Abstract
Cytokines play a key role in the pathogenesis of coronary artery disease (CAD). The aim of current study was to investigate the relationship between the serum concentrations of 12 cytokines with mortality and extent of CAD in individuals undergoing angiography and healthy controls. 342 CAD patients were recruited and divided into 2 groups: those with ≥50% occlusion in at least one coronary artery [Angiography (+)] or <50% obstruction in coronary arteries [Angiography (−)]. Also 120 healthy subjects were enrolled as control group. Lipid profile, fasting blood glucose, body mass index, and blood pressure were evaluated in all the subjects. An Evidence Investigator® was used for measuring 12 cytokines (IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, TNF-α, MCP-1, IFN-γ, EGF, VEGF) using sandwich chemiluminescent assays. Univariate analysis, multivariate regression models, ROC, and Kaplan–Meier survival curves were used for exploring the candidate markers in CAD patients. Serum level of IFN-γ, IL-4, MCP-1, EGF, IL-6, and IL-8 were markedly higher in angiogram-positive patients, while VEGF concentrations were significantly (P < 0.05) lower, compared to control group. ROC analysis for MCP-1 showed that a cut-off of 61.95 pg/mL had 91% sensitivity and 91% specificity for predicting CAD patients. Moreover, >2.16 pg/mL IL-6 had a > 94% sensitivity and 70% specificity in predicting 2 years mortality in the subjects with a serum MCP-1 > 61.95 pg/ mL, and patients having IL-6/MCP-1 combination had a shorter survival.Our findings demonstrate that CAD patients with serum MCP-1 and IL-6 levels of >61.95 and >2.16 pg/mL had a higher mortality with 94.1% sensitivity and 70.5% specificity for predicting mortality in CAD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is the leading cause of mortality globally. Despite advances in the identification of biomarkers useful for an early assessment of CAD risk, only a very small number of useful biomarkers have been identified. There is growing body of evidence demonstrating an association between serum pro- and anti- inflammatory cytokines in pathogenesis of CAD [1, 2]. Atherosclerosis is initiated following endothelial injury and subsequently induction of endothelial adhesion molecules that promote the accumulation of inflammatory cells within the vascular wall [3]. Cytokines are produced by various tissues, including the myocardium, arterial wall, adipose tissue, and cells of the immune system [4], that may be involved in the formation of atherosclerotic plaque, and may also contribute to plaque instability and rupture [3]. Inflammatory cells release proteases and cytokines which may affect cellular and matrix composition of plaque and its structural integrity [5, 6].
The inflammatory processes within the atherosclerotic artery may also stimulate an acute phase response that may be reflected in changes in cytokine concentrations in the peripheral blood [7]. These inflammatory cytokines may also lead to further endothelial dysfunction, leucocyte activation, and vascular smooth muscle cell proliferation [8]. They comprise pleiotropic and small proteins with a molecular weight of <25 kDa [5, 9] and are widely implicated in the orchestration of the inflammation process. Some of the major pro- and anti-inflammatory cytokines include interleukin (IL)-1, IL-2, IL-6, IL-10, interferon-γ (INF-γ),tumors necrosis factor-α (TNF-α),vascular endothelial growth factor (VEGF), monocyte chemotactic peptide-1 (MCP-1) [9]. TNF-α is an important pro-inflammatory cytokine, whilst IL-10 is an anti-inflammatory cytokine that has been reported to be expressed within the atherosclerotic plaque. The TNF-α/IL10 ratio has therefore been proposed as a good indicator of CAD progression [10]. In our previous study, we explored the pattern of 12 cytokines in patient with coronary artery bypass graft candidates and patients undergoing coronary angiography, with, or without obstructive coronary artery disease [11]. We found that low serum VEGF concentration had 92.1% sensitivity, 99.2% specificity, and 100% Positive Predictive value (PPV), and was associated with severity of coronary artery disease. Therefore, in the present study, we further explored the relationship between these cytokines/ growth factors and CAD in patients with and without positive angiography, and also evaluated dietary Intake, also looking at mortality at a 30 month follow-up in the patients.
Materials and methods
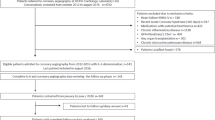
Population
A total of 342 CAD patients were recruited from Mashhad University of Medical Sciences (MUMS, Iran), who had signs or symptoms of cardiac disease (chest pain, ECG changes, unstable angina, angina of effort), who were further investigated by coronary angiography at Ghaem Medical Educational Hospital. Following angiography, these individuals were divided into two groups: those with significant angiographically defined CAD [Angiography (+)] (the case group) who had ≥50% occlusion in at least one coronary artery and those with a normal angiogram (<50% obstruction in coronary arteries) [Angiography (−)].
Moreover, 120 healthy subjects without a history of cardiovascular symptoms were also recruited. We followed all the subjects for 30 months after. Informed consent was obtained from all participants using protocols approved by the Ethics Committee of the MUMS (Ethics registration number: MUMS/900671).
Anthropometric and biochemical measurements
Anthropometric parameters including height, body weight, waist, and hip circumference were measured, as described previously [12]. Systolic and diastolic blood pressures (SBP OR DBP) were evaluated [12]. Fasted blood samples were collected into plain or fluoride-oxalate Vacutainer™ tubes (Catalog No: BD367841 and BD367814) [12]. Total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein, cholesterol, and glucose were measured using Cobas auto-analyser system (ABX Diagnostics, Montpellier, France) [12]. The results of the fasting blood glucose (FBG) <110 mg/dL were interpreted using American Diabetic Association criteria: normal values between 110 and 126 mg/dL, and those >126 mg/dL are considered as impaired fasting glucose (IFG) and DM, respectively [12, 13].
The laboratory measurement of cytokine
The concentrations of 12 cytokines and growth factors (IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, TNF-α, MCP-1, IFN-γ, EGF, and VEGF) were measured using an EV 3513 cytokine biochip array (Randox Laboratories, Crumlin, UK) and competitive chemiluminescence immunoassays (Randox Laboratories, Crumlin, UK), according to the manufacturer’s instructions and described previously [13, 14].
Dietary assessment
Participants’ dietary intake was assessed using 24-hour dietary recall questionnaire, and food analysis was performed using Diet Plan 6 software for evaluation of macro- and micro-nutrient intake.
Statistical analysis
Data were analyzed using SPSS-16 software (SPSS Inc., IL, USA). The Kolmogorov–Smirnov test was used to assess normality of data. Descriptive statistics (frequency/mean, and standard deviation) were determined for normally distributed variables and reported as mean ± SD, while median and IQR was used for non-normally distributed variables. Baseline demographics and clinical characteristics were compared using t-student test, one-way ANOVA test, Chi-square test, and/or Fisher exact test. Multivariate regression modeling and Binary Logistics model analyses were used to investigate the association of serum cytokines level and CAD in the presence of confounding variables (age, BMI, medication [statins] and gender). A ROC curve was constructed. Kaplan–Meier survival curves was analyzed. The statistical significance was set at P < 0.05.
Results
Demographic and clinical characteristics of the population
The clinical and baseline characteristics of the subjects are summarized in Table 1. The average age of subjects in control group, angiogram-negative and -positive groups were 53.26 ± 11.53, 54.78 ± 11.27, and 59.47 ± 11.30 years, respectively. Patients with angiographic evidence of stenosis in an epicardial coronary artery of >50% diameter (angio +) had a significantly higher BMI and FBG, while the level of HDL was significantly (P < 0.05) lower (Table 1). Moreover, there was a significant difference in the prevalence of diabetes mellitus between the groups (P < 0.001). LDL cholesterol concentrations were significantly different between the healthy subjects and the other two groups (P < 0.001), and this may have been related to usage of statin therapy (Table 1).
Altered serum cytokines profile in individuals with angiographically defined CAD
Serum cytokine concentrations are shown in Table 2. We observed that the levels of IFN-γ, IL-4, MCP-1, EGF, IL-6, and IL-8 were significantly (P < 0.05) higher in angiogram-positive subjects, compared to control group, while the serum concentration of VEGF were lower in the angiogram-positive group versus the control group (83.62 ± 69.14 vs. 132.67 ± 101.68). Similar results were also detected for IL-4, MCP-1, VEGF and IL-8 in angiogram-negative subjects with respect to control group (Table 2). Moreover, logistic regression models were constructed for the evaluation of the serum cytokine concentrations and several potential risk factors on the presence of CAD (Supplemental Table 1; Table 3). To perform this analysis, the relationship between cytokines and coronary artery risk factors on CAD among subjects (control and cases) was evaluated using binary logistic regression models. This analysis was made using all cytokines (EGF, IFN-γ, IL-1β, IL-1α, IL-2, IL-4, IL-6, IL-8, IL-10, MCP-1, TNFα, and VEGF,) and all variables which were expected to have a significantly relationship with CAD, based on demographic data, lifestyle behavior, traditional risk factors, novel biomarkers, physical measurements, psychological factors, and family history.
The results showed that the effects of the independent variables on the odds of having a positive angiogram for males was approximately four times more likely compared to females (OR 4.46, CI95% 2.71–9.17, P < 0.05). The odds of a positive angiogram for patients with a positive paternal diabetic history, positive CVD history in a male sibling were at an increased risk [OR 15.928 (CI95% 1.52–166.91) and OR 4.059 (CI95% 1.35–12.12), respectively, Table 3]. Moreover, we observed that FBG, serum concentrations of IL-4, IL-8, IL-10, and several dietary factors (fiber, trans-fat, polyunsaturated fat, sodium, potassium, iron, vitamins E, and vitamin C) were significantly associated with a significantly increased, or reduced risk of CAD (Table 4). In particular, for a one-unit increase, the expected change in log odds of angiography positivity were 0.010, −0.900, 0.066, −0.711, −0.122, 0.971, 0.165, −0.001, 0.000, 0.121, −0.282, and 0.006 for the FBG, IL-4, IL-8, IL-10, dietary intake of fiber, dietary intake of trans fat, dietary intake of polyunsaturated fat, dietary intake of sodium, dietary intake of potassium, dietary intake of iron, dietary intake of vitamin E, and dietary intake of vitamin C, respectively (Table 3). The logistic regression equation shown below was designed to predict the logit of CAD with angiography positivity:
Logit P = 1.496 Gender (Male) + 2.768 Father Diabetic History (Yes) + 1.401 Brothers CVD History (Yes) + 0.010 FBG − 0.900 IL-4 + 0.066 IL-8–0.711 IL-10–0.122 Dietary Intake of Fiber + 0.971 Dietary Intake of Trans Fat + 0.165 Dietary Intake of Polyu Fat − 0.001 Dietary Intake of Sodium + 0.000 Dietary Intake of Potassium + 0.121 Dietary Intake of Iron − 0.282 Dietary Intake of vitamin E + 0.006 Dietary Intake of vitamin C.
In addition, the probability of angiography positive could be obtained using following formula: logit = ln (p/(1−p)).
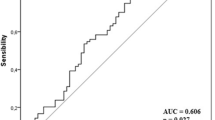
Furthermore, in order to evaluate the predictive performance of the cytokine/ growth factor profile for detecting angiogram positivity, the area under the ROC curve was calculated. We found that MCP-1 using a cut-off value of 61.95 pg/mL had a 91.20% sensitivity and 90.83% specificity, for the identification of subjects who were angiogram positive. The corresponding values for other markers were lower than this (Table 4; Fig. 1a).
a ROC Curve for serum MCP-1, IL-4, and IL-6 concentrations for differentiating angiography-positive subjects from healthy individuals; b Kaplan–Meijer survival curve of angiography-positive and -negative subjects with MCP-1 > 61.95 pg/mL; c ROC Curve for IL-6 and TNF-α/IL-10 ratio for mortality prediction in the subjects who have MCP-1 > 61.95 pg/mL
A Kaplan–Meier survival analysis was used for the evaluation of markers using data from two years of follow-up of the patients undergoing angiography. In the angiogram-positive subjects who had a serum MCP-1 > 61.95 pg/mL, there was approximately 90% survival up to 792 days, and for angiogram-negative individuals, 85% survival was up to 797 days (P < 0.05) (Fig. 1b).
As shown in Table 5, a serum MCP-1 > 61.95 pg/mL, and IL-6 > 2.16 pg/mL had a negative predictive value for mortality. The above cut-off value for IL-6 had a 94.1% sensitivity and 70.5% specificity for the prediction of mortality (Table 5; Fig. 1c).
Discussion
To the best of our knowledge, this is the first study evaluating the association between 12 cytokines and growth factors in individuals undergoing angiography in whom dietary intake and subsequent mortality were assessed. Subjects with a serum MCP-1 of > 61.95 pg/mL and serum IL-6 > 2.16 pg/mL could predict mortality with 94.1% sensitivity and 70.5% specificity, suggesting its value as a biomarkers for predicting mortality in subjects with pre-existing CAD.
Inflammation appears to be an important determinant of clinical implication in patients with CAD [15, 16]. Cytokines play a major role in the activation of adhesion molecule and chemokine expression involved in lymphocyte/monocyte recruitment, endothelial adhesion, and migration into the inflamed vessel wall [1]. Several studies have reported that TNF-α, IL-2, and IL-10 are potential markers for the prediction of cardiovascular events. Moreover, CRP and IL-6 have been identified as independent risk factors for myocardial infarction [3].IL-6 and IL-1 receptor antagonist are also increased in subjects with CAD [3, 15]. In the early phase of atherosclerosis, cytokines can alter endothelial permeability, promoting sub-endothelial lipid accumulation and favoring leukocyte diapedesis. A number of pro-inflammatory cytokines, including TNF-α and IFN-γ, have been shown to modulate the distribution of adhesion receptors involved in cell–cell adhesion and prevent the formation of F-actin stress fibers [17]. Consistent with these observations [18–20], we found a significant difference in serum concentrations of some cytokines between angiogram-positive patients and healthy subjects. In particular, we report higher levels of IL-1α and IL-6 in CAD positive versus CAD negative subjects.
A recent study has suggested a pro-atherosclerotic role for VEGF [21], and high serum of VEGF concentrations in coronary artery disease patients [22]. However, several other studies have reported that serum VEGF concentrations do not correlate with the presence, severity, or extent of CAD [23]. Thus, in the present study we have explored the role of IL-10 in CAD and have found significant differences in serum VEGF concentrations between our groups.
IL-10 is an anti-inflammatory cytokine, which is released by lymphocytes of the Th2 subtype and macrophages; it possesses strong anti-inflammatory properties on cell subpopulations linked with atherogenesis [2]. IL-10 inhibits the expression of tissue factor by macrophages, and may therefore have a role in thrombosis and plaque stability. We found lower concentrations of IL-10 in the angiogram-positive group; however, this difference did not reach statistical significance.
Some investigators have reported that serum IL-2 may be a potential marker for the prediction of cardiovascular events [3, 9, 15]; however, we did not find a significant relationship in our population.
There is growing body of data showing an association between MCP-1 and the presence of Metabolic Syndrome [13] and CAD [9]. In individuals with unstable coronary syndromes, serum MCP-1 is reported to be associated with an enhanced risk of MI or death within 10 months [9]. The current study is consistent with this. We found that serum MCP-1 > 61.95 pg/mL had 91.20% sensitivity and 90.83% specificity for identifying individuals with a positive angiogram. In subjects who had a serum MCP-1 > 61.95 pg/mL, we found that a serum IL-6 could add to the prediction of mortality. A serum IL-6 > 2.16 pg/mL predicted mortality with 94.1% sensitivity and 70.5% specificity. MCP-1 and IL-6 may therefore be particularly useful biomarkers for predicting mortality in subjects with pre-existing CAD. In agreement with our data, De Lemos et al., found that MCP-1 was associated with traditional risk factors for atherosclerosis [24]. In particular, they showed that patients in the fourth quartile of MCP-1 levels had lower survival rate (HR 1.43; 95% CI 0.89–2.31; P = 0.13), and were likely to suffer from death or MI (HR 1.69; 95% CI 1.24–2.31; P = 0.001). Moreover this association was remained statistically significant after adjustment for age; history of diabetes, hypertension, hypercholesterolemia, or coronary disease; creatinine clearance; ST deviation; and cTnI (HR 1.42; 95% CI 1.02–1.98; P = 0.04). In aggregate, these data revealed that patients with acute coronary syndromes, a level of MCP-1 above the 75th percentile was related with traditional risk factors for atherosclerosis as well as an increased risk for death or MI (24). Furthermore, Hoogeveen and colleagues reported that serum MCP-1 concentrations were associated with a significantly increased risk of atherosclerosis [25]. In particular, they investigated the association of plasma MCP-1 to atherosclerosis in a large prospective, population-based, biracial Atherosclerosis Risk in Communities (ARIC) study. These data indicated that the risk of peripheral arterial disease enhanced progressively across tertiles of MCP-1 level after adjusting for BMI, hypertension, diabetes mellitus, total cholesterol, HDL cholesterol, and smoking (OR 2.14; 95% CI 1.28–3.60). This association remained also significant for MCP-1 when its association was adjusted for other inflammatory markers such as white blood cell count, fibrinogen, and vWF (OR 1.82; 95% CI 1.07–3.10). Thus, our hypothesis is that the increased level of MCP-1 is presented its increased production by vascular endothelium and other cells in atherosclerotic lesions. This increase mediate the recruitment of monocytes into vessel wall, and thereby promote the progression of atherosclerosis and plaque instability.
Furthermore, we found that EGF, IL-4, IL6, IL-8, and VEGF concentrations had 80% sensitivity for case finding, supporting further investigation to evaluate their values in the screening for CAD. Goswami et al. have reported a significantly higher serum TNF-α/IL-10 ratio in patients with acute MI [10]. We found similar results for the angiography-positive subjects versus control group, and the TNF-α/IL-10 ratio was predicted mortality with more than 80% sensitivity when 2.02 pg/mL was used as a cut off. Other studies have shown that these pro/anti-inflammatory cytokine ratios may be a potential option in the assessment of CAD [26]. Angiography is a gold standard method for identification of athermanous plaque that impinges on the arterial lumen [27], but angiography is an invasive tool and does not always predict clinical events [28]. This is thought to be related to the fact that unstable plaques may exist within the artery wall, and remodeling of the artery wall may preserve luminal diameter. Therefore non-invasive diagnostic biomarkers are also warranted.
A major strength of the current study was that a large number of cytokines were measured in a well-characterized cohort of individuals and evaluated their prognostic value with respect to the outcome and mortality. Conversely, the main limitation of this study was the use of the 50% cut-off threshold in defining a positive angiogram. Angio(−) subjects may progress to being angiogram positive over time. The procedure that was used only provided the information about internal lumen diameter of coronary artery, and does not provide any information about plaque inflammation, instability, or degree of intramural involvement. Thus, further studies are needed to consider these parameters, compared to the value of emerging cytokines. Moreover we cannot exclude the impact of treatment with anti-inflammatory agents on clinical outcomes and cytokine profiles, which also needs to be evaluated. Additionally, it is possible that other lifestyle characteristics other than diet have an influence on the outcome. The mean age was different between groups, although we attempted to adjust for this variable in the logistic regression model.
In conclusion, patients with angiographically defined coronary artery disease had an altered cytokine profile. Among the studied cytokines, serum MCP-1 and IL-6 were found to have a high sensitivity and specificity for predicting angiogram positivity and mortality in CAD patients. Further studies are warranted to investigate the value of emerging markers for predicting of presence of CAD.
References
Zernecke A, Shagdarsuren E, Weber C (2008) Chemokines in atherosclerosis: an update. Arterioscler Thromb Vasc Biol 28:1897–1908
Martins TB, Anderson JL, Muhlestein JB, Horne BD, Carlquist JF, Roberts WL (2006) Risk factor analysis of plasma cytokines in patients with coronary artery disease by a multiplexed fluorescent immunoassay. Am J Clin Pathol 125:906–913
Martins TB, Anderson JL, Muhlestein JB, Horne BD, Carlquist JF, Roberts WL et al (2006) Risk factor analysis of plasma cytokines in patients with coronary artery disease by a multiplexed fluorescent immunoassay. Am J of clin path 125:906–913
Tousoulis D, Antoniades C, Koumallos N, Stefanadis C (2006) Pro-inflammatory cytokines in acute coronary syndromes: from bench to bedside. Cytokine Growth Factor Rev 17:225–233
Kallio P, Kolehmainen M, Laaksonen DE, Pulkkinen L, Atalay M, Mykkänen H, Uusitupa M, Poutanen K, Niskanen L (2008) Inflammation markers are modulated by responses to diets differing in postprandial insulin responses in individuals with the metabolic syndrome. Am J Clin Nutr 87:1497–1503
Tajfard M, Ghayour Mobarhan M, Rahimi HR, Mouhebati M, Esmaeily H, Ferns GA et al (2014) Anxiety, depression, coronary artery disease and diabetes mellitus; an association study in ghaem hospital, iran. Iran Red Crescent Med J 16:e14589
Hansson GK (2005) Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 352:1685–1695
Zenti MG, Stefanutti C (2011) Effects of selective H.E.L.P. LDL-apheresis on plasma inflammatory markers concentration in severe dyslipidemia: Implication for anti-inflammatory response. Cytokine 56:850–854
Zakynthinos E, Pappa N (2009) Inflammatory biomarkers in coronary artery disease. J Cardiol 53:317–333
Goswami B, Rajappa M, Mallika V, Shukla DK, Kumar S (2009) TNF-alpha/IL-10 ratio and C-reactive protein as markers of the inflammatory response in CAD-prone North Indian patients with acute myocardial infarction. Clin Chim Acta 408:14–18
Mirhafez S, Zarifian A, Ebrahimi M, Ali R, Avan A, Tajfard M, et al (2015) Relationship between serum cytokine and growth factor concentrations and coronary artery disease. Clin Biochem 48:575–580
Zomorrodian D, Khajavi-Rad A, Avan A, Ebrahimi M, Nematy M, Azarpazhooh MR et al (2015) Metabolic syndrome components as markers to prognosticate the risk of developing chronic kidney disease: evidence-based study with 6492 individuals. J Epidemiol Community Health 69:594–598
Mirhafez SR, Pasdar A, Avan A, Esmaily H, Moezzi A, Mohebati M et al (2015) Cytokine and growth factor profiling in patients with the metabolic syndrome. Br J Nutr 113:1911–1919
Mirhafez SR, Mohebati M, Feiz Disfani M, Saberi Karimian M, Ebrahimi M, Avan A et al (2014) An imbalance in serum concentrations of inflammatory and anti-inflammatory cytokines in hypertension. J Am Soc Hypertens 8:614–623
Libby P, Ridker PM, Maseri A (2002) Inflammation and atherosclerosis. Circulation 105:1135–1143
Tajfard M, Latiff LA, Rahimi HR, Mouhebati M, Esmaeily H, Taghipour A, et al (2014) Serum inflammatory cytokines and depression in coronary artery disease. Iran Red Crescent Med J 16:e17111
Wojciak-Stothard B, Entwistle A, Garg R, Ridley AJ (1998) Regulation of TNF-alpha-induced reorganization of the actin cytoskeleton and cell-cell junctions by Rho, Rac, and Cdc42 in human endothelial cells. J Cell Physiol 176:150–165
Schieffer B, Selle T, Hilfiker A, Hilfiker-Kleiner D, Grote K, Tietge UJ et al (2004) Impact of interleukin-6 on plaque development and morphology in experimental atherosclerosis. Circulation 110:3493–3500
Elhage R, Clamens S, Besnard S, Mallat Z, Tedgui A, Arnal J et al (2001) Involvement of interleukin-6 in atherosclerosis but not in the prevention of fatty streak formation by 17beta-estradiol in apolipoprotein E-deficient mice. Atherosclerosis 156:315–320
Merhi-Soussi F, Kwak BR, Magne D, Chadjichristos C, Berti M, Pelli G et al (2005) Interleukin-1 plays a major role in vascular inflammation and atherosclerosis in male apolipoprotein E-knockout mice. Cardiovasc Res 66:583–593
Celletti FL, Waugh JM, Amabile PG, Brendolan A, Hilfiker PR, Dake MD (2001) Vascular endothelial growth factor enhances atherosclerotic plaque progression. Nat Med 7:425–429
Blann AD, Belgore FM, McCollum CN, Silverman S, Lip PL, Lip GY (2002) Vascular endothelial growth factor and its receptor, Flt-1, in the plasma of patients with coronary or peripheral atherosclerosis, or Type II diabetes. Clin Sci 102:187–194
Alber HF, Frick M, Dulak J, Dorler J, Zwick RH, Dichtl W et al (2005) Vascular endothelial growth factor (VEGF) plasma concentrations in coronary artery disease. Heart 91:365–366
de Lemos JA, Morrow DA, Sabatine MS, Murphy SA, Gibson CM, Antman EM et al (2003) Association between plasma levels of monocyte chemoattractant protein-1 and long-term clinical outcomes in patients with acute coronary syndromes. Circulation 107:690–695
Hoogeveen RC, Morrison A, Boerwinkle E, Miles JS, Rhodes CE, Sharrett AR et al (2005) Plasma MCP-1 level and risk for peripheral arterial disease and incident coronary heart disease: atherosclerosis Risk in Communities study. Atherosclerosi 183: 301–307
Khan DA, Ansari WM, Khan FA (2011) Pro/anti-inflammatory cytokines in the pathogenesis of premature coronary artery disease. J Interferon Cytokine Res 31:561–567
Schuijf JD, Pundziute G, Jukema JW, Lamb HJ, van der Hoeven BL, de Roos A et al (2006) Diagnostic accuracy of 64-slice multislice computed tomography in the noninvasive evaluation of significant coronary artery disease. Am J Cardiol 98:145–148
Biancari F, Lahtinen J, Salmela E, Niemela M, Pokela R, Rainio P et al (2003) Does angiographic severity of coronary artery disease predict postoperative outcome after coronary artery bypass surgery? Scand Cardiovasc J 37:275–282
Acknowledgements
The Mashhad University of Medical Science Research Council supported this research (Fund Number MUMS/900671). This study is the subject thesis of Mr. Mohammad Tajfard, which is the PhD Candidate of the community health in University Putra Malaysia. Authors would like to thank Center for International Scientific Studies and Collaboration for their support.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Tajfard, M., Latiff, L.A., Rahimi, H.R. et al. Serum concentrations of MCP-1 and IL-6 in combination predict the presence of coronary artery disease and mortality in subjects undergoing coronary angiography. Mol Cell Biochem 435, 37–45 (2017). https://doi.org/10.1007/s11010-017-3054-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-3054-5