Abstract
There is a clear relationship between the pelvic floor muscles and urinary systems, which relates to urgency, frequency, incontinence, pelvic pain, and bowel complaints. The specific mechanisms which relate these two systems are not clear. Improved understanding of the relation between the pelvic floor muscles and bladder function is clinically relevant in establishing effective treatments to such problems as incontinence, secondary to birth. The following tissues were collected from normal adult female rabbits: pubococcygeus (Pc) and ischiocavernosus/bulbospongiosus (Ic/Bs) pelvic floor muscles. Bladder body muscle and mucosa, bladder base muscle and mucosa, and leg skeletal muscle were also collected. The following enzymatic assays were performed on each tissue: citrate synthase (CS), sarcoplasmic–endoplasmic reticular ATPase (SERCA), and choline acetyltransferase (ChAT). CS and SERCA activities were significantly higher in the Pc compared with the Ic/Bs pelvic floor muscles, whereas the ChAT activity of the Ic/Bs was higher than that of the Pc muscle. Based on our results, the Pc muscle is expected to have a significantly greater capacity to contract and a higher metabolic activity than those of the Ic/Bs muscles. We believe that an understanding of the biochemical activities of these three biomarker enzymes in normal pelvic floor muscles is essential in evaluating the effects of specific experimental dysfunctions created in pelvic floor muscle activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An emerging body of research supports a relationship between the pelvic floor muscles and urinary systems, manifested as urgency, frequency, incontinence, pelvic pain, and bowel complaints [1–5]. It is clear that pelvic floor exercises are effective in the treatment of a variety of lower urinary tract dysfunctions including urge, stress, and postpartum incontinence [6–9]. While the association between excessive tightening or weakness of the pelvic floor muscles and lower urinary tract systems is being atempted to be described in the clinical literature [10], the specific mechanisms and pathways remain elusive [11]. Improved understanding of the relation between the pelvic floor muscles and bladder function is clinically relevant in tailoring the treatment of these patients. Pelvic floor muscles offer a therapeutic target beyond currently employed therapies for the bladder, and an improvement in understanding their biochemical properties could lead to directed local treatment, such as biofeedback, pelvic floor physical therapy, injections, or vaginally delivered medical therapies. In the case of obstructive bladder dysfunction in males (men and rabbit models of partial outlet obstruction), we have demonstrated that there is a direct correlation between contractile dysfunctions associated with obstructive uropathy and specific dysfunctions, in three subcellular organelles: mitochondria, sarcoplasmic reticulum, and the cholinergic synapse. We use three biomarker enzymes for identification of the level of dysfunction: citrate synthase (CS) as a marker for mitochondrial function; sarco-endoplasmic reticular calcium ATPase (SERCA) as a marker for calcium mobilization and storage; and choline acetyltransferase (ChAT) as a marker enzyme for cholinergic synapses [12–15].
In the study of the relationship between the pelvic floor muscles and the muscles of the lower urinary tract, it is important to develop a relevant animal model. Rodents, the most commonly used laboratory animal models, lack a well-defined pelvic floor [16]. The female rabbit, in contrast, has well-defined posterior pubococcygeus (Pc) muscles (homolog to the pelvic floor support in the human) and anterior bulbospongiosus/ischiocavernosus/(Bs/Ic) muscles (homolog to the perineal musculature in humans). A recently published study of micturition in a female rabbit model supported the role of both of these pelvic floor muscles in micturition [17].
Before establishing specific pathologies of the pelvic floor by means of our rabbit model, it is important to understand the characteristics of the normal pelvic floor muscles in comparison with the muscle of the lower urinary tract. Our current study examines the biochemical properties of the two specific rabbit pelvic floor muscles compared to the bladder (body muscle, mucosa, and bladder base muscle and mucosa) and skeletal leg muscle. We compared the three enzymes identified above as important biomarkers of lower urinary tract dysfunction in both male and female rabbits, and in men.
The following are the characteristics of the biochemical markers that were examined:
-
(1)
Citrate synthase (CS) for mitochondrial function. The mitochondrion is an organelle that is located in every living cell and is responsible for oxidative phosphorylation, which generates adenosine triphospate (ATP) [18–20].
-
(2)
SERCA for sarcoplasmic reticular (SR) function. The sarcoplasmic reticulum is a structure in muscle cells, which assists with muscle contraction and relaxation by releasing and storing calcium ions. SERCA is a specific form of calcium ATPase localized in the membrane of the SR of muscle cells, which is responsible for moving calcium out of the cytosol and into storage sites within the SR. [21–23].
-
(3)
ChAt which is responsible for synthesizing acetylcholine, primarily in cholinergic neuronal synapses [24, 25]. Acetylcholine is important for postsynaptic neurotransmission for both the parasympathetic autonomic nervous system, and for all the skeletal muscles. It is also an important neurotransmitter at both cholinergic and adrenergic presynaptic neurons. Acetylcholine reacts with two different receptors: muscarinic receptors localized on smooth and cardiac muscles, and nicotinic receptors localized on skeletal muscles.
The specific aim of this study was to compare the normal activities of these three specific biomarker enzymes between the pelvic floor muscles and those of the lower urinary tract before the development of specific pelvic floor dysfunctions.
Methods
All methods were approved by the Institutional Animal Care and Use Committee of the Stratton VA Medical Center, Albany, NY, USA.
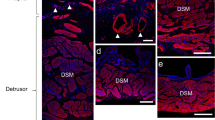
Tissues were surgically extracted from five normal adult female rabbits under anesthetic (isoflurane 1–3 %) during non-survival surgery. The pelvic floor tissues collected were: Pc and Ic/Bs. In brief, after midline incision, the IcBs complex was separated from its insertion on the caudal border of the ischiatic arc to their distal tendons. After separation of the pubic symphysis, the Pc muscle on each side was isolated from the medial surface of the innominate bone to insertion on sacral vertebrae. The bladder was harvested and divided into (1) body smooth muscle (2) body mucosa, and (3) bladder base smooth muscle. Skeletal muscle from the leg was also collected. Each tissue was frozen under liquid nitrogen and stored at −80 °C.
CS [26]
Frozen tissue samples were homogenized in ice-cold Tris buffer (50 mM, pH 7.6) at 50 mg/ml and centrifuged at 2,500×g for 10 min, to remove the cell membranes and nuclei. A sample aliquot (100 μl) of supernate was added to a 0.5 cm cuvette, along with 1.0 ml 50 mM Tris buffer (pH 7.6), 50 μl 0.2–10 mM oxaloacetate (substrate), 30 μl 12.3 mM acetyl-coenzyme A, 100 μl 1 mM 5,5′-dithiobis-2-nitrobenzoic acid (DTNB), and 100 μl 10 % Triton X-100. The free coenzyme-A generated by citrate synthase activity reacted with DTNB to form a colored compound that was quantified at 412 nm. Absorbance was recorded every 30 s for 6 min (reaching steady state), using a Hitachi spectrophotometer. Protein concentration was determined by means of the Lowry method. Citrate synthase activity is given as nmoles Coenzyme-A generated per min, per mg protein.
SERCA [21]
SERCA was evaluated by measuring thapsigargin-sensitive and -insensitive calcium ATPase activity. Frozen tissue samples were homogenized at 10 mg/ml in ice-cold Tris buffer (50 mM, pH 7.4) and centrifuged at 2,500×g for 10 min to remove the cell membranes and nuclei. Aliquots of particulate preparations were incubated at 37 °C in TRIS buffer with 4 mM ATP (substrate) and CaCl2 (1 mM). Complete details of the methods are given in the references. The reaction was measured in the presence and absence of 10 μM thapsigargin. Thapsigargin specifically inhibits the calcium ATPase localized in the SR membrane (SERCA) and thus, the activity of SERCA was quantitated by subtracting the activity in the presence of thapsigargin from the total activity in its absence.
ChAt activity [27]
Each frozen bladder sample was homogenized at 10 mg/ml 0.02 M EDTA (pH 7.6). The homogenate was diluted 1:10 with 0.02 M EDTA, 1 % Triton X-100, and centrifuged at 20,000×g for 30 min. Then, 100 μl aliquots of each supernate were incubated at 37 °C for 10 and 20 min with 200 μ1 of reaction mixture consisting of 0.2–10 mM acetyl-coenzyme A (acetyl-CoA) (substrate), 0.2 mM 3H-acetyl-CoA (200 mCi/mmol), 8 mM choline, 50 mM sodium phosphate, 0.3 M NaCl, 20 mM EDTA, and 96 nM physostigmine. After incubation, each solution was diluted with 5 ml of 0.01 M sodium phosphate, and the reaction stopped with 2 ml of acetonitrile containing 5 mg/ml tetraphenylboron. The contents of each reaction tube were transferred to a 20 ml scintillation vial and 10 ml of Betamax scintillation fluid was added slowly to each vial. The vials were shaken lightly. Samples stood for 1 h while the phases separated, extracting acetylcholine (3H-Ach) into the Betamax phase, while 3H-acetyl-CoA stayed in the aqueous phase. The aqueous phase was removed and 3H-Ach was measured using scintillation spectroscopy. ChAT activity is reported as picomoles Ach generated per min, per mg tissue.
Statistics
All values are given as the mean ± SEM. One-way analyses of variance, followed by the Tukey test for individual differences, were used to determine statistical significance. A p < 0.05 was required for statistical significance.
Results
The CS activities for the various tissues are presented in Fig. 1. As previously reported, the CS activities of the bladder body and base mucosa are significantly higher than those of the bladder body and base muscle. The Pc muscle had a significantly greater CS activity than that of the BS/IC muscles. The activity of the leg skeletal muscle was approximately equal to those of the bladder body and base muscle, and the BS/IC muscles.
Citrate synthase activities of lower urinary tract bladder body and base smooth muscle, and mucosa; pelvic floor skeletal muscles; and leg skeletal muscle. Each bar is the mean ± SEM of 5 individual rabbits. *Significantly different from bladder body and base muscles; x significantly different from coccygeus pelvic floor muscle; p < 0.05
SERCA activity is presented in Fig. 2. SERCA activity of the pelvic Pc muscle was significantly greater than the activity of the BS/IC muscles. The SERCA activities of the bladder body and base mucosa were significantly higher than the activities of their respective muscles, and approximately equal to the activity of the leg muscle. The ChAT activities of the bladder body and base muscles were significantly higher than the activity of the three skeletal muscles with the activity of the leg muscle being the lowest (Fig. 3). The leg muscle had a significantly lower CHaT activity than either of the pelvic floor muscles.
SERCA activities of lower urinary tract bladder body and base smooth muscle, and mucosa; pelvic floor skeletal muscles; and leg skeletal muscle. Each bar is the mean ± SEM of 5 individual rabbits. *Significantly different from bladder body and base muscles; x significantly different from coccygeus pelvic floor muscle; p < 0.05
Choline acetyltransferase activities of lower urinary tract smooth muscle, pelvic floor skeletal muscles, and leg skeletal muscle. Each bar is the mean ± SEM of 5 individual rabbits. *Significantly different from bladder body muscle; x significantly different from coccygeus pelvic floor muscle; p < 0.05
Discussion
Our results offer insight into the biochemical differences between the lower urinary tract and pelvic floor muscles. As observed previously, the CS activity of the mucosa was significantly higher than both the smooth muscle from the bladder body and the base [28]. Interestingly, the CS activity of the Pc muscle was also significantly higher than the CS activity of the BC/IS pelvic floor muscle. Citrate synthase is the first and key enzyme in the Kreb’s cycle in mitochondria. Interesting, the pelvic Pc muscle had a significantly higher CS activity than the pelvic IcBs muscle. These results indicate that the pelvic Pc muscle could provide a stronger contraction per unit mass than the pelvic BS/IC muscle and is more metabolically active, in fact similar to the bladder mucosa.
SERCA controls calcium uptake and storage within the SR, and would directly relate to calcium metabolism within the cell. The higher SERCA activity of the pelvic Pc muscle compared to the pelvic Ic/Bs muscle supports the idea that the Pc muscle is significantly stronger than the Ic/Bs muscle. The leg muscle, which is a very strong muscle, has the highest SERCA activity of any of the muscles tested. The mucosae of both the bladder body and the base have very high metabolic rates and synthetic activity, which involves calcium-activated enzymes; thus, the endoplasmic reticulum of the mucosa has a high SERCA activity.
In general, an increase in SERCA activity would suggest a greater calcium sequestration in the SR which we believe would also relate to a greater release of calcium during nerve-evoked contraction. We know that pathologies such as partial outlet obstruction and ischemic bladder dysfunction, which reduce contractile responses to all forms of stimulation, are associated with a decreased SERCA activity [15, 29, 30]. An increase in SERCA activity is observed in cardiac muscle in response to training and exercising which is associated with increased cardiac function [31, 32]. ChAT is the enzyme responsible for synthesizing acetylcholine in the cholinergic synapses which are the most sensitive organelles to free radical damage, and are the first structures to show damage in ischemic bladder dysfunction [27, 33]. The skeletal muscles of both the pelvic floor and leg have significantly lower activities than either of the bladder smooth muscles. This is expected as smooth muscle has few tight junctions, and greater ratios of synapses/cells are required for full muscle contractile stimulation. Interesting, the leg muscle, which has the greatest contractile force of the skeletal muscles tested, has a significantly lower ChAt activity than either of the pelvic floor muscles, indicating that there are significantly higher densities of tight junctions in the leg muscle than those in the pelvic floor muscles. These differential values are relevant for the use of therapeutic anticholinergic medication.
Based on the larger size and higher enzymatic activity of the Pc muscle, we will focus specifically on this pelvic floor muscle for the development of a rabbit animal model of pelvic floor overactivity in our future studies.
Conclusions
There are significant differences in the biochemical intracellular enzymes between specific pelvic floor muscle groups, compared to both each other and surrounding tissues. Based on our results, the Pc muscle is expected to have a significantly greater capacity to contract and a higher metabolic activity than those of the Ic/Bs muscles. We believe that pelvic floor muscles offer new targets for therapies aimed at reducing pelvic floor dystonia and associated urinary complaints.
References
Shafik A, El-Sibai O (2001) Effect of levator ani muscle contraction on urethrovesical and anorectal pressures and role of the muscle in urination and defecation. Urology 58:193–197
Lamvu G, Williams R, Zolnoun D, Wechter ME, Shortliffe A, Fulton G, Steege JF (2006) Long-term outcomes after surgical and nonsurgical management of chronic pelvic pain: one year after evaluation in a pelvic pain specialty clinic. Am J Obstet Gynecol 195:591–598 (discussion 598–600)
Dumoulin C, Hay-Smith J (2010) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 1: CD005654
Koh CE, Young CJ, Young JM, Solomon MJ (2008) Systematic review of randomized controlled trials of the effectiveness of biofeedback for pelvic floor dysfunction. Br J Surg 95:1079–1087
Wang AC, Wang YY, Chen MC (2004) Single-blind, randomized trial of pelvic floor muscle training, biofeedback-assisted pelvic floor muscle training, and electrical stimulation in the management of overactive bladder. Urology 63:61–66
Whitford HM, Jones M (2011) An exploration of the motivation of pregnant women to perform pelvic floor exercises using the revised theory of planned behaviour. Br J Health Psychol 16:761–778
Santacreu M, Fernandez-Ballesteros R (2011) Evaluation of a behavioral treatment for female urinary incontinence. Clin Interv Aging 6:133–139
Dumoulin C, Glazener C, Jenkinson D (2011) Determining the optimal pelvic floor muscle training regimen for women with stress urinary incontinence. Neurourol Urodyn 30:746–753
Simard C, le Tu M (2010) Long-term efficacy of pelvic floor muscle rehabilitation for older women with urinary incontinence. J Obstet Gynaecol Can 32:1163–1166
Hung HC, Hsiao SM, Chih SY, Lin HH, Tsauo JY (2011) Effect of pelvic-floor muscle strengthening on bladder neck mobility: a clinical trial. Phys Ther 91:1030–1038
Malykhina AP (2007) Neural mechanisms of pelvic organ cross-sensitization. Neuroscience 149:660–672
Buttyan R, Chen MW, Levin RM (1997) Animal models of bladder outlet obstruction and molecular insights into the basis for the development of bladder dysfunction. Eur Urol 32(Suppl 1):32–39
Levin RM, Haugaard N, Mogavero L, Leggett RE, Das AK (1999) Biochemical evaluation of obstructive bladder dysfunction in men secondary to BPH: a preliminary report. Urology 53:446–450
Levin RM, Haugaard N, O’Connor L, Buttyan R, Das A, Dixon JS, Gosling JA (2000) Obstructive response of human bladder to BPH vs. rabbit bladder response to partial outlet obstruction: a direct comparison. Neurourol Urodyn 19:609–629
Kato K, Monson FC, Longhurst PA, Wein AJ, Haugaard N, Levin RM (1990) The functional effects of long-term outlet obstruction on the rabbit urinary bladder. J Urol 143:600–606
Cruz Y, Hudson R, Pacheco P, Lucio RA, Martinez-Gomez M (2002) Anatomical and physiological characteristics of perineal muscles in the female rabbit. Physiol Behav 75:33–40
Corona-Quintanilla DL, Castelan F, Fajardo V, Manzo J, Martinez-Gomez M (2009) Temporal coordination of pelvic and perineal striated muscle activity during micturition in female rabbits. J Urol 181:1452–1458
Bouzidi MF, Enjolras N, Carrier H, Vial C, Lopez-Mediavilla C, Burt-Pichat B, Couthon F, Godinot C (1996) Variations of muscle mitochondrial creatine kinase activity in mitochondrial diseases. Biochim Biophys Acta 1316:61–70
Sherratt HS (1991) Mitochondria: structure and function. Rev Neurol (Paris) 147:417–430
Beeckmans S (1984) Some structural and regulatory aspects of citrate synthase. Int J Biochem 16:341–351
Levin RM, Nicholas TJ, Snitkoff GG, Mandell J, Russell D, Wilbur HJ, Mogavero LJ (1997) Subcellular distribution of SERCA and calcium-activated ATPase in rabbit and human urinary bladder smooth muscle. Pharmacology 55:309–316
Moller JV, Olesen C, Winther AM, Nissen P (2010) The sarcoplasmic Ca2+-ATPase: design of a perfect chemi-osmotic pump. Q Rev Biophys 43:501–566
Brini M, Carafoli E (2009) Calcium pumps in health and disease. Physiol Rev 89:1341–1378
Contestabile A, Ciani E (2008) The place of choline acetyltransferase activity measurement in the “cholinergic hypothesis” of neurodegenerative diseases. Neurochem Res 33:318–327
Dobransky T, Rylett RJ (2003) Functional regulation of choline acetyltransferase by phosphorylation. Neurochem Res 28:537–542
Haugaard N, Potter L, Wein AJ, Levin RM (1992) Effect of partial obstruction of the rabbit urinary bladder on malate dehydrogenase and citrate synthase activity. J Urol 147:1391–1393
Levin RM, Saito M, Wein AJ, Packard D, Cohen A, Haugaard N (1993) Effect of partial outlet obstruction on choline acetyltransferase activity in the rat and rabbit. Neurourol Urodyn 12:255–261
Hypolite JA, Longhurst PA, Gong C, Briscoe J, Wein AJ, Levin RM (1993) Metabolic studies on rabbit bladder smooth muscle and mucosa. Mol Cell Biochem 125:35–42
Levin RM, Haugaard N, Levin SS, Buttyan R, Chen MW, Monson FC, Wein AJ (1995) Bladder function in experimental outlet obstruction: pharmacologic responses to alterations in innervation, energetics, calcium mobilization, and genetics. Adv Exp Med Biol 385:7–19 (discussion 75–79)
Levin RM, Longhurst PA, Monson FC, Kato K, Wein AJ (1990) Effect of bladder outlet obstruction on the morphology, physiology, and pharmacology of the bladder. Prostate Suppl 3:9–26
Bupha-Intr T, Laosiripisan J, Wattanapermpool J (2009) Moderate intensity of regular exercise improves cardiac SR Ca2+ uptake activity in ovariectomized rats. J Appl Physiol 107:1105–1112
Kemi OJ, Ceci M, Condorelli G, Smith GL, Wisloff U (2008) Myocardial sarcoplasmic reticulum Ca2+ ATPase function is increased by aerobic interval training. Eur J Cardiovasc Prev Rehabil 15:145–148
Levin RM, Haugaard N, Wein AJ (1992) Metabolic alterations induced by obstructive hypertrophy of the rabbit urinary bladder. Jpn J Pharmacol 58(Suppl 2):341P
Acknowledgments
This material is based upon work supported in part by the Office of Research and Development Medical Research Service, Department of Veterans Affairs, and in part, by the Capital Region Medical Research Foundation.
Conflict of interest
No financial conflicts of interest are involved with any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spettel, S., De, E., Elias, T. et al. Citrate synthase, sarcoplasmic reticular calcium ATPase, and choline acetyltransferase activities of specific pelvic floor muscles of the rabbit. Mol Cell Biochem 370, 1–5 (2012). https://doi.org/10.1007/s11010-012-1347-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-012-1347-2