Abstract
Upregulation of matrix metalloproteinases (MMPs) is a hallmark of osteoarthritis progression; along with the role reactive oxygen species (ROS) may play in this process. Moreover, mitochondrial DNA damage and dysfunction are also present in osteoarthritic chondrocytes. However, there are no studies published investigating the direct relationship between mitochondrial ROS, mitochondrial DNA damage, and MMP expression. Therefore, the purpose of the present study was to evaluate whether mitochondrial DNA damage and mitochondrial-originated oxidative stress modulates matrix destruction through the upregulation of MMP protein levels. MitoSox red was utilized to observe mitochondrial ROS production while a Quantitative Southern blot technique was conducted to analyze mitochondrial DNA damage. Additionally, Western blot analysis was used to determine MMP protein levels. The results of the present study show that menadione augmented mitochondrial-generated ROS and increased mitochondrial DNA damage. This increase in mitochondrial-generated ROS led to an increase in MMP levels. When a mitochondrial ROS scavenger was added, there was a subsequent reduction in MMP levels. These studies reveal that mitochondrial integrity is essential for maintaining the cartilage matrix by altering MMP levels. This provides new and important insights into the role of mitochondria in chondrocyte function and its potential importance in therapeutic approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
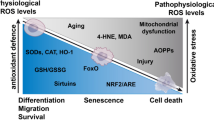
In a variety of tissues, oxidative stress disrupts mitochondrial respiration, and mitochondrial damage has been found to promote aging, cell death, and functional failure and degeneration. One common theme in osteoarthritis (OA) is oxidative stress and mitochondrial dysfunction [1]. Reactive oxygen species (ROS) have been shown to increase in OA [2]. Despite the progress made in recent years to evaluate the role of ROS and oxidative stress in OA progression, our understanding of the redox state of cartilage in pathologic circumstances remains incomplete. Additionally, because articular cartilage chondrocytes must survive and maintain tissue integrity in an avascular and hypoxic environment which requires adaptively increased anaerobic glycolysis to support adenosine triphosphate (ATP) synthesis, a mitochondrial-mediated pathogenesis for OA has not been studied extensively until the past two decades.
Evidence for the involvement of ROS in cartilage matrix degradation comes from animal models showing that ROS scavengers or ROS production inhibitors slowdown cartilage loss [3]. Other studies have not only shown oxidative damage in OA cartilage, but also that chondrocyte production of ROS is required for the enhanced production of cartilage-degrading enzymes, the matrix metalloproteinases (MMPs) [4–7]. Activator protein 1 (AP-1) and E26 transformation-specific (Ets) family transcription factors are important in regulating MMP family members and are sensitive to regulation by redox conditions [8]. Taken together, MMPs can degrade all components of the extracellular matrix [9]. These data provide evidence that oxidative stress plays a regulatory role in the expression of MMPs in cartilage.
The major sites of ROS generation include the mitochondria, non-mitochondrial membrane-bound NADPH oxidase, and xanthine oxidase [10]. Of these, the most likely source is mitochondria: it is estimated that 2–3 % of the total O2 consumed by functional mitochondrial electron transport chains is incompletely reduced to the superoxide anion, rather than to water [11, 12]. Historically, cartilage was thought to reside in hypoxic conditions, hence a role for mitochondria in the pathogenesis of OA was not considered. However, oxygen does diffuse into articular cartilage, and articular chondrocytes possess mitochondria and respire in vitro. Mitochondrial oxidative phosphorylation (OXPHOS) may account for up to 25 % of the ATP produced in cartilage [13]. Although detailed information about mitochondria in human cartilage and chondrocytes is lacking, a number of investigations support the idea that mitochondria may be involved in the degeneration of cartilage and development of OA [14, 15]. Therefore, a possible target that is hypothesized to play a major role in the progression of OA is the mitochondrion.
ROS-induced mitochondrial DNA (mtDNA) damage and mutations lead to the synthesis of functionally impaired respiratory chain subunits, causing further respiratory chain dysfunction and augmented ROS production. More evidence that mtDNA damage is present in OA arises from a study comparing age-matched normal and OA cartilage. In the data shown, there was significantly more mtDNA damage in OA cartilage than in normal cartilage, suggesting that mtDNA is damaged in the pathogenesis of OA [4]. This pathway of ROS-induced mtDNA damage and dysfunction might lead to the impairment of cartilage and joint function in OA. At present, these interactions are not well understood. Moreover, there are no studies published investigating the relationship between mitochondrial ROS, mtDNA damage and MMP expression in cartilage. Based on the above-mentioned findings, we hypothesized that mtDNA damage and mitochondrial-originated oxidative stress modulates matrix destruction in the setting of OA through the upregulation of MMP protein levels.
Methods
Chondrocyte primary culture and chemicals
The cartilage was obtained from neonatal Sprague Dawley rats (3–5 days). Primary chondrocyte cultures were generated by overnight digestion of minced cartilage samples with 5 mg/mL of collagenase B (Roche, Indianapolis, IN) in Dulbecco’s Modified Eagle Medium: Nutrient Mixture F-12 (DMEM/F12; Invitrogen, Carlsbad, CA) supplemented with 10 % fetal bovine serum (FBS; HyClone, Logan, UT) and antibiotics. Cells were plated and used for experiments after reaching confluence (3–5 days). In order to preserve chondrocyte phenotype, primary chondrocyte cultures were never passaged. After reaching confluence, primary chondrocytes were treated with various doses (10, 20 and 50 μM) of menadione (Supelco, Bellefonte, PA) for 1 h. Following menadione treatment, chondrocytes were either lysed immediately (0 h), after 1 h, or after 24 h. Initially, chondrocytes were treated with various doses (from 10 nM to 10 μM) of MitoTempo (Santa Cruz Biotechnology, Santa Cruz, CA) to determine an optimal concentration of 10 μM. The cultures then were treated with MitoTempo (10 μM) before, during, and after menadione (50 μM) treatment and were collected 24 h following menadione treatment.
Flow cytometry
MitoSOX Red mitochondrial superoxide indicator (Invitrogen, Eugene, OR) employs a novel fluorogenic dye for highly selective detection of superoxide in the mitohcondria of live cells [16]. To evaluate mitochondrial ROS production, at the designated time points following recovery from menadione treatment, chondrocytes were trypsinized and collected by centrifugation. To ensure that all cells were harvested, cell culture media from each dish were combined with the resulting cell suspension from the same dish following trypsinization. Cells were resuspended with MitoSOX (2 μM) and allowed to incubate at 37 °C for 10–15 min. Samples were analyzed by a BD FACSCanto™II flow cytometer (Becton–Dickinson, Franklin Lakes, NJ) to identify mean mitochondrial ROS production. Analysis was performed utilizing at least 10,000 events.
Assessment of mitochondrial DNA damage
After the designated time point following treatment, primary chondrocyte cultures were lysed overnight in buffer containing proteinase K (Roche, Indianapolis, IN). DNA was isolated by standard phenol–chloroform extraction, precipitated with cold ethanol, and digested overnight with BamHI (Roche, Indianapolis, IN). Prior to loading on an alkaline agarose gel for Southern blot analysis, each sample containing 5 μg of total DNA was incubated with 0.1 N of NaOH to reveal single strand breaks. After gel electrophoresis under alkaline conditions, DNA was transferred by means of vacuum transfer to a nylon membrane. Membranes were hybridized with a polymerase chain reaction-generated radioactive specific probe representing a part of the cytochrome-c oxidase subunit-III human mitochondrial gene. Autoradiograms were scanned for hybridization band intensity and DNA damage was evaluated as the amount of DNA breaks per 16 kb fragment. Break frequency was determined using the Poison expression (s = −lnP0, where s is the number of breaks per fragment, and P0 is the fraction of fragments free of breaks) [17].
Western blot analysis
To analyze changes in cellular proteins, Western blot analysis was employed. Following the designated treatment times, cells were lysed in cell lysing buffer (Cell Signaling Inc., Danvers, MA) and processed according to the manufacturer’s suggestions. These suspensions were centrifuged at 5,000 g to pellet any remaining debris, and the supernatant protein was used for Western blot analysis. The protein concentration was determined using the Bio-Rad protein dye microassay according to the manufacturer’s recommendation (Bio-Rad Laboratories Inc., Hercules, CA). Matrix metalloproteinase-1 (Pierce Biotechnology, Rockford, IL) and MMP-3 (Lab Vision Corporation, Fremont, CA) were used to evaluate MMP levels. Anti-actin antibody was used to ensure equal loading of total protein fractions.
Stastical analysis
Statistical analyses were performed utilizing one-way analysis of variance (GraphPad Software Inc., La Jolla, CA) where appropriate. These studies consisted of a minimum of an n = 3. A difference of P < 0.05 was considered significant. The Tukey’s post hoc test was used to determine the source of difference.
Results
The purpose of the study was to investigate if mtDNA damage and mitochondrial-originated oxidative stress modulates matrix destruction in the setting of OA through the upregulation of MMP protein levels. To induce mitochondrial-originated oxidative stress, chondrocytes were treated with various doses of the redox cycler menadione for 1 h. Cells were collected immediately after treatment, 1 h after treatment or 24 h after treatment. MitoSOX red was added to the cells and mitochondrial-originated ROS were detected via flow cytometry. MitoSOX red detects ROS in the mitochondria of live cells. Menadione-induced mitochondrial-generated ROS reached statistical significance after 1 h at a 50 μM concentration of menadione compared to control (Fig. 1). Additionally, this significant mitochondrial ROS production persisted even 24 h after menadione treatment. These data not only show significant ROS production, but it also suggests a state of mitochondrial-originated oxidative stress.
Flow cytometry analysis of increasing mitochondrial ROS production of cells treated with menadione. The chondrocytes were treated with various doses of menadione for 1 h. The chondrocytes then were trypsinized immediately after menadione treatment (0 h), 1 h after treatment (1 h) and 24 h after treatment (24 h). The chondrocytes then were collected and incubated with MitoSOX red (2 μM) for 10–15 min at 37 °C. The cells then were analyzed from at least 10,000 events via flow cytometry and mean fluorescent intensity values were recorded. Figures are graphed as the mean ± standard error and fold increase compared to control. The results were obtained from a minimum of three Independent experiments and *represents significant difference (P ≤ 0.05) from control vs sample treated with menadione
Many studies have shown that ROS-induced mtDNA damage and mutations lead to the synthesis of functionally impaired respiratory chain subunits, causing further respiratory chain dysfunction and augmented ROS production. To verify that mtDNA was damaged, Southern blot analysis was performed. Chondrocytes were treated with menadione for 1 h and cells were lysed after 24 h. As mtDNA is damaged, the hybridization band intensity decreases. Figure 2 shows a dose-dependent decrease of mtDNA integrity. The results of Southern blot analysis indicate an increase in mtDNA damage, thus likely resulting in further respiratory chain dysfunction.
Alkaline Southern blot analysis of mitochondrial DNA damage induced following exposure to 50, 20, and 10 μM of menadione for 1 h. Primary chondrocytes cultures were treated with menadione, then left to recover for 24 h. At the appropriate time, chondrocytes were lysed and DNA was isolated, restricted and analyzed with Southern blot analysis. Decreases in band intensity indicate increases in mtDNA damage accumulation (a). The results were obtained from a minimum of three independent experiments, and the graph represents the mean break frequency ± standard error mean (b). *indicates a significant difference (P < 0.05) in comparison to control
To determine whether this mitochondrial-originated oxidative stress leads to an increase in MMP levels, chondrocytes were treated with various doses of menadione. Western blot analysis was performed 24 h after menadione treatment. MMPs-1 and -3 are thought to play an important role in the progressive degradation of the extracellular matrix in OA. The data show that MMP-1 and -3 protein levels increased with increasing doses of menadione (Fig. 3). This increase reached significance at the 50 μM concentration of menadione. Therefore, as mitochondrial-originated ROS significantly increased, MMP protein levels significantly increased. Because MMP levels also reached significance at the 50 μM concentration, this dose was utilized for the remaining experiments.
Western blot analysis showing mitochondrial-generated ROS increases MMP protein levels. Primary chondrocytes cultures were treated with various doses of menadione for 1 h, then given 24 h to recover. The cells then were lysed and subjected to Western blot analysis to determine MMP-1 and MMP-3 (a) protein levels. Graphs represent the mean ± stand error mean of MMP-1 (b) or MMP-3 (c) protein levels. The results were obtained from a minimum of three independent experiments and *indicates a significant difference (P < 0.05) in comparison to control
If MMP protein levels increase with increases in mitochondrial-generated ROS, then we hypothesized that MMP levels would decrease with decreases in mitochondrial-generated ROS. To test this hypothesis, MitoTempo, a mitochondria-targeted antioxidant with superoxide and alkyl radical scavenging properties was employed. To determine the optimal concentration of MitoTempo, chondrocytes were treated with increasing doses of MitoTempo for 24 h. After the treatment time, cells were lysed and Western blot analysis was performed. Western blot analysis revealed a dose-dependent decrease in MMP protein levels (Fig. 4). These data show that scavenging levels of ROS decreases MMP levels.
In order to validate that mitochondrial-originated oxidative stress regulates MMP protein levels, chondrocytes were treated with menadione in the presence of MitoTempo. In Fig. 5, MMP-1 and -3 levels decrease with the addition of MitoTempo in comparison to menadione treatment without the addition of MitoTempo. Therefore, although mitochondrial-originated ROS and MMP protein levels increase with the addition of menadione, the addition of mitochondrial ROS scavengers decreases MMP. To our knowledge, this is the first study to show a relationship among mitochondrial-generated ROS, mtDNA damage, and MMP protein levels.
Mitochondrial ROS scavenging decreases mitochondrial ROS-induced MMP levels. Primary chondrocyte cultures were treated with Mitotempo (10 μM) before, during, and after 1 h treatment with menadione (50 μM). 24 h after menadione treatment, cells were lysed and subjected to Western blot analysis for MMP-1 (a) or MMP-3 (b). Graphs represent the mean ± stand error mean for MMP-1 (c) or MMP-3 (d) protein levels. The results were obtained from a minimum of three independent experiments and *indicates a significant difference (P < 0.05) in comparison to control
Discussion
The results of the present study show that elevated levels of ROS generated in chondrocytes can overwhelm repair mechanisms and significantly damage mtDNA. This damage to mtDNA can initiate signals which lead to the enhanced production of MMP-1 and MMP-3. When the ROS are scavenged by an antioxidant directed toward the mitochondria, mitochondrial-generated ROS is significantly reduced, and there is a concomitant decrease in the production of MMP-1 and MMP-3. These data provide evidence that mitochondrial-originated oxidative stress provides regulation of MMP protein levels.
Due to the importance of DNA repair processes, researchers have sought to correlate the biochemical events of DNA damage and repair with various biological endpoints including cell survival and death. Interest in mtDNA damage has risen with the discovery that defects in the mitochondrial genome are associated with several human hereditary diseases [18]. Additionally, the accumulation of mutations and deletions in mtDNA, with their associated defects in OXPHOS, have been implicated in diabetes, skeletal muscles, neurodegenerative diseases, and aging [19–23]. Furthermore, different mtDNA haplogroups have been shown to correlate with risk of OA [24].
The importance of mtDNA damage and dysfunction in the pathogenesis of OA has not been fully elucidated. One investigation shows that the destructive effects of pro-inflammatory cytokines on chondrocytes include the initiation of mtDNA damage and the concomitant onset of mitochondrial dysfunction [25, 26], consequently leading to increased ROS production in chondrocytes. Mitochondrial ROS can also be produced as a result of physiological mechanical strains, in which ROS plays a critical role as a second messenger [27, 28]. Furthermore, mitochondrial dysfunction could amplify the responsiveness to cytokine-induced chondrocyte inflammation through ROS production and NF-κB activation [29]. At present, it is far from clear which effects are primary or causative and which effects are secondary or associated side effects.
Several studies have been published addressing the effects of ROS on matrix synthesis. A few in vitro studies have reported the degradation of cartilaginous tissues by ROS-generating systems, likely by the direct attack of proteoglycan and collagen molecules by free radicals [30, 31]. It has been shown that incubation of acid soluble type I collagen with superoxide anion radicals, generated by the xanthine oxidase-hypoxanthine system, degraded collagen and prevented the formation of fibrils by this collagen [32]. Thus, ROS may serve as an inhibitory agent for cartilage matrix synthesis. Additionally, ROS may contribute to cartilage degradation by mediating the activation of latent MMPs.
MMPs-1 and -3 have been found to play a role in the destruction of the matrix in OA. Mitochondrial respiratory chain dysfunction has been show to modulate MMP expression [33]. More importantly, data provided in this paper shows it is the ROS generated by the mitochondria that can increase MMP protein levels. And when ROS from the mitochondria is scavenged, it leads to a subsequent decrease in MMP levels. Some researchers have demonstrated how hyaluronic acid reduces the MMP-3 expression and cartilage destruction [9, 14, 34]. Due to the scavenging properties of hyaluronic acid, this data seem to be consistent with our findings.
In conclusion, current evidence indicates that mitochondrial dysfunction and mtDNA damages are important players in the pathogenesis of OA, but data are lacking to support the hypothesis that these processes contribute to the impairment of cartilage integrity. This study shows how mtDNA damage and specifically ROS generated from the mitochondria, or lack thereof, can regulate MMP-1 and -3 protein levels. Future investigations are needed to fully define the relationship of mitochondria and MMPs in the pathogenesis of OA. This work provides new and important insight into the role of mitochondria in chondrocyte function and its potential importance in therapeutic approaches.
References
Pagano G, Talamanca AA, Castello G, Cordero MD, d’Ischia M, Gadaleta MN, Pallardo FV, Petrovic S, Tiano L, Zatterale A (2014) Oxidative stress and mitochondrial dysfunction across broad-ranging pathologies: toward mitochondria-targeted clinical strategies. Oxid Med Cell Longev 1–27 doi.org/10.1155/2014/541230
Ruiz-Romero C, Calamia V, Mateos J, Carreira V, Martinez-Gomariz M, Fernandez M, Blanco F (2009) Mitochondrial dysregulation of osteoarthritic human articular chondrocytes analyzed by proteomics. Mol Cell Proteomics 8(1):172–189
Pelletier JP, Jovanovic DV, Lascau-Coman V, Fernandes JC, Manning PT, Connor JR et al (2000) Selective inhibition of inducible nitric oxide synthase reduces progression of experimental osteoarthritis in vivo: possible link with the reduction in chondrocyte apoptosis and caspase 3 level. Arthritis Rheum 43:1290–1299
Grishko V, Renee H, Wilson GL, Pearsall AW (2009) Diminished mtDNA integrity and repair capacity in OA chondrocytes. Osteoarthritis Cartilage 17:107–113
Johnson K, Jung AS, Andreyev A, Murphy A, Dykens J, Terkeltaub R (2000) Mitochondrial oxidative phosphorylation is a downstream regulator of nitric oxide effects on chondrocyte matrix synthesis and mineralization. Arthritis Rheum 43(7):1560–1570
Loeser RF, Carlson CS, Del Carlo M, Cole A (2002) Detection of nitrotyrosine in aging and osteoarthritic cartilage: correlation of oxidative damage with the presence of interleukin-1 beta and with chondrocyte resistance to insulin-like growth factor 1. Arthritis Rheum 46:2349–2357
Carlo MD, Schwartz D, Erickson EA, Loeser RF (2007) Endogenous production of reactive oxygen species is required for stimulation of human articular chondrocyte matrix metalloproteinase production by fibronectin fragments. Free Radic Biol Med 42:1350–1358
Nelson KK, Melendez JA (2004) Mitochondrial Redox Control of Matrix Metalloproteinases. Free Radic Biol Med 37:768–784
Lewis EJ, Bishop J, Bottomley KM, Bradshaw D, Brewster M, Broadhurst MJ, Brown PA, Budd JM, Elliott L, Greenham AK, Johnson WH, Nixon JS, Rose F, Sutton B, Wilson K (1997) Ro 32-3555, an orally active collagenase inhibitor, prevents cartilage breakdown in vitro and in vivo. Br J Pharmacol 121:540–546
Turrens JF (2003) Mitochondrial formation of reactive oxygen species. J Physiol 552:335–344
Chance B, Williams GR (1995) Respiratory enzymes in oxidative phophorylation. I. Kinetics of oxygen utilization. J Biol Chem 217:383–393
Grill L, Nohl H (2001) The ubiquinol/bc1 redox couple regulates mitochondrial oxygen radical formation. Arch Biochem Biophys 388:34–38
Lee RB, Urban JP (1997) Evidence for a negative Pasteur effect in articular cartilage. Biochem J 321:95–102
Maneiro E, Martin MA, de Andres MC, Lopez-Armada MJ, Fernandez-Sueiro JL, del Hoyo P et al (2003) Mitochondrial respiratory activity is altered in OA human articular chondrocytes. Arthritis Rheum 48:700–708
Roach HI (2008) The complex pathology of osteoarthritis: even mitochondria are involved. Arthritis Rheum 58(8):2217–2218 (32)
Mukhopadhyay P, Rajesh M, Yoshihiro K, Hasko G, Pacher P (2007) Simple quantitative detection of mitochondrial superoxide production in live cell. Biochem Biophys Res Commun 358(1):203–208
Grishko V, Xu M, Wilson G, Pearsall A (2010) Apoptosis and mitochondrial dysfunction in human chondrocytes following exposure to lidocaine, bupivacaine, and ropivacaine. J Bone Joint Surg Am 92:609–618
Schon EA, DiMauro S, Hirano M (2012) Human mitochondrial DNA: roles of inherited and somatic mutations. Nat Rev Genet 13(12):878–890
Suzuki S, Hinokio Y, Komatu K, Ohtomo M, Onoda M, Hirai S, Hirai M et al (1999) Oxidative damage to mitochondrial DNA and its relationship to diabetic complications. Diabetes Res Clin Pract 45(2–3):161–168
Lim PS, Cheng YM, Wei YH (2000) Large-scale mitochondrial DNA deletions in skeletal muscle of patients with end stage renal disease. Free Radic Biol Med 29:454–463
Linnane AW, Marzuki S, Wzawa T, Tanaka M (1989) Mitochondrial DNA mutations as an important contributor to aging and degenerative disease. Lancet i:642–645
Sohal RS, Agarwal A, Agarwal S, Orr WC (1995) Simultaneous overexpression of copper and zinc-containing superoxide dismutase and catalase retards age-related oxidative damage and increases metabolic potential in Drosophila melanogaster. J Biol Chem 270:15671–15674
Sohal RS, Agarwal S, Bubey A, Orr WC (1993) Protein oxidative damage is associated with life expectancy of houseflies. Proc Natl Acad Sci USA 90:7255–7259
Rego-Perez I, Fernandez-Moreno M, Fernandez-Lopez C, Arenas J, Blanco FJ (2008) Mitochondrial DNA haplogroups: role in the prevalence and severity of knee osteoarthritis. Arthritis Rheum 58(8):2387–2396
Kim J, Xu M, Ho R, Mates A, Wilson GL, Pearsall AW, Grishko V (2010) Mitochondrial DNA damage is involved in apoptosis caused by pro-inflammatory cytokines in human OA. Osteoarthritis Cartilage 18:424–432
Lopez-Armada MJ, Carames B, Martin MA, Cillero-Pastor B, Lires-Dean M, Fuentes-Boquete I, Arenas J, Blanco FJ (2006) Mitochondrial activity is modulated by TNF alpha and IL-1beta in normal human chondrocyte cell. Osteoarthritis Cartilage 14(10):1011–1022
Wolff KJ, Ramakrishnan PS, Brouillette MJ, Journot BJ, McKinley TO, Buckwalter JA, Martin JA (2013) Mechanical stress and ATP synthesis are coupled by mitochondrial oxidants in articular cartilage. J Orthop Res 31(2):191–196
Brenneisen P, Wenk J, Klotz LO, Wlaschek M, Briviba K, Krieg T, Sies H, Scharffetter-Kochanek K (1998) Central role of ferrous/ferric iron in the ultraviolet B irradiation-mediated signaling pathway leading to increased interstitial collagenase (matrix-degrading metalloprotease (MMP)-1) and stromelysin-1 (MMP-3) mRNA levels in cultured human dermal fibroblasts. J Biol Chem 273(9):5279–5287
Vaamonde-García C, Riveiro-Naveira RR, Valcárcel-Ares MN (2012) Mitochondrial dysfunction increases inflammatory responsiveness to cytokines in normal human chondrocytes. Arthritis Rheum 64:2927–2936
Stowe DF, Camara AK (2009) Mitochondrial reactive oxygen species production in excitable cells: modulators of mitochondrial and cell function. Antioxid Redox Signal 11:1373–1414
Vincent F, Brun H, Clain E, Ronot X, Adolphe M (1989) Effects of oxygen free radicals on proliferation kinetics of cultured rabbit articular chondrocytes. J Cell Physiol 141:262–266
Monboisse JC, Braquet P, Borel JP (1983) Non enxymatic degradation of acid soluble collagen by superoxide anion: protective effect of flavonoids. Biochem Pharmacol 32:53–58
Cillero-Pastor B, Rego-Perez I, Oreiro N, Fernandez-Lopez C, Blanco Francisco (2013) Mitochondrial respiratory chain dysfunction modulates metalloproteases -1, -3 and -13 in human normal chondrocytes in culture. BMC Musculoskelet Disord 14:235
Henrotin E, Bruckner P, Pujol JP (2003) The role of reactive oxygen species in homeostasis and degradation of cartilage. Osteoarthritis Cartilage 11:747–755
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reed, K.N., Wilson, G., Pearsall, A. et al. The role of mitochondrial reactive oxygen species in cartilage matrix destruction. Mol Cell Biochem 397, 195–201 (2014). https://doi.org/10.1007/s11010-014-2187-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-014-2187-z