Abstract
Deficiency or defective transport of riboflavin (RF) is known to cause neurological disorders, cataract, cardiovascular anomalies, and various cancers by altering the biochemical pathways. Mechanisms and regulation of RF uptake process is well characterized in the cells of intestine, liver, kidney, and brain origin, while very little is known in the heart. Hence, we aimed to understand the expression and regulation of RF transporters (rRFVT-1 and rRFVT-2) in cardiomyocytes during RF deficiency and also investigated the role of RF in ischemic cardiomyopathy and mitochondrial dysfunction in vivo. Riboflavin uptake assay revealed that RF transport in H9C2 is (1) significantly higher at pH 7.5, (2) independent of Na+ and (3) saturable with a Km of 3.746 µM. For in vivo studies, male Wistar rats (110–130 g) were provided riboflavin deficient food containing 0.3 ± 0.05 mg/kg riboflavin for 7 weeks, which resulted in over expression of both RFVTs in mRNA and protein level. RF deprivation resulted in the accumulation of cardiac biomarkers, histopathological abnormalities, and reduced mitochondrial membrane potential which evidenced the key role of RF in the development of cardiovascular pathogenesis. Besides, adaptive regulation of RF transporters upon RF deficiency signifies that RFVTs can be considered as an effective delivery system for drugs against cardiac diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
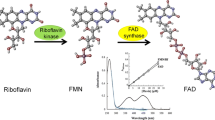
Riboflavin (RF), otherwise known as vitamin B2 is one of the water-soluble vitamins essential for various flavoenzymes involved in oxidation–reduction reactions by means of its cofactors, flavin mononucleotide (FMN) and flavin adenine dinucleotide (FAD) [1, 2]. Deficiency of RF leads to irregularities in biochemical pathways and causes diseases like neurological disorders [3], cataract [4], and various cancers, etc. However, vertebrates are devoid of the capability to synthesis such a crucial micronutrient. Although gut microflora synthesis riboflavin in minimal quantity, it cannot subsidize the requirement of riboflavin by vertebrates, hence the major source of RF is by dietary intake, which is primarily absorbed in the intestine transporters. As soon as riboflavin enters the blood stream, it is transported to each organ by means of tissue specific RFVTs. Hitherto, three genes, SLC52A1/hRFVT-1, SLC52A2/hRFVT-2, and SLC52A3/hRFVT-3 have been identified and characterized to transport riboflavin in human [5,6,7,8], whereas in rat only two RFVTs (rRFVT-1 and rRFVT-2) have been characterized [5, 9, 10]. The ortholog rRFVT-1 (reported as human ortholog of the porcine receptor for endogenous retrovirus A [11]) in rat showed 81.41% similarity with hRFVT-2 and rRFVT-2 showed 75.97% similarity with hRFVT-3. Functional characterization showed that SLC52A2 is involved in hepatic riboflavin homeostasis in rat [12], while knock out of SLC52A3 in mice resulted in impaired riboflavin uptake and neonatal lethality, thus proved that SLC52A3 is responsible for placental riboflavin transport [13]. Riboflavin deficiency resulted in various disorders including mitochondrial myopathies, where its supplementation was shown to normalize the biochemical abnormalities in neurological disorders [14] and complex I deficiency of electron transport chain [15]. Besides the deficiency of riboflavin, mutations associated with any of these transporters may also lead to diseased conditions by altering the vitamin transport physiology [16,17,18,19]. Thus, RFVTs are crucial for transporting and maintaining RF homeostasis in the body.
As RF is involved in various biochemical pathways, its deficiency may lead to accumulation of unusual or lethal metabolic products. For instance, homocysteine, an atypical amino acid, which is involved in the pathogenesis of Parkinson’s and Alzheimer’s diseases [20, 21] is also considered as a risk for cardiovascular diseases [22,23,24,25]. Homocysteine is produced during the synthesis of an essential amino acid methionine in one carbon metabolism. MTHFR (10-methylenetetrahydrofolate reductase) is one of the flavin-dependent enzyme that require FAD for the conversion of N 5,N 10-methylenetetrahydrofolate to N 5-methyltetrahydrofolate with subsequent conversion of homocysteine to methionine in remethylation pathway of methionine. Furthermore, homocysteine along with reactive oxygen species (ROS) produced during cell division, exert toxic effects in mitochondria by altering mitochondrial membrane potential and permeability [26,27,28]. Hence, RF deficiency results in accumulation of homocysteine with subsequent alteration of membrane potential and causes cardiovascular abnormalities. Further, administration of homocysteine-related compounds in male Wistar albino rats, showed a reduction in the contraction ability of cardiac muscle with decreased dp/dt max value (maximum rate of pressure in the left ventricle) [29]. Likewise, dietary RF and MTHFR deficiency in mice during pregnancy resulted in prominent increases in the incidence of congenital abnormalities with decreased left ventricular wall thickness in embryonic hearts [30]. On the other hand, cardioprotective effects of RF against diabetic cardiomyopathy in rats have been demonstrated by reduced formation of lipid peroxides and carbonyl content and also by the increased production of antioxidant enzymes like superoxide dismutase (SOD) and heme oxygenase (HO) [31].
The heart contains high levels of RF [32], which is known to be essential for its normal cellular physiology, structure, and function. However, cardiac muscle cells in mammals are devoid of the ability to synthesize RF and are dependent on exogenous dietary sources through transport across cell membrane. Despite the importance of RF, there is nothing much known about the molecular mechanisms that regulate the RF uptake process and about the distribution of RF transporters in cardiovascular system. In this study, we have aimed to understand the expression pattern of RFVTs in cardiomyocytes using cultured rat cardiomyoblast H9C2 cells and its consequences upon RF deficiency in in vivo conditions with Wistar rats as an animal model. In addition, the molecular mechanisms behind the regulation of homocysteine levels and alteration of membrane potential by RF was determined and correlated with mitochondrial dysfunction in cardiomyocytes.
Materials and methods
Cell culture and maintenance
H9C2, a cardiomyoblast cell line of embryonic rat ventricle origin obtained from National Centre for Cell Science, Pune, India was cultured and maintained in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% FBS, glutamine (0.29 g/L), sodium bicarbonate (2.2 g/L), penicillin (100,000 U/L), and streptomycin (10 mg/L). Cells were grown in 75-cm2 plastic flasks at 37 °C in a 5% CO2-95% air atmosphere with media changes at every 2 days. Experiments were performed using cells between passages 10 and 16. H9C2 cells were subcultured by trypsinization with 0.05% trypsin and 0.9 mM EDTA in PBS free from Ca2+ and Mg2+ and plated onto 24-well plates at a density of 1 × 105 cells/well. Uptake of RF was performed 2–3 days following confluence.
Animal handling and maintenance
All the animal experiments were performed in accordance with Institutional Ethical Committee of Madurai Kamaraj University, Madurai, India. Standard and RF-deficient food pellet was purchased from Krish Scientific Shoppe, Bangalore, India. Male Wistar rats (age 6 weeks; body weight 110–130 g) were used throughout the study and they were maintained in 25 ± 2 °C with an alternating 12 h dark/light cycle. Initially, during acclimatization period all the animals were fed ad libitum with standard chow (AIN-93M) containing 6.50 ± 0.42 mg/kg RF for 2 weeks. Subsequently, the animals were provided with RF-deficient food pellet containing 0.3 ± 0.05 mg/kg RF [10] for 7 weeks, while the animals in control group were provided with standard pellet. Then the experimental animals were euthanized with pentobarbital sodium (50 mg/kg) and organs were collected for further functional characterization.
Effect of pH, Na+ and extracellular RF levels on RF uptake by H9C2 cells
RF uptake assay was performed with confluent monolayers of H9C2 cells by incubating with KR buffer containing [3H]-riboflavin (6.2 Ci/mmol with 96% radiochemical purity was purchased from Moravek Biochemicals, Inc, USA) at 37 °C for 10 min. Labeled and unlabeled RF were added to the incubation buffer at the onset of uptake experiment and the reaction was terminated after 10 min of incubation by the addition of 2 ml of ice-cold KR buffer followed by immediate aspiration. Cells were then digested by incubating at 80 °C for 20 min with 1 N NaOH followed by neutralization with 10 N HCl. Digested cell contents were harvested and then counted for radioactivity using a Scintillation counter (Beckman Coulter LS6500). The protein content of cell digests was measured from the experimental and control wells using Bradford assay and used for the normalization of uptake data. To determine the effect of pH on RF uptake, the assay was performed with KR buffer adjusted to different pH ranging from 5.5, 6.5, 7.5, and 8.5. Na+ dependency of RF uptake was tested by isosmotically replacing the Na+ in the incubation buffer with other monovalent cation, namely lithium or with the nonionic mannitol. Similarly to determine the rate of RF uptake by H9C2 cells, uptake assay was performed with increasing concentration of riboflavin (0.0075–4.0 µM).
Semi-quantitative PCR
Total RNA from confluent H9C2 cells and cardiac tissue of male Wistar rats (100 mg) was isolated using the guanidine isothiocyanate-based TRIzol solution (Bio Basic Inc., Canada) according to the manufacturer’s specifications. Three micrograms of total RNA were reverse transcribed with oligo(dT) primers using QuantiTect® Reverse Transcription Kit (Qiagen) following the manufacturer’s instructions. Semi-quantitative PCR was performed to determine the expression level of rRFVT-1 and rRFVT-2 in the H9C2 cells as described previously [33]. Gene-specific primers corresponding to the PCR targets were designed using the standard specifications. For the rRFVT-1, the primers were forward, 5′-CCCGCTGTACAGAGCTTTTC-3′; reverse, 5′-CAGCAGACAGAGGCCATACA-3′. For rRFVT-2, the primers were forward, 5′- CTGTCACCTTCTTGCCCTTC-3′; reverse, 5′-GGTGATACCTGAGCCTTGGA-3′. For GAPDH, the primers were forward, 5′-CCATCACCATCTTCCAGGAG-3′; reverse, 5′-CCTGCTTCACCACCTTCTTG-3′. For each 50 µl PCR reaction, 2 µl of cDNA was used as template and the amplification program consisted of 1 cycle at 94 °C with a 2-min hold followed by 20–30 cycles at 94 °C for 1 min, specified annealing temperature with 45 s, 72 °C with 30 s for extension. GAPDH was used as internal control. The PCR samples were electrophoresed on 2.0% agarose gels in TAE buffer and imaged. Densitometry values were measured at each cycle sampling using the ImageJ software. RT-PCR values are presented as a ratio of the specified gene’s signal in the selected linear amplification cycle divided by the GAPDH signal.
Western blotting
Expression of rRFVT-1 and -2 proteins in normal and riboflavin-deficient rats were examined by western blotting. Fresh heart tissue (100 mg) was minced with RIPA lysis buffer (containing 0.01 M Tris–HCl buffer pH 7.4, 1% Triton X-100, 1% sodium deoxycholate, 1% SDS), supplemented with 1 mg/ml protease inhibitors, incubated at 4 °C for 1 h and homogenized [34]. Tissue homogenates were centrifuged at 13,000 rpm for 3 min at 4 °C and supernatant was harvested for protein estimation. Subsequently, 60 μg of protein was resolved on 10% SDS-PAGE. Proteins were transferred to PVDF membrane and the membrane was blocked with 5% skim milk in Tris-buffered saline (pH 7.4)/0.1% Tween 20. The membrane was incubated overnight with primary antibodies specific for rRFVT-1 (GPR172A rabbit polyclonal antibody-Orb183899, Biorbyt) and rRFVT-2 (C20ORF54 rabbit polyclonal antibody-SC-85426, Santa Cruz) at a dilution of 1:300 and then washed three times with Tris-buffered saline. Subsequently, the membrane was incubated with secondary antibody coupled with HRP at a dilution of 1:1000 (Goat anti-rabbit IgG-HRP-SC-2004, Santa Cruz) for 1 h. The expression level of rRFVT-1 and rRFVT-2 was determined based on the immunoreactive bands observed after developing with 3,3′-diaminobenzidine tetrahydrochloride (DAB).
Expression profile of cardiac biomarkers
Blood sample obtained from the RF-deficient rats were checked for the levels of cardiac biomarkers to determine the effect of riboflavin deficiency on cardiomyopathy. Briefly, blood samples were collected from normal and RF-deficient rats after 7 weeks of riboflavin deficiency and the well-known cardiac biomarkers, viz., homocysteine, creatine kinase, and creatine kinase myoglobin in serum samples were measured quantitatively based on the release of NADH using ERBA kits and the chemiluminescence was measured by auto analyzer. Neverthless, qualitative assay was performed to detect the presence of troponin-I based on sandwich immunoassay using rapid diagnostic kit.
Histopathological examinations
After 7 weeks of experimental conditions, animals were euthanized and heart was excised from normal and RF-deficient rats to examine the myocardial damage. For histopathological investigations, excised heart was placed in 4% formaldehyde with 2% sodium acetate. The tissue was then embedded in paraffin and cut to a thickness of 5 mm. Histopathological tissue sections of heart were stained with hematoxylin and eosin and then observed under light microscope to study for any morphological changes by RF deficiency.
ROS and mitochondrial membrane potential
Reactive oxygen species (ROS) production was estimated as a measure of cell death using flow cytometer. For this, cells were dissociated from excised heart tissue by means of cell dissociation solution (Sigma, USA) and assessed for the internal ROS production by treating with 2′,7′-dichlorodihydrofluorescein diacetate (H2DCF-DA) (Sigma, USA) for 30 min. H2DCF-DA, a non-fluorescent compound which upon deacetylation and oxidation reaction by ROS produce highly fluorescent DCF (2′,7′-dichlorofluorescein). In addition, mitochondrial membrane potential is crucial for the production of ATP during respiratory chain. Hence, the integrity of mitochondrial membrane was evaluated by treating with MitoTracker Deep Red (Thermo Scientific Fisher, USA), mitochondria-selective probe for 15 min. A total of 10,000 cells were used to assess the ROS production and membrane potential based on the fluorescence emission using flow cytometer (BD FACSAria III, BD Biosciences, USA). FlowJo software was used for data analysis and to discriminate the cell cycle phases.
Statistical analysis
Kinetic parameters of the saturable component of RF uptake were calculated by subtracting the diffusing component [determined from the slope of the uptake line between a high substrate concentration of RF (1 mM) and the point of origin] from total uptake at each concentration using Michaelis–Menten equation as described previously [35].
Results
Effect of pH, Na+ and extracellular RF levels on RF uptake by H9C2 cells
Experiments were performed to understand and validate the potential of cardiomyoblast cell line (H9C2) for RF transport across the membrane using radiolabeled RF (3H-RF). Initially, we investigated pH dependency of cardiomyocytes in RF transport by performing RF uptake assay using 3H-RF in KR buffer with different pH ranging from 5.5 to 8.5 and varying ions. The results showed RF (7.5 nM) uptake to be pH dependent as maximum of RF uptake was at pH 7.5 and started to decline with either increasing or decreasing the pH to acidic and alkaline conditions. At acidic pH 5.5, 77% RF uptake rate was lost, and 24% RF uptake rate was lost in alkaline pH 8.5 when compared with pH 7.5 (Fig. 1A). In addition, the effect of 3H-RF uptake by H9C2 was studied by replacing sodium ion with equimolar concentrations of lithium chloride and mannitol, no changes in the RF uptake was noticed (Fig. 1B), which demonstrated that Na+ is not essential for driving riboflavin uptake. Thus, the results revealed that RF uptake in cardiomyocyte is pH dependent and sodium independent.
Riboflavin uptake by H9C2 (2–1) cells in different conditions. (A) Effect of incubation buffer pH, (B) Effect of Na+ ion replacement, and (C) different concentrations of riboflavin. Confluent monolayer of H9C2 (2–1) cells were incubated in respective KR buffers with 7.5 nM of 3H-RF for 10 min at 37 °C. Data are mean ± S.E.M. of 3–4 separate uptake experiments
In another study, we examined the initial rate of RF uptake by H9C2 cells as a function of substrate concentration in the KR buffer with pH 7.5 (0.0075–4.0 µM). As shown in the Fig. 1C, the results showed that RF uptake was concentration dependent and saturable. The apparent Km and Vmax of the saturable component of RF uptake were then determined and was found to be 3.746 µM and 56.391 pmol/mg protein/10 min, respectively. Thus, it is evident from these results that RF uptake in H9C2 cells is a carrier mediated process in nature.
Effect of riboflavin deficiency in vivo
After 7 weeks of RF deprivation, the experimental animals were examined for body weight and heart weight. As a result, the body weight and heart weight of male Wistar rats fed with RF-deficient diet was 190 ± 10 and 0.81 ± 0.1 g, while the body weight of normal Wistar rat was found to be 210 ± 15 and 0.86 ± 0.1 g, respectively. These results denoted that RF deprivation in rats showed a significant reduction in the final body weight (P < 0.05) than control, while changes were not significant with the heart size between the groups. Plasma concentrations of RF were significantly lower in the rats fed with RF deficient diet (2.4 µg/dL) than the control (4 µg/dL).
RF transporters expression in the cardiomyocyte H9C2 cells and rat heart
Rodents are known to contain two RF transporters RFVT-1 and RFVT-2, where RFVT-1 is orthologous to hRFVT-1 and hRFVT-2; RFVT-2 is orthologous to hRFVT-3. Thus, to further enhance our understanding the molecular mechanisms responsible for RF uptake, we initially performed semi-quantitative PCR to determine the expression levels of RF transporters in the H9C2 cell lines. The results show that both the transporters rRFVT-1 and rRFVT-2 were expressed at mRNA levels in cardiomyocytes. In comparison, the basal level expression of rRFVT-1 mRNA was four times higher than rRFVT-2 mRNA in H9C2 cell line (Fig. 2A). We next investigated the effect of RF deficiency in vivo in the whole heart tissue of rats fed on a RF-deficient chow for 7 weeks compared to controls. As a result, due to riboflavin deprivation the expression of rRFVT-1 and rRFVT-2 mRNA was 0.9- and 1.1-fold higher in cardiac tissue of RF-deficient rats than controls (Fig. 2B).
Semi-Quantitative PCR analysis. Tissue distribution of rRFVT-1 and -2 mRNA in rat cardiomyocytes cell line H9C2 (2–1) (A) in vitro and (B) its adaptive regulation upon RF deficiency in cardiac tissue in vivo. Data were normalized relative to the expression of GAPDH. Inlet Semi-quantitative RT-PCR products analyzed in 2% agarose gel (**P < 0.01)
In addition to mRNA expression, the expression of RF transporters at protein level was also assessed by western blotting, which revealed that both rRFVT-1 and rRFVT-2 proteins were expressed in the rat heart tissues (Fig. 3). Albeit, the expression of both rRFVT-1 and rRFVT-2 was higher at protein levels in cardiac tissue of RF deficient rats compared to normal rats, expression of rRFVT-1 was significantly higher compared to rRFVT-2 (Fig. 3). Thus, it is evidently observed that RF uptake process is adaptively regulated in the rat heart based on the extracellular RF levels, where both the RF transporters play a major role in such regulation in the cardiac tissue.
Western blotting analysis for the expression of rRFVT-1 and -2 protein in cardiac tissue of control and RF deficient rats. Protein was isolated from cardiac tissue of control and RF deficient rats using RIPA lysis buffer, separated in 10% SDS-PAGE and transferred to PVDF membrane. Immuno reactive bands were observed upon incubation with 1:300 dilution of specific primary and 1:1000 dilution of secondary antibodies
Expression profile of cardiac biomarkers
Having understood the obvious changes in the expression pattern of RF transporters in the heart during RF deficiency, we were intended to underscore any adverse effects in the heart function by RF deficiency. For this, blood sample was collected from normal and RF deficient rats and the level of expression of cardiac biomarkers in the serum samples were determined. As a result, the level of homocysteine, creatine kinase, and creatine kinase myoglobin were 1.3-, 1.4-, and 2.0-fold higher in RF-deficient rats compared to normal rats (Table 1). Likewise, qualitative analysis performed to check the presence of Troponin-I in RF-deficient rat using specific strip showed a band in the test region, while there was no band in the strip containing serum of control rats (Supplementary Fig. S1), thus showing the increase of Troponin-I levels in RF-deficient rats. Therefore, the elevated levels of gold standard cardiac biomarkers that were recorded in RF-deficient rat are indicative of cardiac injury in the animal model by RF deficiency.
Histopathological studies
Next, we investigated whether any gross anatomical changes are induced during RF deficiency by histology with the heart excised from normal and deficient rats by examining under light microscope after staining with hematoxylin–eosin. The results showed aberrations such as degeneration of muscle fibers, loss of cross striations and dwindle nuclei in heart tissue of RF deficient rats, while in control rats the elongated nuclei and intercalated discs were clear (Fig. 4). Therefore, histological examinations suggested that RF deficiency resulted in disruption of the cellular architecture of cardiac cells.
ROS and mitochondrial membrane potential
To determine whether RF deficiency leads to cardiac dysfunction, the level of ROS and the integrity of mitochondrial membrane potential were investigated by flow cytometry. As shown in the Fig. 5, a shift or reduction in fluorescent intensity in FACS revealed that heart mitochondrial membrane potential and ROS production (APC and FITC respectively) was reduced in RF deficient conditions. In comparison, a decrease in ROS production was observed in deficient rats (0.9%) compared to control rats (10%) (Fig. 5A). Also, a significant reduction in mitochondrial membrane potential was observed in deficient rats (80%) than control (98%) (Fig. 5B). Hence, these results collectively illustrated that RF deficiency resulted in cardiac myopathy in rats in vivo.
Discussion
Riboflavin regulates cellular processes by means of FMN and FAD, which catalyze various biological reactions of carbohydrate, protein, lipid, and other vitamin metabolism [36]. Distribution of RFVTs and its mechanism behind RF transport have been characterized in different organs like liver, kidney, intestine, retina, and brain. Heart is another important organ, which serves as body’s circulatory pump, wherein RF deficiency complications act as one of the leading cause of cardiovascular diseases. Cardiovascular diseases that arise due to unhealthy diet, obesity, use of tobacco, alcohol, etc., are the major cause of death globally. According to WHO 2012, 17.5 million people died from CVD worldwide. But then the precise mechanism behind riboflavin transport and its regulations were poorly understood. This study has revealed that the optimum physiological pH for riboflavin transport by cardiomyocytes is 7.5 and the transport process is Na+ independent since there is no effect on the replacement of Na+ ion. Thus, RF transport mechanisms in cardiomyocytes were reasonably similar to the mechanism of RF transport by HK-2 cells [37], BeWo cells [38], ARPE-19 [39], and primary hepatocyte of mice [12].
Functional characterization of RFVTs in rat demonstrated that rRFVT-1 is mainly distributed in intestine and able to transport RF in minimal amount [5], while rRFVT-2 is a major intestinal RF transporter predominantly involved in RF absorption from diet [9, 10]. A significant increase in the rRFVT-1 expression at mRNA level indicates that rRFVT-1 is the predominant transporter in cardiomyocyte H9C2 cells compared to rRFT-2. However, a profound increase in the expression of both rRFVT-1 and rRFVT-2 was observed in RF-deficient conditions in the rat heart tissue in vivo. Furthermore, elevated expression of rRFVT-1 and rRFVT-2 at protein level during RF deficiency was also demonstrated consistently. Though changes in the bodyweight between control and deficient rats were noticed, no significant changes were observed in the body-to-heart weight ratio in vivo. Overall, these results clearly evidenced that RF uptake process is adaptively regulated in the rat heart depending upon the extracellular RF concentrations, where both rRFVT-1 and rRFVT-2 play a major role in such regulation in the cardiac tissue, which appears to be mediated (in part) via transcriptional regulatory mechanisms.
Riboflavin by means of FAD regulates the catabolic pathway of homocysteine, which is well known as a noxious amino acid. RF deficiency was previously shown to elevate the level of homocysteine [40] which ultimately leads to cardiac dysfunction. Therefore, the levels of homocysteine, creatine kinase, creatine kinase myoglobin, and cardiac Troponin-I which are deliberated as an early sensitive diagnostic marker for acute myocardial infraction [41] were evaluated in this study. As a result, the increased level of cardiac biomarkers such as homocysteine, creatine kinase, creatine kinase myoglobin, and Troponin-I than its normal range in the course of RF deficiency suggest that male rats fed with RF-deficient feed were found to have impaired cardiac functions and resulted in cardiomyopathy. Subsequently, abnormalities witnessed in the texture of RF-deficient cardiac muscle could be due to the accumulation of cardiac biomarkers which further altered the normal pathophysiology of cardiac tissues like ventricular and coronary dysfunction, degeneration of muscle fiber, loss of distinct nuclei, and muscle contraction efficiency, etc.
Cardiomyocytes require high energy for its contraction which can be obtained from the ATP generated in mitochondria. Hence, the integrity of mitochondrial membrane potential is essential for the constant production and supply of ATP. However, the decrease in mitochondrial membrane potential in RF-deficient cardiac tissue could be associated with mitochondrial dysfunction and apoptosis due to irregularities in the cardiac profile. Several studies have shown that homocysteine induces ROS production and leads to apoptosis [42]. On the contrary, in some cases homocysteine is proved to regulate the production of ROS differentially in each organ based on the physiology [43]. For instance, homocysteine was found to increase the level of ROS in kidney mitochondria and reduce it in rat liver, brain, and heart mitochondria [44]. Thus, the reduced ROS production observed in RF-deficient cardiac tissue suggests that homocysteine does not necessarily induce ROS production for the cells to undergo apoptosis.
Riboflavin transporters seem to have a key role in maintaining riboflavin homeostasis in heart and may be suitable targets for various drugs with therapeutic potential against cardiovascular diseases. Administration of drugs through G-protein-coupled receptors (GPCR) is an effective method than other drug delivery strategies, as they are transducers of extracellular signals and modulators of intracellular signaling. Previously, vitamin transporter like vitamin B9 [45] and B12 [46] were utilized in drug delivery for numerous diseases and were shown to enhance the absorption of drugs conjugated to vitamins. Since, rRFVT-1 is a GPCR with crucial role in heart, it can serve as an possible drug target for drugs like prostaglandins, pyrvinium pamoate for treating congestive heart failure and acute myocardial infarction by conjugating with riboflavin, which can pass specifically through RFVTs across the membrane. Likewise, rRFVT-2 deliberated as an ortholog of hRFVT-3 can also be utilized as a therapeutic option for cardioprotective and cardiorestorative treatments.
Conclusions
The results in this study serve as an evidence for the presence of two RF transporters (rRFVT-1 and rRFVT-2) in cardiac tissue of rat. In addition, we have shown that both riboflavin transporters are adaptively regulated upon RF deficiency. We also showed that the deprivation of RF leads to the accumulation of cardiac biomarkers, alteration of cardiac pathophysiology, and reduction of mitochondrial membrane potential and thus resulted in congenital heart disease. As a consequence, it is clear that supplementation of RF would be beneficial to alleviate the pathologic complications in the heart. Moreover from a pharmaceutical perspective, RF transporters could serve as one of the promising route for target-specific drug delivery into the cells and tissues for treatment against cardiovascular diseases.
References
Barquera B, Zhou W, Morgan JE, Gennis RB (2002) Riboflavin is a component of the Na+-pumping NADH-quinone oxidoreductase from Vibrio cholera. Proc Natl Acad Sci USA 99(16):10322–10324
Lienhart W-D, Gudipati V, Macheroux P (2013) The human flavoproteome. Arch Biochem Biophys 535(2):150–162
Cooperman JM, Lopez R (1984) Riboflavin. In: Machlin LJ (ed) Handbook of vitamins: nutritional, biochemical and clinical aspects. Dekker, New York, pp 299–327
Cumming RG, Mitchell P, Smith W (2000) Diet and cataract: the Blue Mountains Eye Study. Ophthalmology 107(3):450–456
Yonezawa A, Masuda S, Katsura T, Inui K (2008) Identification and functional characterization of a novel human and rat riboflavin transporter, RFT1. Am J Physiol Cell Physiol 295:632–641
Yao Y, Yonezawa A, Yoshimatsu H, Masuda S, Katsura T (2010) Identification and comparative functional characterization of a new human riboflavin transporter hRFT3 expressed in the brain. J Nutr 140(7):1220–1226
Subramanian VS, Subramanya SB, Rapp L, Marchant JS, Ma TY, Said HM (2011) Differential expression of human riboflavin transporters-1, -2, and -3 in polarized epithelia: a key role for hRFT-2 in intestinal riboflavin uptake. Biochim Biophys Acta Biomembr 1808(12):3016–3021
Yoshimatsu H, Yonezawa A, Yao Y, Sugano K, Nakagawa S, Omura T, Matsubara K (2014) Functional involvement of RFVT3/SLC52A3 in intestinal riboflavin absorption. Am J Physiol Gastrointest Liver Physiol 306(2):102–110
Yamamoto S, Inoue K, Ohta KY, Fukatsu R, Maeda JY, Yoshida Y, Yuasa H (2009) Identification and functional characterization of rat riboflavin transporter 2. J Biochem 145(4):437–443
Fujimura M, Yamamoto S, Murata T, Yasujima T, Inoue K, Ohta KY, Yuasa H (2010) Functional characteristics of the human ortholog of riboflavin transporter 2 and riboflavin-responsive expression of its rat ortholog in the small intestine indicate its involvement in riboflavin absorption. J Nutr 140(10):1722–1727
Ericsson TA, Takeuchi Y, Templin C, Quinn G, Farhadian SF, Wood JC, Oldmixon BA, Suling KM, Ishii JK, Kitagawa Y, Miyazawa T, Salomon DR, Weiss RA, Patience C (2003) Identification of receptors for pig endogenous retrovirus. Proc Natl Acad Sci USA 100:6759–6764
Yao Y, Yonezawa A, Yoshimatsu H, Omura T, Masuda S, Matsubara K (2013) Involvement of riboflavin transporter RFVT2/Slc52a2 in hepatic homeostasis of riboflavin in mice. Eur J Pharmacol 714:281–287
Yoshimatsu H, Yonezawa A, Yamanishi K, Yao Y, Sugano K, Nakagawa S, Imai S, Omura T, Nakagawa T, Yano I, Masuda S, Inui K, Matsubara K (2016) Disruption of Slc52a3 gene causes neonatal lethality with riboflavin deficiency in mice. Sci Rep 6:27557
Bosch AM, Abeling NGGM, Ijlst L, Knoester H, Van Der Pol WL, Stroomer AEM, Wanders RJ, Visser G, Wijburg FA, Duran M, Waterham HR (2011) Brown-Vialetto-Van Laere and Fazio Londe syndrome is associated with a riboflavin transporter defect mimicking mild MADD: a new inborn error of metabolism with potential treatment. J Inherit Metab Dis 34:159–164
Griebel V, Krigeloh-Mann I, Ruitenbeek W, Trijbels JMF, Paulus W (1990) A mitochondrial myopathy in an infant with lactic acidosis. Dev Med Child Neurol 32:528–531
Green P, Wiseman M, Crow YJ et al (2010) Brown-Vialetto-Van Laere Syndrome, a ponto-bulbar palsy with deafness, is caused by mutations in C20orf54. Am J Hum Genet 86(3):485–489
Johnson JO, Gibbs JR, Van Maldergem L, Houlden H, Singleton AB (2010) Exome sequencing in Brown-Vialetto-van Laere syndrome. Am J Hum Genet 87(4):567–569
Johnson JO, Gibbs JR, Megarbane A et al (2012) Exome sequencing reveals riboflavin transporter mutations as a cause of motor neuron disease. Brain 135(9):2875–2882
Haack TB, Makowski C, Yao Y et al (2012) Impaired riboflavin transport due to missense mutations in SLC52A2 causes Brown-Vialetto-Van Laere syndrome. J Inherit Metab Dis 35(6):943–948
Duan W, Ladenheim B, Cutler RG, Kruman II, Cadet JL, Mattson MP (2002) Dietary folate deficiency and elevated homocysteine levels endanger dopaminergic neurons in models of Parkinson’s disease. J Neurochem 80(1):101–110
Kruman II, Culmsee C, Chan SL, Kruman Y, Guo Z, Penix L, Mattson MP (2000) Homocysteine elicits a DNA damage response in neurons that promotes apoptosis and hypersensitivity to excitotoxicity. J Neurosci 20(18):6920–6926
Clare R, Daly L, Robinson K, Naughten E, Cahalane S, Fowler B, Graham I (1991) Homocysteinemia: an independent risk factor for vascular disease. NEJM 324(17):1149–1155
Stampfer MJ, Malinow MR, Willett W, Newcomer LM, Upson B, Ullmann D, Tishler PV, Hennekens CH (1992) A prospective study of plasma homocysteine and risk of myocardial infarction in US physicians. JAMA 268:877–881
Boushey CJ, Beresford SA, Omenn GS, Motulsky AG (1995) A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA 274:1049–1057
Wang CY, Chen ZW, Zhang T, Liu J, Chen SH, Liu SY, Han LY, Hui ZH, Chen YM (2014) Elevated plasma homocysteine level is associated with ischemic stroke in Chinese hypertensive patients. Eur J Intern Med 25(6):538–544
Reid RA, Moyle J, Mitchell P (1992) Synthesis of adenosine triphosphate by a proton motive force in rat liver mitochondria. Nature 212:257–258
Ratter F, Gassner C, Shatrov V, Lehmann V (1999) Modulation of tumor necrosis factor-alpha-mediated cytotoxicity by changes of the cellular methylation state: mechanism and in vivo relevance. Int Immunol 11(4):519–527
Lassus P, Opitz-Araya X, Lazebnik Y (2002) Requirement for caspase-2 in stress-induced apoptosis before mitochondrial permeabilization. Science 297:1352–1354
Zivkovic V, Jakovljevic V, Djordjevic D, Vuletic M, Barudzic N, Djuric D (2012) The effects of homocysteine-related compounds on cardiac contractility, coronary flow, and oxidative stress markers in isolated rat heart. Mol Cell Biochem 370:59–67
Chan J, Deng L, Mikael LG et al (2010) Low dietary choline and low dietary riboflavin during pregnancy influence reproductive outcomes and heart development in mice. Am J Clin Nutr 91(4):1035–1043
Wang J, Yuan X, Sun B, Cao Y (2011) Inhibition of lipid peroxidation by enzymatic hydrolysates from wheat bran. Food Technol Biotechnol 49(4):481–488
Schaus R, Kirk JE, Lauresn TJS (1955) The riboflavin content of human aortic tissue. J Gerontol 10:170–177
Ashokkumar B, Mohammed ZM, Vaziri ND, Said HM (2007) Effect of folate oversupplementation on folate uptake by human intestinal and renal epithelial cells. Am J Clin Nutr 86(1):159–167
Rohrbach S, Yan X, Weinberg EO, Hasan F, Bartunek J, Marchionni MA, Lorell BH (1999) Neuregulin in cardiac hypertrophy in rats with aortic stenosis. Differential expression of erbB2 and erbB4 receptors. Circulation 100(4):407–412
Ashokkumar B, Vaziri ND, Said HM (2006) Thiamin uptake by the human-derived renal epithelial (HEK-293) cells: cellular and molecular mechanisms. Am J Physiol Renal Physiol 291(4):796–805
Bates CJ, Fuller NJ (1986) The effect of riboflavin deficiency on metheylenetetrahydrofolate reductase (NADPH) and folate metabolism in the rat. Br J Nutr 55:455–464
Kumar CK, Yanagawa N, Ortiz A, Said HM (1998) Mechanism and regulation of riboflavin uptake by human renal proximal tubule epithelial cell line HK-2. Am J Physiol 274:F104–F110
Huang S, Swaan PW (2001) Riboflavin uptake in human trophoblast-derived BeWo cell monolayers: cellular translocation and regulatory mechanisms. J Pharmacol Exp Ther 298(1):264–271
Said HM, Wang S, Ma TY (2005) Mechanism of riboflavin uptake by cultured human retinal pigment epithelial ARPE-19 cells: possible regulation by an intracellular Ca2+-calmodulin-mediated pathway. J Physiol 566:369–377
Lakshmi R, Lakshmi V, Bamji MS (1990) Mechanism of impaired skin collagen maturity in riboflavin or pyridoxine deficiency. J Biosci 15(4):289–295
Adams JE, Abendschein DR, Jaffe AS (1993) Biochemical markers of myocardial injury. Is MB creatine kinase the choice for the 1990s? Circulation 88(2):750–763
Sipkens JA, Krijnen PAJ, Meischl C et al (2007) Homocysteine affects cardiomyocyte viability: concentration-dependent effects on reversible flip-flop, apoptosis and necrosis. Apoptosis 12(8):1407–1418
Forneris F, Battaglioli E, Mattevi A, Binda C (2009) New roles of flavoproteins in molecular cell biology: histone demethylase LSD1 and chromatin. FEBS J 276:4304–4312
Gomez J, Sanchez-Roman I, Gomez A, Sanchez C, Suarez H, Lopez-Torres M, Barja G (2011) Methionine and homocysteine modulate the rate of ROS generation of isolated mitochondria in vitro. J Bioenerg Biomembr 43(4):377–386
Lu Y, Low PS (2002) Folate-mediated delivery of macromolecular anticancer therapeutic agents. Adv Drug Deliv Rev 54:675–693
Russell-Jones GJ, Westwood SW, Habberfield AD (1995) Vitamin B12 mediated oral delivery systems for granulocyte-colony stimulating factor and erythropoietin. Bioconjug Chem 6:459–465
Acknowledgements
BA acknowledges DBT-RGYI, INDIA for the financial support [No. BT/PR15134/GBD/27/330/2011] and ICMR, India for the International Biomedical Scientists Fellowship (No. INDO/FRC/452/(Y83)/2016-17-IHD). TU thank DST-PURSE, MKU for the fellowship. Authors gratefully acknowledge DST-PURSE Program (India), Madurai Kamaraj University for the infrastructure and facilities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict to declare in this research.
Electronic supplementary material
Below is the link to the electronic supplementary material.

11010_2017_3163_MOESM1_ESM.jpg
Supplementary Figure S1: Qualitative assay to detect the presence of Cardiac Troponin-I. Control (A) and RF deficient (B) rat using Troponin-I test strip. The presence of band in the test region of RF deficient sample indicates that the concentration of Troponin-I is greater than 1.5 ng/mL. Supplementary material 1 (JPEG 100 kb)
Rights and permissions
About this article
Cite this article
Udhayabanu, T., Karthi, S., Mahesh, A. et al. Adaptive regulation of riboflavin transport in heart: effect of dietary riboflavin deficiency in cardiovascular pathogenesis. Mol Cell Biochem 440, 147–156 (2018). https://doi.org/10.1007/s11010-017-3163-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-3163-1