Abstract
Proliferation of human retinal endothelial cells (HRECs) is an important event in the development of diabetic retinopathy. Glucose fluctuations are strong predictor of diabetic vascular complications. In this study we have investigated the effect of intermittent high glucose on proliferation and expression of vascular endothelial growth factor (VEGF) in HRECs. The possible involvement of mitochondrial reactive oxygen species (ROS) was assessed. HRECs were incubated for 72 h in media containing different glucose concentrations: 5, 25, 5 mmol/l alternating with 25 mmol/l glucose, with or without Mn(III)tetrakis(4-benzoic acid) porphyrin chloride (MnTBAP) and thenoyltri-fluoroacetone (TTFA). The cell proliferation, VEGF expression, mitochondrial ROS, nitrotyrosine and 8-hydroxydeoxyguanosine (8-OHdG) were measured. In cultured HRECs, treatment with constant or intermittent high glucose significantly increased [3H]thymidine incorporation in a time-dependent manner. Treatment with constant high glucose for 48 h resulted in significant increases in [3H]thymidine incorporation, mRNA and protein levels of VEGF compared with HRECs treated with the normal glucose, which were markedly enhanced in cells exposed to intermittent high glucose. The levels of mitochondrial ROS, nitrotyrosine and 8-OhdG were significantly elevated under both intermittent and constant high glucose conditions, the effect being greater under intermittent high glucose. In addition, the antioxidants MnTBAP or TTFA can effectively prevent cell proliferation and overexpression of VEGF, as well as overproduction of mitochondrial ROS, nitrotyrosine and 8-OhdG in HRECs induced by constant or intermittent high glucose. Intermittent high glucose enhances cell proliferation and overexpression of VEGF through reactive oxygen species (ROS) overproduction at the mitochondrial transport chain level in HRECs, indicating that glycemic variability have important pathological effects on the development of diabetic retinopathy dependent of mitochondrial ROS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy is the most common complication of diabetes and a leading cause of blindness, affecting approximately three-fourths of diabetic patients within 15 years after onset of the disease [1, 2]. Proliferation of vascular endothelial cells is an important event in the development of neovascularization. VEGF is a peptide growth factor, generated in the vascular wall, has been identified as a primary mediator of the vascular alterations in diabetic retinopathy [3]. VEGF is involved in regulation of endothelial cell proliferation and migration [3, 4]. A number of clinical studies have shown a strong correlation between increases in intraocular VEGF concentration and the development of proliferative diabetic retinopathy [5].
Oxidative stress induced by hyperglycemia is an important pathway of diabetic microvascular complications. An increasing number of studies place mitochondrial ROS overproduction at the heart of pathogenesis of diabetic microvascular complications. Normalizing mitochondrial superoxide production can block other pathways of hyperglycemic damage [6, 7]. Mitochondrial electron transport chain is one of the main sources of reactive oxygen species (ROS). Recent studies showing that diabetes-induced retinal vascular dysfunction can be prevented by inhibitors of reactive oxygen species provide further support for the role of oxidative stress in diabetic retinopathy [8, 9]. Oxidative stress has been correlated with the increased production of VEGF under in vitro conditions and is thought to be involved in the upregulation of VEGF expression during diabetes [10]. Studies showing that diabetes-induced increases in retinal VEGF concentrations in streptozotocin-induced diabetic rats can be prevented by antioxidant treatment [11] provide strong support for this hypothesis.
Chronic hyperglycemia has been identified as a risk factor for the onset and progression of microvascular complications. Clinicians, however, often wonder why some patients under good metabolic control develop complications, while others remain free of such complications despite poor control [12]. One factor that can influence differing susceptibility to the appearance of microvascular complications despite similar levels of HbA1c is the blood glucose control variability. There is increasing evidence that glycemic disorders such as glucose fluctuations over a daily period might play an important role on diabetic complications [13]. A mean follow-up of 5.2 years shows that FPG variability, irrespective of mean HbA1c, is an independent contribution to the onset of diabetic retinopathy in a group of Type 2 diabetic patients [14]. However, the mechanism and the effects of intermittent hyperglycemia on diabetic retinopathy are poorly understood. So, it is necessary to investigate the importance of glucose variability to the development of microvascular complications in greater depth.
In order to investigate the effects of exposure to intermittent high glucose on cell proliferation and expression of VEGF, as well as the possible involvement of mitochondrial ROS production, HRECs culture medium was enriched with the superoxide dismutase (SOD) mimetic MnTBAP [15], a cell-permeable superoxide dismutase mimetic or TTFA, an inhibitor of mitochondrial complex II [7]. As an index of oxidative damage mitochondrial ROS, nitrotyrosine and 8-OHdG have been measured.
Materials and methods
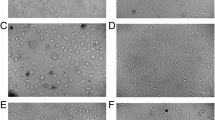
Cell culture
HRECs were isolated as previously described [16]. Cells were used at passages 3–6 for all experiments. Cells were grown in attachment factor-coated dishes and maintained in serum-free medium supplemented with 10% FBS, 100 IU/ml penicillin, 100 μg/ml streptomycin, and 0.25 μg/ml amphotericin B. The number of live cells was counted using a blood counting instrument after 0.4% trypan blue staining.
Experimental protocol
HRECs at the logarithmic growth phase were trypsinized to a single cell suspension, adjusted to cell concentration 1 × 105/ml, and transferred to a 6-well plate. After the cells reached confluence, the medium was replaced with serum-free DMEM and incubated for 24 h for synchronization. Cells were then incubated for a further 72 h in glucose-specific basic media. The cells were randomly divided into four groups: (1) constant normal glucose medium (5 mmol/l); (2) constant high glucose medium (25 mmol/l); (3) alternating normal and high glucose media every 6 h; (4) an osmotic control of 25 mmol/l mannose. 10 μmmol/l TTFA and 100 μmmol/l MnTBAP were also added individually to the four media previously described. The media in all groups were changed every 6 h, and the experiment was repeated at least five times.
Assessment of cell proliferation
[3H]thymidine incorporation was used in the assessment of cell proliferation. Briefly, HRECs were subcultured in 6-well plates as described in the experimental protocol. Quiescent cultures were then exposed to either constant or intermittent high glucose in serum-free medium for 12, 24, 48, 72 h. [3H]thymidine (1 mCi/ml, specific activity 20 Ci/mmol) was added to one set of wells in the last 4 h of incubation. The other sets of wells were processed for cell counting. For the assessment of [3H]thymidine incorporation, media was removed at the end of incubation, and cells were washed with 10% trichloroacetic acid and digested with 0.5 N NaOH. Radioactivity in the cell digest was counted in a Beckman scintillation counter. [3H]thymidine incorporation is expressed as the total counts per minute per well.
Measurement of VEGF by ELISA
VEGF were measured in culture media using RayBio® human VEGF ELISA (enzyme-linked immunosorbent assay) kit according to the manufacturer’s instructions. The kits are of high sensitivity (<3 pg/ml, minimum detectability), and with stated intra- and inter-assay coefficients of variation of <12%. Absorbance at 490 nm was measured in a microplate reader. The standard graph was drawn.
Northern blot analysis
For the assessment of the mRNA levels of VEGF, HRECs were subcultured in 75-cm3 flasks. Total RNA was isolated from the cells using TRIzol reagent (Sigma, Louis, MO). For Northern analysis, 20 μg aliquots of total RNA were separated on 1% agarose-formaldehyde gels, transferred to nylon membranes (Hybond-Nt; Amersham), and hybridized with [32P]-labeled cDNA probe (Sangon Biological Engineering Co. Ltd) of VEGF and rat glyceraldehyde-3-phosphate dehydrogenase (GAPDH) by random priming. Quantitations of Northern blots were performed by densitometric analysis by using an Eagle Eye II video system. Also we used GAPDH as an internal control to standardize the amount of total RNA utilized for Northern blot analysis.
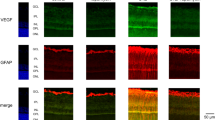
Mitochondrial ROS production
Mitochondrial ROS generation in HRECs was assessed with MitoSox red (Invitrogen), which is a fluorescent probe targeted to the mitochondria. Briefly, HRECs were incubated with 1 μmol/l MitoSox for 30 min at 37°C according to the manufacturer’s protocol. Cells were washed twice with PBS and the fluorescence intensity was captured at 510/580 nm using an Olympus IX70 microscope equipped with a digital cooled charged-coupled device camera. Determination of the mitochondrial ROS concentration by fluorescence intensity of the MitoSox red probe, expressed as the percentage of the value of normal glucose condition (100%).
Determination of 8-OhdG
8-OHdG amount was determined in HRECs DNA digests using Bioxytech 8-OHdG-EIA Kit, a competitive ELISA. HRECs DNA was isolated using DNAzol reagent, according to the manufacturer’s instructions, and quantified using a spectrophotometer. Samples containing 400 μg of DNA were resuspended in 50 μl of reaction mixture, containing 100 mmol/l sodium acetate (pH 5.0) and 5 mmol/l MgCl2, and digested with 1 μl of DNaseI, for 10 min at room temperature. DNA-digested samples were added to the microtiter plate precoated with 8-OHdG, and the assay was performed according to the manufacturer’s instructions. Intra-assay and inter-assay coefficients of variation were 2.1 and 4.5%, respectively.
Determination of nitrotyrosine
Nitrotyrosine content was evaluated by ELISA. Briefly, an identical amount of protein from cell lysates (50 μg) was applied to a Maxisorp ELISA plate (NUNC Brand Products) together with nitrated BSA standard and allowed to bind overnight at 4°C. After blocking, wells were incubated at 37°C for 1 h with a mouse monoclonal antibody anti-nitrotyrosine (Upstate Biotechnology, Lake Placid, NY) (5 μg/ml) and then for 45 min at 37°C with a peroxidase conjugated goat anti-mouse IgG secondary antibody diluted 1:1,000. After washing, peroxidase reaction product was generated using TMB peroxidase substrate. Intra-assay and inter-assay coefficients of variation were 10 and 12%, respectively.
Statistical analysis
Protein content was expressed as a change from the control value (normal glucose) which was regarded as 100%. Results are expressed as mean ± SD. Statistical comparisons between groups were made by analysis of variance (ANOVA), with pairwise multiple comparisons made by Fisher’s protected least-significant differences test. Analyses were by the software package, SPSS 13.0. A value of P less than 0.05 was considered significant.
Results
Effect of intermittent high glucose on proliferation of HRECs
As shown in Fig. 1, high glucose stimulated the proliferation of cultured HRECs in a time-dependent manner. The significant increase was observed after 12 h of high glucose treatment, further deteriorated afterwards and reached the maximum incorporation at 48 h. Continuous increasing effect was not found when the cells were treated for the longer time (72 h). Therefore, 48 h was selected as the treated time in subsequent studies. Mannose (25 mmol/l), an enhancer of osmotic pressure, did not affect the proliferation of HRECs, indicating that high glucose-induced HRECs proliferation was not due to an enhanced osmotic pressure.
Effect of high glucose on proliferation of HRECs. NG constant normal glucose (5 mmol/l), OC osmotic control (25 mmol/l mannose was used as a negative control), HG constant high glucose (25 mmol/l), N/HG 5 mmol/l alternating with 25 mmol/l glucose. The growth-arrested HRECs were exposed to glucose at different concentration for indicated time and total cell lysates were harvested. Cell proliferation was evaluated by the assessment of [3H]thymidine incorporation. The data expressed as mean ± SD of at least five independent experiments. *P < 0.01 versus NG, # p < 0.01 versus HG
Exposure to constant high glucose produced significant 23.0, 51.3, and 120.2, 63.2% increases in [3H]thymidine incorporation at 12, 24, 48, and 72 h of incubation, respectively, compared with cells exposed to normal glucose (a basic level of serum, here as a control). This effect was further enhanced when cells were exposed to intermittent high glucose medium, which caused 36.8, 101.3, and 157.9, 115.8% stimulation of [3H]thymidine incorporation compared with normal glucose conditions, respectively (Fig. 1).
These results indicate that intermittent high glucose appears to cause an additive stimulatory effect on proliferation of HRECs.
Effect of intermittent high glucose on expression of VEGF
Because VEGF has been shown to play an important role in the development of diabetic retinopathy, we examined whether intermittent high glucose enhance VEGF expression in HRECs. Quiescent cultures of HRECs were exposed to constant or intermittent high glucose condition for 48 h. VEGF protein and mRNA levels were assessed.
As shown in Fig. 2a, compared with normal glucose group, the concentration of VEGF protein was significantly increased (up to 176.2 ± 5.6%, P < 0.01) when HRECs were cultured in constant high glucose for 48 h. This effect was further enhanced following exposure of HRECs to intermittent high glucose with VEGF secretion increased (up to 254.7 ± 6.9%, p < 0.01) compared with cells exposed to constant normal glucose. There was a statistically significant increase in the protein content of VEGF exposed to intermittent high glucose compared with cells exposed to constant high glucose (p < 0.01).
The effect of high glucose on VEGF protein (a) and mRNA (b) expression in cultured HRECs. NG constant normal glucose (5 mmol/l), OC osmotic control (25 mmol/l mannose was used as a negative control), HG constant high glucose (25 mmol/l), N/HG 5 mmol/l alternating with 25 mmol/l glucose. Quiescent cells were exposed to glucose at different concentration for 48 h. VEGF protein and mRNA expression were assessed by ELISA and Northern blot analysis, respectively. VEGF protein levels are expressed as a percent of the value of NG (100%). “mRNA relative expression” means the ratio of VEGF over GAPDH. The data expressed as mean ± SD of at least five independent experiments. *P < 0.01 versus NG, # p < 0.01 versus HG
Both constant and intermittent high glucose significantly increased VEGF mRNA expression in HRECs compared with cells exposed to normal glucose (relative expression: 1.24 ± 0.04 vs. 0.72 ± 0.02, P < 0.01; 1.86 ± 0.06 vs. 0.72 ± 0.02, P < 0.01, respectively; Fig. 2b). Moreover, this effect was further enhanced in HRECs exposed to intermittent high concentrations than cells exposed to constant high glucose (1.86 ± 0.06 vs. 1.24 ± 0.04, P < 0.01, Fig. 2b).
Consistent with our data from the proliferations of HRECs, these results suggest that constant and intermittent high glucose treatment not only increases VEGF mRNA expression, but also increases its protein synthesis and secretion from HRECs, but in the intermittent high glucose condition the increase was more marked.
Effect of intermittent high glucose on levels of 8-OhdG, nitrotyrosine and mitochondrial ROS
After 48 h, when no oxidative stress inhibitory substance was added, the concentration of 8-OhdG and nitrotyrosine increased in the constant high glucose and more in intermittent high glucose in comparison with the normal glucose. The adding of the inhibitory substances, MnTBAP and TTFA equally prevented the increases of nitrotyrosine and 8-OhdG in the constant and intermittent high glucose condition as regards the same conditions where no inhibitor was added (Fig. 3a, b).
The effects of MnTBAP and TTFA on production of 8-OHdG (a), nitrotyrosine (b) and mitochondrial ROS (c) in HRECs cultured under intermittent or constant high glucose condition for 48 h. NG constant normal glucose (5 mmol/l), OC osmotic control (25 mmol/l mannose was used as a negative control), HG constant high glucose (25 mmol/l), N/HG 5 mmol/l alternating with 25 mmol/l glucose. The production of mitochondrial ROS are expressed as a percent of the value of NG (100%) The data expressed as mean ± SD of at least five independent experiments. *P < 0.01 versus NG, **P < 0.01 versus control
Similarly, after 48-h cultures, the amount of mitochondrial ROS increased both in the constant and intermittent high glucose, but in the latter the increase was more marked (Fig. 3c). The presence of the inhibitors (MnTBAP and TTFA) equally blocked the mitochondrial ROS overproduction in both the constant and intermittent high glucose conditions (Fig. 3c).
Role of ROS in proliferation of HRECs induced by intermittent high glucose
To examine a role for ROS in proliferation of HRECs induced by intermittent high glucose, quiescent HRECs were exposed to constant and intermittent high glucose for 48 h in the absence or presence of MnTBAP and TTFA, and then [3H]thymidine incorporation was assessed. MnTBAP and TTFA completely prevented the increase in [3H]thymidine incorporation induced by constant and intermittent high glucose (Fig. 4). MnTBAP and TTFA had no effect on [3H]thymidine incorporation under normal glucose or 25 mmol/l mannose conditions (Fig. 4).
Role of ROS in proliferation of cultured HREC induced by high glucose. NG constant normal glucose (5 mmol/l), OC osmotic control (25 mmol/l mannose was used as a negative control), HG constant high glucose (25 mmol/l), N/HG 5 mmol/l alternating with 25 mmol/l glucose. Quiescent cells were exposed to glucose at different concentration for in the absence or presence of MnTBAP or TTFA, and [3H]thymidine incorporation was assessed. The data expressed as mean ± SD of at least five independent experiments. **P < 0.01 versus control
Role of ROS in stimulation of VEGF expression in HRECs induced by intermittent high glucose
The quiescent HRECs were exposed to constant and intermittent high glucose for 48 h in the absence or presence of MnTBAP and TTFA, and then VEGF expression was assessed. The presence of the inhibitors (MnTBAP and TTFA) equally inhibited the overexpression of VEGF under constant and intermittent high glucose condition as regards the same conditions where no inhibitor was added (Fig. 5a, b). MnTBAP and TTFA had no effect on the expression of VEGF under normal glucose or high osmotic pressure conditions (Fig. 5).
Role of ROS in overexpression of VEGF protein (a) and mRNA (b) in cultured HRECs induced by high glucose. NG constant normal glucose (5 mmol/l), OC osmotic control (25 mmol/l mannose was used as a negative control), HG constant high glucose (25 mmol/l), N/HG 5 mmol/l alternating with 25 mmol/l glucose. Quiescent cells were exposed to glucose at different concentrations for in the absence or presence of MnTBAP or TTFA. VEGF protein and mRNA expression were assessed by ELISA and Northern blot analysis, respectively. VEGF protein levels are expressed as a percent of the value of NG (100%). “mRNA relative expression” means the ratio of VEGF over GAPDH. The data expressed as mean ± SD of at least five independent experiments. **P < 0.01 versus control
Discussion
This study has shown that cultured HRECs exposed to high glucose concentrations have increased cell proliferation, the expression of VEGF and the production of mitochondrial ROS, 8-OhdG and nitrotyrosine, as index of oxidative damage. Moreover, these effects were further enhanced in cells that were exposed to intermittent rather than constant high glucose. These findings suggest that variability in glycaemic control could be more deleterious to the HRECs than constant high glucose. Furthermore, inhibiting mitochondrial ROS with MnTBAP and TTFA reverses the exacerbated cell proliferation and overexpression of VEGF induced by intermittent high glucose. These findings suggest an important role of intermittent hyperglycemia in the initiation and/or development of diabetic retinopathy and demonstrate an important role of oxidative damage in mediating this process.
Angiogenesis may be a principle mechanism of tissue damage in specific pathological conditions, as is the case in proliferative diabetic retinopathy (PDR). Angiogenesis may be the most devastating outcome of growth factor alterations in PDR. Retinal changes in diabetes are thought to be initiated by sustained hyperglycemia leading to biochemical anomalies and alterations of various vasoactive factors and growth factors [6, 17, 18]. The primary target of glucose-induced dysfunction is endothelial cells and they are therefore most susceptible to proliferating signals [19, 20]. Growth factor alterations are believed to be important in both early and late stages of diabetic retinopathy. Endothelial cell damage is an important factor that may further aggravate a growth factor-mediated proliferative response, resulting in increased ECM deposition and basement membrane thickening [21]. Growth factors such as VEGF, stimulated by hyperglycemia and cellular degeneration, lead to further increased permeability and increased extracellular matrix protein deposition. In addition, various growth factors are involved in later stages of diabetic retinopathy, leading to proliferation and migration of endothelial cells and subsequent neovascularization [22, 23]. VEGF is considered to be the primary angiogenesis factor in this sequence of events [24, 25]. It is clear that alteration in VEGF expression is an important event that may in part be responsible for the development and progression of diabetic retinopathy to the proliferative stage.
In studying the cause of diabetic retinopathy, we have emphasized the effect of fluctuating hyperglycemia on the metabolic activity of HRECs. Consistent with in vitro studies of Premanand et al. [26], cultured HRECs exposed to high glucose conditions have increased cell proliferation and the expression of VEGF. More importantly, we have shown that the exposure of HRECs to intermittent high glucose significantly enhanced the effects of the exposure of such cells to constant high glucose, supporting a pathophysiologic link between intermittent high glucose and increased risk of microvascular complications [14, 27, 28]. Intermittent high glucose may be more dangerous for the cells than constant high glucose. Similarly, fluctuations of glucose display a more dangerous effect than stable high glucose on both tubulointerstitial cells and human renal cortical fibroblasts, in terms of cell proliferation [29, 30]. New diabetes therapies focused on reducing post-prandial hyperglycemia have become available and may benefit glycemic control and reduce risk of microvascular complications [14, 28]. It is now recognized that hyperglycemia at 2 h during an oral glucose challenge, as well as glucose fluctuations are strong predictor of microvascular complications [31], and it has been suggested that “hyperglycemic spikes” may play a direct and significant role in the pathogenesis of diabetic vascular complications [32].
Our present study showed that intermittent high glucose significantly enhanced the expression of VEGF, compared with constant high glucose, indicating a direct role for intermittent high glucose in the pathology of DR. Some studies in various models indicate that hyperglycemia in vivo or high glucose exposure in vitro induces the formation of angiogenic factors [33, 34]. While multiple growth factors and cytokines have been implicated in retinal neovascular diseases, VEGF has been identified as a primary mediator of the vascular alterations in diabetic retinopathy [3, 5]. Expression of VEGF is increased by hypoxia, oxidative stress, high glucose and inflammatory reactions. A number of clinical studies have shown a strong correlation between increases in intraocular VEGF concentration and the development of proliferative diabetic retinopathy [5]. Studies in streptozotocin diabetic rats have shown that retinal vascular alterations similar to background diabetic retinopathy in patients are associated with increases in retinal VEGF levels and increased expression of VEGF receptor [35, 36].
Currently four major biochemical pathways have been hypothesized to explain the mechanism of diabetic eye diseases all starting initially from hyperglycemia-induced vascular injury [37]. These mainly include enhanced glucose flux through the polyol pathway, increased intracellular formation of advanced glycation end-products (AGE), activation of PKC isoforms, and stimulation of the hexosamine pathway. Studies have suggested that these mechanisms seem to reflect a hyperglycaemia-induced process initiated by superoxide overproduction by mitochondrial electron transport chain [6]. Therefore, mitochondrial ROS overproduction is likely to be the central factor that induced other pathways of diabetic retinopathy.
The present study also addresses the signaling pathways responsible for dysfunction of HRECs induced by high glucose treatment. We found that constant high glucose produced an increase in oxidative stress generation. Moreover, the pathway involved in the damaging effect of intermittent high glucose on HREC is, at least in part, the same one working in constant high glucose concentrations. It appears noteworthy that it is enhanced in intermittent high glucose conditions. We confirm that intermittent glucose enhance oxidative stress generation and worsen the effects of high glucose on dysfunction of HRECs. The cell proliferation and VEGF expression are accompanied by increases of mitochondrial ROS, 8-OHdG and nitrotyrosine and can be prevented by the SOD mimetic MnTBAP. This study showed that inhibiting the mitochondrial electron transport complex II prevents the dysfunction HRECs induced by both constant and intermittent high glucose. The effect of TTFA, a specific antioxidant active at mitochondrial level, in normalizing cell proliferation and VEGF expression, as well as mitochondrial ROS, nitrotyrosine and 8-OHdG, was equivalent to those of MnTBAP suggesting that an overproduction of free radicals at mitochondrial level is the mediator of the dysfunction of HRECs. Actually, MnTBAP and SOD were active against ROS originating in different districts inside the cell. The fact that a specific mitochondrial oxidative stress inhibitor achieves the same results suggests that the major source of ROS inside the cell, due to high glucose exposition, is the mitochondrial electron transport chain. To be specific, TTFA selectively inhibits mitochondrial complex II activity; our findings support Brownlee theory: inhibition of entrance of electron to ubiquinone from complex II blocks off ROS generation, preventing all downstream processes.
At present, the molecular mechanisms specifically triggered on cultured HRECs by periodically changing glucose concentrations are not known. A possible explanation may be that during chronic exposure to high glucose, some metabolic variations induced by this constant situation might change or feed back regulatory cell controls, partially counteracting the glucose toxic effect. Intermittent exposure to high glucose might reduce such adaptation, causing more pronounced toxicity. El-Osta et al. [38] reported that transient exposure of aortic endothelial cells to hyperglycemia induces persistent epigenetic changes and leads to a sustained increase in expression of the NF-κB-responsive proatherogenic genes MCP-1 and VCAM-1. These epigenetic changes are caused by increased generation of methylglyoxal because of hyperglycemia-induced ROS formation by the mitochondrial electron transport chain. This finding is consistent with our observation that glycemic variability has important pathological effects on the development of diabetic complications dependent on mitochondrial ROS.
In conclusion, our study showing that the exposure to intermittent high glucose enhances cell proliferation and overexpression of VEGF in HRECs supports the hypothesis that glucose fluctuation may be involved in the development or progression of diabetic retinopathy. Moreover, our data suggest that this phenomenon is related to overproduction of mitochondrial superoxide in HRECs. However, this study is not without its limitations with regard to the extrapolation of findings to real-time situation in patients with diabetic retinopathy. First and foremost is the fact that the recent trials of measuring a variety of different surrogates in different models of both cell culture and patient experiments are not definitive proof of the role of glycemic variability in the pathogenesis of the vascular complications of diabetes [39, 40]. In addition, there are no prospective interventional studies providing evidence on the association between glucose variability and the development of diabetic vascular complications. Thus, further randomized controlled clinical trials are needed to better assess the association between glucose variability and the development of long-term diabetic complications.
References
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL (1984) The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol 102:520–526
Sjolie AK, Stephenson J, Aldington S, Kohner E, Janka H, Stevens L, Fuller J (1997) Retinopathy and vision loss in insulin-dependent diabetes in Europe. The EURODIAB IDDM complications study. Ophthalmology 104:252–260
Miller JW, Adamis AP, Aiello LP (1997) Vascular endothelial growth factor in ocular neovascularization and proliferative diabetic retinopathy. Diabetes Metab Rev 13:37–50
Simorre-Pinatel V, Guerrin M, Chollet P, Penary M, Clamens S, Malecaze F, Plouet J (1994) Vasculotropin-VEGF stimulates retinal capillary endothelial cells through an autocrine pathway. Invest Ophthalmol Vis Sci 35:3393–3400
Duh E, Aiello LP (1999) Vascular endothelial growth factor and diabetes: the agonist versus antagonist paradox. Diabetes 48:1899–1906
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, Yoerk MA, Beebe D, Oates PJ, Hammes HP et al (2000) Normalizing mitochondrial superoxide production blocks three pathways of hyperglycemic damage. Nature 404:787–790
Kowluru RA, Tang J, Kern TS (2001) Abnormalities of retinal metabolism in diabetes and experimental galactosemia. VII. Effect of long-term administration of antioxidants on the development of retinopathy. Diabetes 50:1938–1942
Kowluru RA, Engerman RL, Kern TS (2000) Abnormalities of retinal metabolism in diabetes or experimental galactosemia VIII. Prevention by aminoguanidine. Curr Eye Res 21:814–819
Kuroki M, Voest EE, Amano S, Beerepoot LV, Takashima S, Tolentino M, Kim RY, Rohan RM, Colby KA, Yeo KT, Adamis AP (1996) Reactive oxygen intermediates increase vascular endothelial growth factor expression in vitro and in vivo. J Clin Invest 98:1667–1675
Obrosova IG, Minchenko AG, Marinescu V, Fathallah L, Kennedy A, Stockert CM, Frank RN, Stevens MJ (2001) Antioxidants attenuate early up regulation of retinal vascular endothelial growth factor in streptozotocin-diabetic rats. Diabetologia 44:1102–1110
Klein R (1995) Hyperglycemia and microvascular and macrovascular disease in diabetes. Diabetes Care 18:258–268
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C (2006) Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295:1681–1687
Gimeno-Orna JA, Castro-Alonso FJ, Boned-Juliani B, Lou-Arnal LM (2003) Fasting plasma glucose variability as a risk factor of retinopathy in type 2 diabetic patients. J Diabetes Complicat 17:78–81
Quagliaro L, Piconi L, Assaloni R (2003) Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes 52:2795–2804
Xia P, Aiello LP, Ishii H, Jiang ZY, Park DJ, Robinson GS, Jiang ZY, Park DJ, Robinson GS, Jiang ZY et al (1996) Characterization of vascular endothelial growth factor’s effect on the activation of protein kinase C, its isoforms, and endothelial cell growth. J Clin Invest 98:2018–2026
Sheetz MJ, King GL (2002) Molecular understanding of hyperglycemia’s adverse effects for diabetic complications. JAMA 288:2579–2588
King GL, Brownlee M (1996) The cellular and molecular mechanisms of diabetic complications. Endocrinol Metab Clin North Am 25:255–270
De Vriese AS, Verbeuren TJ, Van de Voorde J, Lameire NH, Vanhoutte PM (2000) Endothelial dysfunction in diabetes. Br J Pharmacol 130:963–974
Hink U, Li H, Mollnau H, Oelze M, Matheis E, Hartmann M, Skatchkov M, Thaiss F, Stahl RA, Warnholtz A et al (2001) Mechanisms underlying endothelial dysfunction in diabetes mellitus. Circ Res 88:E14–E22
Williamson JR, Kilo C (1983) Capillary basement membrane in diabetes. Diabetes 32:96–100
D’Amore PA (1994) Mechanisms of retinal and choroidal neovascularization. Invest Ophthalmol Vis Sci 35:3974–3979
Sholley MM, Ferguson GP, Seibel HR, Montour JL, Wilson JD (1984) Mechanisms of neovascularization. Vascular sprouting can occur without proliferation of endothelial cells. Lab Invest 51:624–634
Witmer AN, Vrensen GF, Van Noorden CJ, Schlingemann RO (2003) Vascular endothelial growth factors and angiogenesis in eye disease. Prog Retin Eye Res 22:1–29
Gariano RF, Gardner TW (2005) Retinal angiogenesis in development and disease. Nature 438:960–966
Premanand C, Rema M, Sameer MZ, Sujatha M, Balasubramanyam M (2006) Effect of curcumin on proliferation of human retinal endothelial cells under in vitro conditions. Invest Ophthalmol Vis Sci 47:2179–2184
Kilpatrick ES, Rigby AS, Atkin SL (2009) The effect of glucose variability on the long-term risk of microvascular complications in type 1 diabetes. Diabetes Care 32:901–1903
Kilpatrick ES, Rigby AS, Atkin SL (2008) A1C variability and the risk of microvascular complications in type 1 diabetes: data from the Diabetes Control and Complications Trial. Diabetes Care 31:L2198–L2202
Jones SC, Saunders HJ, Qi W, Pollock CA (1999) Intermittent high glucose enhances cell growth and collagen synthesis in cultured human tubulointerstitial cells. Diabetologia 42:1113–1119
Takeuchi A, Throckmorton DC, Brogden AP (1995) Periodic high extracellular glucose enhances production of collagens III and IV by mesangial cells. Am J Physiol 268:F13–F19
Singleton JR, Smith AG, Russell JW, Feldman EL (2003) Microvascular complications of impaired glucose tolerance. Diabetes 52:2867–2873
Ceriello A (1998) The emerging role of post-prandial hyperglycaemic spikes in the pathogenesis of diabetic complications. Diabet Med 15:188–193
Chakrabarti S, Cukiernik M, Hileeto D, Evans T, Chen S (2000) Role of vasoactive factors in the pathogenesis of early changes in diabetic retinopathy. Diabetes Metab Res Rev 16:393–407
Sanchez-Elsner T, Botella LM, Velasco B, Corbi A, Attisano L, Bernabeu C (2001) Synergistic cooperation between hypoxia and transforming growth factor-beta pathways on human vascular endothelial growth factor gene expression. J Biol Chem 276:38527–38535
Hammes HP, Lin J, Bretzel RG, Brownlee M, Breier G (1998) Upregulation of the vascular endothelial growth experimental background diabetic retinopathy of the rat. Diabetes 47:401–406
Gilbert RE, Vranes D, Berka JL, Kelly DJ, Cox A, Wu LL, Stacker SA, Cooper ME (1998) Vascular endothelial growth factor and its receptors in control and diabetic rat eyes. Lab Invest 78:1017–1027
Balasubramanyam M, Rema M, Premanand C (2002) Biochemical and molecular mechanisms of diabetic retinopathy. Curr Sci 83:1506–1514
El-Osta A, Brasacchio D, Yao D, Pocai A, Jones PL, Roeder RG, Cooper ME, Brownlee M (2008) Transient high glucose causes persistent epigenetic changes and altered gene expression during subsequent normoglycemia. J Exp Med 205:2409–2417
Siegelaar SE, Holleman F, Hoekstra JB, DeVries JH (2010) Glucose variability: does it matter? Endocr Rev 31:171–182
Nalysnyk L, Hernandez-Medina M, Krishnarajah G (2010) Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes Metab 12:288–298
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, J., Xu, Y., Sun, S. et al. Intermittent high glucose enhances cell proliferation and VEGF expression in retinal endothelial cells: the role of mitochondrial reactive oxygen species. Mol Cell Biochem 343, 27–35 (2010). https://doi.org/10.1007/s11010-010-0495-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-010-0495-5