Abstract
High mobility group box-1 (HMGB1) has recently been implicated as a proinflammatory cytokine that plays critical roles in endothelial dysfunction and atherosclerosis. Atorvastatin, a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor, exerts anti-inflammatory effects in the cardiovascular system beyond its cholesterol-lowering property. The aim of our study was to investigate whether atorvastatin inhibits HMGB1-induced vascular endothelial activation, and elucidate the underlying molecular mechanism. In this study, we found that atorvastatin, at concentrations ranging from 0.1 to 10 μM, effectively and in a dose-dependent manner inhibited HMGB1-induced endothelial cells (ECs) activation. Incubation of ECs with 10 μM atorvastatin reduced adhesion molecules (ICAM-1 and E-selectin) expression concomitant with a significant inhibition in HMGB1-stimulated leukocyte-endothelial adhesion. Further experiments showed that atorvastatin markedly suppressed HMGB1-induced Toll like receptor 4 (TLR4) expression, Nuclear factor kappaB (NF-κB) nuclear translocation and DNA binding activity in ECs. Similar effects were also observed in ECs pretreated with the TLR4- specific inhibitor CLI-095, suggesting an important role of TLR4/NF-κB pathway. These findings indicate that atorvastatin attenuates HMGB1-induced vascular endothelial activation. The underlying mechanism involves, at least in part, inhibition of TLR4/NF-κB-dependent signaling pathway, which provied the new evidence for therapeutic application of statins to target inflammatory processes in cardiovascular disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothelial injury and dysfunction is regarded as an important initial event in atherogenesis and restenosis after percutaneous coronary intervention [1–3]. Growing evidence supports the concept that inflammation might significantly contribute to endothelial activation and subsequent polymorphonuclear leukocytes (PMNs) adhesion to vascular endothelium [4, 5]. Hence, effective anti-inflammation therapy may improve outcome in patients with coronary heart disease.
High mobility group box-1 (HMGB1) is a highly conserved nuclear DNA-binding protein that stabilizes nucleosomes and facilitates transcription [6, 7]. Recent studies indicate that HMGB1 as a potent extracellular cytokine is involved in cellular activation and proinflammatory response through interactions with its receptors [8, 9]. In addition to the receptor for advanced glycation end-products (RAGE), members of the Toll-like family of receptors (TLRs) are also confirmed to mediate HMGB1 signaling [9–11]. TLR4 is the first identified TLR of mammals that plays a critical role in the induction of inflammatory response by recognition of endogenous molecules / ligands such as heat shock proteins, matrix proteins and HMGB1 [10, 12, 13]. Activation of TLR4 may lead to the Nuclear factor kappaB (NF-κB) nuclear translocation and inflammation-related genes expression in several cell types [14, 15]. Nevertheless, few data are available regarding the role of TLR4 in HMGB1 induced vascular endothelial activation.
Statins, inhibitors of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, are extensively used for treatment of coronary heart disease as cholesterol-lowering agents [16]. However, researchers have reported statins exert beneficial cholesterol-independent vascular effects such as plaque stabilization, anti-inflammation and endothelial prevention [17–20]. Moreover, TLR4 signaling could be regulated by statins both in vivo and in vitro. Our previous investigation clearly demonstrated fluvastatin pretreatment significantly suppressed myocardial ischemia-reperfusion injury, which was associated with downregulation of TLR4 activity [21]. To date, the prevention mechanism of statins on vascular endothelial activation and their effects on TLR4 expression in endothelial cells (ECs) have not been fully elucidated.
In the present study, therefore, we investigated whether the HMG-CoA reductase inhibitor, atorvastatin, has an inhibitory effect on endothelial activation induced by HMGB1. Furthermore, we also explored whether the suppression was mainly through TLR4/NF-κB signaling pathway.
Materials and methods
Reagents
Atorvastatin (calcium salt) was kindly provided by Pfizer (Ann Arbor, MI, USA). Recombinant human HMGB1 and red fluorescent membrane dye PKH26 were purchased from Sigma (St. Louis, MO, USA). TLR4 inhibitor (CLI-095) was obtained from InvivoGene (San Diego, Calif., USA). Anti-TLR4, anti-NF-κB p65, anti-ICAM-1, anti-E-selectin, anti-CD31 and anti-β-actin antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA).
Cell culture
Primary ECs were isolated from the thoracic aorta of male Sprague-Dawley rats (100-150 g) as described previously, and then cultured in endothelial basal medium (EBM) containing 20% fetal bovine serum (FBS), ECs growth supplements, 100 U/ml penicillin, and 100 μg/ml streptomycin. Cells were incubated at 37°C in a humidified atmosphere of 95% air and 5% CO2. The purity of ECs was approximately 85%-90% as determined by flow cytometric analysis with the anti-CD31 antibody. Only ECs from passages 2–5 were studied. All procedures and animal care were approved by the Animal Care and Use Committee of Wuhan University, and conformed to the Guide for the Care and Use of Laboratory Animals by the National Institutes of Health (NIH Publication No. 80-23).
PMN preparation and adhesion
Fresh polymorphonuclear neutrophils (PMNs) were isolated from rat blood using the hetastarch exchange transfusion and sedimentation technique [22, 23], and labeled with the red fluorescent cell membrane linker PKH26 for assessment of adherence. ECs were seeded at a density of 1 × 104 cells/well in gelatin-coated 96-well culture plates, and grown to confluence. The EC monolayers were pretreated with atorvastatin or medium alone for 8 h and stimulated with HMGB1 for 16 h prior to the adhesion assay. After stimulation and washing, ECs were exposed to PKH26-loaded PMNs for 30 min. Next, nonadherent PMNs were removed by gentle washing with PBS, and the fluorescence of the adherent cells was measured at excitation of 551 nm and emission 567 nm. PMNs adherence was calculated as the proportion of the adherent PMNs fluorescence intensity among the total added cells. Data was represented as the fold change in cell adhesion compared to control value.
Cell viability assay
Cell viability was determined by bright field microscopy using trypan blue dye exclusion assay. Briefly, after ECs were treated with atorvastatin and/or HMGB1, cells were stained with 0.4% trypan blue dye for a few minutes and viewed under a light microscope. Cell viability was defined as the percentage of unstained cells relative to the total number of cells.
RNA extraction and real-time RT-PCR
Total RNA extraction from cells was performed according to the TRIZOL reagent protocol (Invitrogen, Carlsbad, CA). Isolated RNA (2 μg) was converted into cDNA using high-capacity cDNA synthesis kit (TaKaRa, Japan). Real-time PCR was performed with a ABI Prism 7500 sequence detection system (PE Applied Biosystems). The SYBR Green Real-time PCR Master Mix kit (TaKaRa, Japan) was utilized in subsequent PCR assays in accordance with the manufacturer’s instructions. The primers used for PCR amplification were synthesized by Sangon Gene Company (Shanghai, China) and seen in Table 1. Semilog amplification curves were analyzed using the 2−ΔΔCt comparative quantification method [24], and the expression of each gene was normalized to GAPDH.
Western blot analysis
Cells were washed with ice-cold PBS and harvested in lysis buffer. Nuclear, cytoplasmic or total protein samples were separated on 10% SDS-polyacrylamide gels under denaturing conditions, and transferred to nitrocellulose membranes. The membranes were blocked with 5% non-fat dry milk in Tris-buffer saline (TBS)-0.05% Tween. Afterwards, the blots were incubated with primary antibodies (anti-TLR4, anti-NF-κB p65, anti-ICAM-1, anti-E-selectin and anti-β-actin antibody, respectively) and horseradish peroxidase-conjugated secondary antibody. Proteins were detected by an ECL chemiluminescence detection kit (Pierce).
Electrophoretic mobility shift assay (EMSA)
To measure NF-κB activation, ECs were collected on ice 1 h after HMGB1 stimulation. Nuclear extracts were prepared using the NE-PER kit (Pierce) following the manufacturer’s instructions. Equal amounts of nuclear extract protein (5 μg) were incubated with 10 × binding buffer, 1 μg/μl poly (dI-dC), and 400 fmol biotin-labelled double-stranded NF-κB binding consensus oligonucleotides 5′-AGTTGAGGGGACTTTCCCAGGC-3′ (total vol 15 μl) using a LightShift® Chemiluminescent EMSA kit (Viagene Biotech, Ningbo, China). Specificity of binding was ascertained by competition with a 50-fold excess of unlabeled consensus oligonucleotides.
Statistical analysis
Data were expressed as mean ± SD of at least four experiments. One-way analysis of variance (ANOVA) and Student-Newman-Keuls (SNK)-q test were performed with SPSS 13.0 statistical analysis software. P value < 0.05 was considered significant.
Results
Effect of atorvastatin on ECs viability
Atorvastatin had no relevant effect on ECs viability at concentrations up to 10 μM (cell viability > 95%), except for 88.7% with atorvastatin 100 μM for 24 h (Fig. 1A). In addition, incubation of ECs for 16 h with HMGB1 from 50 to 1000 ng/ml did not exhibit an altered morphology or uptake of trypan blue (Fig. 1B).
Effect of atorvastatin and HMGB1 on cell viability. ECs were treated with different concentrations of atorvastatin (A) or HMGB1 (B) for indicated time periods. Cell viability was determined by trypan blue staining. All values were expressed as mean ± SD of four separate experiments. ★ P < 0.05 as compared with control
Atorvastatin suppresses HMGB1-induced ECs activation
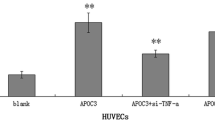
Upon activation of the EC monolayers with HMGB1, PMNs adhesion to ECs was markedly increased compared to that in the absence of activation in a static assay (Fig. 2A). To assess whether TLR4 signaling pathway was involved in HMGB1-mediated ECs activation, ECs were pretreated with the TLR4-inhibitor CLI-095, for 30 min before HMGB1 stimulation. The data showed that CLI-095 significantly inhibited PMNs adhesion to ECs induced by HMGB1 (P < 0.05). Moreover, we observed that atorvastatin dose-dependently suppressed HMGB1-induced ECs activation. The inhibitive rate was about 50% with 10 μM of atorvastatin pretreatment (P < 0.05, Fig. 2B).
Atorvastatin prevented HMGB1-induced PMNs adhesion to ECs. (A) ECs were stimulated for 16 h with varying concentrations of HMGB1. (B) ECs were stimulated for 16 h with HMGB1 (1000 ng/ml) that was preincubated with CLI-095 (1 μM) or various concentrations of atorvastatin for indicated time periods. After different treatment, PMNs adhesion was detected as described in Materials and methods. Four independent experiments were done and the data were expressed as mean ± SD. ★ P < 0.05 compared with cells treated with medium only; △ P < 0.05 compared with HMGB1 alone treatment
Effect of atorvastatin on TLR4 expression in ECs
As shown in Fig. 3, untreated ECs expressed low levels of TLR4 in vitro. After 4 h of HMGB1 stimulation (1000 ng/ml), the levels of TLR4 mRNA and protein were significantly up-regulated 4.2- and 3.1-fold, respectively (P < 0.05). Furthermore, enhanced expression of TLR4 by HMGB1 was reduced by 10 μM atorvastatin pretreatment (P < 0.05). However, compared with ECs control, atorvastatin itself did not affect TLR4 expression.
Effect of atorvastatin on TLR4 expression in ECs. (A) TLR4 mRNA expression was determined by Real-time PCR. (B) TLR4 protein level was measured by Western blot analysis. Original representative Western blots are reported in the upper panel. Data from four independent experiments were shown and expressed as mean ± SD. ★ P < 0.05 compared with cells treated with medium only; △ P < 0.05 compared with HMGB1 alone treatment
Atorvastatin inhibits HMGB1-induced NF-κB activation in ECs
HMGB1 activates TLR4 signal-transduction pathways. Therefore, in order to investigate the effect of atorvastatin on TLR4/NF-κB signaling pathway induced by HMGB1 stimulation, NF-κB translocation and DNA binding were both examined. A significant increase in NF-κB p65 nuclear translocation and DNA binding activity over the control was noted upon stimulation with HMGB1 in the absence of atorvastatin or CLI-095 pretreatment (P < 0.05). Meanwhile, HMGB1-mediated NF-κB activation was obviously blunted by incubation with atorvastatin (10 μM, 8 h) or CLI-095 (1 μM, 30 min) prior to HMGB1 stimulation for 1 h (P < 0.05, Fig. 4).
Pretreatment with atorvastatin or CLI-095 inhibited HMGB1-induced NF-κB nuclear translocation and DNA binding in ECs. (A) Cellular nuclear extracts were subjected to Western immunoblotting to detect NF-κB p65 subunit nuclear translocation. (B) DNA binding activity of NF-κB was measured by EMSA. Figures show data of mean ± SD of four independent experiments. ★ P < 0.05 compared with cells treated with medium only; △ P < 0.05 compared with HMGB1 alone treatment
Effect of atorvastatin on the expression of adhesion molecules in HMGB1-stimulated ECs
PMNs adhesion to ECs was mediated by several adhesion molecules including ICAM-1 and E-selectin. In addition, the transcription of these adhesion molecules was controled by NF-κB activation. As shown in Fig. 5, ECs showed a low baseline expression of ICAM-1 and E-selectin which was markedly increased following stimulation with HMGB1 for 16 h (P < 0.05). In contrast, the induction of these two molecules expression by HMGB1 was inhibited by pretreatment with atorvastatin (P < 0.05). Consistent with above results, CLI-095 could also efficiently suppress HMGB1-induced upregulation of both ICAM-1 and E-selectin (P < 0.05).
Effect of atorvastatin and CLI-095 on HMGB1-stimulated adhesion molecules production. (A) ICAM-1 and E-selectin mRNA levels were analyzed by Real-time PCR. (B) protein levels were measured by Western blot analysis. Shown in the upper panel are original representative Western blots. Data were mean ± SD of four independent experiments. ★ P < 0.05 compared with cells treated with medium only; △ P < 0.05 compared with HMGB1 alone treatment
Discussion
In the present study, we have shown that atorvastatin pretreatment could significantly suppress HMGB1 induced vascular endothelial activation in vitro via regulation of adhesion molecules (ICAM-1 and E-selectin) expression. The effect appears to be associated with its inhibition in TLR4 expression and NF-κB activation. These results suggest that TLR4/NF-κB signaling pathway may be a novel therapeutic potential of atorvastatin for HMGB1 mediated endothelial activation.
Vascular endothelial activation contributing to atherogenesis is triggered by multiple factors, including inflammation, hypoxia and physical damage [4, 25–27]. Among these, inflammatory response is considered to be the most important. Emerging evidence has suggested that HMGB1, a proinflammatory cytokine secreted from necrotic cells and activated macrophages/monocytes could lead to the endothelial activation after binding to the RAGE [9]. Indeed, TLR4 as an alternative cell surface receptor for HMGB1, also plays a key role in initiating inflammatory response. However, it remains unclear whether TLR4 is involved in mediating HMGB1 induced vascular endothelial activation. Our data clearly demonstrated that TLR4 expression, NF-κB activation and adhesion molecules production were all significantly up-regulated in ECs after HMGB1 stimulation. Moreover, inhibition of TLR4 signaling pathway by CLI-095 could effectively attenuate PMNs adhesion to ECs, which indicates that HMGB1 induced vascular endothelial activation is partly through TLR4/NF-κB signaling pathway.
Activated TLR4 may augment its expression per se, resulting in the enhancement of host innate immunity and anti-stress capacity [28]. In such case, TLR4 expression is protective in the process of endothelial dysfunction. Nevertheless, over-expression of TLR4 may lead to endothelial injury. In the present study, we found that TLR4 expression was up-regulated more than 4-fold in ECs with HMGB1, as compared to untreated controls. TLR4 is a well-known stimulator of NF-κB signaling and the major adhesion molecules (ICAM-1 and E-selectin) are the best-known target genes of NF-κB signaling [29–31]. Furthermore, several studies have highlighted that activation of NF-κB, and the subsequent expression of adhesion molecules, are key events in the recruitment of leukocytes to stimulated vascular endothelium in inflammation [32, 33]. Our results reported above are very consistent with these studies.
Atorvastatin, one of the most potent statins on the market, along with its well-established actions on lipid lowering, also exerts anti-inflammation and endothelial protection effects [18, 19, 34]. Although direct beneficial effects of atorvastatin on endothelium have already been reported, the mechanisms involved remain poorly understood. Interestingly, the results of our study revealed that atorvastatin pretreatment may attenuate HMGB1 induced the endothelial-leukocyte interaction by reducing ICAM-1 and E-selectin expression. Moreover, the inhibitory action of atorvastatin on endothelial activation post-HMGB1 induction was mainly through the TLR4/NF-κB signaling pathway down-regulation. Another important finding of the present investigation was that the same dose of atorvastatin did not significantly influence surface expression of TLR4 in HMGB1-non-stimulation ECs compared with control. We speculate that the feedback mechanism may be crucial for maintaining stable gene expression in normal condition.
In summary, this is the first study to show that atorvastatin prevented HMGB1-induced vascular endothelial activation by specifically inhibiting the TLR4/NF-κB pathway. These results underline the ability of atorvastatin to protect endothelial function under pathological conditions. We believe that TLR4/NF-κB signaling pathway will become a potential therapeutic target for the treatment of atherogenesis and other inflammatory vascular disorders.
References
Celermajer DS (1997) Endothelial dysfunction: does it matter? Is it reversible? J Am Coll Cardiol 30:325–333
Xi H, Akishita M, Nagai K, Yu W, Hasegawa H, Eto M et al (2007) Potent free radical scavenger, edaravone, suppresses oxidative stress-induced endothelial damage and early atherosclerosis. Atherosclerosis 191:281–289
Sima AV, Stancu CS, Simionescu M (2009) Vascular endothelium in atherosclerosis. Cell Tissue Res 335:191–203
Mazzone A, De Servi S, Ricevuti G, Mazzucchelli I, Fossati G, Pasotti D et al (1993) Increased expression of neutrophil and monocyte adhesion molecules in unstable coronary artery disease. Circulation 88:358–363
Lush CW, Cepinskas G, Kvietys PR (2000) LPS tolerance in human endothelial cells: reduced PMN adhesion, E-selectin expression, and NF-kappaB mobilization. Am J Physiol Heart Circ Physiol 278:H853–H861
Bustin M, Reeves R (1996) High-mobility-group chromosomal proteins: architectural components that facilitate chromatin function. Prog Nucleic Acid Res Mol Biol 54:35–100
Park JS, Arcaroli J, Yum HK, Yang H, Wang H, Yang KY et al (2003) Activation of gene expression in human neutrophils by high mobility group box 1 protein. Am J Physiol Cell Physiol 284:C870–C879
Kostova N, Zlateva S, Ugrinova I, Pasheva E (2010) The expression of HMGB1 protein and its receptor RAGE in human malignant tumors. Mol Cell Biochem 337:251–258
Scaffidi P, Misteli T, Bianchi ME (2002) Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature 418:191–195
Park JS, Svetkauskaite D, He Q, Kim JY, Strassheim D, Ishizaka A et al (2004) Involvement of toll-like receptors 2 and 4 in cellular activation by high mobility group box 1 protein. J Biol Chem 279:7370–7377
Park JS, Gamboni-Robertson F, He Q, Svetkauskaite D, Kim JY, Strassheim D et al (2006) High mobility group box 1 protein interacts with multiple Toll-like receptors. Am J Physiol Cell Physiol 290:C917–C924
Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X et al (1998) Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282:2085–2088
Miyake K (2007) Innate immune sensing of pathogens and danger signals by cell surface Toll-like receptors. Semin Immunol 19:3–10
Baumgarten G, Knuefermann P, Nozaki N, Sivasubramanian N, Mann DL, Vallejo JG (2001) In vivo expression of proinflammatory mediators in the adult heart after endotoxin administration: the role of toll-like receptor-4. J Infect Dis 183:1617–1624
Sassá MF, Saturi AE, Souza LF, Ribeiro LC, Sgarbi DB, Carlos IZ (2009) Response of macrophage Toll-like receptor 4 to a Sporothrix schenckii lipid extract during experimental sporotrichosis. Immunology 128:301–309
Blumenthal RS (2000) Statins: effective antiatherosclerotic therapy. Am Heart J 139:577–583
Ross R (1999) Atherosclerosis–an inflammatory disease. N Engl J Med 340:115–126
Elrod JW, Lefer DJ (2005) The effects of statins on endothelium, inflammation and cardioprotection. Drug News Perspect 18:229–236
Balk EM, Karas RH, Jordan HS, Kupelnick B, Chew P, Lau J (2004) Effects of statins on vascular structure and function: a systematic review. Am J Med 117:775–790
Stalker TJ, Lefer AM, Scalia R (2001) A new HMG-CoA reductase inhibitor, rosuvastatin, exerts anti-inflammatory effects on the microvascular endothelium: the role of mevalonic acid. Br J Pharmacol 133:406–412
Yang J, Zhang XD, Yang J, Ding JW, Liu ZQ, Li SG et al (2010) The cardioprotective effect of fluvastatin on ischemic injury via down-regulation of toll-like receptor 4. Mol Biol Rep doi:10.1007/s11033-010-9970-z
Williams JH Jr, Moser KM, Ulich T, Cairo MS (1987) Harvesting the noncirculating pool of polymorphonuclear leukocytes in rats by hetastarch exchange transfusion (HET): yield and functional assessment. J Leukoc Biol 42:455–462
Hu G, Vogel SM, Schwartz DE, Malik AB, Minshall RD (2008) Intercellular adhesion molecule-1-dependent neutrophil adhesion to endothelial cells induces caveolae-mediated pulmonary vascular hyperpermeability. Circ Res 102:e120–e131
Yang J, Yang J, Ding JW, Chen LH, Wang YL, Li S et al (2008) Sequential expression of TLR4 and its effects on the myocardium of rats with myocardial ischemia-reperfusion injury. Inflammation 31:304–312
Szmitko PE, Wang CH, Weisel RD, Jeffries GA, Anderson TJ, Verma S (2003) Biomarkers of vascular disease linking inflammation to endothelial activation: Part II. Circulation 108:2041–2048
Chow SE, Hshu YC, Wang JS, Chen JK (2007) Resveratrol attenuates oxLDL-stimulated NADPH oxidase activity and protects endothelial cells from oxidative functional damages. J Appl Physiol 102:1520–1527
Wang JS, Singh H, Zhang F, Ishizuka T, Deng H, Kemp R et al (2006) Endothelial dysfunction and hypertension in rats transduced with CYP4A2 adenovirus. Circ Res 98:962–969
Medzhitov R, Preston-Hurlburt P, Janeway CA Jr (1997) A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature 388:394–397
Ibeagha-Awemu EM, Lee JW, Ibeagha AE, Bannerman DD, Paape MJ, Zhao X (2008) Bacterial lipopolysaccharide induces increased expression of toll-like receptor (TLR) 4 and downstream TLR signaling molecules in bovine mammary epithelial cells. Vet Res 39:11
Kang JS, Park SK, Yang KH, Kim HM (2003) Silymarin inhibits TNF-alpha-induced expression of adhesion molecules in human umbilical vein endothelial cells. FEBS Lett 550:89–93
Kim I, Moon SO, Kim SH, Kim HJ, Koh YS, Koh GY (2001) Vascular endothelial growth factor expression of intercellular adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1), and E-selectin through nuclear factor-kappa B activation in endothelial cells. J Biol Chem 276:7614–7620
Collins T, Read MA, Neish AS, Whitley MZ, Thanos D, Maniatis T (1995) Transcriptional regulation of endothelial cell adhesion molecules: NF-kappa B and cytokine-inducible enhancers. FASEB J 9:899–909
Zhou Z, Connell MC, MacEwan DJ (2007) TNFR1-induced NF-kappaB, but not ERK, p38MAPK or JNK activation, mediates TNF-induced ICAM-1 and VCAM-1 expression on endothelial cells. Cell Signal 19:1238–1248
Osman L, Amrani M, Ilsley C, Yacoub MH, Smolenski RT (2008) Atorvastatin accelerates extracellular nucleotide degradation in human endothelial cells. Mol Cell Biochem 308:209–217
Acknowledgements
This work was supported by the Natural Science Foundation of Hubei province, China (Grant No. 2008CDZ044) and the Education Foundation of Hubei Province, China (Grant No. B20081303).
Author information
Authors and Affiliations
Corresponding author
Additional information
Jun Yang and Jian Yang are Contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yang, J., Huang, C., Yang, J. et al. Statins attenuate high mobility group box-1 protein induced vascular endothelial activation : a key role for TLR4/NF-κB signaling pathway. Mol Cell Biochem 345, 189–195 (2010). https://doi.org/10.1007/s11010-010-0572-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-010-0572-9