Abstract
Involvement of genetic polymorphisms in arterial hypertension has already been reported, including GST genes, with contrasting results. The present research evaluates the possible association between GST gene polymorphisms and essential hypertension (EH) in an Italian population sample. 193 hypertensive subjects and 210 healthy controls were recruited. Buccal cells were collected from each subject using an oral swab and DNA was extracted using the phenol:chloroform:isoamilic alcohol method. GST SNPs were determined using the PCR-RFLP method, while GST null polymorphisms were determined using a Multiplex PCR. Among GST polymorphisms, only the frequency of the GSTT1 null phenotype was significantly higher in hypertensive patients than in normotensive participants. GSTT1 null individuals were significantly associated with increased risk of hypertension [P < 0.001; adjusted OR 2.24 (1.43–3.50)]. In sex-based analysis, the risk was significantly higher in female hypertensives [P < 0.001; adjusted OR 3.25 (1.78–5.95)] but not in male subjects. This study analyzed all GST gene that, in other research, have been studied in relation to arterial hypertension and the GSTO polymorphisms, showing an association only with GSTT1. The results for the GSTO genes represent the first analysis of this GST class in relation to blood pressure regulation. The association between the GSTT1 null phenotype and EH was confirmed in the overall population and in women, but not in men. These data suggest that GSTT1 could be a sex-specific candidate gene for EH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human hypertension is classified as a complex, multifactorial, polygenic disease despite the fact that its genetic components still remain unknown [1]. Oxidative stress is an important pathogenetic factor in the development of cardiovascular diseases. Increased production of reactive oxygen species (ROS) and/or reduced defences against ROS not only immediately lead to endothelial dysfunction but also cause structural damage to tissue and organs [2].
Among the antioxidant mechanisms, glutathione is the most abundant nonprotein intracellular thiol, with multiple roles as antioxidant agent. Reduced glutathione (GSH) acts to scavenge ROS as well as to regenerate other antioxidants from their oxidized forms. During these processes, GSH is converted to its oxidized form (GSSG), which must be reduced by NADPH-glutathione reductase. The cell’s ability to maintain glutathione levels is highly important for its integrity and cellular function [3]. Moreover, GSH is also an essential cofactor for different enzymes like glutathione S-transferases (GSTs) [4].
The supergene family of GSTs is associated with the regulation of inflammation through modulation of prostaglandin signalling pathways and oxidative stress and through the regulation of normal cellular physiology [4]. The cytosolic family of GSTs is divided into seven classes: Alpha, Mu, Omega, Pi, Sigma, Theta, and Zeta [5]. Common variants of these genes may, therefore, have health implications for individuals exposed to oxidative stress [4]. The association between the variations in the GST activity in vivo and the susceptibility to cardiovascular and other diseases has been studied primarily through the use of GSTM1 null and GSTT1 null genotypes, as indicators of a systemic lack of expression of the corresponding proteins [6]. Different studies have successfully investigated the role of several GST gene polymorphisms in relation to the expression and development of complex diseases [7, 8]. Regarding the arterial hypertension, to date seven studies have been conducted on GST gene variability [9–15], but only one study has analyzed the association between GST and the essential hypertension (EH) [15]. Moreover, the results of these studies are in some cases conflicting. Therefore, previous published data are insufficient to prove the role of GST gene polymorphisms in arterial hypertension.
The mechanisms whereby GSTs influence the development and the expression of hypertension are complex and interactive. In this scenario, the conflicting results for the GST genes and blood pressure (BP) could be due not only to publication bias and sample size but also to extreme gene–environment interactions characterizing the hypertensive phenotypes.
The aim of this study is, therefore, the analysis of the possible involvement of GST gene variants in essential hypertensive subjects, living in central Italy. We investigated several GST gene polymorphisms to contribute to the knowledge about the genetics of EH. In particular, we focused our attention on functional polymorphisms of GST genes (GSTA1*-69C/T, GSTM1 null, GSTP1*I105V, GSTT1 null) that had been previously studied in relation to BP, and on two functional GSTO gene polymorphisms (GSTO1*A140D and GSTO2*N142D) not yet studied in relation to hypertension.
Methods
Study population
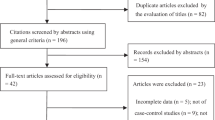
The study population consisted of 403 adult people who were not relatives and lived in Rome (Central Italy). 193 patients with a history of EH were recruited in the Clinical Physiopathology and Hypertension Centers of Fatebenefratelli Hospital. The hypertension diagnosis was based on the physician’s diagnosis and on the use of antihypertensive medications. All enrolled patients had appropriate clinical, laboratory, and radiological evaluations to exclude secondary hypertension and chronic kidney disease. 210 healthy individuals who visited Fatebenefratelli Hospital for an annual check-up and hospital staff members were used as a control group for this study. Control subjects were selected among healthy people with BP less than 140/90 mmHg and no history of hypertension and other cardiovascular diseases. BP was measured after 5 min of rest in a quiet environment and the average of three consecutive BP measurements was used as BP. Exclusion criteria were obesity (body mass index [BMI] > 30 kg/m2), diabetes mellitus, dyslipidemia, and chronic diseases. Information regarding smoking habits, vegetable intake, fruit intake, psychological stress, type of work, and physical activity were obtained by face-to-face interviews with medical staff members using a structured questionnaire. Written informed consent was obtained from all subjects and the study was approved by the Ethical Committee of Fatebenefratelli Hospital.
Genotyping procedures
Buccal cells were collected with an oral swab. All subjects were instructed to brush their teeth and refrain from eating and drinking for at least 1 h before sample collection. Patients had each cheek brushed for at least 30 s and the brushes were placed in plastic tubes. DNA from buccal cells was obtained using the Phenol: Chloroform: Isoamilic alcohol method [16].
The GSTA1–69C/T polymorphism was determined using the PCR-restriction fragment length polymorphism (RFLP) method using the restriction enzyme EarI [17]. The GSTO1*A140D and GSTO2*N140D polymorphisms were determined using the PCR-RFLP method with Cac8I and MboI restriction enzymes, respectively [18]. The GSTP1*I105V was analyzed by PCR-RFLP analysis with BsmAI [19]. Genotyping of GSTM1 and GSTT1 null polymorphisms was carried out by a Multiplex PCR reaction [20].
The genotypes were defined by different electrophoretic bands as already described in our previous study [21]. To ensure the reliability of the results, approximately 15% of the samples were randomly selected and genotyped independently by a second researcher using the same protocol: in all cases the outcome was concordant. Finally, the laboratory was not informed of the patients’ diagnoses until the final analysis. Patients and controls were identified by progressive numbers.
Statistical analysis
Descriptive analyses were performed using t-tests for continuous variables, while the Chi-square (χ2) test was used for categorical variables. The results of genotyping procedures were used to verify the Hardy–Weinberg equilibrium. Logistic regression was used to calculate adjusted odds ratios (ORs) and 95% CIs for the association between GST gene polymorphisms and hypertension. Since, we investigated six genetic markers in control and case groups, the standard significance level of 5% has been adjusted to α = 0.05/6 = 0.008, according the application of Bonferroni correction for multiple testing. All statistical calculations were performed using the SPSS software package version 15.0 for Windows (SPSS Inc., Chicago, IL).
Results
The characteristics of the participants are shown in Table 1. Age, sex, and BMI were not significantly different between hypertensive patients and normotensive participants, or were smoking habits and physical activity. Conversely, vegetable and fruit intake, psychological stress, and type of work were significantly different between the two groups. The genotype frequencies of GSTA1-69C/T, GSTO1*A140D, GSTO2*N142D, and GSTP1*I105V were in Hardy–Weinberg equilibrium. All genotype frequencies of GST polymorphisms in our controls were within the ranges reported previously in Italy and also in other European populations [22, 23]. The distributions of GST genotypes in the hypertensive and normotensive participants are shown in Table 2. Table 3 reports univariate and adjusted ORs in the overall population and in the sex-segregated populations. Regarding GSTA1*-69C/T, GSTM1 positive/null, GSTO1*A140D, GSTO2*N142D and GSTP1*I105V, no significant differences in the genotypic distributions between hypertensive subjects and healthy controls were found: χ2 test and adjusted ORs did not show any association between these genetic polymorphisms and EH in either the overall population and in the sex-segregated populations. Conversely, the GSTT1 null phenotype showed a significantly different distribution between the two groups with an evident increase in hypertensive individuals (P < 0.001), taking into account the Bonferroni corrected significance level (α = 0.008). Subjects with the GSTT1 null phenotype had a 2.24-fold increased risk of EH when compared with control subjects [adjusted OR 2.24 (1.43–3.50)]. When the GSTT1 phenotype distribution was stratified for sex, two different situations can be observed. Male individuals did not show a significant association between the GSTT1 null phenotype and EH [adjusted OR 1.66 (0.74–3.74)]. Conversely, in female individuals, the GSTT1 phenotype distribution showed significant differences between hypertensive patients and healthy controls: subjects with the GSTT1 null phenotype had a 3.25-fold increased risk of EH when compared with control subjects [adjusted OR 3.25 (1.78–5.95)].
Discussion
GSH is an important hydrophilic antioxidant and an essential cofactor for different enzymes like GSTs [4]. GSTs are phase II enzymes involved in xenobiotics metabolism, which occurs after these compounds are activated by phase I enzymes [24]. GST genetic polymorphisms imply variations in enzyme activities that can result in oxidative stress susceptibility through alterations in GSH metabolism [25]. In humans as well as in animal models, a significant body of data has been accumulated linking mutant expression of GSTs with the development and expression of several complex diseases [7, 8]. Different studies of hypertension have investigated the role of GST variants in BP regulation, but the results are conflicting [9–15]. The aim of this study is to verify the possible association between six GST gene polymorphisms and EH in an Italian population sample.
The data presented show that only the GSTT1 null phenotype was significantly associated with EH. Additionally, the results for the GSTO genes (GSTO1*A140D and GSTO2*N142D) represent the first attempt to analyze this GST class in relation to BP regulation. Naturally, further independent studies will be required to rule out a possible association between GSTO enzymes and arterial hypertension.
The significant association between the GSTT1 null phenotype and EH was confirmed by logistic regression analysis, proving that the confounding variables examined did not influence this association. Our result is in agreement with some previous studies [9, 11, 12, 15] but conflict with some others [10, 13, 14]. The heterogeneity in the outcomes for the GST genes and BP could be due to extreme gene–environment interactions that characterize the hypertensive phenotypes but could also be related to the difference in the selection of cases and controls. Our study is focused on EH whereas most GST studies are focalized on hypertensive phenotype. Therefore, independent studies are necessary to verify these results on EH.
Moreover, in sex-based analysis, only female individuals confirmed a significant association between the GSTT1 null phenotype and EH. This result could be due to the differences between sexes in the pathophysiology and risks of EH. Before the menopause, there are obvious hormonal differences between the sexes and it is now known that after the menopause, the arterial tree ages differently [26]. Moreover, in the genetics of hypertension several studies have reported sex-specific effects of gene variants and gene-by-sex interactions in human hypertension [27–30]. One potential mechanism by which the GSTT1 null phenotype might contribute to EH in females is that this variant could increase the sensibility of cells to xenobiotics (i.e., contraceptive agents) and to oxidative stress (i.e., menopause effects). Although this is consistent with the fact that females have some sex-specific primary causes of hypertension [26], more studies will be necessary to demonstrate the possible interaction with the GSTT1 null phenotype. The association of genetic polymorphisms with complex polygenic disorders, such as hypertension, is strongly influenced by ethnicity, environmental factors, differences in the selection of cases and controls, sample size, age, BMI, and other ecological factors [31]. Moreover, among confounding variables, socioeconomic status could have a strong impact on gene-candidate studies. Indeed, several modifiable socioeconomic determinants, such as education and occupation, are associated with hypertension and, the awareness of hypertension, prevention, control, accessibility, and adherence to medical treatment differ significantly among socioeconomic groups [32]. Therefore, the analysis of socioeconomic status could explain some conflicting results of hypertension genetic studies.
Finally, future studies of large size samples should focus on interactions of GST genes with environmental oxidative exposure and with other genes involved in pathophysiological pathways to explain the role of GST gene polymorphisms in hypertension status.
References
Ehret GB (2010) Genome-wide association studies: contribution of genomics to understanding blood pressure and essential hypertension. Curr Hypertens Rep 12:17–25
Hamilton CA, Miller WH, Al-Benna S, Brosnan MJ, Drummond RD, McBride MW et al (2004) Strategies to reduce oxidative stress in cardiovascular disease. Clin Sci (Lond) 106:219–234
Kaplowitz N, Aw TY, Ookhtens M (1985) The regulation of hepatic glutathione. Ann Rev Pharmacol Toxicol 25:715–744
Hayes JD, Flanagan JU, Jowsey IR (2005) Glutathione transferases. Annu Rev Pharmacol Toxicol 45:51–88
Frova C (2006) Glutathione transferases in the genomic era: new insights and perspectives. Biomol Engin 23:149–169
Fuciarelli M, Caccuri A, De Francesca M, Ferazzoli F, Piacentini S, Porreca F (2009) Modulation of the GSTT1 activity by the GSTM1 phenotype in a sample of Italian farm-workers. Arch Toxicol 83:115–120
Bolt HM, Thier R (2006) Relevance of the deletion polymorphisms of the glutathione S-transferases GSTT1 and GSTM1 in pharmacology and toxicology. Curr Drug Metab 7:613–628
Di Pietro G, Magno LA, Rios-Santos F (2010) Glutathione S-transferases: an overview in cancer research. Expert Opin Drug Metab Toxicol 6:153–170
Tamer L, Ercan B, Camsari A, Yildirim H, Ciçek D, Sucu N et al (2004) Glutathione S-transferase gene polymorphism as a susceptibility factor in smoking-related coronary artery disease. Basic Res Cardiol 99:223–229
Marinho C, Alho I, Arduíno D, Falcão LM, Brás-Nogueira J, Bicho M (2007) GST M1/T1 and MTHFR polymorphisms as risk factors for hypertension. Biochem Biophys Res Commun 353:344–350
Doney AS, Lee S, Leese GP, Morris AD, Palmer CN (2005) Increased cardiovascular morbidity and mortality in type 2 diabetes is associated with the glutathione S transferase theta-null genotype: a Go-DARTS study. Circulation 111:2927–2934
Oniki K, Hori M, Takata K, Yokoyama T, Mihara S, Marubayashi T, Nakagawa K (2008) Association between glutathione S-transferase A1, M1 and T1 polymorphisms and hypertension. Pharmacogenet Genomics 18:275–277
Delles C, Padmanabhana S, Lee WK, Miller WH, McBride MW, McClure JD et al (2008) Glutathione S-transferase variants and hypertension. J Hypertens 26:1343–1352
Capoluongo E, Onder G, Concolino P, Russo A, Santonocito C, Bernabei R, Zuppi C, Ameglio F, Landi F (2009) GSTM1-null polymorphism as possible risk marker for hypertension: Results from the aging and longevity study in the Sirente Geographic Area (ilSIRENTE study). Clin Chim Acta 399:92–96
Bessa SS, Ali EM, Hamdy SM (2009) The role of glutathione S- transferase M1 and T1 gene polymorphisms and oxidative stress-related parameters in Egyptian patients with essential hypertension. Eur J Intern Med 20:625–630
Budowle B, Moretti T, Smith J, Dizinno J (2000) DNA typing protocols: Molecular Biology and Forensic analysis. A Bio Techniques® Books Publications. Eaton Publishing, Natick
Ping J, Wang H, Huang M, Liu Z (2006) Genetic analysis of glutathione S-transferase A1 polymorphism in the Chinese population and the influence of genotype on enzymatic properties. Toxicol Sci 89:438–443
Takeshita H, Fujihara J, Takastuka H, Agusa T, Yasuda T, Kunito T (2009) Diversity of glutathione S-transferase omega 1 (A140D) and 2 (N142D) gene polymorphisms in worldwide populations. Clin Exp Pharmacol Physiol 36:283–286
Harries L, Stubbins MJ, Forman D, Howard GCW, Wolf CR (1997) Identification of genetic polymorphisms at the glutathione S-transferase Pi locus and association with susceptibility to bladder, testicular and prostate cancer. Carcinogenesis 18:641–644
Abdel-Rahman SZ, El-Zein RA, Anwar WA, Au WW (1996) A multiplex PCR procedure for polymorphic analysis of GSTM1 and GSTT1 genes in population studies. Cancer Lett 107:229–233
Piacentini S, Polimanti R, Moscatelli B, Re MA, Fuciarelli R, Manfellotto D, Fuciarelli M (2010) Glutathione S-transferase gene polymorphisms and air pollution as interactive risk factors for asthma in a multicenter Italian field study: a preliminary study. Ann Hum Biol 37:427–439
Piacentini S, Polimanti R, Porreca F, Martínez-Labarga C, De Stefano GF, Fuciarelli M (2010) GSTT1 and GSTM1 gene polymorphisms in European and African populations. Mol Biol Rep 38:1225–1230
Polimanti R, Piacentini S, Porreca F, Fuciarelli M (2010) Glutathione S-transferase Omega class (GSTO) polymorphisms in a sample from Rome (Central Italy). Ann Hum Biol 37:585–592
Singh MS, Michael M (2009) Role of xenobiotic metabolic enzymes in cancer epidemiology. Methods Mol Biol 472:243–264
Aydemir B, Onaran I, Kiziler AR, Alici B, Akyolcu MC (2007) Increased oxidative damage of sperm and seminal plasma in men with idiopathic infertility is higher in patients with glutathione S-transferase Mu-1 null genotype. Asian J Androl 9:108–115
Safar ME, Smulyan H (2004) Hypertension in women. Am J Hypertens 17:82–87
Li N, Wang H, Yang J, Zhou L, Hong J, Guo Y, Luo W, Chang J (2009) Genetic variation of NEDD4L is associated with essential hypertension in female Kazakh general population: a case-control study. BMC Med Genet 10:130
Rana BK, Insel PA, Payne SH, Abel K, Beutler E, Ziegler MG et al (2007) Population-based sample reveals gene-gender interactions in blood pressure in white Americans. Hypertension 49:96–106
Russo P, Loguercio M, Lauria F, Barba G, Arnout J, Cappuccio FP et al (2007) Age- and gender-dependent association of the −344C/T polymorphism of CYP11B2 with blood pressure in European populations. J Hum Hypertens 21:333–336
Wang Z, Liu Y, Liu J, Liu K, Lou Y, Wen J et al (2010) E-selectin gene polymorphisms are associated with essential hypertension: a case-control pilot study in a Chinese population. BMC Medical Genetics 11:127
Hajat C (2011) An introduction to epidemiology. Methods Mol Biol 713:27–39
Grotto I, Huerta M, Sharabi Y (2008) Hypertension and socioeconomic status. Curr Opin Cardiol 23:335–339
Acknowledgments
This research was supported by a grant from the University of Rome “Tor Vergata” (RSA 2009) to M.F. and by grants from AFaR (Associazione Fatebenefratelli per la Ricerca) and from SIIA (Società Italiana dell’Ipertensione Arteriosa—Lega Italiana contro l’Ipertensione Arteriosa) to D.M. The authors thank the volunteer participants for their generous co-operation and the collaborators of the “San Giovanni Calibita” Fatebenefratelli Hospital for their valuable contributions. The authors declare that they have no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Polimanti, R., Piacentini, S., Lazzarin, N. et al. Glutathione S-transferase variants as risk factor for essential hypertension in Italian patients. Mol Cell Biochem 357, 227–233 (2011). https://doi.org/10.1007/s11010-011-0893-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-011-0893-3