocks were also stained with hematoxylin and eosin (H&E) and examined under an optical microscope (Olympus, Japan).
Cell culture and transfections
Human lung adenocarcinoma A549 cells were from American type culture collection (ATCC) and cultured in DMEM with 10% FBS (Gibco, USA). The cells were incubated at 37 °C in a humidified atmosphere of 5% CO2 and 95% air.
Plasmid containing HSP88 gene (pcDNA-HSPB8) and negative control (pcDNA) were constructed from Genechem (Shanghai, China). Small interference RNA-targeting HSPB8 (siRNA-HSPB8) and negative control (si-control) were purchased from GenePharma (Shanghai, China). Transfection with appropriate concentrations of vectors was performed using Lipofectamine 3000 (Invitrogen, USA) according to the manufacturer’s instructions. After 24 h, transfected cells were used to assess the transfection efficiency and changes in cell morphology and function.
Cell activity assay
Cell activity was determined by a Cell Counting Kit-8 (CCK-8, Beyotime, China) as previously described [18]. Briefly, 4 × 103 cells/100μL was seeded in 96-well plates and the cells were incubated with CCK-8 for 1 h at the indicated time points. A microplate reader (Thermo, USA) was used to measure the absorbance which is directly proportional to the number of viable cells.
Cell proliferation assay
Cell proliferation was evaluated by a Cell-Light EdU Apollo 567 in Vitro Imaging Kit (Ribobio, China) as previously described [31]. Briefly, 5 × 103 cells/wells were seeded in 96-well plates and exposed to treatments accordingly, the cells were then incubated with 50 μM 5-ethynyl-29-deoxyuridine (EdU) for 2 h at 37 °C and images were observed by fluorescence microscopy (Olympus, Japan).
Scratch assay
A549 cells (3 × 105 cells) were seeded in six-well plates. After transfection for 24 h, a straight scratch wound was made by a sterilized 10 μl pipette tip and then the wound debris was washed away using PBS. Then the cells were cultured in serum-free medium for 48 h. Images of migration area were captured by an optical microscope (Olympus, Japan) and analyzed by Image J after 0 h, 24 h, and 48 h.
MtROS and membrane potential measurement
MitoSOX Red probe (Thermo, USA) was used to detect mtROS production according to the manufacturer's specifications. The cells were incubated with Hank’s balanced salt solution containing 5 μmol/l MitoSOX at 37 °C for 15 min and then observed by fluorescence microscopy (Olympus, Japan). The mitochondrial membrane potential was measured using JC-1 immunochemistry staining as previously described. Briefly, the cells were incubated with JC-1 at 10 μg/ml for 15 min at 37 °C and then observed by fluorescence microscopy. All images were analyzed with ImageJ.
Measurement of SOD and MDA levels
Superoxide dismutase (SOD) activities and content of malondialdehyde (MDA) were measured using Total Superoxide Dismutase Assay Kit and Lipid Peroxidation MDA Assay Kit (both of them from Beyotime, China), respectively, according to the manufacturer's protocols. The assay results were normalized to the protein concentration in each group, and expressed as nmol/mg protein or units/mg protein.
Western blot
The proteins were extracted using RIPA lysis buffer (Applygen, China) supplemented with a protease inhibitor (Sigma, USA). The total protein concentrations were measured using a BCA protein assay kit (Beyotime, China). Equal amounts of total protein (30 μg) were separated by SDS-PAGE electrophoresis and electro transferred to a PVDF membrane. The membranes were blocked in 5% non-fat milk and then incubated overnight at 4 °C with different antibodies, including HSPB8, MNF2, p-Drp1, Drp1, GAPDH (Abcam, USA). For quantification, the electrochemiluminescence (ECL) signals were digitized using Quantity One software.
Statistical analysis
Data were presented as the means ± S.E.M. Data were assessed using student’s t-test and chi square tests as appropriate. *P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 19.0 software.
Results
HSPB8 protein is significantly upregulated in LUAC
Morphological change was first examined in 35 LUAC issue samples and matched normal tissues using H&E staining (P < 0.05, Fig. 1a). Then, the levels of HSPB8 protein in these tissues were assessed by IHC. The results showed that HSPB8 protein was mainly located in the cytoplasm and upregulated in LUAC tissues (P < 0.05, Fig. 1b-c). The detailed information was also shown in Table 1. Among these cases, twenty-three showed HSPB8 overexpression (65.7%, P < 0.01). The relationship between HSPB8 protein expression and clinicopathological features in 35 LUAC patients was compared and the results demonstrated that there were differences between HSPB8 expression and tumor size and location (Table 2). However, no significant difference was found between HSPB8 expression and age, gender, histological differentiation, T stage, N stage, or TNM stage.
Changes of lung adenocarcinoma tissues and the expression of HSPB8 protein. a Hematoxylin and eosin staining (H&E) staining of lung adenocarcinoma (LUAC) tissues (original magnification × 10 and × 40). b Immunohistochemical staining for HSPB8 in LUAC (original magnification × 10 and × 40). c Quantification of positive staining for HSPB8 in LUAC and normal tissue. *P < 0.05 vs. Non-ca
HSPB8 overexpression increases proliferation and migration in A549 cells
As HSPB8 overexpression was related to tumor size, we suppose that HSPB8 may stimulate LUAC proliferation and migration. HSPB8 protein expression and A549 cells activity were first investigated. The results confirmed that HSPB8 overexpression increased cell viability in A549 cells (P < 0.05, Fig. 2a–c). EdU was then used to assess cell proliferation and the result showed that HSPB8 significantly enhanced A549 cells proliferation ability (P < 0.05, Fig. 2d–e). Moreover, migration of A549 cells were monitored using scratch assay. As expected, the migration capacity of A549 cells were raised after HSPB8 overexpression (P < 0.05, Fig. 2f–g). The above evidence demonstrated that HSPB8 may promote A549 cells proliferation and migration.
HSPB8 overexpression promotes cell proliferation and migration in A549 cells. a Human A549 lung carcinoma cells were transfected with pcDNA or pcDNA-HSPB8. After 24 h, the expression of HSPB8 was detected using western blot. b Quantification of HSBP8 protein expression in A549 cells. c Cell viability in A549 cells was detected using CCK-8 assay. d Cell proliferation was assessed by EdU assay in A549 cells. e Quantification of cell proliferation in different groups. f Cell migration was monitored using scratch assay in A549 cells. g Quantification of cell migration in different groups. *P < 0.05 vs pcDNA
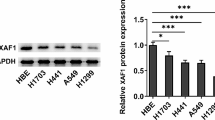
HSPB8 deficiency decreases proliferation and migration in A549 cells
We further elucidated the role of HSPB8 in A549 cells proliferation and migration using an HSPB8-silenced A549 cells line. In contrast, a decreased cell proliferation and migration were observed after the silencing of HSPB8. CCK-8 and EdU assays showed that silencing of HSPB8 suppressed A549 cells viability and proliferation ability (P < 0.05, Fig. 3a–e). Similar trends were observed in scratch assay that silencing of HSPB8 declined the ability of wound healing in A549 cells (P < 0.05, Fig. 3f–g).
Silencing of HSPB8 inhibits cell proliferation and migration in A549 cells. a Human A549 lung carcinoma cells were transfected with si-control or si-HSPB8. After 24 h, the expression of HSPB8 was detected using western blot. b Quantification of HSBP8 protein expression in A549 cells. c Cell viability in A549 cells was detected using CCK-8 assay. d Cell proliferation was assessed by EdU assay in A549 cells. e Quantification of cell proliferation in different groups. f Cell migration was monitored using scratch assay in A549 cells. g Quantification of cell migration in different groups. *P < 0.05 vs si-control
HSPB8 overexpression inhibits mitochondrial oxidative stress and mitochondrial impairment in A549 cells
Previous research suggested that the increasing of ROS and mitochondrial dysfunction promoted apoptosis of A549 cells and inhibits drug resistance [32,33,34]. Our former study confirmed that HSPB8 reduced hyperglycemia-induced endothelial injury by inhibiting mitochondrial oxidative stress and mitochondrial damage [18]. Therefore, we hypothesized that the effects of HSPB8 in A549 cells depend on the reduction of mitochondrial oxidative stress and maintaining mitochondrial function. To determine whether HSPB8 inhibits mtROS production in A549 cells, we detected mtROS production using MitoSOX Red probe and the data presented that HSPB8 overexpression reduced the level of mtROS in A549 cells (P < 0.05, Fig. 4a and b). The activity of SOD and level of MDA were used to further determine the level of mitochondrial oxidative stress in A549 cells. The results displayed that HSPB8 overexpression enhanced the activity of SOD and inhibited MDA formation in A549 cells (P < 0.05, Fig. 4c and d). To gain insight into the change in mitochondrial fusion and fission, we assessed the expression of mitochondrial fusion–related protein MFN2 and mitochondrial fission–related proteins p-Drp1/Drp in A549 cells. Western blotting results displayed that HSPB8 overexpression increased MFN2 expression and decreased p-Drp1/Drp1 expression (P < 0.05, Fig. 4e–g). Subsequently, mitochondrial function in A549 cells was evaluated by JC-1 staining assays. As expected, compared with pcDNA group, HSPB8 overexpression increased the mitochondrial function in A549 cells (P < 0.05, Fig. 4h–i). Overall, these results suggest that HSPB8 overexpression suppresses mitochondrial oxidative stress and maintains mitochondrial function in A549 cells.
HSPB8 overexpression inhibits mitochondrial oxidative stress and mitochondrial impairment in A549 cells. a MtROS was detected by MitoSOX Red probe in A549 cells. b Quantification of mtROS levels in different groups. c The activity of SOD was estimated in A549 cells. d The level of MDA was valued in A549 cells. e–g Mitochondrial fusion–related protein MFN2 and mitochondrial fission–related proteins p-Drp1/Drp1 were detected using western blot in A549 cells. h Mitochondrial membrane potential was examined by JC-1 staining assays in A549 cells. i Quantification of mitochondrial membrane potential in different groups. *P < 0.05 vs pcDNA
HSPB8 deficiency rises mitochondrial oxidative stress and mitochondrial damage in A549 cells
We also verified the effects of HSPB8-silence on mitochondrial oxidative stress and mitochondrial function in A549 cells. As expected, silencing of HSPB8 amplified the levels of mtROS and MDA, simultaneously diminished the activity of SOD (P < 0.05, Fig. 5a–d). Similarly, compared with si-control group, HSPB8 deficiency reduced the expression of MFN2 and increased p-Drp1/Drp1 expression (P < 0.05, Fig. 5e–g). Moreover, silencing of HSPB8 increased mitochondrial injury for mitochondrial membrane potential decreased (P < 0.05, Fig. 5h–i).
Silencing of HSPB8 aggravated mitochondrial oxidative stress and mitochondrial impairment in A549 cells. a MtROS was detected by MitoSOX Red probe in A549 cells. b Quantification of mtROS levels in different groups. c The activity of SOD was estimated in A549 cells. d The level of MDA was valued in A549 cells. e–g Mitochondrial fusion–related protein MFN2 and mitochondrial fission–related proteins p-Drp1/Drp1 were detected using western blot in A549 cells. h Mitochondrial membrane potential was examined by JC-1 staining assays in A549 cells. i Quantification of mitochondrial membrane potential in different groups. *P < 0.05 vs si-control
Discussion
Tumor proliferation and migration are important to the progression of LUAC. Increasing evidence emphasized that there is a close relationship between proliferation and migration and abnormal expression of tumor-related genes and mutation [21, 35, 36]. Recent studies reported that HSPB8 plays important roles in multiple tumors [17,18,19,20,21,22,−23]. In our study, we found that HSPB8 overexpression is occurred in LUAC tissues and HSPB8 inhibits mitochondrial oxidative stress and protects mitochondrial function, result in promoting A549 cells proliferation and migration. Here, for the first time, we reported that HSPB8 upregulation was associated with LUAC proliferation and migration.
HSPB8 was a member of the small heat shock proteins (sHSPs) and participated in various cell biological processes including cell proliferation and migration [19, 22]. In recent years, more and more studies about the roles of HSPB8 in tumors emerged. However, there was inconsistent with the expression and function of HSPB8 in different tumors. Some studies demonstrated that HSPB8 is highly expressed in tumors and increases cell proliferation and migration via regulating cell cycle progression and anti-apoptosis [19, 21,22,23]. Conversely and intriguingly, other studies showed that HSPB8 is downregulated in tumors and upregulation of HSPB8 contributed to increase in tumor cell resting in the G0/G1 phase and apoptosis, eventually increasing the chemosensitivity and cancer cells death [20, 24, 25]. In our study, we focused on the expression of HSPB8 in LUAC and the result suggested that HSPB8 was higher in tumor tissue than the normal lung tissues. Next, A549 cells overexpressing and silencing HSPB8 protein were constructed to confirm the role of HSPB8, respectively. Our results revealed that HSPB8 overexpression enhanced cancer cell proliferation and migration and the opposite effect was obtained after silencing it. Collectively, previous studies and our research suggested that HSPB8 may have dual role in tumor progression depending on cell types, cell differentiation and the expression of HSPB8. Further investigations are needed to explore the mechanism of action of HSP22 in cancer cells.
Oxidative stress and mitochondrial function play important roles in lung cancer [11]. HSPB8 is a stress-related protein and upregulated in response to stress conditions [37]. Accumulation of evidence showed that HSPB8 resists to oxidative stress and exerts protective effects in various cells [13, 18, 28]. Therefore, we explored the role of HSPB8 in oxidative stress and mitochondrial function of A549 cells. Our data demonstrated that HSPB8 inhibited oxidative stress, specifically suppressing mtROS formation, leading to reducing mitochondrial damage. Our results are consistent with former studies that HSPB8 protects cells from injury by inhibition of oxidative stress and protecting the function of mitochondria. Accumulating evidence indicated that cancer cell proliferation and migration are closed related to oxidative stress and mitochondrial function [38,39,40]. Collectively, these results indicate that HSPB8 may promote LUAC progress by restraining mitochondrial oxidative stress and protecting mitochondrial function.
Mitochondrial fusion and fission also participate in cell proliferation, migration and cell growth in A549 lung adenocarcinoma cells [7,8,9, 41]. In our study, we found that HSPB8 upregulated the expression of MFN2 protein and restrained p-Drp1/Drp1 expression, which contributed to improve the mitochondrial function. Our results are consistent with the former research that the increasing of mitochondrial fusion could protect A549 cells [8, 9, 42]. However, surprisingly, other studies got the opposite conclusion that increased fission and decreased fusion of mitochondria amplified lung cancer cell proliferation [5]. Previous studies suggested that tumor cells have heterogeneity and cancer stem cells (CSCs) which mainly contribute to tumor progression and drug resistance is characterized by genetic heterogeneity compared with non-CSCs [43,44,45]. Furthermore, lung cancer is also highly heterogeneous and has hundreds of mutant genes present in subclonal fractions with the increasing of tumor-grade [45]. These may explain the different effects of the dynamics balance of mitochondrial fusion and fission in tumor progression. Taken together, there is relationship between HSPB8-mediated mitochondrial fusion and A549 lung adenocarcinoma cells proliferation and migration. However, more studies are needed to clarify the action of HSPB8-mediated mitochondrial fusion and fission in lung cancer.
In summary, we found that HSPB8 plays an important role in cell proliferation and migration of LUAC. Inhibiting mitochondrial oxidative stress and increasing mitochondrial fusion, as well as maintaining mitochondrial function may the potential pathways that were responsible for the effect of HSPB8 in lung cancer cells progression (Fig. 6). Our findings may highlight a new entry point for lung cancer treatment via targeting regulation HSPB8 expression.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Ge C, Li R, Song H, Geng T, Yang J, Tan Q, Song L, Wang Y, Xue Y, Li Z, Dong S, Zhang Z, Zhang N, Guo J, Hua L, Chen S, Song X (2017) Phase I clinical trial of a novel autologous modified-DC vaccine in patients with resected NSCLC. Bmc Cancer 17:884
Peng Z, Wang J, Shan B, Yuan F, Li B, Dong Y, Peng W, Shi W, Cheng Y, Gao Y, Zhang C, Duan C (2017) Genome-wide analyses of long noncoding RNA expression profiles in lung adenocarcinoma. Sci Rep 7:15331
Hong QY, Wu GM, Qian GS, Hu CP, Zhou JY, Chen LA, Li WM, Li SY, Wang K, Wang Q, Zhang XJ, Li J, Gong X, Bai CX (2015) Prevention and management of lung cancer in China. Cancer-Am Cancer Soc 121(Suppl 17):3080–3088
Wu S, Zhou F, Zhang Z, Xing D (2011) Mitochondrial oxidative stress causes mitochondrial fragmentation via differential modulation of mitochondrial fission-fusion proteins. Febs J 278:941–954
Weinberg SE, Chandel NS (2015) Targeting mitochondria metabolism for cancer therapy. Nat Chem Biol 11:9–15
Chen SS, Tu XY, Xie LX, Xiong LP, Song J, Ye XQ (2018) Peptide nucleic acids targeting mitochondria enhances sensitivity of lung cancer cells to chemotherapy. Am J Transl Res 10:2940–2948
Lou Y, Li R, Liu J, Zhang Y, Zhang X, Jin B, Liu Y, Wang Z, Zhong H, Wen S, Han B (2015) Mitofusin-2 over-expresses and leads to dysregulation of cell cycle and cell invasion in lung adenocarcinoma. Med Oncol 32:132
Xie Y, Lv Y, Zhang Y, Liang Z, Han L, Xie Y (2019) LATS2 promotes apoptosis in non-small cell lung cancer A549 cells via triggering Mff-dependent mitochondrial fission and activating the JNK signaling pathway. Biomed Pharmacother 109:679–689
Kudryavtseva AV, Krasnov GS, Dmitriev AA, Alekseev BY, Kardymon OL, Sadritdinova AF, Fedorova MS, Pokrovsky AV, Melnikova NV, Kaprin AD, Moskalev AA, Snezhkina AV (2016) Mitochondrial dysfunction and oxidative stress in aging and cancer. Oncotarget 7:44879–44905
Wu HY, Yang FL, Li LH, Rao YK, Ju TC, Wong WT, Hsieh CY, Pivkin MV, Hua KF, Wu SH (2018) Ergosterol peroxide from marine fungus Phoma sp. induces ROS-dependent apoptosis and autophagy in human lung adenocarcinoma cells. Sci Rep 8:17956
Hseu YC, Huang YC, Thiyagarajan V, Mathew DC, Lin KY, Chen SC, Liu JY, Hsu LS, Li ML, Yang HL (2019) Anticancer activities of chalcone flavokawain B from Alpinia pricei Hayata in human lung adenocarcinoma (A549) cells via induction of reactive oxygen species-mediated apoptotic and autophagic cell death. J Cell Physiol 234:17514–17526
Jo HS, Kim DW, Shin MJ, Cho SB, Park JH, Lee CH, Yeo EJ, Choi YJ, Yeo HJ, Sohn EJ, Son O, Cho SW, Kim DS, Yu YH, Lee KW, Park J, Eum WS, Choi SY (2017) Tat-HSP22 inhibits oxidative stress-induced hippocampal neuronal cell death by regulation of the mitochondrial pathway. Mol Brain 10:1
Hu Z, Zeng Q, Zhang B, Liu H, Wang W (2014) Promotion of p53 expression and reactive oxidative stress production is involved in zerumbone-induced cisplatin sensitization of non-small cell lung cancer cells. Biochimie 107 Pt B:257–262
Park SH, Kim JH, Chi GY, Kim GY, Chang YC, Moon SK, Nam SW, Kim WJ, Yoo YH, Choi YH (2012) Induction of apoptosis and autophagy by sodium selenite in A549 human lung carcinoma cells through generation of reactive oxygen species. Toxicol Lett 212:252–261
Smith CC, Yu YX, Kulka M, Aurelian L (2000) A novel human gene similar to the protein kinase (PK) coding domain of the large subunit of herpes simplex virus type 2 ribonucleotide reductase (ICP10) codes for a serine-threonine PK and is expressed in melanoma cells. J Biol Chem 275:25690–25699
Bouhy D, Juneja M, Katona I, Holmgren A, Asselbergh B, De Winter V, Hochepied T, Goossens S, Haigh JJ, Libert C, Ceuterick-de GC, Irobi J, Weis J, Timmerman V (2018) A knock-in/knock-out mouse model of HSPB8-associated distal hereditary motor neuropathy and myopathy reveals toxic gain-of-function of mutant Hspb8. Acta Neuropathol 135:131–148
Yu L, Liang Q, Zhang W, Liao M, Wen M, Zhan B, Bao H, Cheng X (2019) HSP22 suppresses diabetes-induced endothelial injury by inhibiting mitochondrial reactive oxygen species formation. Redox Biol 21:101095
Piccolella M, Crippa V, Cristofani R, Rusmini P, Galbiati M, Cicardi ME, Meroni M, Ferri N, Morelli FF, Carra S, Messi E, Poletti A (2017) The small heat shock protein B8 (HSPB8) modulates proliferation and migration of breast cancer cells. Oncotarget 8:10400–10415
Yao J, Chen Y, Nguyen DT, Thompson ZJ, Eroshkin AM, Nerlakanti N, Patel AK, Agarwal N, Teer JK, Dhillon J, Coppola D, Zhang J, Perera R, Kim Y, Mahajan K (2019) The Homeobox gene, HOXB13, regulates a mitotic protein-kinase interaction network in metastatic prostate cancers. Sci Rep 9:9715
Shen J, Li M, Min L (2018) HSPB8 promotes cancer cell growth by activating the ERKCREB pathway and is indicative of a poor prognosis in gastric cancer patients. Oncol Rep 39:2978–2986
Suzuki M, Matsushima-Nishiwaki R, Kuroyanagi G, Suzuki N, Takamatsu R, Furui T, Yoshimi N, Kozawa O, Morishige K (2015) Regulation by heat shock protein 22 (HSPB8) of transforming growth factor-alpha-induced ovary cancer cell migration. Arch Biochem Biophys 571:40–49
Li XS, Xu Q, Fu XY, Luo WS (2014) Heat shock protein 22 overexpression is associated with the progression and prognosis in gastric cancer. J Cancer Res Clin Oncol 140:1305–1313
Matsushima-Nishiwaki R, Toyoda H, Takamatsu R, Yasuda E, Okuda S, Maeda A, Kaneoka Y, Yoshimi N, Kumada T, Kozawa O (2017) Heat shock protein 22 (HSPB8) reduces the migration of hepatocellular carcinoma cells through the suppression of the phosphoinositide 3-kinase (PI3K)/AKT pathway. Biochim Biophys Acta Mol Basis Dis 1863:1629–1639
Cui XY, Wang N, Yang BX, Gao WF, Lin YM, Yao XR, Ma XT (2012) HSPB8 is methylated in hematopoietic malignancies and overexpression of HSPB8 exhibits antileukemia effect. Exp Hematol 40:14–21
Smith CC, Li B, Liu J, Lee KS, Aurelian L (2011) The Levels of H11/HspB8 DNA methylation in human melanoma tissues and xenografts are a critical molecular marker for 5-Aza-2'-deoxycytidine therapy. Cancer Invest 29:383–395
Gober MD, Smith CC, Ueda K, Toretsky JA, Aurelian L (2003) Forced expression of the H11 heat shock protein can be regulated by DNA methylation and trigger apoptosis in human cells. J Biol Chem 278:37600–37609
Yang S, Tian J, Zhang F, Liu A, Xie B, Chen Q (2019) The protective effects of heat shock protein 22 in lung ischemia-reperfusion injury mice. Biochem Biophys Res Commun 512:698–704
Dadhania V, Zhang M, Zhang L, Bondaruk J, Majewski T, Siefker-Radtke A, Guo CC, Dinney C, Cogdell DE, Zhang S, Lee S, Lee JG, Weinstein JN, Baggerly K, McConkey D, Czerniak B (2016) Meta-analysis of the luminal and basal subtypes of bladder cancer and the identification of signature immunohistochemical markers for clinical use. Ebiomedicine 12:105–117
Hu DD, Li PC, He YF, Jia W, Hu B (2018) Overexpression of coiled-coil domain-containing protein 34 (CCDC34) and its correlation with angiogenesis in esophageal squamous cell carcinoma. Med Sci Monit 24:698–705
Lu W, Zhang H, Niu Y, Wu Y, Sun W, Li H, Kong J, Ding K, Shen HM, Wu H, Xia D, Wu Y (2017) Long non-coding RNA linc00673 regulated non-small cell lung cancer proliferation, migration, invasion and epithelial mesenchymal transition by sponging miR-150-5p. Mol Cancer 16:118
Datta S, Choudhury D, Das A, Mukherjee DD, Dasgupta M, Bandopadhyay S, Chakrabarti G (2019) Correction to: autophagy inhibition with chloroquine reverts paclitaxel resistance and attenuates metastatic potential in human nonsmall lung adenocarcinoma A549 cells via ROS mediated modulation of beta-catenin pathway. Apoptosis 24:434
Strohecker AM, Guo JY, Karsli-Uzunbas G, Price SM, Chen GJ, Mathew R, McMahon M, White E (2013) Autophagy sustains mitochondrial glutamine metabolism and growth of BrafV600E-driven lung tumors. Cancer Discov 3:1272–1285
Maryam A, Mehmood T, Yan Q, Li Y, Khan M, Ma T (2018) Proscillaridin a promotes oxidative stress and ER stress, inhibits STAT3 activation, and induces apoptosis in a549 lung adenocarcinoma cells. Oxid Med Cell Longev 2018:3853409
Tripathi SK, Pandey K, Panda M, Spinella MJ, Rengasamy KR, Biswal BK (2019) The potential of retinoids for combination therapy of lung cancer: updates and future directions. Pharmacol Res 147:104331
Knutson TP, Lange CA (2014) Tracking progesterone receptor-mediated actions in breast cancer. Pharmacol Ther 142:114–125
Li F, Xiao H, Hu Z, Zhou F, Yang B (2018) Exploring the multifaceted roles of heat shock protein B8 (HSPB8) in diseases. Eur J Cell Biol 97:216–229
Wong CC, Qian Y, Li X, Xu J, Kang W, Tong JH, To KF, Jin Y, Li W, Chen H, Go MY, Wu JL, Cheng KW, Ng SS, Sung JJ, Cai Z, Yu J (2016) SLC25A22 promotes proliferation and survival of colorectal cancer cells With KRAS mutations and xenograft tumor progression in mice via intracellular synthesis of aspartate. Gastroenterology 151:945–960
Zhang X, Gibhardt CS, Will T, Stanisz H, Korbel C, Mitkovski M, Stejerean I, Cappello S, Pacheu-Grau D, Dudek J, Tahbaz N, Mina L, Simmen T, Laschke MW, Menger MD, Schon MP, Helms V, Niemeyer BA, Rehling P, Vultur A, Bogeski I (2019) Redox signals at the ER-mitochondria interface control melanoma progression. Embo J 38:e100871
Mori K, Uchida T, Yoshie T, Mizote Y, Ishikawa F, Katsuyama M, Shibanuma M (2019) A mitochondrial ROS pathway controls matrix metalloproteinase 9 levels and invasive properties in RAS-activated cancer cells. Febs J 286:459–478
Ma JT, Zhang XY, Cao R, Sun L, Jing W, Zhao JZ, Zhang SL, Huang LT, Han CB (2019) Effects of dynamin-related protein 1 regulated mitochondrial dynamic changes on invasion and metastasis of lung cancer cells. J Cancer 10:4045–4053
Thomas KJ, Jacobson MR (2012) Defects in mitochondrial fission protein dynamin-related protein 1 are linked to apoptotic resistance and autophagy in a lung cancer model. PLoS ONE 7:e45319
Eun K, Ham SW, Kim H (2017) Cancer stem cell heterogeneity: origin and new perspectives on CSC targeting. Bmb Rep 50:117–125
Garcia-Mayea Y, Mir C, Masson F, Paciucci R, LLeonart ME (2019) Insights into new mechanisms and models of cancer stem cell multidrug resistance. Semin Cancer Biol. https://doi.org/10.1016/j.semcancer.2019.07.022
Sosa IV, Giuranno L, Dubois LJ, Theys J, Vooijs M (2018) Drug resistance in non-small cell lung cancer: a potential for NOTCH targeting? Front Oncol 8:267
Acknowledgements
This work was supported by the Natural Science Foundation of Jiangxi Province (20202BABL216035, 20202BAB206042), the National Natural Science Foundation excellent youth cultivation project (20202ZDB01017), the Science and technology plan project of Jiangxi Administration of traditional Chinese Medicine, China (2019A067).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors claim no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, LL., Wang, Y., Xiao, ZK. et al. Heat shock protein B8 promotes proliferation and migration in lung adenocarcinoma A549 cells by maintaining mitochondrial function. Mol Cell Biochem 476, 187–197 (2021). https://doi.org/10.1007/s11010-020-03896-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-020-03896-3