Abstract
Expression of angiotensin II (Ang II) and its receptors (AT1/AT2) is undetected in the mature microglia in normal brain. We report here that the immunoexpression of Ang II and AT1/AT2 was altered in activated microglia notably at 1 week in rats subjected to middle cerebral artery occlusion (MCAO). Immunolabeled activated microglia were widely distributed in the infarcted cerebral tissue after MCAO. By enzyme immunoassay, Ang II protein expression levels of the ischemic tissues were decreased drastically at 12 h after ischemia, then rose rapidly at 3 days and 1 week after MCAO when compared with the control. On the other hand, AT1 and AT2 receptor mRNA and protein levels were up-regulated after MCAO, peaking at 12 h, but declined thereafter. Expression of tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) mRNA and protein levels was concomitantly increased. Edaravone significantly suppressed Ang II and AT1/AT2 receptor expression as well as that of TNF-α and IL-1β suggesting that microglia-derived Ang II can act through an autocrine manner via its receptor that may be linked partly to the production of proinflammatory cytokines. We conclude that neuroinflammation in MCAO may be attenuated by Edaravone which acts through suppression of expression of Ang II and its receptors and proinflammatory cytokines in activated microglia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiotensin II (Ang II) is a peptide hormone which not only acts on the vasculature and heart, but also in the brain to mediate important neuroendocrine functions [1, 2]. Ang II exerts its effects on the central nervous system (CNS) primarily via the two G protein-coupled receptors, Ang II type 1 receptor (AT1), and Ang II type 2 receptor (AT2). The peptide Ang II, via AT1 receptor, is one of the most important inflammation and oxidative stress inducers, and produces reactive oxygen species (ROS) by activation of the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase complex [3].
Experimental evidence suggests an important role of Ang II and its receptors in hypoxic/ischemic brain injury. Ang II participates in the pathogenesis of ischemia via AT1. The selective AT1 receptor blocker improves the neurological outcome and reduces the infarct volume after experimental ischemia in the rat brain [4]. The cerebral AT2 receptors are associated with neurite outgrowth and protection of brain tissue after focal cerebral ischemia [5]. Ang II could attenuate hypoxia-induced apoptosis in primary cortical neuronal cultures through activation of the AT2 receptor [6]. The inflammatory response is mediated by the activated microglia which respond robustly to the neuronal damage [7]. However, the involvement of Ang II and its receptors in microglial activation and brain injuries (or inflammation) remains to be clarified.
We have previously demonstrated the expression of Ang II and AT1/AT2 receptors in amoeboid microglial cells (AMC) in the developing brain [8]. It was suggested that Ang II and AT1/AT2 receptors localized in AMC might be linked to regulation and release of chemokines and cytokines [8]. Expression of Ang II and its receptors, however, in microglia was progressively reduced with the transformation of AMC into mature microglia with advancing age. This study aimed to determine if mature microglia in adult brain, when activated in ischemic condition such as middle cerebral artery occlusion (MCAO), would be induced to express Ang II and its receptors. A hallmark of brain injury is the accumulation of activated microglia [9]; therefore, we have used a rat model of MCAO to investigate the activation of microglia [10]. More specifically, this study sought to ascertain if Ang II and its receptors are expressed in activated microglia in response to ischemia. We also investigated whether Edaravone, a neuroprotective agent and an antioxidant, would regulate microlglia expression of Ang II and AT1/AT2 receptors.
Materials and methods
Animals and animal surgery
All the experiments were carried out in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals. 135 adult male Sprague Dawley rats weighing between 250 and 280 g were used. Anesthesia of the rats was achieved by an intraperitoneal injection of sodium pentobarbital (50 mg/kg). The surgical procedure followed that described previously by Wu et al [10]. Briefly, a circular aperture 3 mm in diameter was burred in the right parietal bone with a dental drill, and the main trunk of the middle cerebral artery (MCA) was exposed and cauterized. In the sham-operated rats, the same surgical procedure was followed but the MCA was not cauterized. The rats were randomly divided into MCAO groups (3, 6, 12 h, 1, 2, 3 days, and 1 week after MCAO, n = 15 at each time point), sham-operated rats (n = 15) and normal rats (n = 15).
Injection of Edaravone
Twenty rats were divided into two groups for real-time polymerase chain reactions (RT-PCR) and western blotting analysis, respectively. 10 rats were used for each group sacrificed at 3 days (n = 5) and 1 week (n = 5), respectively. The rats in the respective groups were given an intraperitoneal (i.p.) injection of Edaravone (3-methyl-1-phenyl-2-pyrazolin-5-one) (5 mg/kg dissolved in saline; Cat. No. S2007001158, CHI) at 2 h before MCAO and at 12, 24, and 36 h after MCAO. Along with the Edaravone injected rats, 10 rats receiving an equal volume of saline served as matching controls.
Real-time polymerase chain reactions
Under deep anesthesia, the rats were killed by decapitation. The ischemic cortex from rats sacrificed at 3, 6, 12 h, and 1, 2, 3, 7 days after MCAO and at 3 days, 1 week after Edaravone treatment groups (n = 5 at each time point), their matching shams (n = 5), normal controls (n = 5), and vehicle-treated group (n = 5) were removed and immediately frozen in liquid nitrogen and stored at −80 °C until RNA isolation. Total RNA was extracted from the control and ischemic rat cortex using RNAesy mini kit (Qiagen, CA, USA) according to the manufacturer’s protocol. Quantitative RT-PCR was carried out on a Light Cycler 3 instrument using a FastStart DNA Master plus SYBR Green I kit (Roche Diagnostics GmbH, Roche Applied Science, Mannheim, Germany) according to the manufacturer’s instructions. The cDNA was used to amplify a 214, 196, 134, and 123-bp fragment using specific primers for AT1 (forward 5′-tgatcaccaggtcaagtgga-3′; reverse 5′-atcaccaccaagctgtttcc-3′), AT2 (forward 5′-ccttcttggatgctctgacc-3′; reverse 5′-tggagccaagtaatgggaac-3′), TNF-α (forward 5′-ccaacaaggaggagaagttcc-3′; reverse 5′-ctctgcttggtggtttgctac-3′), and IL-1β (forward 5′-ggaacccgtgtcttcctaaag-3′; reverse 5′-ctgacttggcagaggacaaag-3′), respectively. For the control and normalizing the quantities of each sample, rat β-actin was adopted. The β-actin forward primer 5′-tcatgaagtgacgttgacatccgt-3′ and reverse primer 5′-cctagaagcatttgcggtgcaggatc-3′, lead to amplification of a 285-bp DNA fragment. Gene expression was quantified using a modification of the 2−ΔΔct method as previously described [11].
Western blotting
The ischemic cortex respectively derived from MCAO (n = 5 for each time point), Edaravone treatment groups (n = 5 for each time point), vehicle-treated group (n = 5), their matching shams (n = 5) and normal controls (n = 5) rats, was snap-frozen in liquid nitrogen and stored at −80 °C. Tissue samples from various groups were homogenized with protein extraction reagent (Pierce, IL, USA) containing protease inhibitors. The protein concentrations were measured by the method of Bradford (1976) using bovine serum albumin as a standard. Samples of supernatants containing 40-μg protein were heated to 95 °C for 5 min, and were separated by sodium dodecyl sulfate-poly-acrylamide gel electrophoresis in 10 % gels, in a Mini-Protein II apparatus (Bio-Rad, CA, USA). Protein bands were electroblotted onto polyvinylindene difluoride (PVDF) membrane and blocked with non-fat dried milk. The membranes were incubated with AT1 (rabbit polyclonal IgG 1:200) (Santa Cruz Biotechnology, CA, USA; Cat. No. sc-1173), AT2 (rabbit polyclonal IgG 1:200) (Santa Cruz Biotechnology, CA, USA; Cat. No. sc-9040), TNF-α (rabbit polyclonal IgG 1:1000) (Chemicon International, Temecula, CA, USA; Cat. No. AB1837P), IL-1β (rabbit polyclonal IgG 1:5000) (Chemicon International; Cat. No. AB1832P), and β-actin (mouse monoclonal IgG 1:5000) (Sigma; Cat. No. A2172) primary antibodies diluted in blocking solution overnight at 4 °C. They were then incubated with the secondary antibodies, horseradish peroxidase (HRP) conjugated anti-rabbit IgG (dilution 1:5000) (Cell Signaling Technology; Cat. No 7074). Specific binding was revealed by an enhanced chemiluminescence kit (GE Healthcare UK Limited, Bucks, UK) following the manufacturer’s instructions.
Analysis of angiotensin II concentration by enzyme immunoassay (EIA)
The quantity of Ang II released in the cerebral cortex samples from the control, sham, following ischemic exposure, Edaravone treatment groups for each time point and vehicle-treated group were determined using the Ang II EIA kit (RayBiotech, Inc. Cat#: EIA-ANGII-1). Homogenates, as described above for Western blotting, were prepared and EIA measurements were performed according to the manufacturer’s protocol. Briefly, 100 μl anti-AngiotensinIIantibody was added into the pre-coated 96-well plate and incubated for 1.5 h at room temperature (22–24 °C) or overnight at 4 °C. After thorough washing four times with washing buffer, 100 μl of prepared standards or supernatant of the cerebral cortex samples was added into each well and a further incubation for 2.5 h at room temperature or overnight at 4 °C was carried out; then washing four times with washing buffer. Following this, 100 μl of prepared streptavidin solution was added into each well and incubated for 45 min at room temperature. After thorough washing four times with washing buffer, 100 μl of TMB one-step substrate reagent was added into each well in the dark and incubated for 30 min at room temperature. Subsequently, 50 μl of stop solution was added into each well, then the optical density was measured at 450 nm. The quantity of Ang II (ng/ml) detected in each sample was compared with an Ang II standard curve.
Immunofluorescence and double labeling
Rats killed at 3, 6, 12 h, and 1, 2, 3 days and 1 week after ischemia (n = 5 at each time interval) along with their matching sham rats (n = 5) and normal controls (n = 5) were used for double immunofluorescence. Following deep anesthesia with 6 % sodium pentobarbital, the rats were sacrificed by perfusion with 2 % paraformaldehyde in 0.1 M phosphate buffer. The brain was removed and the tissue was embedded in paraffin. Coronal sections of 10-μm thickness were cut and the sections were restored with 0.01 M citric acid buffer solution (pH 6.0). Endogenous peroxidase was blocked with 0.03 % hydrogen peroxide for 15 min. After several washes with phosphate buffered saline (PBS), the tissue sections were incubated in a humidified chamber with polyclonal rabbit anti-AT1 (rabbit polyclonal IgG 1:200; Cat. No. sc-1173), AT2 (rabbit polyclonal IgG 1:200; Cat. No. sc-9040), and polyclonal rabbit anti-Ang II (Santa Cruz Biotechnology, CA, USA; Cat. No. sc-20717). The sections were incubated respectively with fluorescent secondary antibodies: CY3-conjugated goat anti-rabbit IgG and FITC-conjugated lectin that labels both microglia and blood vessel endothelial cells for 1 h at room temperature. Some sections were treated simultaneously without the primary antibodies to confirm the specificity of immunoreactivities. Co-localization was verified by confocal microscopy (FV1000, Olympus company Pte Ltd, Tokyo, Japan).
Statistical analysis
The statistical analysis of the data was carried out using one-way ANOVA. The data represent mean ± SD. Significance of difference is indicated in the bar graphs by an asterisk (*p < 0.05).
Results
Changes in amount of angiotensin II in ischemic cerebral tissue
Enzyme immunoassay revealed that Ang II was detected in the cerebral cortex of ischemic rats. The Ang II concentration decreased drastically (p < 0.05) at 12 h, and then rose significantly at 3 days and 1 week (p < 0.05) after MCAO when compared with the control (Fig. 1).
Changes in AT1/AT2, TNF-α, and IL-1β gene expression in ischemic cerebral tissue
The expression levels of both AT1 and AT2 mRNA were progressively increased, peaking at 12 h after the ischemic insult (Fig. 2a, b); thereafter, the expression declined drastically so that by 1 week, it was comparable to that of the control. TNF-α and IL-1β mRNA expression levels were coincident with that of AT1 and AT2, respectively. The expression levels of both proinflammatory cytokines rose rapidly by more than tenfolds at their peak at 12 h after the ischemic injury, when compared with the controls (p < 0.05). At 1 week, TNF-α mRNA level was comparable to that of the control; on the other hand, MCAO induced increase in IL-1β expression was maintained at levels above that of the controls throughout the remaining duration (Fig. 2c, d) (p < 0.05).
RT-PCR analysis of AT1, AT2, TNF-α, and IL-1β gene expression of the normal control and sham-operated rats, and of rats at 3, 6, 12 h, and 1, 2, 3 days and 1 week after MCAO. Graphical representation of fold change of mRNA of AT1 (a), AT2 (b), TNF-α (c) ,and IL-1β (d) as quantified by normalization to the β-actin as an internal control. Each bar represents mean ± SD. *Significant differences in mRNA levels in rats after the ischemia when compared with the control at each time point, p < 0.05. All the experiments were carried out in triplicate
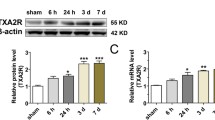
Changes in AT1/AT2, TNF-α, and IL-1β protein expression in ischemic cerebral tissue
AT1 and AT2 , which were detected at 43 and 44 kD, were significantly increased (Fig. 3a), respectively, in density 3 h to 1 week, and 6 h to 1 week when compared with the controls (p < 0.05) (Fig. 3b, c). Expression of both receptors peaked at 12 h after MCAO, but it declined thereafter. The immunoreactive band of TNF-α protein levels that appeared at approximately 30 kDa (Fig. 4a) increased drastically in optical density at 3, 6, 12 h and 1 day after ischemic exposure as compared with the controls (p < 0.05) (Fig. 4b). TNF-α protein expression was markedly reduced at 2 days and remained at a low level after this time point. The immunoreactive band of IL-1β protein levels that appeared at ~17 kDa (Fig. 4a) increased significantly in optical density after ischemia notably at 6 h as compared with the controls (p < 0.05) (Fig. 4c); beyond this time point, IL-1β protein expression level was progressively reduced.
Western blotting of AT1 and AT2 protein expression of cerebral cortex tissue supernatants of rats in the control and sham-operated rats, and of rats at 3, 6, 12 h, and 1, 2, 3 days and 1 week after MCAO. a AT1 (43 kDa), AT2 (44 kDa), and β-actin (43 kDa) immunoreactive bands. Bar graphs significant change in the optical density of AT1 (b), and AT2 (c) following ischemia (mean ± SD). *Significant differences in protein levels in rats after the ischemia when compared with the control at each time point, p < 0.05. All the experiments were carried out in triplicate
Western blotting of TNF-α and IL-1β protein expression of cerebral cortex tissue supernatants of rats in the control and sham-operated rats, and of rats at 3, 6, 12 h, and 1, 2, 3 days and 1 week after MCAO. a TNF-α (30 kDa), IL-1β (17 kDa), and β-actin (43 kDa) immunoreactive bands. Bar graphs significant change in the optical density of TNF-α (b), and IL-1β (c) following ischemia (mean ± SD). *Significant differences in protein levels in rats after the ischemia when compared with the control at each time point, p < 0.05. All the experiments were carried out in triplicate
Localization of angiotensin II in microglial cells
Angiotensin II immunoreactivity was undetected in microglial cells in the control rats. At 2 and 3 days after MCAO, Ang II immunofluorescence in activated microglia was hardly detected; however, it was induced in many lectin labeled activated microglial cells in both the infarcted and peri-infacted zones at 1 week after MCAO (Fig. 5).
Confocal images showing lectin (green) labeled microglial cells double labeled with angiotensin II (red) in the ischemic cortex at 3 days and 1 week after MCAO and the normal controls. Co-localized expression of lectin and angiotensin II in microglial cells is seen in the ischemic cortex notably at 1 week after MCAO (yellow, arrows). Blood vessels (asterisk) also display moderate angiotensin II immunoreactivity. Scale bar 50 μm. (Color figure online)
Localization of AT1 /AT2 receptor in microglial cells
In the control rats, AT1 /AT2 expression was not detected in the microglial cells. At 3 days and 1 week following ischemia, intense AT1 /AT2 immunoreactivity was induced in the activated microglial cells both in the infarcted and peri-infarted (penumbral) zones when compared with the controls (Figs. 6, 7). At 1 week, AT1 /AT2 immunoreactive activated microglia were clearly hypertrophic and appeared amoeboidic with some cells closely associated with the blood vessels (Figs. 6, 7).
Confocal images showing lectin (green) labeled microglial cells double labeled with AT1 receptor (red) in the ischemic cortex at 3 days and 1 week after MCAO and the controls. Co-localized expression of lectin and AT1 is seen in the massive microglial cells being most conspicuous at 1 week (yellow, arrows). Blood vessels (asterisk) also display a moderate AT1 immunoreactivity. Scale bar 50 μm. (Color figure online)
Confocal images showing lectin (green) labeled microglial cells double labeled with AT2 receptor (red) in the ischemic cortex at 3 days and 1 week after MCAO and the controls. Co-localized expression of lectin and AT2 in microglial cells is seen in merge images after MCAO (yellow, arrows). Blood vessels (asterisk) also display a moderate AT2 immunoreactivity. Scale bars 50 μm. (Color figure online)
Edaravone suppressed AT1 /AT2 receptor, TNF-α, and IL-1β gene expression after ischemia
Expression levels of AT1/AT2 receptor, TNF-α, and IL-1β mRNAs were markedly suppressed at 3 days after Edaravone treatment when compared with the vehicle-treated controls (p < 0.05) (Fig. 8a–d). At 1 week, AT1/AT2, TNF-α, and IL-1β mRNAs expression levels were comparable to that of the corresponding control (Fig. 8a–d).
RT-PCR analysis of AT1, AT2, TNF-α, and IL-1β gene expression of rats at 3 days and 1 week after Edaravone treatment and matching controls. Graphical representation of fold change of mRNA of AT1 (a), AT2 (b), TNF-α (c), and IL-1β (d) as quantified by normalization to the β-actin as an internal control. Each bar represents mean ± SD. *Significant differences in mRNA levels in rats after Edaravone treatment when compared with the matching control at each time point, p < 0.05
Edaravone suppressed angiotensin II, AT1/AT2 receptor, TNF-α, and IL-1β protein expression after ischemia
Enzyme immunoassay revealed that the Ang II concentration decreased significantly (p < 0.05) at 3 days with Edaravone treatment after ischemic injury when compared with the controls. At 1 week, Ang II protein level also remained lower than that of the control (Fig. 9). By western blot analysis, the protein expression levels of AT1 /AT2 receptor, TNF-α, and IL-1β which were detected at 43 and 44 kD, 30 and 17 kDa (Fig. 10a) were drastically suppressed at 3 days after the Edaravone treatment when compared with the vehicle-treated controls (Fig. 10b–e). At 1 week, AT1, TNF-α, and IL-1β protein expression levels returned to level comparable to that of the control, whereas that of AT2 was not restored to the control level.
Angiotensin II tissue concentration in the rat cerebral cortex samples at 3 days and 1 week after Edaravone treatment and matching controls determined by EIA. Data represent mean ± SD. *Significant differences in angiotensin II concentration in rats after Edaravone treatment when compared with the matching control at each time point, p < 0.05
Western blotting of AT1, AT2, TNF-α, and IL-1β protein expression of cerebral cortex tissue supernatants of rats at 3 days and 1 week after Edaravone treatment and matching controls. a AT1 (43 kDa), AT2 (44 kDa) TNF-α (30 kDa), IL-1β (17 kDa), and β-actin (43 kDa) immunoreactive bands. Bar graphs significant change in the optical density of AT1 (b), AT2 (c), TNF-α (d), and IL-1β (e) at 3 days and 1 week following Edaravone treatment (mean ± SD). *Significant differences in protein levels in rats after Edaravone treatment when compared with the matching control at each time point, p < 0.05
Discussion
The principal cellular source of brain angiotensin is the astrocytes and neurons [12, 13]. It exerts various actions mainly via interaction with AT1/AT2, and contributes to blood pressure regulation and the process of growth and development and tissue repair [14]. Expression of Ang II and its receptors in microglial cells has been reported in the AMC [8]. Expression of Ang II and its receptors in AMC was progressively reduced with advancing age and was undetected in the mature microglia. This suggests that Ang II and its receptors are less active in the normal mature microglia. We show here that the expression of Ang II and AT1/AT2 was altered at different time points after MCAO.
By EIA analysis, Ang II concentration in the ischemic cortex decreased drastically (p < 0.05) at 12 h, and then rose significantly at 3 days and 1 week (p < 0.05) after MCAO. On the other hand, AT1/AT2 mRNA and protein expression responded swiftly to MCAO as early as 3–6 h after ischemia revealed by RT-PCR and western blot analysis, and peaking at 12 h after MCAO. The decrease in Ang II at 12 h after MCAO may be an autoregulation mechanism to allow more blood flow to the ischemic cortex. Mean while, expression of AT1/AT2 was markedly increased which may be due to a compensatory response. Notwithstanding, it is suggested that both Ang II and AT1/AT2 are responsive to ischemic change with the latter expression being more sensitive as the increase occurred at 3 h. A major finding of this study was the localization of intense Ang II immunofluorescence in activated microglia at 1 week after MCAO indicates them as an important cellular source of Ang II in the ischemic brain other than the neurons and astrocytes [12, 13]. This is consistent with the EIA results which showed a rise in Ang II at this time point. AT1/AT2 immunofluorescence was also pronounced at 1 week in activated microglia after MCAO. The co-expression of Ang II and AT1/AT2 in activated microglia in ischemia suggests that Ang II can act through its receptors via an autocrine manner. The occurrence of a large number of activated microglia at 3 days and 1 week after MCAO is consistent with the findings by Kato et al [15] and Soltys et al [16]. It is well documented that microglia produce a variety of inflammatory factors in CNS injuries. The intense expression of Ang II and AT1/AT2 after MCAO suggests its involvement in microglial primary function such as production of proinflammatory cytokines as reported by us [8]. Indeed, the mRNA and protein expression of TNF-α and IL-1β, which are the major molecules induced by various inflammatory stimuli was concurrently increased in activated microglia after MCAO.
We show here a significant decrease in Ang II concentration at 12 h after MCAO. Remarkably, increase in expression of AT1 and AT2 receptors mRNA and protein was acute in onset after MCAO, peaking at 12 h indicating that Ang II has exerted the hormonal actions on blood pressure and body fluid homoeostasis via the AT1 receptor subtype. Decrease in the total tissue Ang II expression at 12 h after ischemia may increase the brain blood flow by reducing the constriction of the cerebral microvessels. In addition to the regulating blood pressure, Ang II participates in the pathogenesis of ischemia via AT1 [17]. AT1 receptor blockers can reduce the infarct volumes and enhance functional recovery in the experimental cerebral ischemia model [4, 18]. Ang II exerts an opposite action to that of the AT1 receptor via AT2 receptors. Ang II acting through the AT2 receptor represents a neurotrophic factor for neurons in the central nervous system [19]. There is also evidence that cerebral AT2 receptors exert neuroprotective actions and support neuronal survival in response to ischemia-induced neuronal injury via inhibiting AT1 receptors [5]. The present results have also shown a significant increase in Ang II concentration at 3 days and 1 week after MCAO. This was coincident with a moderate decline from the peak expression of AT1 and AT2 receptors at 12 h following MCAO suggesting that both the receptors act in concert for a balanced interaction with Ang II in longer surviving animals. It is evident that the underlying mechanism for this remains subtle and complex and it remains to be further investigated.
Angiotensin II is the principal inducer of oxidative stress and inflammation in CNS injury [20, 21]. It has been reported that AT1 receptor blockers attenuate the inflammatory and oxidative stress [22], regulate the nitric oxide synthase isoenzymes in the brain [23], and inhibit or ameliorate apoptosis [15]. Stimulation of AT2 receptors exerts an opposite effect, i.e., the protective role of AT2 receptors against inflammatory response. In this connection, it has been reported that Edaravone as a hydroxyl radical scavenger is effective in inhibiting the inflammatory responses [24], brain edema [25], ROS generation, oxidative tissue damage [26], and delayed neuronal death [27]. We show here an unequivocal anti-inflammatory action of Edaravone in the MCAO model. At various time points after Edaravone treatment, the expression of Ang II, AT1/AT2 receptors, TNF-α, and IL-1β was suppressed, notably at 3 days. This therefore suggested that Edaravone may be used to reduce inflammatory-related damage mediated by activated microglia. We reported previously that Edaravone suppressed TNF-α and IL-1β production by lipopolysaccharide activated BV-2 microglia. It may act directly on Ang II/AT1/AT2 and thence on production of cytokines. This is because the neutralization of AT2 with its antibody resulted in decrease in TNF-α and IL-1β production [8]. The often possibility is that Edaravone may exert its effect on the pathways such as the NF-κB for TNF-α and IL-1β production [28, 29].
Conclusion
A major finding in this study was induced expression of Ang II and AT1/AT2 in activated microglia after MCAO. The accumulation of large numbers of activated microglia at the site of infarct suggests their significant contribution to production of Ang II at the site of ischemia which can act via an autocrine manner on microglial cells bearing the two receptors. Edaravone treatment effectively suppresses the expression of Ang II, AT1/AT2 receptors along with that of TNF-α and IL-1β. Ang II via their receptors AT1/AT2 is known to regulate the production of TNF-α and IL-1β in activated microglia. The suppresion of Ang II and its receptors by Edaravone in activated microglia in MCAO suggests that it is an important molecular target, among others, for amelioration of neuroinflammation in cerebral ischemia in which the activated microglial cells are implicated.
References
Thomas WG, Greenland KJ, Shinkel TA, Sernia C (1992) Angiotensinogen is secreted by pure rat neuronal cell cultures. Brain Res 588:191–200
Lanz TV, Ding Z, Ho PP, Luo J, Agrawal AN, Srinagesh H, Axtell R, Zhang H, Platten M, Wyss-Coray T, Steinman L (2010) Angiotensin II sustains brain inflammation in mice via TGF-β. J Clin Invest 120:2782–2794
Joglar B, Rodriguez-Pallares J, Rodriguez-Perez AI, Rey P, Guerra MJ, Labandeira-Garcia JL (2009) The inflammatory response in the MPTP model of Parkinson’s disease is mediated by brain angiotensin: relevance to progression of the disease. J Neurochem 109:656–669
Dai WJ, Funk A, Herdegen T, Unger T, Culman J (1999) Blockade of central angiotensin AT (1) receptors improves neurological outcome and reduces expression of AP-1 transcription factors after focal brain ischemia in rats. Stroke 30:2391–2398
Li J, Culman J, Hörtnagl H, Zhao Y, Gerova N, Timm M, Blume A, Zimmermann M, Seidel K, Dirnagl U, Unger T (2005) Angiotensin AT2 receptor protects against cerebral ischemia-induced neuronal injury. FASEB J 19:617–619
Grammatopoulos T, Morris K, Ferguson P, Weyhenmeyer J (2002) Angiotensin protects cortical neurons from hypoxic-induced apoptosis via the angiotensin type 2 receptor. Mol Brain Res 99:114–124
Dheen ST, Kaur C, Ling EA (2007) Microglial activation and its implications in the brain diseases. Curr Med Chem 14:1189–1197
Li JJ, Lu J, Kaur C, Sivakumar V, Wu CY, Ling EA (2009) Expression of angiotensin II and its receptors in the normal and hypoxic amoeboid microglial cells and murine BV-2 cells. Neuroscience 158:1488–1499
Ling EA, Ng YK, Wu CH, Kaur C (2001) Microglia: its development and role as a neuropathology sensor. Prog Brain Res 132:61–79
Wu YP, Tan CK, Ling EA (1998) Expression of c-fos immunoreactivity in brain spinal cord neurons following the occlusion of middle cerebral artery in rats. Exp Brain Res 115:129–136
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2 (-Delta Delta C (T) Method. Methods 24:402–408
Hermann K, Raizada MK, Sumners C, Phillips MI (1988) Immunocytochemical and biochemical characterization of angiotensin I and II in cultured neuronal and glial cells from rat brain. Neuroendocrinology 47:125–132
Lind RW, Swanson LW, Ganten D (1985) Organization of angiotensin II immunoreactive cells and fibres in the rat central nervous system: an immunocytochemical study. Neuroerldocrinology 40:2–24
Stoll M, Unger T (2001) Angiotensin and its AT2 receptor: new insights into an old system. Regul Pept 99:175–182
Kato H, Takahashi A, Itoyama Y (2003) Cell cycle protein expression in proliferating microglia and astrocytes following transient global cerebral ischemia in the rat. Brain Res Bull 60:215–221
Soltys Z, Orzylowska-Sliwinska O, Zaremba M, Orlowski D, Piechota M, Fiedorowicz A, Janeczko K, Oderfeld-Nowak B (2005) Quantitative morphological study of microglial cells in the ischemic rat brain using principal component analysis. J Neurosci Methods 146:50–60
Jung KH, Chu K, Lee ST, Kim SJ, Song EC, Kim EH, Park DK, Sinn DI, Kim JM, Kim M, Roh JK (2007) Blockade of AT1 receptor reduces apoptosis, inflammation, and oxidative stress in normotensive rats with intracerebral hemorrhage. J Pharmacol Exp Ther 322:1051–1058
Nishimura Y, Ito T, Saavedra JM (2000) Angiotensin II AT (1) blockade normalizes cerebrovascular autoregulation and reduces cerebral ischemia in spontaneously hypertensive rats. Stroke 31:2478–2486
Culman J, Baulmann J, Blume A, Unger T (2001) The renin-angiotensin system in the brain: an update. J Renin Angiotensin Aldosterone Syst 2:96–102
Iadecola C, Gorelick PB (2004) Hypertension, angiotensin, and stroke: beyond blood pressure. Stroke 35:348–350
Chalupsky K, Cai H (2005) Endothelial dihydrofolate reductase: critical for nitric oxide bioavailability and role in angiotensin II uncoupling of endothelial nitric oxide synthase. Proc Natl Acad Sci USA 102:9056–9061
Ando H, Zhou J, Macova M, Imboden H, Saavedra JM (2004) Angiotensin II AT1 receptor blockade reverses pathological hypertrophy and inflammation in brain microvessels of spontaneously hypertensive rats. Stroke 35:1726–1731
Ito T, Yamakawa H, Bregonzio C, Terron JA, Falcon-Neri A, Saavedra JM (2002) Protection against ischemia and improvement of cerebral blood flow in genetically hypertensive rats by chronic pretreatment with an angiotensin II AT1 antagonist. Stroke 33:2297–2303
Zhang N, Komine-Kobayashi M, Tanaka R, Liu M, Mizuno Y, Urabe T (2005) Edaravone reduces early accumulation of oxidative products and sequential inflammatory responses after transient focal ischemia in mice brain. Stroke 36:2220–2225
Abe K, Yuki S, Kogure K (1988) Strong attenuation of ischemic and postischemic brain edema in rats by a novel free radical scavenger. Stroke 19:480–485
Uno M, Kitazato KT, Suzue A, Matsuzaki K, Harada M, Itabe H, Nagahiro S (2005) Inhibition of brain damage by edaravone, a free radical scavenger, can be monitored by plasma biomarkers that detect oxidative and astrocyte damage in patients with acute cerebral infarction. Free Radic Biol Med 39:1109–1116
Yamamoto T, Yuki S, Watanabe T, Mitsuka M, Saito KI, Kogure K (1997) Delayed neuronal death prevented by inhibition of increased hydroxyl radical formation in a transient cerebral ischemia. Brain Res 762:240–242
Kim YJ, Hwang SY, Oh ES, Oh S, Han IO (2006) IL-1beta, an immediate early protein secreted by activated microglia, induces iNOS/NO in C6 astrocytoma cells through p38 MAPK and NF-kappaB pathways. J Neurosci Res 84:1037–1046
Tse AK, Wan CK, Shen XL, Yang M, Fong WF (2005) Honokiol inhibits TNF-alpha-stimulated NF-kappaB activation and NF-kappaB-regulated gene expression through suppression of IKK activation. Biochem Pharmacol 70:1443–1457
Acknowledgments
This study is supported by the National Natural Science Research Grants of China No. 30900778 (J J Li) and 31260254 (CY Wu).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, CY., Zha, H., Xia, QQ. et al. Expression of angiotensin II and its receptors in activated microglia in experimentally induced cerebral ischemia in the adult rats. Mol Cell Biochem 382, 47–58 (2013). https://doi.org/10.1007/s11010-013-1717-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-013-1717-4