Abstract
Chronic hepatitis B virus infection is the dominant global cause of hepatocellular carcinoma (HCC), especially hepatitis B virus-X (HBx) plays a major role in this process. HBx protein promotes cell cycle progression, inactivates negative growth regulators, and binds to and inhibits the expression of p53 tumor suppressor gene and other tumor suppressor genes and senescence-related factors. However, the relationship between HBx and autophagy during the HCC development is poorly known. Previous studies found that autophagy functions as a survival mechanism in liver cancer cells. We suggest that autophagy plays a possible role in the pathogenesis of HBx-induced HCC. The present study showed that HBx transfection brought about an increase in the formation of autophagosomes and autolysosomes. Microtubule-associated protein light chain 3, Beclin 1, and lysosome-associated membrane protein 2a were up-regulated after HBx transfection. HBx-induced increase in the autophagic level was increased by mTOR inhibitor rapamycin and was blocked by treatment with the PI3K–Akt inhibitor LY294002. The same results can also be found in HepG2.2.15 cells. These results suggest that HBx activates the autophagic lysosome pathway in HepG-2 cells through the PI3K–Akt–mTOR pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the third leading cause of cancer death worldwide. Surgery with curative intent is feasible for only 15–25 % of patients, and most patients die from locally advanced or metastatic diseases in a relatively short period of time. To date, cytotoxic chemotherapy has not been a standard treatment for HCC. Recently, molecular-targeted therapy, which acts on specific dysregulated signal transduction pathways, has shown promise as a treatment for advanced HCC. Development of novel agents to enhance the effectiveness of treatment is mandatory.
It is estimated that there are 350 million people chronically infected with hepatitis B virus (HBV), which is significantly associated with development of HCC, one of the most common forms of cancer worldwide [1–3].
The HBV genome contains four open reading frames, encoding the viral envelope proteins (also known as surface antigens), the viral core protein which comprises the viral capsid, a polymerase/reverse transcriptase, and the nonstructural regulatory protein known as hepatitis B virus-X (HBx). HBx gene is the smallest of the four partially overlapping open reading frames of HBV. It comprises 452 nucleotides that encode a 154-amino acid regulatory protein with a molecular mass of 17 kDa [4, 5]. HBx, known as a multifunctional protein, is involved in the activation of a wide variety of different enhancer/promoter functions by direct or indirect interactions with transcription factors, activation of signal transduction pathways, sensitization of cells to apoptosis, loss of cell cycle checkpoints, induction of cell growth arrest, and modulation of proteolytic degradation pathways in cells [6–10]. Circumstantial evidence also suggests that it may play roles directly or indirectly in the genesis of hepatocellular carcinoma. HBx is, therefore, an essential viral protein with pleiotropic activity that might act directly or indirectly in the development of hepatocellular carcinoma during chronic hepadnavirus infection.
Autophagy is an evolutionarily conserved catabolic pathway where cells deliver their own cytoplasmic material and/or organelles to lysosomes for degradation [11]. It is linked to many diseases and is required for normal development. Macroautophagy (here referred to as autophagy) has been proposed to involve in clearing unfolded protein away under certain stress conditions. Under normal growth conditions, a housekeeping level of autophagy exists. Under stress, such as nutrient starvation, autophagy is strongly induced resulting in the engulfment of cytosolic components and organelles in specialized double-membrane structures termed autophagosomes. Autophagy is controlled by the highly conserved atg genes (for autophagy-related genes). Two protein conjugation systems are necessary for autophagosome formation, that is, the Atg12-Atg5 and Atg8-phosphatidyl ethanolamine conjugation systems [12]. Atg12-Atg5 assists the formation and elongation of phagophores and autophagosomes, but dissociates from the membranes once the autophagosome is completed. Atg8, called LC3 in mammals, also assists autophagosome formation, possibly by enhancing membrane fusion. Recent work has implicated autophagy in many disease pathologies, including cancer.
Autophagy or autophagic cell death, also known as type II programmed cell death, is shown to be prevented in the presence of either autophagic inhibitors or reduced expression of the ATG gene. Apoptosis also plays an important role for the living to clear excess, corrupted, and virus-infected cells. The relationship between autophagy and apoptosis is complex and varies between the cell types and the stress distinction. On occasion, autophagy and apoptosis occur instantaneously after stress; at other times, only autophagy or apoptosis is observed. The mechanisms responsible for autophagy are still not very clear [13].
Whether autophagy is a protective mechanism or a mechanism of cell death in the response of tumor cells to anticancer therapy remains unclear. There is still no direct evidence to support a role for autophagy in the HBx-induced HCC. Here, we hypothesized that autophagy in HepG2 cells is activated by HBx, and such activation is via PI3K–Akt–mTOR pathway.
In this study, we investigated the expression change of Beclin 1, LC3I, LC3II, and lamp2a, and also observed ultrastructural changes in both normal HepG2 cells and HBx transfected HepG2 cells using rapamycin or LY294002 or none. The results suggest that HBx enhances autophagy in HepG2 cells, and this autophagy is regulated through PI3K–Akt–mTOR pathway.
Materials and methods
Cancer cell culture
The HepG2 cell line was obtained from the Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China) and cultured in RPMI 1640 medium supplemented with 10 % fetal calf serum (Gibco BRL, Gaithersburg, MD, USA), 2 mmol/L glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin at 37 °C in humidified 5 % CO2.
Stable transfection
HepG2 cells were transfected with pCMV-hbxip8 or pCMV-tag2B (empty vector) with Lipofectamine 2000 according to the manufacturer’s instructions. Twenty-four hours after transfection, the cells were diluted 1:10 and cultured in growth medium containing G418 (700 μg/mL) for 3 weeks. Stable transfected clones were picked and maintained in a medium containing 350 μg/mL G418 for additional studies.
Transmission electron microscopy (TEM)
Cells were fixed for TEM by removing culture medium, washing three times in PBS (pH 7.4), and adding 2.5 % PBS-buffered glutaraldehyde at 4 °C for 1 h, postfixation in 1 % OsO4 for another hour, dehydration in a graded ethanol series, and flat embedding in Araldite. Ultrathin sections (40–60 nm) were placed on grids (200 mesh), and double-stained with uranyl acetate and lead citrate. The grids containing the sections were observed on a Philips CM-120 electron microscope.
Western blotting
The MAP1-LC3, beclin 1, lamp2a, and GAPDH proteins were detected with the antibodies rabbit polyclonal anti-MAP-LC3, rabbit polyclonal anti-beclin 1, rabbit polyclonal anti-lamp2a, and rabbit polyclonal anti-GAPDH (Santa Cruz Biotechnology, Europe). Protein concentration was determined using a BCA kit (Pierce, Rockford, IL). Thirty micrograms of protein from the homogenized sample was mixed 1:4 with loading buffer, separated by 10 % SDS–PAGE, and transferred to a nitrocellulose membrane. After blocking the non-specific binding sites with 5 % milk powder, the membrane was treated with the first antibodies at 4 °C overnight, then washed and incubated for 2 h with horseradish peroxidase-conjugated rabbit anti-goat antibody, goat anti-rabbit IgG, and rabbit anti-mouse antibody (Vector Laboratories, Burlingame, CA) in TBST containing 3 % nonfat dry milk. Densitometry of bands representing protein expression was done using Sigma Scan Pro5 software. For each immunoblot, the band intensity of each lane was normalized relative to the loading control GAPDH.
Statistical analysis
All experiments were repeated at least three times. The numerical data were presented as mean ± SD. Data was analyzed using the two-tailed t test. A P value less than 0.05 was considered statistically significant.
Results
HBx-induced autophagy in HepG2 cells
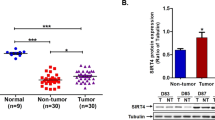
Since formation of autophagosomes is by far the most important morphological feature of autophagic cells, observation of the double-membrane vesicle intracellular remains currently the gold standard to detect autophagy [14]. Ultrastructural changes in cells were examined with transmission electron microscope after HBx transfection. TEM images showing normal nucleus, chromatin, cytoplasm, and mitochondria in control HepG-2 cells, with few or no autophagosomes were observed (Fig. 1A-a). In contrast, the TEM images displayed many autophagosomes at various developmental stages in stable HBx-transfected HepG-2 cells (Fig. 1A-b). Autophagosomes are derived from isolated membranes that, possibly, originated from ribosome-free endoplasmic reticulum. These isolated membranes elongate and curve at both ends to form C-shaped structures and double-membrane vacuoles [15]. In Fig. 1A-b, the photo showed typical C-shaped double-membrane structures, double-membrane autophagosomes, and lysosomes fusing with autophagosomes (indicated by arrows). LC3-II and beclin 1 are also two well-known markers of autophagy. When HepG-2 cells were stable after HBx transfection, we confirmed that LC3-II and beclin 1 expression were significantly up-regulated (Fig. 1B-a,b). In addition, we examined another marker of autophagy—lamp2a. The data showed that lamp2a expression was also significantly up-regulated (Fig. 1B-c). These data indicated that HBx enhances autophagy in HepG-2 cells.
HBx-induced autophagy in HepG2 cells. A Increased signs of autophagy in HepG2 cells after HBx transfection. Typical autophagosomes with the characteristic double membrane are noted (arrows). B Western blot analysis revealed that LC3I, LC3-II, lamp2a, and beclin 1 protein expression were up-regulated after HBx transfection, which indicated HBx-induced autophagy in HepG2 cells. Upper panels show examples of protein levels from western blots; lower panels show statistics of optical density measurements. GAPDH expression was used as a reference, and data are mean ± SD. t test demonstrated significant difference (*P < 0.05, n = 3), compared with control group. Scale bars 5 µm
HBx enhanced the expression of mTOR and PI3K/Akt in HepG-2 cells
The regulation of autophagy is complex, in which PI3K–Akt–mTOR is a major pathway. We examined the expression of mTOR and PI3K/Akt after HBx transfection.
The data confirmed our suspicion that mTOR and PI3K/Akt expression were significantly up-regulated after HBx transfection in HepG2 cells (Fig. 2). These results suggest that the autophagy induced by HBx is regulated via PI3K–Akt–mTOR pathway.
HBx enhanced the expression of mTOR and PI3K/Akt in HepG-2 cells. Western blot analysis showed that mTOR, PI3K, and Akt expression were up-regulated after HBx transfection. Upper panels show examples of protein levels from western blots; lower panels show statistics of optical density measurements. Data are mean ± SD. t test demonstrated significant difference (*P < 0.05, n = 3), compared with control group. Scale bars 5 µm
The activation of autophagy induced by HBx is increased, but the expression of mTOR is decreased by rapamycin treatment
In order to investigate the enhanced autophagy induced by HBx either through activating mTOR or activating PI3K–Akt, we first selected rapamycin treatment. Rapamycin is a widely used inhibitor of mTOR. Ultrastructural changes in cells and the LC3I, LC3II levels after rapamycin treatment have been observed. The photo showed that few or no autophagosomes were observed (Fig. 3A-a). After rapamycin treatment, there are some autophagosomes in the control cells (Fig. 3A-b) (indicated by arrows), but less than in HBx transfected cells (Fig. 3A-c, d) (indicated by arrows). There are much more double-membrane structures, double-membrane autophagosomes, and lysosomes fusing with autophagosomes after rapamycin treatment in HBx transfected cells (indicated by arrows). We found that LC3I and LC3II expression were significantly up-regulated after rapamycin treatment. LC3II/LC3I is also up-regulated after rapamycin treatment (Fig. 3B). We observed that the level of mTOR was significantly down-regulated after rapamycin treatment. This result suggests that the enhanced autophagy induced by HBx was through activating mTOR.
The activation of autophagy induced by HBx is increased by rapamycin treatment, the level of mTOR is decreased. A After rapamycin treatment (10 nM), some autophagosomes are observed in control groups (b) (arrows), but less than in HBx transfected cells (c, d) (arrows). Much more double-membrane structures, double-membrane autophagosomes, and lysosomes fusing with autophagosomes after rapamycin treatment in HBx transfected cells (d) (arrows). B Western blot analysis revealed that LC3I and LC3-II expression were up-regulated after rapamycin treatment both in control groups and HBx transfected groups. The mTOR expression was down-regulated after rapamycin treatment in HBx transfected groups. Upper panels show examples of protein levels from western blots; lower panels show statistics of optical density measurements. GAPDH expression was used as a reference, and data are mean ± SD. t test demonstrated significant difference (*P < 0.05, n = 3), compared with control group (#P < 0.05, n = 3), compared with rapamycin treatment. Scale bars 5 µm
The activation of autophagy and p-Akt/Akt induced by HBx is decreased by LY294002 treatment
We then assessed the effects of LY294002, a well-known inhibitor of PI3K/Akt. Same as rapamycin, we observed the ultrastructural changes in cells and the LC3I and LC3II levels after LY294002 treatment. The microscopic images indicated that there are few or no autophagosomes in control cells both before and after LY294002 treatment (Fig. 4A-a, b), while fewer autophagosomes were observed in HBx transfected cells after LY294002 treatment (Fig. 4A-c, d). The data showed that LC3I and LC3II expression were significantly down-regulated after Rapamycin treatment. LC3II/LC3I is also down-regulated after Rapamycin treatment (Fig. 3B). We found that the level of p-Akt/Akt was significantly down-regulated after LY294002 treatment. This result suggests that the enhanced autophagy induced by HBx was through activating PI3K–Akt–mTOR pathway.
The activation of autophagy and p-Akt/Akt induced by HBx is decreased by LY294002 treatment. A After LY294002 treatment(50 μm); few or no autophagosomes were observed in control cells both before and after LY294002 treatment (a, b) (arrows). Fewer double-membrane structures, double-membrane autophagosomes, and lysosomes fusing with autophagosomes after LY294002 treatment in HBx transfected cells (c, d) (arrows). B Western blot analysis revealed that LC3I and LC3-II expression were down-regulated after LY294002 treatment in HBx transfected groups. The level of p-Akt/Akt was down-regulated after rapamycin treatment in HBx transfected groups. Upper panels show examples of protein levels from western blots; lower panels show statistics of optical density measurements. GAPDH expression was used as a reference, and data are mean ± SD. t test demonstrated significant difference (*P < 0.05, n = 3), compared with control group. (#P < 0.05, n = 3), compared with rapamycin treatment. Scale bars 5 µm
The expression of LC3I, LC3II, mTOR, and PI3K/Akt were higher in HepG2.2.15 cells. This activation of LC3I and LC3II was increased by rapamycin treatment and decreased by LY294002 treatment
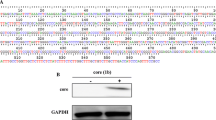
HepG2.2.15, however, is a well-established version of the HepG2 cell line that constitutively expresses HBV. These cells support full replication of HBV and secrete hepatitis B surface antigen (HBsAg), hepatitis B e antigen (HBeAg), and virions into the culture medium [16]. Therefore, comparative analysis of HepG2.2.15 and HepG2 may provide valuable clues for understanding the activation of autophagy induced by HBx. We examined the expression of LC3-II/LC3-I, mTOR, and PI3K/Akt in HepG2.2.15 cells, and observed the changes of LC3I and LC3II levels after rapamycin and LY294002 treatment. we confirmed that the level of LC3-II/LC3-I and the expression of mTOR, PI3K, and Akt were significantly up-regulated (Fig. 5A). This activation is increased by rapamycin treatment (Fig. 5B) and decreased by LY294002 treatment (Fig. 5C). These results were the same as that of HepG2 cells. So we believed that HepG2 cells transfected by HBx have the same biological activity as HepG2.2.15 cells.
The expression of LC3I, LC3II, mTOR, and PI3K/Akt were higher in HepG2.2.15 cells. This activation of LC3I and LC3II were increased by rapamycin treatment and decreased by LY294002 treatment. Western blot analysis revealed that LC3I, LC3-II, mTOR, p-AKt, and AKt expression were higher than the control in HepG2.2.15 cells (A), which indicated that the activation of autophagy was higher in HepG2.2.15 cells. This higher activation of LC3I and LC3II were increased by rapamycin treatment (B) and decreased by LY294002 treatment (C). These results were the same as that of HepG2 cells. So we believed that HepG2 cells transfected by HBx have the same biological activity as HepG2.2.15 cells
Discussion
Chronic hepatitis B virus (HBV) infection is the dominant global cause of HCC, accounting for 55 % of cases worldwide, the highest incidence regions of the tumor. HBV DNA is integrated into the chromosomal DNA of hepatocytes in the great majority of patients with HBV-induced HCC, and this is believed to play a pivotal role in the pathogenesis of the tumor by either promoting cell survival [17] or inducing cell death [18, 19]. The mechanisms by which HBV infection results are still unclear.
Previous research suggests that HBx affects a variety of cellular processes, including gene transcription, cell cycle progression, DNA damage repair, cell proliferation, and apoptosis. It has been shown that cytoplasmic HBx activates the Ras–Raf MAPK signaling pathway, which is essential for HBV gene expression and transformation of differentiated Hepatocytes [20, 21]. HBx contributes to the transcriptional regulation of matrix metallopeptidase 9 through the ERK and PI3K–Akt/PKB pathway, and increases the invasive potential of cells [22]. In addition, the proliferation of HepG2 cells promoted by hepatitis B X-interacting protein (HBXIP) is associated with activation of the PI3K/Akt signaling pathway [23]. Several groups reported that HBx was capable of inhibiting cell apoptosis. HBx could up-regulate surviving expression in hepatoma tissues [24]. HBx in liver cells down-regulate the expression of PTEN and activated Akt, and HBx has an effect on the p53-mediated transcription of PTEN, which, in turn, is associated with tumor suppression [25]. In contrast, it has been reported that HBx interacts with various cellular signaling factors to enhance apoptosis by interacting with cellular signaling proteins such as c-FLIP [26] and Hsp60 [27].
Cancer cells have an antioxidant system where antioxidant enzymes such as manganese-superoxide dismutase (SOD), catalase, and glutathione peroxidase eliminate ROS [28]. Chen et al. [29] recently reported that oxidative stress induced by H2O2 or SOD inhibitor 2-methoxyestradiol (2-ME) can cause autophagic cell death in transformed cell line HEK293, and cancer cell lines U87 and HeLa. Oxidative stress induced by VPA occurs upstream of autophagy in glioma cell lines [30].
Autophagy plays a dual role in cancer: on the one hand, autophagy is a tumor suppressor [31–34]; on the other hand, it is a tumor promoter [35–37].
Since normal hepatocytes are not sensitive to autophagy, the observed effect of autophagy on HBV-induced hepatitis may be due to the altered sensitivity of HBV-infected cells. In order to test this theory, we transfected a widely used human hepatoma cell line HepG-2 plasmids that carry the HBV X gene (HBx). In the present study, we demonstrated that Beclin 1, LC3II/LC3I, and lamp2a expression were up-regulated by HBx transfection in HepG2 cells. More double-membrane structures and double-membrane autophagosomes were observed in HBx transfected HepG2 cells. In conclusion, HBx enhances the level of autophagy in HepG2 cells.
There are extensive molecular interactions that occur between these gene products in the early stages of autophagosome formation. The most well-known mechanism is that of the class I phosphoinositol-3-kinase (PI3K) pathway, which initiates an upstream signaling cascade to regulate the activity of the mammalian target of rapamycin (mTOR), a kinase, which is a major regulatory anabolic protein, and a suppressor of autophagy. The mammalian TOR (mTOR) includes the HEAT repeat sequence, the FAT domain, the FRB kinase domain, and the NRD and the FATC domain. Rapamycin can bind with the FKBP12–rapamycin to form FKBP–rapamycin complex, then activate the dephosphorylation of Atg13, which is a central regulatory protein in numerous processes of cell metabolism including cell growth, proliferation, and survival under both physiological and pathological conditions, many experimental data show that autophagy is regulated by the mTOR pathway [38–40]. Although the exact mechanism of how mTOR regulates autophagy remains unclear, it has been reported that the activation of mTOR leads to inhibition of Atg1, a key signal in autophagy induction, thus inhibiting the binding affinity of Atg13 with Atg1 to form a complex which signals the induction of autophagy [41]. mTOR plays a role in down-regulation of the process of autophagy. In addition, multiple crucial factors in the mTOR pathway are closely related to cancer. As such, mTOR may be exploited to investigate the relation between cancer and autophagy.
Here, we have provided evidence that the expression of mTOR, PI3K, and Akt were increased by HBx transfection. Furthermore, we used rapamycin (mTOR inhibitor) and LY294002 (PI3K/Akt inhibitor) to verify that the autophagy induced by HBx transfection in HepG-2 cells was regulated through PI3K/Akt/mTOR pathway.
As mTOR is a down-regulator of autophagy, the inhibitor of mTOR always activates autophagy through mTOR pathway. In the upstream of mTOR, multiple mTOR activators are oncogenes, which suppress autophagy through the activation of mTOR. One of the upstream pathway which is responsible for the activation of mTOR is the phosphoinositide-3-kinase (PI3K/Akt) cell survival pathway [42, 43]. Recently, data show that PI3K/Akt has been confirmed to bring about stimulation of mTOR function. Activated PI3K/Akt effect on mTOR activity is mediated by Akt kinase inhibitory phosphorylation of the tumor suppressor tuberous sclerosis complex 1/2 [44].
The present study demonstrated that mTOR inhibitor rapamycin can increase the expression of LC3II/LC3I induced by HBx transfection in HepG-2 cells, and this expression can be inhibited by PI3K/Akt inhibitor LY294002. These data further confirmed that the autophagy induced by HBx transfection in HepG-2 cells was regulated through PI3K/Akt/mTOR pathway. But which site is the key site on this pathway during the regulation of autophagy is still unknown.
References
Bosch FX, Ribes J, Diaz M, Cleries R (2004) Primary liver cancer: worldwide incidence and trends. Gastroenterology 127(5 Suppl 1):S5–S16
Parkin DM, Bray FI, Devesa SS (2001) Cancer burden in the year 2000, The global picture. Eur J Cancer 37 (Suppl 8):S4–S66
Montalto G, Cervello M, Giannitrapani L, Dantona F, Terranova A, Castagnetta LA (2002) Epidemiology, risk factors, and natural history of hepatocellular carcinoma. Ann NY Acad Sci 963:13–20
Seeger C, Mason WS (2000) Hepatitis B virus biology. Microbiol Mol Biol Rev 1:51–68
Tang H, Oishi N, Kaneko S, Murakami S (2006) Molecular functions and biological roles of hepatitis B virus x protein. Cancer Sci 10:977–983
Diao J, Khine AA, Sarangi F, Hsu E, Iorio C, Tibbles LA et al (2001) X protein of hepatitis B virus inhibits Fas-mediated apoptosis and is associated with up-regulation of the SAPK/JNK pathway. J Biol Chem 11:8328–8340
Kim JY, Song EH, Lee HJ, Oh YK, Choi KH, Yu DY et al (2010) HBx-induced hepatic steatosis and apoptosis are regulated by TNFR1 and NF-jB-dependent pathway. J Mol Biol 4:917–931
Pan J, Duan LX, Sun BS, Feitelson MA (2001) Hepatitis B virus X protein protects against anti-Fas-mediated apoptosis in human liver cells by inducing NF-kappa B. J Gen Virol 82:171–182
Lara-Pezzi E, Armesilla AL, Majano PL, Redondo JM, Lopez-Cabrera M (1998) The hepatitis B virus X protein activates nuclear factor of activated T cells (NF-AT) by a cyclosporin A-sensitive pathway. EMBO J 23:7066–7077
Gearhart TL, Bouchard MJ (2010) The hepatitis B virus X protein modulates hepatocyte proliferation pathways to stimulate viral replication. J Virol 6:2675–2686
Ravikumar B, Futter M, Jahreiss L, Korolchuk VI, Lichtenberg M, Luo S et al (2009) Mammalian macroautophagy at a glance. J Cell Sci 122:1707–1711
Ohsumi Y (2001) Molecular dissection of autophagy: two ubiquitinlike systems. Nat Rev Mol Cell Biol 2:211–216
Lockshin RA, Zakeri Z (2004) Apoptosis, autophagy, and more. J Biochem Cell Biol 36:2405–2419
Eskelinen EL (2008) To be or not to be? Examples of incorrect identification of autophagic compartments in conventional transmission electron microscopy of mammalian cells. Autophagy 4:257–260
Wang Y, Hang R, Liang ZQ, Wu JC, Zhang XD, Gu ZL et al (2008) An autophagic mechanism is involved in apoptotic death of rat striatal neurons induced by the non-N-methyl-D-aspartate receptor agonist kainic acid. Autophagy 4:214–226
Pan J, Duan LX, Sun BS (2001) Hepatitis B virus X protein protects against anti-Fas-mediated apoptosis in human liver cells by inducing NF-kappa B. J Gen Virol 82:171–182
Diao J, Khine AA, Sarangi F (2001) X protein of hepatitis B virus inhibits Fasmediated apoptosis and is associated with up-regulation of the SAPK/JNK pathway. J Biol Chem 276:8328–8340
Wang WH, Gregori G, Hullinger RL (2004) Sustained activation of p38 mitogen-activated protein kinase and c-Jun N-terminal kinase pathways by hepatitis B virus X protein mediates apoptosis via induction of Fas/FasL and tumor necrosis factor (TNF) receptor 1/TNF-alpha expression. Mol Cell Biol 24:10352–10365
Chirillo P, Pagano S, Natoli G (1997) The hepatitis B virus X gene induces p53-mediated programmed cell death. Proc Natl Acad Sci USA 94:8162–8167
Stöckl L, Berting A, Malkowski B, Foerste R, Hofschneider PH, Hildt E (2003) Integrity of c-Raf-1/MEK signal transduction cascade is essential for hepatitis B virus gene expression. Oncogene 22:2604–2610
Tarn C, Lee S, Hu Y, Ashendel C, Andrisani OM (2001) Hepatitis B virus X protein differentially activates RAS-RAF-MAPK and JNK pathways in X-transforming versus non-transforming AML12 hepatocytes. J Biol Chem 276:34671–34680
Chung TW, Lee YC, Kim CH (2004) Hepatitis B viral HBx induces matrix metalloproteinase-9 gene expression through activation of ERK and PI-3K/AKT pathways: involvement of invasive potential. FASEB J 18:1123–1125
Wang FZ, Fei HR, Lian LH, Wang JM, Qiu YY (2011) Hepatitis B x-interacting protein induces HepG2 cell proliferation through activation of the phosphatidylinositol 3-kinase/Akt pathway. Exp Biol Med 236:62–69
Zhang X, Dong N, Yin L, Cai N, Ma H, You J, Ye L et al (2005) Hepatitis B virus X protein upregulates survivin expression in hepatoma tissues. J Med Virol 77:374–381
Chung TW, Lee YC, Ko JH, Kim CH (2003) Hepatitis B virus X protein modulates the expression of PTEN by inhibiting the function of p53, a transcriptional activator in liver cells. Cancer Res 63:3453–3458
Kim KH, Seong BL (2003) Pro-apoptotic function of HBV X protein is mediated by interaction with c-FLIP and enhancement of death-inducing signal. EMBO J 22:2104–2116
Satoh T, Enokido Y, Aoshima H, Uchiyama Y, Hatanaka H (1997) Changes in mitochondrial membrane potential during oxidative stress-induced apoptosis in PC12 cells. J Neurosci Res 50:413–420
Scherz-Shouval R, Elazar Z (2007) ROS, mitochondria and the regulation of autophagy. Trends Cell Biol 17:422–427
Chen Y, McMillan-Ward E, Kong J et al (2008) Oxidative stress induces autophagic cell death independent of apoptosis in transformed and cancer cells. Cell Death Differ 15:171–182
Jun Fu Shao CJ, Chen FR, Ng HK, Chen ZP (2010) Autophagy induced by valproic acid is associated with oxidative stress in glioma cell lines. Neuro-Oncology 12(4):328–340
Qu X, Yu J, Bhagat G, Furuya N, Hibshoosh H, Troxel A et al (2003) Promotion of tumorigenesis by heterozygous disruption of the beclin 1 autophagy gene. J Clin Invest 112:1809–1820
Chen N, Debnath J (2010) Autophagy and tumorigenesis. FEBS Lett 584:1427–1435
Mathew R, Karp CM, Beaudoin B, Vuong N, Chen G, Chen HY et al (2009) Autophagy suppresses tumorigenesis through elimination of p62. Cell 137:1062–1075
Young AR, Narita M, Ferreira M, Kirschner K, Sadaie M, Darot JF et al (2009) Autophagy mediates the mitotic senescence transition. Genes Dev 23:798–803
Yoo BH, Wu X, Derouet M, Haniff M, Eskelinen EL, Rosen K (2009) Hypoxia-induced downregulation of autophagy mediator Beclin 1 reduces the susceptibility of malignant intestinal epithelial cells to hypoxia-dependent apoptosis. Autophagy 5:1166–1179
Turcotte S, Chan DA, Sutphin PD, Hay MP, Denny WA, Giaccia AJ (2008) A molecule targeting VHL-deficient renal cell carcinoma that induces autophagy. Cancer Cell 14:90–102
Fung C, Lock R, Gao S, Salas E, Debnath J (2008) Induction of autophagy during extracellular matrix detachment promotes cell survival. Mol Biol Cell 19:797–806
Guertin DA, Sabatini DM (2007) Defining the role of mTOR in cancer. Cancer Cell 12:9–22
Noda T, Ohsumi Y (1998) Tor, a phosphatidylinositol kinase homologue, controls autophagy in yeast. J Biol Chem 273:3963–3966
Scott RC, Schuldiner O, Neufeld TP (2004) Role and regulation of starvation-induced autophagy in the Drosophila fat body. Dev Cell 7:167–178
Kamada Y, Funakoshi T, Shintani T, Nagano K, Ohsumi M, Ohsumi Y (2000) Tor- mediated induction of autophagy via an Apg1 protein kinase complex. J Cell Biol 150:1507–1513
Sarbassov DD, Guertin DA, Ali SM, Sabatini DM (2005) Phosphorylation and regulation of Akt/PKB by the rictor–mTOR complex. Science 307:1098–1101
Meley D, Bauvy C, Houben-Weerts JH, Dubbelhuis PF, Helmond MT, Codogno P et al (2006) AMP-activated protein kinase and the regulation of autophagic proteolysis. J Biol Chem 281:34870–34879
Inoki K, Li Y, Zhu T, Wu J, Guan KL (2002) TSC2 is phosphorylated and inhibited by Akt and suppresses mTOR signaling. Nat Cell Biol 4:648–657
Acknowledgments
The authors thank Prof. Shuang-ping Guo for providing the plasmids. We also thank Tao Tao for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, P., Guo, Qs., Wang, Zw. et al. HBx induces HepG-2 cells autophagy through PI3K/Akt–mTOR pathway. Mol Cell Biochem 372, 161–168 (2013). https://doi.org/10.1007/s11010-012-1457-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-012-1457-x