Abstract
Somatostatin (SST) is one of the main regulators of thyroid function. It acts by binding to its receptors, which lead to the dissociation of G proteins into Gαi and Gβγ subunits. However, much less is known about the function of Gβγ in thyroid cells. Here, we studied the role of SST and Gβγ dimers released upon SST stimulation on the Ras-ERK1/2 pathway in FTRL-5 thyroid cells. We demonstrate that SST activates Ras through Gi proteins, since SST-induced Ras activation is inhibited by pertussis toxin. Moreover, the specific sequestration of Gβγ dimers decreases Ras-GTP and phosphorylated ERK1/2 levels, and overexpression of Gβγ increases ERK1/2 phosphorylation induced by SST, indicating that Gβγ dimers released after SST treatment mediate activation of Ras and ERK1/2. On the other hand, SST treatment does not modify the expression of the thyroid differentiation marker sodium/iodide symporter (NIS) through ERK1/2 activation. However, SST increases AKT activation and the inhibition of the Src/PI3K/AKT pathway increases NIS levels in SST-treated cells. Thus, we conclude that, in thyroid cells, signalling from SST receptors to ERK1/2 involves a Gβγ-mediated signal acting on a Ras-dependent pathway. Moreover, we demonstrate that SST might regulates NIS expression through a Src/PI3K/AKT-dependent mechanism, but not through ERK1/2 signalling, showing the main role of this hormone in thyroid function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proliferation of follicular thyroid cells is mainly regulated by the positive actions of thyrotrophin (TSH) and insulin-like growth factor I, and the antimitogenic signals induced by somatostatin (SST) [1]. Moreover, thyroid differentiation is also mainly induced by TSH through the expression of the different genes required for thyroid hormone synthesis such as the sodium/iodide symporter (NIS), thyroglobulin and thyroperoxidase. The NIS protein mediates iodide uptake by the thyroid follicular cell, which constitutes the first step in thyroid hormone biosynthesis [2]. However, less is known about the signals affecting thyroid cell function regulated by SST.
SST is a widely distributed peptide that inhibits hormone secretion, neurotransmission and cell proliferation. Its actions are mediated by specific G protein-coupled receptors (GPCRs) SSTR1-SSTR5 [3], which are coupled functionally to trimeric Gi proteins. The binding of this hormone to its receptor leads to the dissociation of Gi proteins into Gαi and Gβγ subunits. Most SST actions are mediated by Gαi and inhibition of the adenylyl cyclase/cAMP cascade, which is required for thyroid cell differentiation and proliferation [1, 2].
Although the main functions of G proteins were thought to be mediated by the Gα subunits, Gβγ complexes also regulate more than 20 effectors including phospholipases, adenylyl cyclases, ion channels, β-adrenergic receptor kinase (βARK) and PI3Ks [5]. Thus, Gβγ dimers regulate intracellular signals involved in proliferation and differentiation in different cell types by mechanisms involving the activation of the Ras/ERK and the PI3K/AKT pathways [6–15].
TSH activates the Ras/RAF/MEK/ERK signalling pathway after increase cAMP production by both PKA-dependent [16] and independent mechanisms [17]. SST also regulates the ERK1/2 pathway, but its modulation differs according to the receptor subtypes and the cellular models. Thus, whereas in some cell SST inhibits ERK1/2 phosphorylation, in others mediates a sustained activation of ERK1/2 [18–20]. Nonetheless, in thyroid cells, the role of SST on ERK1/2 activation and the functions of Gβγ subunits in the transmission of its intracellular signals remain essentially unknown.
It has been demonstrated that Gβγ released after TSH receptor activation affect thyroid differentiation via a PI3K-dependent pathway [21]. This, together with the fact that not all the actions of SST can be explained by a cAMP decrease, led us to study the involvement of Gβγ dimers in SST-dependent signalling and the regulation of the Ras/RAF/MEK/ERK pathway. We found that SST activates Ras and ERK through a Gβγ-initiated pathway in thyroid cells. Moreover, SST also activates the Src/PI3K/AKT pathway, which may interfere with NIS protein expression.
Materials and methods
Materials
TSH, SST and pertussis toxin (PTX) were from Sigma. The inhibitors used were U0126 (Promega), and LY294002 and PP1 (Calbiochem). Antibodies used were anti-phospho ERK1/2, anti-FLAG and anti-tubulin (Sigma); anti-Gαt and anti-CD8, anti-ERK2 (Santa Cruz Biotechnology); anti-Ras (BD-Biosciences); anti-phospho AKT on S473 and anti-AKT (Cellular Signalling). Anti-NIS antibody was a generous gift from Dr. N. Carrasco (Albert Einstein College of Medicine, Bronx, NY). The pcDNA3.1-FLAG-Gβ1 and pcDNA3.1-HA-Gγ2 plasmids were obtained from the Guthrie cDNA Resource Centre (Sayre, PA). pCisGαt expression vector for the α-subunit of bovine transducin and pcDNA-CD8-βARK, an expression vector bearing the extracellular and transmembrane domain of CD8 lymphocyte-specific receptor and the C-terminus of βARK1 were kindly provided by Dr. F. Mayor Jr. (CNB CSIC-UAM, Madrid, Spain). The luciferase reporter plasmid containing the full-length NIS promoter (pNIS-2.8) was kindly donated by Dr. P. Santisteban (IIB CSIC-UAM, Madrid, Spain).
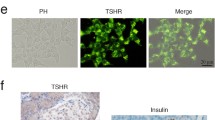
Cell culture
FRTL-5 thyroid cells were cultured in Coon’s modified Ham’s F-12 medium (Gibco) supplemented with 5 % donor calf serum and six-hormone mixture (6H, complete medium), including 10 ng/ml glycyl-l-histidyl-l-lysine, 5 μg/ml transferrin, 10 nM hydrocortisone, 10 ng/ml SST, 10 μg/ml insulin and 1 nM TSH. Before treatments, cell cultures were maintained for 3 days in medium depleted of TSH, insulin and SST in the presence of 0.2 % BSA (starvation medium), and then treated as indicated in the figures.
Transfections
FRTL-5 cells were plated 48 h before and transfection was performed by calcium phosphate coprecipitation as described previously [1, 4]. After 24 h, culture medium was changed to starvation medium; cells were maintained in this medium for 48 h and then treated as described in figure legends.
The NIS reporter assays were performed as previously described [22]. Cells were transfected with pNIS-2.8-Luc reporter plasmid and the internal transfection standard Renilla in pRL-TK, used to monitor transfection efficiency. After transfection, cells were maintained 48 h in starvation medium and then treated for additional 24 h. Cells were harvested in 100 μl reporter lysis buffer (Promega) and dual luciferase and Renilla reporter assays were performed following the protocol provided by the manufacturer.
Activated Ras affinity precipitation assay
The assay was performed essentially as described [23]. Cell extracts were lysed in extraction buffer, lysates were centrifuged and the supernatants assayed for protein concentration by the Bradford method. Supernatants were incubated with mixing with GST-RBD (Ras Binding Domain of CRAF), previously bound to glutathione-Sepharose beads. After washing, beads were boiled with SDS-PAGE sample buffer. Eluted proteins were resolved in 12 % SDS-PAGE and analyzed by Western blot with anti-Ras antibody.
Protein extraction and Western blot analysis
Cells were collected and homogenized in a buffer containing 50 mM HEPES (pH 7.4), 2 mM MgCl2, 250 mM NaCl, 0.1 mM EDTA, 0.1 mM EGTA, 0.1 % NP40, 1 mM dithiothreitol, 2 mM Na3VO4, 10 mM NaF and protease inhibitors. Cell extracts were normalized for protein content, and then analyzed by standard techniques using the indicated antibodies.
Statistical analysis
In statistical analysis, the student´s t test was performed using the SSCStat software (V2.18, University of Reading, United Kingdom).
Results
SST increases Ras activity
In order to study the role of SST and Gβγ on the Ras/RAF/MEK/ERK cascade in thyroid cells, we first examined Ras activation in FRTL-5 cells stimulated with SST, or TSH as control, at different times. We observed that SST increased the proportion of activated Ras-GTP by approximately threefold over control cell levels in a time-dependent manner, and that this increase was similar to that observed after TSH stimulation (Fig. 1a). To confirm these data, we treated the cells with increasing SST concentrations and observed that Ras activation increased in a dose-dependent manner (Fig. 1b). These data indicate that SST and TSH activate Ras by a cAMP-independent pathway, since both hormones exert opposite effect on the production of this second messenger.
SST and TSH activate Ras. FRTL-5 cells were treated with TSH (10 nM) or SST (10 μM) for the indicated times (a), or with increasing concentrations of SST for 15 min (b). Ras activation was measured as described in “Materials and methods” section (upper panels). 5 % of each lysate was loaded onto another gel to analyze total Ras protein levels (lower panels). Data shown are the mean±SEM of three independent experiments performed with similar results and blots are for one representative experiment. **0.001 < p < 0.01, ***p < 0.001, significant differences compared to the corresponding control
SST stimulates Gi-dependent Ras activation via a Gβγ subunit-initiated pathway
To analyze whether Ras activation by SST was Gi-dependent, we performed experiments using PTX, which inhibits Gi signalling. Treatment with PTX completely abolished SST-induced Ras activation, showing that a Gi-dependent pathway is the main route used by SST to activate Ras in FRTL-5 cells (Fig. 2a).
TSH and SST activate Ras through a Gβγ-dependent pathway. a Cells were left untreated or preincubated with PTX (150 ng/ml, 16 h) and then stimulated with SST (10 μM, 15 min). Cells were transfected with control vector, CD8-βARK (b and e) or pCisGαt (c, d and e). After transfection, cells were maintained for 48 h in starvation medium and left untreated or treated for 15 min with SST (10 μM) (b and c), TSH (10 nM) (d) or insulin (100 nM) (e). Cells were then harvested and active GTP-bound Ras was extracted from lysates and measured. CD8-βARK and Gαt expressions were detected by immunoblot with anti-CD8 or anti-Gαt antibodies, respectively. Blots shown are from one representative experiment performed three times with similar results
Upon SST binding to its receptors, Gi proteins dissociate into the inhibitory Gαi subunit and Gβγ subunits. To study the function of Gβγ dimers released after SST treatment, we inhibited Gβγ signalling by using two different Gβγ scavengers, CD8-βARK and Gαt [24, 25]. Thus, expression of CD8-βARK produced a decrease of SST-induced Ras activity (Fig. 2b). The same results were obtained in cells transfected with Gαt and treated with SST (Fig. 2c). To confirm the role of Gβγ on Ras activation, we performed a similar experiment after TSH treatment, observing that Gαt overexpression also inhibited Ras activation by this hormone (Fig. 2d). However, as negative control, in insulin-treated cells Gβγ inhibition did not produce any significant change of Ras activation (Fig. 2e), showing the specificity of this approach. Together, these results show that SST activates Ras through the Gβγ subunits released from Gi rather than through the Gαi subunits.
SST stimulates ERK1/2 through Gβγ subunits
Next, we studied whether SST could also increase ERK1/2 phosphorylation through activation of Gβγ. Figure 3a shows that SST significantly increased ERK1/2 phosphorylation in a time-dependent manner. This effect is exerted upstream of MEK, since cell treatment with the MEK inhibitor U0126 completely blocked SST-induced ERK1/2 phosphorylation (Fig. 3a). To study whether Gβγ dimers are directly responsible for ERK1/2 phosphorylation, we first used cells transiently cotransfected with expression vectors for Gβ1 and Gγ2 subunits. The results showed that overexpression of Gβγ dimers significantly increased ERK1/2 phosphorylation in both basal and SST-stimulated cells (Fig. 3b). We also explored the effect of Gβγ sequestration on ERK1/2 activity after SST treatment. Activation of ERK1/2 by SST was significantly reduced in cells transfected with CD8-βARK or Gαt compared to control cells (Fig. 3c). Since TSH also activates Ras by a Gβγ-dependent mechanism, we investigated the ERK1/2 activation by this hormone and whether Gβγ dimers could also be involved in the TSH-stimulated ERK1/2 activation. As expected, TSH increased ERK1/2 activation and this effect was blocked by the inhibitor U0126 (Fig. 3d). Moreover, in cells transiently transfected with βARK or Gαt, TSH-stimulated ERK1/2 activation was reduced compared with control cells (Fig. 3e). These data suggest that Gβγ subunits are key molecules in SST activation of the Ras-ERK1/2 cascade in thyroid cells.
Gβγ activates ERK1/2. a Cells were pretreated for 30 min with DMSO, as control, or U0126 (10 μM) and then left untreated or treated with SST (10 μM) for the indicated times. b Cells were transfected with control vector or the FLAG-Gβ1 and HA-Gγ2 plasmids. After transfection, cells were maintained in starvation medium for 48 h, and then left untreated, treated with SST (10 μΜ) or incubated in complete medium (6H) for 30 min. c Cells were transfected with control vector, CD8-βARK, pCisGαt, or FLAG-Gβ1 and HA-Gγ2. After 48 h, cells were treated with SST (10 μΜ) for 30 min. d Cells were treated with TSH (10 nΜ) for the indicated times (left panels), or pretreated with DMSO or U0126 (10 μM) for 30 min and then stimulated with TSH 30 min (right panels). e Cells transfected as in B were left untreated or treated with TSH (10 nΜ) for 30 min. Phosphorylated ERK1/2 (pERK) was detected using the appropriate phospho-specific antibody. Blots were reprobed with anti-ERK2 antibody as loading control. When indicated, FLAG-epitope-tagged Gβ1 protein was detected with anti-FLAG antibody. Blots are for one representative experiment from three performed with similar results
SST activates the PI3K/AKT pathway and regulates NIS expression
NIS is one of the main differentiation markers of thyroid cells, whose expression is regulated by TSH through Gαs/cAMP- and Gβγ-dependent pathways. Then, we analyzed the expression of the NIS gene to determine whether SST, which exerts the same effect as TSH on the Ras-ERK1/2 pathway through Gβγ, could modify differentiation in FRTL-5 cells. As predicted, TSH increased NIS protein levels compared to control cells; however, SST had no significant effect (Fig. 4a). We also studied whether SST could regulate transcription of the NIS gene transfecting a luciferase reporter plasmid containing the full-length NIS promoter. As previously described, TSH significantly increased NIS promoter activity [21, 22], whereas SST treatment did not have any effect (Fig. 4b). To explore the lack of effect of SST on NIS expression, we initially examined the role of the Ras/RAF/MEK/ERK pathway by testing the effects of the MEK inhibitor U0126 in SST-treated cells. Inhibition of MEK/ERK signalling did not significantly increase NIS protein expression either in basal conditions or after SST stimulation (data not shown). This indicates that the activation of the Ras and ERK1/2 by SST is independent of NIS expression in these cells.
SST activates the PI3K/AKT pathway and regulates NIS expression. a Cells were starved for 7 days, then left untreated or stimulated with TSH (10 nM), SST (10 μM) or complete media (6H) for 24 h and NIS protein levels were detected using the specific antibody. Blots were reprobed with anti-tubulin antibody as loading control. b Cells were transfected with pNIS-2.8 Luc and pRL-TK-Renilla reporter plasmids. 48 h after transfection, cells were treated with TSH, SST or 6H for 24 h. Cell extracts were assayed for luciferase and Renilla activities. Luciferase activity was normalized with Renilla activity and expressed as fold increase from control. Data shown represent the mean±SEM of four independent experiments performed in duplicate. c, d Cells were pretreated with the inhibitors LY294002 (20 μM) (c) or PP1 (10 μM) (d) 30 min before addition of SST (10 nM) for the indicated times. Cells were then harvested and phosphorylation of AKT (pAKT) was detected using the appropriate phospho-specific antibody. For each pair of rows, an image of the phospho-specific blot is shown with the reprobed image with anti-AKT antibody. e Cells were starved 7 days, then pretreated with the inhibitors LY294002 (20 μM) or PP1 (10 μM) 30 min before addition SST (10 μM) for 24 h. Cells were then harvested for Western Blot analysis and NIS expression was detected with anti-NIS antibody. Blots are from representative experiments of three performed with similar results. ***p < 0.001, significant differences compared to the corresponding control
Since different studies suggest that PI3K regulates NIS gene transcription [21, 22], we also studied the role of the PI3K/AKT signalling pathway on NIS expression after SST treatment. First, to determine whether SST activates PI3K, we examined phosphorylation of endogenous AKT protein. AKT was not phosphorylated in resting cells, but its phosphorylation was stimulated within 10 min of treatment with SST and continued to rise over a 60-min period (Fig. 4c). Accordingly, SST-induced AKT phosphorylation was completely blocked in cells pretreated with the PI3K inhibitor LY294002 (Fig. 4c). Src acts as an early intermediate of PI3K activation in response to GPCRs [13]; then, we also used the Src inhibitor PP1 to characterize the involvement of this kinase in PI3K/AKT activation by SST. Exposure of cells to PP1 abrogated SST-induced AKT activation (Fig. 4d). These results indicate that Src acts upstream of PI3K to activate AKT in response to SST.
To study whether SST-mediated PI3K activation was implicated in NIS expression, we treated the cells with PP1 or LY294002 inhibitors, followed by treatment with SST, and observed that the inhibition of both Src and PI3K significantly increased NIS protein levels in both basal conditions and SST-treated cells (Fig. 4e). Altogether, these data suggest that the activation of Src/PI3K/AKT pathway could be responsible for the lack of effect of SST on NIS expression.
Discussion
Here, we show for the first time that SST can activate Ras and ERK1/2 via a previously undescribed Gβγ-dependent pathway in thyroid cells. Moreover, SST may regulate NIS gene expression in thyroid cells by activation of the PI3K/AKT signalling pathway and independently of ERK1/2 activation.
In thyroid cells G protein activating signals to Ras and ERK1/2 more often involve activation of Gαs and generation of cAMP [16, 17]. However, here we show that in addition to the cAMP pathway, signals other than cAMP can activate Ras and ERK1/2 in FRTL-5 cells, since TSH and SST exert opposite effects on cAMP production [1, 4]. We demonstrate the involvement of Gi protein in SST-mediated Ras and ERK1/2 activation based on the sensitivity to PTX. In addition, we present evidence that Gβγ dimers released upon TSH and SST binding to their surface receptors are involved in Ras and ERK1/2 activation. Although the implication of Gβγ subunits in this signalling pathway was observed in other systems [6–10, 13–15], this is the first evidence in thyroid cells. Thus, our results are similar to those obtained in CHO cells stably transfected with SSTR1 [19] or SSTR2 [20]. The mechanisms underlying this effect are not fully known and a Gβγ molecular target upstream of Ras has not been rigorously defined to date. In this sense, it has been shown that Gβγ can activate Ras by different mechanisms involving PI3K, the adaptor proteins Shc, Grb2 or GRF-2, transactivation of tyrosine kinase receptors, the tyrosine phosphatase SHP-2 or Src [10–13, 26]. We have not studied the direct target of Gβγ dimers, thus, further studies are essential to clarify the signalling molecules linking Gβγ activated by SST and Ras in thyroid cells.
Although, we still do not know the biological processes affected by this new SST/Gβγ/Ras/ERK pathway in thyroid cells, it is possible that the previously reported SST anti-proliferative effect may be triggered by the previously identified SHP-1-SHP-2-PI3K/Ras-Rap1/BRAF/MEK/ERK/p27Kip pathway [11, 20], in which Gβγ dimers released after SSTR activation can be included at any step above Ras activation. On the other hand, our data indicate that SST may inhibit the expression of the thyroid differentiation marker NIS, through a Src/PI3K/AKT-dependent and ERK1/2-independent mechanism. In contrast to TSH, SST does not increase the levels of NIS, although both hormones activate ERK1/2, suggesting that additional pathways to Ras/ERK are involved in regulation of NIS expression by SST. The role of ERK1/2 in thyroid cell differentiation has been addressed by previous studies with opposite result. It has been described that ERK1/2 inhibition has no effect on TSH induction of NIS expression [22], but blunted the inhibitory effects of RET/PTC on expression of this symporter [27]. Moreover, although over-activation of ERK1/2 by oncogenic V600EBRAF silences thyroid-specific gene expression in papillary and anaplastic thyroid cancer [28], experiments with differentiated PCCl3 thyroid cells demonstrated that overexpression of V600EBRAF sharply impaired both NIS expression and targeting to membrane and, surprisingly, this impairment was not totally dependent on the MEK/ERK pathway [29].
Besides its role on proliferation and survival, the implication of the PI3K/AKT pathway on differentiation has not been fully characterized. The PI3K/AKT pathway, however, might be responsible for the lack of effect of SST on NIS expression. We observed that SST activates AKT and that inhibition of PI3K and Src decreases AKT phosphorylation and increases NIS levels. Our data are in agreement with the studies showing that AKT activation by isoproterenol requires Ras, Src and Gβγ [13]. Furthermore, our data concur with previous results showing that the PI3K/AKT pathway inhibits the expression of the thyroid differentiation marker NIS, as well as the activity of its activator Pax8, considered another thyroid marker [21, 22, 30]. The Gβγ subunits released after TSH stimulation activate PI3K to inhibit NIS gene expression, demonstrating a functional role for Gβγ dimers in thyroid cell differentiation [21]. This Gβγ function has also been shown in other cell models; for instance, Gβγ mediates agonist-induced differentiation of vascular smooth muscle cells [31], and differentiation of PC12 cells by Purkinje cell protein-2 (Pcp2) requires a Gβγ-mediated activation of Ras [32]. Thus, it is possible that SST, through activation of the Gβγ/PI3K/AKT pathway, impedes NIS expression, allowing us to speculate that a pathway specifically governed by Gβγ dimers release after SST stimulation might affect thyroid differentiation. The opposite results exerted by TSH and SST could be responsible to maintain a tight control of NIS protein levels, since iodide uptake is a crucial step for thyroid function. Nonetheless, the possible role of Gβγ subunits released upon SST activation on the thyroid cell differentiation process remains to be elucidated. Moreover, the great similarities in multiple aspects of thyroid physiology between humans and small rodents have facilitated the rapid translation of experimental findings to the clinical realm. However, we should note that using a rat model does not reflect the human situation and that the in vitro experiments should be taken into account if the experimental findings are to have clinical relevance. This, our findings warrant further investigation to address the mechanisms underlying ERK PI3K activation by SST and its role on differentiation in human cells.
References
Medina DL, Toro MJ, Santisteban P (2000) Somatostatin interferes with thyrotropin-induced G1-S transition mediated by cAMP-dependent protein kinase and phosphatidylinositol 3-kinase. Involvement of RhoA and cyclin E cyclin-dependent kinase 2 complexes. J Biol Chem 275:15549–15556
Riesco-Eizaguirre G, Santisteban P (2006) A perspective view of sodium iodide symporter research and its clinical implications. Eur J Endocrinol 155:495–512
Patel YC (1999) Somatostatin and its receptor family. Front Neuroendocrinol 20:157–198
Medina DL, Velasco JA, Santisteban P (1999) Somatostatin is expressed in FRTL-5 Thyroid cells and prevents thyrotropin-mediated down-regulation of the cyclin-dependent kinase inhibitor p27kip1. Endocrinology 140:87–95
Birnbaumer L (2007) Expansion of signal transduction by G proteins. The second 15 years or so: from 3 to 16 alpha subunits plus betagamma dimers. Biochim Biophys Acta 1768:772–793
Crespo P, Xu N, Simonds WF, Gutkind JS (1994) Ras-dependent activation of MAP kinase pathway mediated by G-protein βγ subunits. Nature 369:418–420
Faure M, Voyno-Yasenetskaya TA, Bourne HR (1994) cAMP and beta gamma subunits of heterotrimeric G proteins stimulate the mitogen-activated protein kinase pathway in COS-7 cells. J Biol Chem 269:7851–7854
Koch WJ, Hawes BE, Allen LF, Lefkowitz RJ (1994) Direct evidence that Gi-coupled receptor stimulation of mitogen-activateed protein kinase is mediated by G beta gamma activation of p21ras. Proc Natl Acad Sci USA 91:12706–12710
Hwang JI, Choi S, Fraser ID, Chang MS, Simon MI (2005) Silencing the expression of multiple Gbeta-subunits eliminates signaling mediated by all four families of G proteins. Proc Natl Acad Sci USA 102:9493–9498
Van Biesen T, Hawes BE, Luttrell DK, Krueger KM, Touhara K, Porfiri E et al (1995) Receptor-tyrosine-kinase- and G beta gamma-mediated MAP kinase activation by a common signalling pathway. Nature 376:781–784
Craddock BL, Hobbs J, Edmead CE, Welham MJ (2001) Phosphoinositide 3-kinase-dependent regulation of interleukin-3-induced proliferation: involvement of mitogen-activated protein kinases, SHP2 and Gab2. J Biol Chem 276:24274–24283
Ferjoux G, Lopez F, Esteve JP, Ferrand A, Vivier E, Vely F et al (2003) Critical role of Src and SHP-2 in sst2 somatostatin receptor-mediated activation of SHP-1 and inhibition of cell proliferation. Mol Biol Cell 14:3911–3928
Schmitt JM, Stork PJ (2002) Galpha and Gbeta gamma require distinct Src-dependent pathways to activate Rap1 and Ras. J Biol Chem 277:43024–43032
Jin M, Min C, Zheng M, Cho DI, Cheong SJ, Kurose H, Kim KM et al (2013) Multiple signaling routes involved in the regulation of adenylyl cyclase and extracellular regulated kinase by dopamine D(2) and D(3) receptors. Pharmacol Res 67:31–41
Vidal M, Wieland T, Lohse MJ, Lorenz K (2012) β-Adrenergic receptor stimulation causes cardiac hypertrophy via a Gβγ/Erk-dependent pathway. Cardiovasc Res 96:255–264
Ciullo I, Diez-Roux G, Di Domenico M, Migliaccio A, Avvedimento EV (2001) cAMP signaling selectively influences Ras effectors pathways. Oncogene 20:1186–1192
Iacovelli L, Capobianco L, Salvatore L, Sallese M, D′Ancona GM, de Blasi A (2001) Thyrotropin activates Mitogen-activated protein kinase pathway in FRTL-5 by a cAMP-dependent protein kinase A-independent mechanism. Mol Pharmacol 60:924–933
Cattaneo MG, Taylor JE, Culler MD, Nisoli E, Vicentini LM (2000) Selective stimulation of somatostatin receptor subtypes: differential effects on Ras/MAP kinase pathway and cell proliferation in human neuroblastoma cells. FEBS Lett 481:271–276
Florio T, Yao Y, Carey KD, Dillon TJ, Stork PJ (1999) Somatostatin activation of mitogen-activated protein kinase via somatostatin receptor 1 (SSTR1). Mol Endocrinol 13:24–37
Lahlou H, Saint-Laurent N, Esteve JP, Eychene A, Pradayrol L, Pyronnet S, Susini C (2003) sst2 Somatostatin receptor inhibits cell proliferation through Ras-, Rap1-, and B-Raf-dependent ERK2 activation. J Biol Chem 278:39356–39371
Zaballos MA, García B, Santisteban P (2008) Gbetagamma dimers released in response to thyrotropin activate phosphoinositide 3-kinase and regulate gene expression in thyroid cells. Mol Endocrinol 22:1183–1199
García B, Santisteban P (2002) PI3K is involved in the IGF-I inhibition of TSH-induced sodium/iodide symporter gene expression. Mol Endocrinol 16:342–352
de Rooij JL, Bos J (1997) Minimal Ras-binding domain of Raf1 can be used as an activation-specific probe for Ras. Oncogene 14:623–625
Crespo P, Cachero TG, Xu N, Gutkind JS (1995) Dual effect of beta-adrenergic receptors on mitogen-activated protein kinase. Evidence for a beta gamma-dependent activation and a G alpha s-cAMP-mediated inhibition. J Biol Chem 270:25259–25265
Avidor-Reiss T, Nevo I, Levy R, Pfeuffer T, Vogel Z (1996) Chronic opioid treatment induces adenylyl cyclase V superactivation. Involvement of Gbetagamma. J Biol Chem 271:21309–21315
Obara Y, Okano Y, Ono S, Yamauchi A, Hoshino T, Kurose H, Nakahata N (2008) Betagamma subunits of G(i/o) suppress EGF-induced ERK5 phosphorylation, whereas ERK1/2 phosphorylation is enhanced. Cell Signal 20:1275–1283
Knauf JA, Kuroda H, Basu S, Fagin JA (2003) RET/PTC-induced dedifferentiation of thyroid cells is mediated through Y1062 signaling through SHC-RAS-MAP kinase. Oncogene 22:4406–4412
Xing M (2007) BRAF mutation in papillary thyroid cancer: pathogenic role, molecular bases, and clinical implications. Endocr Rev 28:742–762
Riesco-Eizaguirre G, Gutiérrez-Martínez P, García-Cabezas MA, Nistal N, Santisteban P (2006) The oncogene BRAFV600E is associated with a high risk of recurrence and less differentiated papillary thyroid carcinoma due to the impairment of Na+/I- targeting to the membrane. Endocr Relat Cancer 13:257–269
Liu YY, Zhang X, Ringel MD, Jhiang SM (2012) Modulation of sodium iodide symporter expression and function by LY294002, Akti-1/2 and Rapamycin in thyroid cells. Endocr Relat Cancer 19:204–291
Reusch HP, Schaefer M, Plum C, Schultz G, Paul M (2001) Gbeta gamma mediate differentiation of vascular smooth muscle cells. J Biol Chem 276:19540–19547
Guan J, Luo Y, Denker BM (2005) Purkinje cell protein-2 (Pcp2) stimulates differentiation in PC12 cells by Gbetagamma-mediated activation of Ras and p38 MAPK. Biochem J 392:389–397
Acknowledgments
We are grateful to Dr F. Mayor Jr. for providing βARK and Gαt vectors. This work was supported by Dirección General de Investigación, MICINN, Grant SAF2010-19921.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rodríguez-Álvarez, F.J., Jiménez-Mora, E., Caballero, M. et al. Somatostatin activates Ras and ERK1/2 via a G protein βγ-subunit-initiated pathway in thyroid cells. Mol Cell Biochem 411, 253–260 (2016). https://doi.org/10.1007/s11010-015-2587-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-015-2587-8