Abstract
The muscle Lim protein knock-out (MLP-KO) mouse model is extensively used for studying the pathophysiology of dilated cardiomyopathy. However, explanation is lacking for the observed long survival of the diseased mice which develop until adulthood despite the gene defect, which theoretically predestines them to early death due to heart failure. We hypothesized that adaptive changes of cardiac intracellular calcium (Ca 2+i ) handling might explain the phenomenon. In order to study the progression of changes in cardiac function and Ca 2+i cycling, myocardial Ca 2+i -transients recorded by Indo-1 surface fluorometry were assessed with concomitant measurement of hemodynamic performance in isolated Langendorff-perfused hearts of 3- and 9-month old MLP-KO animals. Hearts were challenged with β-agonist isoproterenol and the sarcoplasmic reticular Ca2+-ATPase (SERCA2a) inhibitor cyclopiazonic acid (CPA). Cardiac mRNA content and levels of key Ca2+ handling proteins were also measured. A decline in lusitropic function was observed in 3-month old, but not in 9-month old MLP-KO mice under unchallenged conditions. β-adrenergic responses to isoproterenol were similar in all the studied groups. The CPA induced an increase in end-diastolic Ca 2+i -level and a decrease in Ca2+-sequestration capacity in 3-month old MLP-KO mice compared to age-matched controls. This unfavorable condition was absent at 9 months of age. SERCA2a expression was lower in 3-month old MLP-KO than in the corresponding controls and in 9-month old MLP-KO hearts. Our results show time-related recovery of hemodynamic function and an age-dependent compensatory upregulation of Ca 2+i handling in hearts of MLP-KO mice, which most likely involve the normalization of the expression of SERCA2a in the affected hearts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cause of dilative cardiomyopathy is multifactorial [1]. The end stage of the disease is characterized by severe dilation of the left ventricular chamber and cardiac failure. Detailed information on cardiac alterations in earlier stages of the disease is scarce, but is vital to understand the precise pathophysiological mechanisms to develop effective therapeutic strategies. Unfortunately, this type of research is hampered by the lack of proper animal models mimicking the progress of human dilated cardiomyopathy. Commonly applied models, such as chronic infusion with isoproterenol [2], aortic banding [3], and high frequency pacing [4] only mimic a few aspects of the human disease. It is of note that about a decade ago, Arber et al. developed a transgenic mouse model being deficient in muscle LIM protein (MLP-KO), a striated muscle-specific Lim-only protein. Interestingly, this transgenic experimental model was found to express a great number of features of human dilated cardiomyopathy [5]. The importance of the MLP-KO model is underlined by the clinical observation that mutations of Z-disk proteins, including MLP, eventually result in overt cardiomyopathy in humans [6].
The transgenic MLP-KO model of dilated cardiomyopathy has been well characterized [7, 8]. Hemodynamic analysis of hearts of MLP-KO mice showed a sequential deterioration of cardiac function, i.e., reduction of positive and negative dP/dt max and ejection fraction, and loss of β-adrenergic function [5, 7, 9, 10]. Since both inotropy (+dP/dt max) and lusitropy (−dP/dt max) of the heart strongly depend on intracellular calcium (Ca 2+i ) cycling, determination of Ca2+-fluxes through sarcolemmal and sarcoplasmic reticular channels, as well as rate of removal of Ca2+ by transporters from the cytoplasm during the course of the disease is pivotal to understanding the cause of impaired mechanical function. In order to elucidate the etiological background of inotropy and lusitropy, studies have been performed on cardiomyocytes isolated from MLP-KO mice [7, 9, 11, 12] with conflicting results with regard to Ca 2+i handling.
The study of Arber et al. [5] on MLP-KO hearts also indicated the presence of an “early” and “adult” phenotype of mice deficient in muscle LIM protein. A substantial number of MLP-KO animals succumb soon after birth (early phenotype) while other littermates with an identical gene defect develop until adulthood (adult phenotype). There is no satisfactory explanation at hand for this phenomenon. Here, we hypothesize that timely adaptations of the Ca 2+i handling machinery in the cardiomyocyte are instrumental in the long survival of the adult phenotype MLP-KO mice.
The major aim of the present study was to determine cardiac Ca 2+i handling in conjunction with hemodynamic performance of MLP-KO mice, using an ex vivo perfused, intact heart model, and to explore whether age-related alterations in cardiac Ca 2+i handling might reflect a potential adaptive process to rescue MLP-KO mice from overt heart failure. In order to follow the progression of changes in Ca 2+i cycling and cardiac function, studies were performed on hearts from 3- and 9-month old animals. Hearts were challenged by either β-adrenergic stimulation (isoproterenol) or inhibition of sarcoplasmic reticulum (SR) Ca2+-ATPase (cyclopiazonic acid). Ca 2+i handling was determined by Indo-1 surface fluorometry. Moreover, cardiac mRNA expression and concentration of proteins involved in Ca 2+i handling, such as ryanodine receptor subtype 2 (RyR2), sarcoplasmic reticular Ca2+-ATPase subtype 2a (SERCA2a), its major regulator protein phospholamban (PLN), and sarcolemmal Na+–Ca2+ exchanger (NCX) were assessed.
Materials and methods
Animal model
The muscle Lim protein-deficient mice were examined at the age of 3 and 9 months. The background strain to the MLP−/− mice was a hybrid cross of 129/Sv and C57BL/6 strains [5, 13]. The breeding pairs were a generous gift by L. J. De Windt (Department of Cardiology, Cardiovascular Research Institute Maastricht, University of Maastricht, the Netherlands). Age-matched wild-type mice were used as controls. The animals were bred in our animal facility under SPF conditions. The mice were maintained at a 12-h light/12-h dark cycle with free access to food and water. Tail tip DNA-test was performed with PCR technology in one randomly selected mouse from each MLP-KO litter to confirm the presence of homozygote genotype for the modified MLP allele. Experiments on animals followed the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996). The study protocol was approved by the Laboratory Animals Committee of the Semmelweis University of Budapest.
Langendorff heart preparation—Indo-1 AM loading and fluorescence measurement
The procedure to measure hemodynamic parameters and fluorescence signals in a beating heart preparation was outlined previously in detail [14]. In short, at 3 and 9 months of age, the animals were anesthetized by 40 mg/kg i.p. pentobarbital (Nembutal—Sanofi, Budapest, Hungary). Hearts were quickly excised and mounted on a Langendorff perfusion apparatus, and perfusion was initiated with a modified Krebs-Henseleit solution, containing (in mM) NaCl (118), KCl (4.3), NaHCO3 (25), MgSO4 (1.2), KH2PO4 (1.2), Na-EDTA (0.5), CaCl2 (2.0), glucose (11), and pyruvate (5) (all chemicals purchased from Sigma, Budapest, Hungary), which was equilibrated with 95% O2 and 5% CO2. The temperature of the buffer was maintained at 37°C, and pH was adjusted to 7.4. The perfusion pressure was set to 70 mmHg. Left ventricular pressure was registered by inserting a balloon catheter in the left ventricle, and coronary flow was measured by an ultrasonic transducer (T-106, Transonic Systems Inc., Ithaca, NY, USA) inserted in the perfusion line.
Details of Indo-1 administration and optical measurement of Ca 2+i -transients were published elsewhere [15, 16]. In brief, hearts were loaded with 6.25 μM Indo-1 AM and were illuminated at 355 nm by a mercury arc lamp. The light emitted by Indo-1 was recorded at 400 nm (Ca 2+i -bound dye) and 506 nm (Ca 2+i -free dye) using a custom-made fluorometer. The fluorescence signals and the hemodynamic parameters were recorded and stored for off-line analysis (Haemosys, Experimetria, Budapest, Hungary).
After loading of Indo-1 the perfusate was supplemented with 0.6 mM probenecid (Sigma) to prevent dye-leakage from cardiomyocytes. After 15 min of dye-washout, the fluorescence signals were recorded in the basal state. Thereafter, the hearts were challenged with 5 nM isoproterenol (Sigma) infused via the aortic line. Heart rate, systolic, and diastolic pressure stabilized in about 5 min after start of infusion, at which stage the fluorescence signals were recorded. Cessation of isoproterenol infusion was followed by a 20-min stabilization period. After reaching control hemodynamic values, infusion with the SERCA2a inhibitor cyclopiazonic acid (CPA, 5 μM) (Sigma) was started. At steady state of CPA administration, the parameters were recorded again.
Data analysis and interpretation
Ca 2+i -transients were obtained by the ratiometric technique from 400 and 506 nm signals. Prior to calculation, the individual fluorescence signals were corrected for closed shutter background and tissue autofluorescence of the unloaded tissue (correction for redox changes of NAD(P)+/NAD(P)H). Changes of autofluorescence caused by the experimental interventions were tested in three unloaded hearts, but autofluorescent signals did not alter significantly from baseline values at either wavelength throughout the experimental procedure.
Ca 2+i -concentration ([Ca2+]i) was calculated with the formula determined by Grynkiewicz et al. [17]. The Indo-1 dissociation constant (K d) for calcium was determined previously at 844 nM [18]. The fluorescent ratios at zero [Ca2+]i (R min) and at saturating [Ca2+]i (R max) were determined in separate experiments. Three mouse hearts loaded with Indo-1 were treated with 20 μM BAPTA-AM to define R min , and three separate hearts were infused with 1 μM 4-bromo-calcium-ionophore (A23187) to determine R max. The calcium transient was assessed to determine systolic and diastolic [Ca2+]i and Ca 2+i -amplitude. Maximal rates of rise of [Ca2+]i (+d[Ca2+]i/dt max) and decline of [Ca2+]i (−d[Ca2+]i/dt max) were obtained as indices for the rate of Ca2+ release from and sequestration back into the SR, respectively. Representative tracings of calcium-transients and cyclic changes in left ventricular pressure in an isolated, perfused MLP-KO mouse heart are shown in Fig. 1.
Representative tracings of left ventricular pressure (P lv, dotted line) and Ca 2+i -transient (solid line) recorded on the isolated, perfused heart of a 3-month old MLP-KO mouse. The Ca 2+i -transient was obtained by calibrating the ratio of corrected 400 and 506 nm fluorescent signals recorded after Indo-1 loading
RNA isolation, reverse transcription, Quantitative Real-Time PCR (qPCR)
Tissue samples of the left ventricle were pulverized under liquid nitrogen using a mortar and pestle. Total RNA was isolated using TRIzol (Invitrogen, Paisley, UK) and quantified using NanoDrop ND-1000 (Peqlab, Erlangen, Germany). Three micrograms of total RNA were then reverse-transcribed into cDNA using 15 U of AMV reverse transcriptase (Promega, Madison, WI, USA) and 0.025 μg/μl random primers (Promega). qPCR was performed with the ABI Prism 7000 sequence detection system (Applied Biosystems, Foster City, CA. USA) using the TaqMan primers, probes, and the TaqMan universal PCR master mix protocol (Applied Biosystems): assay ID Mm00441524_m1 for mouse NCX (Slc8a1), Mm00465877_m1 for mouse RyR2, Mm00437634_m1 for mouse SERCA2a (Atp2a2), and Mm00452263_m1 for mouse PLN. As internal control, the transcript of glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was determined (assay ID Mm99999915_g1 for mouse GAPDH). Changes in relative mRNA expression were evaluated as described earlier [19] using the ΔΔCT method suggested by a protocol of Applied Biosystems.
Western blot analysis
Left ventricular tissue samples were pulverized in liquid nitrogen and aliquots of tissue powder were suspended in ice-cold Tris–EDTA buffer, containing (in mM) Tris (20), EDTA (1), and 1:100 dilution of protease inhibitor cocktail. This latter contained (in μM) 4-(2-aminoethyl)benzenesulfonyl fluoride (1000), aprotinin (0.8), leupeptin (20), bestatin (40), pepstatin A (15), and E-64 (14) (Sigma, Budapest, Hungary). Following sonication at 0°C, the suspension was centrifuged at 100,000×g at 4°C for 90 min. The pellet was then resuspended in ice-cold Tris–EDTA buffer containing 2% Triton X-100 (Sigma) and centrifuged again at 100,000×g at 4°C for 45 min. Samples of the supernatant were subsequently subjected to SDS-PAGE as described before [20]. Gels (8%) were loaded with equal amounts of 40 μg protein per lane and transferred to nitrocellulose membranes (BioRad, Hercules, CA, USA). Membranes were incubated with 1:50–1:100 dilution of primary rabbit antibodies against NCX and RyR2 (Chemicon, Billerica, MA, USA), SERCA2a (Novus, Littleton, CO, USA), and PLN (Santa Cruz, Santa Cruz, CA, USA); thereafter, secondary antibody labeling was performed using an anti-rabbit ABC kit (Vector Laboratories, Burlingame, CA, USA). Immuno-reactive bands were visualized by an ECL Western blotting detection kit (Pierce, Rockford, IL, USA) on light-sensitive film. In order to obtain negative controls, samples were also probed with primary antibodies preincubated with antigenic (control) peptides. In all cases, the specific staining was suspended by adding the control peptide. In order to assess equal loading, nitrocellulose membranes were stripped in 200 ml of Tris–HCl buffer (50 mM, pH 7.5) containing 2% SDS and β-mercapto-ethanol (0.1 mM) at 65°C for 1 h and were re-probed with a mouse anti-GAPDH antibody (Novus). Band density was quantified using a GelDoc instrument (BioRad) on films exposed and processed equally. Optical density values obtained were normalized to those of GAPDH of the same sample. The normalized values of the control hearts were set at 100%. Normalized densitometric values of several (n = 3–5) independent experiments were then averaged. In all cases, specific staining disappeared when the primary antibody was preincubated with the control peptide (findings not shown).
Statistics
Results are expressed as mean ± SEM. Three- and 9-month old MLP-KO and control groups were compared using ANOVA. For comparison of untreated, CPA-infused and isoproterenol-challenged values of the same hearts, repeated measurement ANOVA was used. Subgroup testing was carried out using Student–Neumann–Keuls post hoc test. A statistically significant difference of P < 0.05 was accepted throughout.
Results
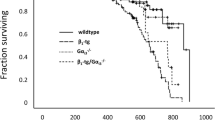
Survival rate, heart, and body mass
Approximately 60% of the MLP-KO animals died within 7 days after birth (early phenotype) in contrast to controls (15% death rate). The remaining MLP-KO animals, belonging to the adult phenotype, developed and behaved similar to the control animals: on the average, less than 10% of MLP-KO and controls were lost between 7 days and 9 months after birth. The surviving animals were included in the experiments at 3 and 9 months of age. Females, however, involved in the breeding program, died after a few pregnancies and were not included. All randomly selected MLP-KO mice proved to be homozygous for the mutant MLP gene on basis of the tail tip DNA test.
Heart and body mass did not differ significantly between control and MLP-KO mice either at 3 or 9 months of age. The ratio of heart to body mass, calculated as an index of cardiac hypertrophy, was not different between control and MLP-KO animals at either age (3-month old MLP-KO vs. control: 6.2 × 10−3 ± 0.4 × 10−3 vs. 5.8 × 10−3 ± 0.6 × 10−3, 9-month old MLP-KO vs. control: 6.2 × 10−3 ± 0.9 × 10−3 vs. 6.8 × 10−3 ± 1.0 × 10−3, g/g).
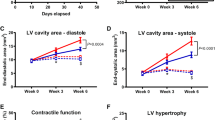
Hemodynamic function of isolated perfused hearts
Under unchallenged conditions, heart rate, left ventricular developed pressure, end-diastolic pressure, and contractility (+dP lv/dt max) did not differ among the groups studied (Table 1a; Fig. 2a). However, the lusitropic function (−dP lv/dt max) of 3-month old MLP-KO hearts was significantly lower when compared with hearts of controls of the same age (Fig. 2b). This difference could not be observed when comparing hearts of 9-month old MLP-KO with corresponding controls. Coronary flow was significantly higher both in the 3- and 9-month old MLP-KO hearts relative to age-matched controls (Table 1a).
Maximum rate of rise (a) and decline (b) of the left ventricular pressure and end-diastolic pressure values (c) of hearts isolated from control (open square, n = 6 and 6) and age-matched MLP-KO (filled square, n = 7 and 9) mice at 3 and 9 months of age, respectively, under unchallenged conditions, and at the end of 5 nM isoproterenol (ISO) or 5 μM cyclopiazonic acid (CPA) treatment. P lv left ventricular pressure. * Indicates significant difference between MLP-KO hearts and corresponding age-matched controls; # indicates significant difference between challenged and unchallenged conditions of corresponding MLP-KO hearts or controls (P < 0.05)
The β-adrenergic agonist isoproterenol (5 nM) produced significant elevation of heart rate, +dP lv/dt max and −dP lv/dt max (Table 1b; Fig. 2a, b). No differences between MLP-KO hearts and controls could be identified. Isoproterenol infusion hardly affected coronary flow compared to the unchallenged conditions with the exception of a small, but significant increase in the 3-month old MLP-KO hearts (Table 1b).
Exposure to the SERCA2-blocker CPA resulted in a significantly higher rise in end-diastolic left ventricular pressure in 3-month old MLP-KO hearts than in age-matched controls (85 and 14%, respectively) (Fig. 2c). This difference in response completely disappeared in hearts of animals at 9 months of age. CPA affected developed pressure also more severely in the 3-month old hearts compared to age-matched controls (Table 1c). The same holds for the decline in +dP lv/dt max, and −dP lv/dt max in CPA-treated, 3-month old hearts (Fig. 2a, b).
CPA challenge significantly decreased coronary flow in all experimental groups, whereas this intervention did not affect the difference between control and age-matched MLP-KO hearts (Table 1c).
Intracellular Ca2+ cycling
In unchallenged hearts, all characteristic parameters of the Ca 2+i -transient had similar values in MLP-KO and age-matched controls, both in the 3- and 9-month old hearts (Fig. 3a–c). During isoproterenol stimulation, end-diastolic [Ca2+]i, and both +d[Ca2+]i/dt max and −d[Ca2+]i/dt max were significantly elevated in the hearts of each group. No differences in response between control and MLP-deficient hearts could be observed (Fig. 3a–c).
Maximum rate of rise (a) and decline (b) of Ca2+-transients and the end-diastolic values of [Ca2+]i (c) in hearts isolated from control (open square, n = 6 and 6) and age-matched MLP-KO (filled square, n = 7 and 9) mice at 3 and 9 months of age, respectively, under unchallenged conditions, and at the end of 5 nM isoproterenol (ISO) or 5 μM cyclopiazonic acid (CPA) treatment. * Indicates significant difference between MLP-KO hearts and corresponding age-matched controls; # indicates significant difference between challenged and unchallenged conditions of corresponding MLP-KO hearts or controls (P < 0.05)
Exposure to CPA induced a significant elevation of end-diastolic [Ca2+]i in each of the studied groups (Fig. 3c). It is of note that the increase in end-diastolic [Ca2+]i in the 3-month old MLP-KO group significantly exceeded that of age-matched control hearts during CPA administration (238 and 112%, respectively). The striking difference in response to CPA between MLP-KO and controls disappeared at 9 months of age. CPA infusion significantly decreased +d[Ca2+]i/dt max in all but the 9-month old MLP-KO hearts (Fig. 3a). Moreover, −d[Ca2+]i/dt max was significantly reduced in 3-month old MLP-KO CPA-treated hearts; this effect was absent in 9-month old hearts (Fig. 3b).
mRNA and protein levels of proteins involved in Ca2+ cycling
The GAPDH-normalized mRNA expression of the major sarcoplasmic reticular Ca2+-releasing channel, RyR2, did not differ between 3-month old control and MLP-KO animals. At the age of 9 months, RyR2 mRNA level showed a minor, albeit significant reduction in MLP-KO hearts. In contrast, the RyR2 protein content was neither significantly different between the two 3-month old groups nor between the two 9-month old groups (Table 2).
Among the Ca2+-sequestering transporters, NCX mRNA expression was similar in each of the studied groups. The tissue protein content of NCX was also not statistically different among the various groups (Table 2).
In contrast, mRNA expression levels of SERCA2a were significantly lower in hearts of 3-month old MLP-KO mice than in age-matched control hearts (Fig. 4a). The SERCA2a mRNA expression in the 9-month old MLP-KO mice was significantly higher than that in the 3-month old MLP-KO animals and the difference between controls and MLP-KO hearts disappeared. A comparable pattern was observed in protein levels (Fig. 5). The SERCA2a protein concentration was also significantly lower in 3-month old MLP-KO hearts compared with corresponding, age-matched controls (Fig. 6a). A considerable (although not significant, i.e., P = 0.07) 60% increase was observed in cardiac SERCA2a protein levels of 9-month old MLP-KO mice compared with corresponding 3-month old animals. The SERCA2a protein expression did not significantly differ between 9-month old MLP-KO hearts and age-matched controls, strongly suggesting that SERCA2a normalized in 9-month old MLP-deficient animals both at the mRNA and protein level (Figs. 4a, 5, 6a).
SERCA2a (a) and PLN (b) mRNA expression normalized to GAPDH in hearts of control (open square, n = 6 and 6) and age-matched MLP-KO (filled square, n = 7 and 9) mice at 3 and 9 months of age, respectively. * Indicates statistically significant difference between MLP-KO and corresponding age-matched controls (P < 0.05). # Indicates statistically significant difference between 9-month old and corresponding 3-month old mice (P < 0.05)
Protein content of SERCA2a (a) and PLN (b) normalized to GAPDH in hearts of control (open square, n = 6 and 6) and MLP-KO (filled square, n = 7 and 9) mice at 3 and 9 months of age, respectively. * Indicates statistically significant difference between MLP-KO and corresponding age-matched controls (P < 0.05). # Indicates statistically significant difference between 9-month old and corresponding 3-month old mice (P < 0.05)
Similar to the SERCA2a mRNA and protein expression, the mRNA and protein levels of PLN were lower in 3-month old MLP-KO mice than in age-matched controls. Increased PLN expression was observed in hearts of 9-month old MLP-KO mice compared to the 3-month old hearts. This alteration was reflected by both mRNA and protein data. In 9-month old MLP-KO hearts PLN mRNA and protein concentrations exceeded those measured in age-matched control animals (Figs. 4b, 5, 6b).
Discussion
In their seminal paper on MLP-deficient mice, Arber et al. [5] pointed out that the animals showed two distinct phenotypes. The “early” phenotype is characterized by lethal changes in cardiac cyto-architectural organization; these animals die within 2 weeks after birth. The “adult” phenotype refers to littermate mice who developed to adulthood and were viable till the age of at least 9 months, despite the fact that they also lacked the MLP gene. It is of note that in the clinical setting hypertrophic cardiomyopathy caused by missense mutation of MLP are diagnosed late, i.e., at an average of 48 years [6]. One may speculate that in both situations, created either by knocking out MLP in mice or by mutation of MLP in patients, compensatory mechanisms are responsible for the late manifestation of heart failure. Until now, the precise nature of these adaptive mechanisms remained unexplained. Since calcium ions play a pivotal role in cardiac contractile performance, we hypothesized that beneficial, adaptive mechanisms during early life, resulting in compensation for the detrimental effects of the loss of MLP during later adulthood of MLP-KO mice, are related to the process of calcium handling in the affected heart.
In the past, several studies aimed to elucidate the pathological changes in Ca2+ cycling underlying inotropic and lusitropic dysfunction [7, 9, 11, 12]. These studies were performed on cardiomyocytes isolated from MLP-KO mice, and their outcomes were contradictory. Enhanced basal sarcoplasmic reticulum function [11, 12] and depressed calcium transients [7] were both reported. It should be realized, however, that the deviant findings could be caused by the experimental conditions applied. Isolated cardiomyocytes are different from those in the intact heart in terms of, for instance, mechanical loading, absence of extracellular matrix and specific conditions in the interstitial fluid. Our experiments were performed in an ex vivo perfused intact heart model which is closer to the in vivo situation than the isolated cardiomyocyte.
This study clearly shows that hearts of MLP-KO mice possess substantially lower SERCA2a mRNA and protein levels with concomitantly impaired lusitropic cardiac function at the age of 3 months, compared to age-matched healthy wild-type. At the age of 9 months, cardiac SERCA2a mRNA and protein expression, on the one hand, and the rate of relaxation, on the other, were undistinguishable from values of their wild-type littermates. These findings indicate that during aging, the MLP-KO mice are able to mobilize an adaptive mechanism most likely involving the expression of SERCA2a. The presence of an age-dependent adaptive process in the heart of the MLP-KO mice is also substantiated by earlier findings of Costandi et al. [13], indicating an improvement in both lusitropic and inotropic function of MLP-KO hearts in situ between 15 and 31 weeks of age.
The data presented here corroborate earlier observations in cardiomyocytes isolated from 6-month old MLP-KO hearts, showing normal to enhanced function of the sarcoplasmic reticulum [12]. Unfortunately, as no hearts of MLP-KO mice at a younger age were studied, no conclusion can be drawn from their study about the physiological significance of age-related changes in cardiomyocyte calcium handling.
The observation that Ca 2+i -transients (Fig. 3) in unchallenged, 3-month old MLP-KO hearts were not significantly different from those of age-matched controls underlines the complex relationship between cardiac calcium homeostasis and contractile performance. Normal Ca 2+i -transients with concomitantly decreased expression of SERCA2a indicates that, despite a decline in the number of functional SERCA2a, the cardiomyocyte is still able to pump Ca2+ back into the sarcoplasmic reticulum at a sufficiently high rate, in other words the pump reserve capacity of SERCA2a is not exhausted under these conditions. This phenomenon may, at least partially, be caused by the concomitantly decreased level of PLN (see below).
In addition, the apparent discrepancy between lusitropic function (declined) and rate of Ca2+ removal (normal) in 3-month old MLP-KO hearts may be caused by an enhanced calcium sensitivity of the contractile apparatus. Indeed, studies of Van der Velden et al. [21] strongly suggest that in the diseased heart the sensitivity of the contractile machinery toward cytoplasmic Ca2+ is increased, which could explain the decline in diastolic relaxation at apparently normal Ca 2+i -concentration and rhythmic changes therein.
In order to explore in more detail the relationship between SERCA2a, Ca 2+i -transients and contractile performance, isolated hearts of MLP-KO and control animals were exposed to the SERCA2a blocker CPA. The findings of this study clearly show that the 3-month old MLP-KO mouse heart is more sensitive to CPA treatment than the 9-month old heart, when compared to their age-matched controls. Both inotropic and lusitropic function were significantly affected (Fig. 2), and end-diastolic left ventricular pressure almost doubled after CPA treatment in 3-month old hearts. The effect of CPA on these functional parameters did not reveal major differences between MLP-KO and control hearts at the age of 9 months, again strongly suggesting the presence of a calcium-related compensatory mechanism during aging of the “adult” MLP-KO phenotype. This notion is supported by the observation that the detrimental effect of CPA on the reuptake of Ca2+ into the SR, as reflected by −d[Ca2+]/dt max (Fig. 3b) is very pronounced at the age of 3 months and virtually absent in 9-month old MLP-KO hearts. The same holds for the parameter reflecting the end-diastolic cytoplasmic Ca2+ concentration. The enhanced sensitivity toward CPA in 3-month old MLP-KO hearts can be explained by the lower cardiac SERCA2a mRNA and protein expression in these animals (Figs. 4a, 6a).
SERCA2a activity cannot be judged without considering the changes in the level of the major SERCA2a regulatory PLN and its level of phosphorylation. Alterations in PLN mRNA and protein levels followed the same pattern as the changes of SERCA2a mRNA and protein profiles (Figs. 4, 5, 6). At 3 months of age, PLN expression was lower in MLP-KO hearts, and its level of expression increased by a similar rate as SERCA2a expression till the age of 9 months. This finding is in agreement with those studies, which also showed that SERCA2a and PLN expression change parallel in different cardiac failure models [22, 23]. In 9-month old MLP-KO animals, the expression of PLN was higher than in age-matched controls. This was not reflected by enhanced SERCA2a inhibition, as at this age normalization of lusitropic dysfunction could be observed, and the increased susceptibility of diastolic calcium concentration to CPA administration disappeared. This phenomenon could be caused by an altered degree of phosphorylation of PLN, but this issue was not examined in the present study.
Davidson and Koch observed a persistent decline in β-adrenergic receptor activity in MLP-KO hearts. In their study, they were able to normalize the β-adrenergic responses by expressing a cardiac-targeted transgene, which blocks the function of β-adrenergic receptor kinase-1 (βARK1) [24]. Since enhanced activity of βARK1 inhibits the β-adrenergic receptor activity, deletion of βARK1 is supposed to increase the functionality of the β-adrenergic receptor [25]. It is of note, however, that in this study on intact hearts exposed to isoproterenol to activate the β-adrenergic receptor, no differences were found in the effect of isoproterenol either on hemodynamic parameters or on dynamic parameters of the Ca 2+i -transients between the MLP-KO and age-matched control hearts in both the 3- and 9-month old groups (Table 1b; Figs. 2, 3). Our findings are, therefore, not compatible with a persistent decline in β-adrenergic receptor activity as previously observed [24]. The apparent discrepancy between the outcomes of the two studies is incompletely understood; other downstream changes in the signaling cascade may be involved.
Alterations in Ca 2+i handling could theoretically also be explained by changes in the function and/or expression of other Ca 2+i handling proteins such as NCX and RyR2. Although altered function of these proteins cannot be excluded, our data do not provide evidence for major differences in NCX and RyR2 protein levels between MLP-KO and control hearts. The findings presented here are in agreement with those of Antoons et al. [11], who also failed to show change in NCX levels of 3-month old MLP-KO heart.
We were intrigued by the novel observation that in the unchallenged heart of the MLP-KO mice coronary flow was significantly higher than in age-matched controls. On average, in the hearts of 3-month old mice, flow was increased by about 61% due to coronary dilatation, resulting in a surplus coronary flow since cardiac mechanical function and, hence, expected cardiac energy demand, did not differ to a significant extent. This observation might point to a loss of efficiency in the conversion of chemical into mechanical energy, the precise mechanism of which remains elusive. It is of note that Van den Bosch and colleagues showed that mitochondrial dysfunction is clearly evident in MLP-KO mice leading to energy deficiency [26] which may explain the significantly higher coronary flow in 3-month old MLP-KO animals compared to controls. As the percentage increase in coronary flow declined to 29% at the age of 9 months, cardiac energetic efficiency may improve during maturation of the affected mice.
In summary, the findings of this study suggest that in the adult phenotype of MLP-deficient hearts, the initial changes in Ca 2+i handling, as observed at 3 months of age, could be rescued by compensatory mechanisms later in life. These mechanisms may exert a beneficial effect on cardiomyocyte Ca 2+i homeostasis and, hence, contractile properties, as seen in hearts of 9-month old MLP-KO mice. The beneficial mechanisms might involve the normalized expression of SERCA2a in the affected heart. The findings of this study also indicate a transient decline in efficiency in the hearts of surviving MLP-deficient mice. Overall, age-related alterations in cardiac Ca 2+i handling might offer a potential adaptive process to rescue MLP-KO mice from early heart failure.
References
Sipido KR, Eisner D (2005) Something old, something new: changing views on the cellular mechanisms of heart failure. Cardiovasc Res 68:167–174
Linck B, Boknik P, Baba HA, Eschenhagen T, Haverkamp U, Jackel E, Jones LR, Kirchhefer U, Knapp J, Laer S, Müller FU, Schmitz W, Scholz H, Syska A, Vahlensieck U, Neumann J (1998) Long-term beta adrenoceptor-mediated alteration in contractility and expression of phospholamban and sarcoplasmic reticulum Ca2+-ATPase in mammalian ventricle. J Pharmacol Exp Ther 286:531–538
Boluyt MO, Robinson KG, Meredith AL, Sen S, Lakatta EG, Crow MT, Brooks WW, Conrad CH, Bing OHL (2005) Heart failure after long-term supravalvular aortic constriction in rats. Am J Hypertens 18:202–212
Pogwizd SM, Qi M, Yuan W, Samarel AM, Bers DM (1999) Upregulation of Na+/Ca2+ exchanger expression and function in an arrhythmogenic rabbit model of heart failure. Circ Res 85:1009–1019
Arber S, Hunter JJ, Ross J Jr, Hongo M, Sansig G, Borg J, Perriard JC, Chien KR, Caroni P (1997) MLP-deficient mice exhibit a disruption of cardiac cytoarchitectual organization, dilated cardiomyopathy, and heart failure. Cell 88:393–403
Bos JM, Poley NP, Ny M, Tester DJ, Xu X, Vatta M, Towbin JA, Gersh BJ, Ommen SR, Ackerman MJ (2006) Genotype-phenotype relationships involving hypertrophic cardiomyopathy-associated mutations in titin, muscle LIM protein and telethonin. Mol Genet Metab 88:78–85
Esposito G, Santana LF, Dilly K, Crus JD, Mao L, Lederer WJ, Rockman HA (2000) Cellular and functional defects in a mouse model of heart failure. Am J Physiol Heart Circ Physiol 279(6):H3101–H3311
Minamisawa S, Hoshijima M, Chu G, Ward CA, Frank K, Gu Y, Martone ME, Wang Y, Ross J, Kranias EG, Giles WR, Chien KR (1999) Chronic phospholamban-sarcoplasmic reticulum calcium ATPase interaction is the critical calcium cycling defect in dilated cardiomyopathy. Cell 99:313–322
Lorenzen-Schmidt I, Stuyvers BD, Keurster HEDJ, Date M, Hoshijima M, Chien KR, McCulloch AD, Omens JH (2005) Young MLP deficient mice show diastolic dysfunction before the onset of dilated cardiomyopathy. J Mol Cell Cardiol 39:241–250
Omens JH, Usyk TP, Li Z, McCulloch AD (2002) Muscle LIM protein deficiency leads to alterations in passive ventricular mechanics. Am J Physiol Heart Circ Physiol 282:H680–H687
Antoons G, Vangheluwe P, Volders PGA, Bito V, Holemans P, Ceci M, Wuytack F, Caroni P, Mubagwa K, Sipido KR (2006) Increased phospholamban phosphorylation limits the force-frequency response in the MLP−/− mouse with heart failure. J Mol Cell Cardiol 40:350–360
Su Z, Yao A, Zubair I, Sugishita K, Ritter M, Li F, Hunter JJ, Chien KR, Barry WH (2001) Effects of deletion of muscle LIM protein on myocyte function. Am J Physiol Heart Circ Physiol 280(6):H2665–H2673
Costandi PN, Frank LR, McCulloch AD, Omens JH (2006) Role of diastolic properties in the transition to failure in a mouse model of the cardiac dilatation. Am J Physiol Heart Circ Physiol 291:H2971–H2979
Ivanics T, Miklos Z, Dezsi L, Ikrenyi K, Toth A, Roemen TH, Van der Vusse GJ, Ligeti L (2001) Concomitant accumulation of intracellular free calcium and arachidonic acid in the ischemic-reperfused rat heart. Mol Cell Biochem 226(1–2):119–128
Op den Buijs J, Miklos Z, van Riel NAW, Prestia CM, Szenczi O, Tóth A, Van der Vusse GJ, Ligeti L, Ivanics T (2002) Beta-adrenergic activation reveals impaired cardiac calcium handling at early stage of diabetes. Life Sci 76:1083–1098
Op den Buijs J, Ligeti L, Ivanics T, Miklos Z, Van der Vusse GJ, Van Riel NAW (2008) Mathematical modelling of the calcium–left ventricular pressure relationship in the intact diabetic rat heart. Acta Physiol 193:205–217
Grynkiewicz G, Poenie M, Tsien RY (1985) A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260(6):3440–3450
Bassani JW, Bassani RA, Bers DM (1995) Calibration of indo-1 and resting intracellular [Ca2+]i in intact rabbit cardiac myocytes. Biophys J 68(4):1453–1460
Bodó E, Bíró T, Telek A, Czifra G, Griger Z, Tóth IB, Mescalchin A, Ito T, Bettermann A, Kovács L, Paus R (2005) A “hot” new twist to hair biology—involvement of vanilloid receptor-1 (VR1/TRPV1) signaling in human hair growth control. Am J Pathol 166(4):985–998
Fülöp L, Bányász T, Szabó G, Tóth IB, Bíró T, Lőrincz I, Balogh Á, Pető K, Mikó I, Nánási PP (2006) Effect of sex hormones on ECG parameters and expression of cardiac ion channels in dogs. Acta Physiol (Oxf) 188(3–4):163–171
Van der Velden J, Papp Z, Boontje NM, Zaremba R, de Jong JW, Janssen PML, Hasenfuss G, Stienen GLM (2003) The effect of myosin light chain 2 dephosphorylation on Ca2+-sensitivity of force is enhanced in failing human hearts. Cardiovasc Res 57:505–514
Qi MY, Feng Y, Dai DZ, Li N, Cheng YS, Dai Y (2010) CPU86017, a berberine derivative, attenuates cardiac failure through normalizing calcium leakage and downregulated phospholamban and exerting antioxidant activity. Acta Pharmacol Sin 31(2):165–174
Kiss E, Ball NA, Kranias EG, Walsh RA (1995) Differential changes in cardiac phospholamban and sarcoplasmic reticular Ca2+-ATPase protein levels. Effects on Ca2+ transport and mechanics in compensated pressure-overload hypertrophy and congestive heart failure. Circ Res 77:759–764
Davidson MJ, Koch WJ (2001) Genetic manipulation of β-adrenergic signalling in heart failure. Acta Physiol Scand 173:145–150
Rockman HA, Chien KR, Choi DJ, Iaccarino G, Hunter JJ, Ross JJ, Lefkowitz RJ, Koch WJ (1998) Expression of a beta-adrenergic receptor kinase 1 inhibitor prevents the development of myocardial failure in gene-targeted mice. Proc Natl Acad Sci USA 95:7000–7005
Van den Bosch BJC, van den Burg CMM, Schoonderwoerd K, Lindsey PJ, Scholte HR, de Coo RFM, van Rooij E, Rockman HA, Doevendans PA, Smeets HJM (2005) Regional absence of mitochondria causing energy depletion in the myocardium of muscle LIM protein knockout mice. Cardiovasc Res 65:411–418
Acknowledgments
The authors acknowledge the excellent technical assistance of Margit Kerék and Judit Fábián. This study was supported by grants from OTKA (K61694 and F68502), Hungary.
Author information
Authors and Affiliations
Corresponding author
Additional information
László Ligeti—deceased.
Rights and permissions
About this article
Cite this article
Kemecsei, P., Miklós, Z., Bíró, T. et al. Hearts of surviving MLP-KO mice show transient changes of intracellular calcium handling. Mol Cell Biochem 342, 251–260 (2010). https://doi.org/10.1007/s11010-010-0492-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-010-0492-8