Abstract
Free fatty acids (FFA)-induced proliferation and apoptosis was studied in human umbilical vein endothelial cells (HUVECs). A recombinant adenovirus containing a RNAi cassette targeting the GSK-3β gene was produced and its silencing effect on GSK-3β gene was detected by Western blot analysis and immunohistochemistry assay in HUVECs. The effect of the RNAi on the protein level of β-catenin was explored by transfecting the RNAi adenovirus to inhibit the expression of GSK-3β protein. The subsequent effect on the Wnt/GSK-3β/β-catenin signal pathway and on proliferation and apoptosis of HUVECs cultured with FFAs, was analyzed by BrdU assay, Annexin V-FITC/PI Apoptosis Detection Kit, and 4′,6-diamidino-2- phenylindole(DAPI) to explore the possible connection between the signaling pathway and FFA-induced proliferation and apoptosis. The Western blot results showed that the expression of GSK-3β protein in HUVECs could be inhibited efficiently by the RNAi adenovirus, and that the protein level of β-catenin was increased by RNAi adenovirus transfection. The results of the BrdU assay suggested that knockdown of GSK-3β with the RNAi adenovirus may stimulate the proliferation of HUVECs. Apoptosis was observed in HUVECs exposed to FFAs (0.75 mmol/L) for 72 h, and this effect could be partly reversed when interfering with the RNAi adenovirus. It may be concluded that the RNAi adenovirus specific to GSK-3β may partly protect HUVECs from apoptosis induced by FFAs, probably through the up-regulation of the Wnt/β-catenin signal pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple factors, including hyperglycemia, hyperlipidemia, inflammatory factors, oxidative stress, and ROS have been identified as key players in the pathogenesis of the vascular complications of diabetes. These factors initiate various signaling pathways that include NF-κB, p38 MAPK, JNK/STAT, AGE/RAGE, polyols (e.g., sorbitol), and hexosamine. Recently, it has been proposed that the canonic Wnt signaling pathway (Wnt/GSK3β/β-catenin) is also involved in this complex signal network [1–4]. Wnt proteins are secreted signaling factors that play critical role in regulating a number of proliferative, apoptotic, and developmental processes. The currently discovered vertebrate Wnt family comprises 20 members. Wnt proteins act by binding to Frizzled and low density lipoprotein receptor-related protein cell surface receptors. Upon Wnt binding, Frizzled receptors transduce signals through the β-catenin-LEF/TCF pathway, Ca2+-calmodulin-PKC pathway, or JNK-dependent pathway. The β-catenin-LEF/TCF pathway is the best characterized to date and is conserved from Drosophila to humans. In the absence of Wnt binding to Frizzled receptors, β-catenin is found to form complexes with cytoplasmic proteins such as glycogen synthase kinase 3β, Axin, and adenomatous polyposis coli (APC), and remains phosphorylated. Phosphorylated cytoplasmic β-catenin molecules become ubiquitinated and are directed for proteasome-assisted degradation. On the other hand, when Wnt proteins bind to the receptors, degradation is inactivated and a “free” form of β-catenin accumulates in the cytoplasm. Accumulated β-catenin molecules translocate to the nucleus and serve as a co-activator of resident LEF/TCF transcriptional factors, resulting in complexes that bind to response sequences and modulate expression of target genes [5]. Fan et al. found that activation of β-catenin signal pathway could protect against endothelial cell apoptosis [6]. Choi et al. used the lithium, a GSK-3 inhibitor in palmitate-induced HUVEC apoptosis research, showed a strong protective effect. Pretreatment with other GSK-3beta inhibitors, e.g., SB216763 or TDZD-8, as well as adenoviral transduction with a catalytically inactive GSK-3β had significant protective effects against palmitate-induced HUVEC apoptosis [7]. In this study, we constructed an adenoviral RNAi expression vector targeting GSK3β, the key factor in the Wnt pathway, to explore the influence of Wnt signaling on high free fatty acid (FAA)-induced proliferation and apoptosis in human umbilical vein endothelial cells (HUVECs).
Methods and procedures
Cell culture
HEK 293A Cells (Invitrogen) were cultured in DMEM (high glucose) supplemented with 10% fetal calf serum, 2 mM glutamine, and non-essential amino acids. Cells were kept at 37°C in 5% CO2 with 100% humidity and were trypsinized and passaged when at 80–90% confluence.
Primary cultures of HUVECs were obtained from umbilical veins from healthy women after laparotomy. The lumen of each vein was washed 2–3 times with PBS to remove the remaining blood. Pre-warmed collagenase II (10–15 ml) injected into the lumen was incubated at 37°C for 16 min. After terminating the digestion with 4 ml fetal calf serum, the lumen was washed using 40–50 ml sterile PBS. The wash-out was centrifuged at 6,000g for 10 min and HUVECs were collected after discarding the supernatant. HUVECs were cultured in M199 with 20% fetal calf serum. After the cells adhered to the dishes, direct immunostaining for factor VIII was conducted to confirm that over 98% cells were endothelial. The third generation of cells was used for assays.
Preparation of free fatty acids (FFA)
FFA stock was a mixture of oleic acid and palmitic acid with a molar ratio of 2:1, and was prepared as follow: dissolve oleic and palmitic acid in 10 ml 99% ethanol and mix for 1 h, then add 40 μl 10 M NaOH to 10 ml FFA, mix, dry overnight in a laminar flow hood, then add 10 ml distilled water and heat until it was transparent and soap-like, and finally mix it with 40 ml pre-cooled lipid-free BSA. The FFA stock was sterilized by filtering through a 0.22-μm filter and stored at −20°C.
Construction of adenoviral RNAi expression vectors
Lipofectamine 2000 and the adenoviral transfection vector, BLOCK-iTTM Adenoviral RNAi Expression System, were from Invitrogen. Based on the GSK3β mRNA sequence from Genbank (NM_002093.2 GI: 21361339), three RNAi starting points (382, 640, and 1457) were selected to synthesize three pairs of short hairpin RNA (shRNA) oligonucleotides of 21 base pairs each (Table 1). Single-stranded oligonucleotides were annealed and ligated with linearized pENTRTM/U6. The product was selected on agarose plates with kanamycin and characterized by PCR and sequencing to isolate correct clones. Isolated plasmid DNAs were named pEntry640 and pEntry1457. They were then recombined with an adenoviral backbone vector, and the recombinants were selected on agarose plates with ampicillin and then characterized by PCR. From clones double selected on agarose plates with kanamycin and ampicillin, successfully recombined plasmid DNAs were isolated and named pAd640 and pAd1457. Adenoviral backbone vector without recombination was named pAd-DEST.
The plasmids pAd640, pAd1457, and pAd-DEST were digested by PacI, purified, and transfected into HEK 293A cells using Lipofectamine 2000. Between 7 and 9 days after transfection, cytopathic effect (CPE) cells reached 80% of the total cells. Cells were then collected and freeze-thawed three times; the supernatant was the original virus solution. Viruses were amplified two times by infecting HEK 293A cells with the original virus solution. The supernatants of third generation viruses were collected and named Ad-DEST, Ad-640, and Ad-1457, respectively. Virus titers were measured by plaque assay through infection of HEK 293A cells with the third generation viruses.
Western blot for protein levels targeted by RNAi adenovirus
In order to measure the effect of RNAi Adenovirus on GSK3β protein expression in HUVECs, healthy third generation HUVECs were digested with 0.25% trypsin, counted, seeded at 1.0 × 106 cells/6 ml dish, and infected with adenovirus (Ad-DEST, Ad-640, or Ad-1457) at 0, 25, 50, 100, 150, or 200 MOI. Cellular proteins were obtained 72 h after infection. Then, HUVECs were infected with adenovirus (Ad-DEST, Ad-640, or Ad-1457) at 50 MOI and the cellular proteins were collected at 0, 24, 48, 72, 96, 120, and 144 h after infection. Western blots were conducted to monitor the GSK3β protein levels of HUVECs in response to adenoviral infection in terms of different viral MOI or time. The first antibody was mouse-anti-human GSK3β monoclonal antibody at 1: 2,500 dilution, and the results were normalized to GADPH immunostaining.
In order to measure the effect of GSK3β knockdown on β-Catenin protein expression, healthy third generation HUVECs were digested with 0.25% trypsin, counted, seeded at 1.0 × 106 cells/6 ml dish, and infected with adenovirus (Ad-DEST, Ad-640, or Ad-1457) at 50, 100, or 200 MOI. Cellular proteins were obtained 0, 72, 96, 120, and 144 h after infection. Western blotting was conducted to monitor the β-catenin protein levels of HUVECs in response to adenoviral infection in terms of different viral MOI or time. The first antibody was mouse-anti-human β-Catenin monoclonal antibody at 1:500 dilution, and the results were normalized to GADPH immunostaining.
Immunohistochemical analysis of GSK3β and β-catenin protein levels in response to RNAi adenovirus
Healthy third generation HUVECs were digested with 0.25% trypsin, counted, and seeded into a coverslip in a 6-well tissue culture plate. On the next day, RNAi adenovirus (Ad-640) was used to infect HUVECs at 50 MOI in multiple wells. Normal cells and cells infected with -DEST were included as controls. After 72 h, GSK3β and β-catenin protein levels were assayed by immunohistochemical staining with mouse-anti-human GSK3β monoclonal antibody (1:100) and mouse-anti-human β-catenin monoclonal antibody (1:150).
HUVEC proliferation examined by BrdU
Our experiments were divided into three test groups and a control group: (1) FFA: 0.5, 0.75, and 1.0 mM; (2) RNAi Adenovirus: Ad-640 and Ad-DEST; (3) Ad-640 + FFA and Ad-DEST + FFA; (4) normal cells. Experiments were conducted in 96-well plates with three repeats at each time point (0, 24, 48, 72, and 96 h after infection).
For the BrdU assay the medium was replaced at 0, 24, 48, 72, and 96 h after infection with 100 μl/well DMEM containing 10% fetal calf serum. At each time point to be tested, 20 μl/well BrdU working solution was added, and cells were cultured 24 h in 5% CO2 at 37°C. Then, the medium was discarded and fix solution was added (200 μl/well). After 30 min incubation at room temperature, fix solution was discarded, and BrdU antibody was added (100 μl/well). Cells were incubated at room temperature for 1 h then washed three times with wash buffer. Peroxidase-labeled goat-anti-mouse IgG complex was added (1:1,000; 100 μl/well) and incubated for 30 min at room temperature. Cells were then washed three times with wash buffer. Substrate was added (100 μl/well) and incubated in darkness for 15 min at room temperature. Afterwards, termination buffer was added (100 μl/well) to terminate the reaction. Within 30 min, the absorptions at dual wavelengths 450–595 nm were measured.
HUVEC apoptosis analysis by annexin V-FITC apoptosis detection kit
Our experiments were divided into three test groups and a control group: (1) FFA: 0.75 mM; (2) RNAi Adenovirus: Ad-640 and Ad-DEST; (3) Ad-640 + FFA and Ad-DEST + FFA; (4) normal cells. Experiments were repeated three times on 6 cm plates.
Healthy third generation HUVECs were digested with 0.25% trypsin, counted, and seeded into a coverslip in a 6-well tissue culture plate and 6 cm plates. Cells were detected 48 h after infection: (1) Wash cells with 1× PBS, discard the supernatant repeat for a total of 2–3 washes; (2) Resuspend the cell pellet in 1× Binding Buffer to a final concentration of 2–5 × 105 cells/ml; (3) Transfer 195 μl cell suspension to a clean tube and add 5 μl Annexin V-FITC. Mix and incubate for 10 min at room temperature; (4) Wash the cells with 1× Binding Buffer and centrifuge at 1,000 rpm to pellet the cells. Discard the supernatant; (5) Resuspend the cell pellet in 190 μl 1× Binding Buffer and add 10 μl Propidium Iodide (final concentration = 1 μg/ml); (6) The coverslip was analyzed by fluorescence microscopy, and cells of the 6-cm plates was analyzed by flow cytometry.
HUVEC apoptosis analysis by DAPI staining
Our experiment groups were divided the same as above. Healthy third generation HUVECs were digested with 0.25% trypsin, counted, and seeded into a coverslip in a 6-well tissue. Cells were detected 72 h after infection by DAPI Staining: (1) Dilute the DAPI stock solution to 30 nM in PBS. Pipet 300 μL of this staining solution directly onto the cells. (2) Incubate the specimen in the dark for 30 min at room temperature. (3) Remove the coverslip and rinse the specimen with PBS or ddH2O to remove unbound dye. (4) Remove excess liquid from the slide. (5) View the sample using a fluorescence microscope with appropriate filters.
Materials
DMEM (high glucose), M199, and fetal calf serum were from Gibco. Collagenase II and gelatin were from Sigma. Oleic acid, palmitic acid, lipid-free BSA, and the BrdU Cell Proliferation assay were from Merck-Calbiochem. The Mouse-anti-human GSK3β and mouse-anti-human β-catenin antibodies were from BD Biosciences. Annexin V-FITC Apoptosis Detection Kit was from Merck-Calbiochem (Cat.No.CBA059); DAPI was from Roche (Cat.No.D8200).
Statistical analysis
Statistical analysis was carried out with SPSS 13.0 software. Data were presented as mean ± SD. Comparison between different time points and groups were conducted by square analysis with P < 0.05 as statistically meaningful and P < 0.01 as statistically significant.
Results
Construction of adenoviral RNAi expression vectors
PCR was used for identification of pEntry and pAd, pEntry was also sequenced. The result showed the size and open reading frame of pEntry640 and pEntry1457 were correct (292 bp). The clones (pAd) with correct recombination were 600 bp. The sequence of the vector with inserted shRNA was the same as designed by the software. Virus was titrated by the virus plaque assay. Results were showed as follows (Table 2).
Immunohistochemical analysis of GSK3β and β-Catenin protein levels in response to RNAi adenovirus
Our RNAi adenovirus significantly inhibited GSK3β expression 72 h after infection at 50 MOI (Fig. 1a), at the same time increased the protein level of intracellular β-catenin (Fig. 1b).
Western blot for protein levels of GSK3β targeted by RNAi adenovirus
A significant difference in GSK3β expression was detected in the RNAi adenovirus group at different MOIs (P < 0.01), especially at MOI 25–50, whereas no significant difference was detected in the Ad-DEST group at different MOIs (P > 0.05) (Fig. 2a, b). The results suggested expression of GSK3β protein significantly decreased between 48 and 144 h after RNAi infection (P < 0.01). There were no obvious changes in Ad-DEST group (P > 0.05) (Fig. 2c, d).
a The effect of Ad-Dest on the expression of GSK-3β in HUVEC with different MOI; b The effect of Ad-640 on the expression of GSK-3β in HUVEC with different MOI; c The effect of Ad-640 on the expression of GSK-3β in HUVEC at different time after infection; d The effect of Ad-DEST on the expression of GSK-3β in HUVEC at different time after infection; e The effect of Ad-640 on the protein level ofβ-catenin in HUVEC with different MOI at different time after infection; f The effect of Ad-DEST on the protein level of β-catenin in HUVEC with different MOI at different time after infection
Western blot for protein levels of β-catenin after RNAi adenoviral infection
The protein level of β-catenin was increased after the infection of RNAi adenovirus, with the effect that was obvious as early as 72 h after infection at MOI 50, and the increase was more pronounced with the increase of MOI and the time of infection (Fig. 2e, f).
HUVECs proliferation examined by BrdU
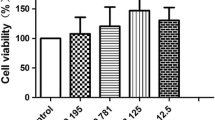
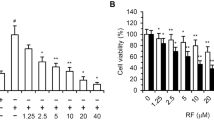
Results are shown in Table 3 and Fig. 3. Cells were infected by Ad-640 at MOI 50 and compared to cells with mock or Ad-DEST infection. After 72 h of infection, the proliferation of cells infected with Ad-640 significantly increased while there was no difference in proliferation between cells with mock and Ad-DEST infection. The BrdU assay indicated that the proliferation of cells in the Ad-640 + FFA group was increased, compared with that of the FFA and Ad-DEST + FFA groups. There was also difference in proliferation between the Ad-640 + FFA and normal cell groups with reduced proliferation in the Ad-640 + FFA group. No significant difference in proliferation was observed between the Ad-DEST + FFA and FFA groups.
a The effects of FFAs/RNAi adenovirus on the proliferation in HUVEC. * P < 0.01, Ad-640 group versus Normal group; ** P < 0.01, FFA group versus Normal group; b The effects of FFAs/RNAi adenovirus + FFAs on the proliferation in HUVEC.* P < 0.01, Ad-640 + FFA group versus FFAs group & Ad-DEST + FFA group; ** P < 0.01, Ad-640 + FFA group versus Normal group
Apoptosis analysis of HUVECs by Annexin V-FITC Apoptosis Detection Kit
Results are shown in Table 4 and Fig. 4. Apoptotic cells were detected using the calcium-binding protein annexin V. In particular, phosphatidylserine residues, which are normally located in the internal phospholipid layer, are actively translocated to the external layer in apoptotic cells and thus become detectable by annexin V. However, staining with only annexin V cannot distinguish between apoptotic and necrotic cells, we used Propidium Iodide (PI) to identify necrotic cells. As shown in Fig. 5, after treated with FFA (0.75 mM), apoptotic cells were greatly increased to 27.8% (Fig. 4b) compared with only 1.04% in the control group (Fig. 4a), and the necrotic cells were 10.8% compared with 4.11%, which demonstrated that FFA at the concentration of 0.75 mM could induce apoptosis of HUVECs. When cells were treated with FFA + Ad-640(MOI 50) for 48 h (Fig. 4c), the proportion of apoptotic cells dramatically decreased to 8.92%, and the necrotic cells decreased to 0.8%, but with FFA + Ad-DEST (MOI 50) (Fig. 4d), the proportion of apoptotic cells was 32.2%, which was nearly similar to the FFA group. This indicated our RNAi adenovirus mainly decreased the apoptosis induced by FFA, instead of necrotic.
Apoptosis analysis of HUVECs by DAPI staining
Results are shown in Figs. 5 and 6. The excitation maximum for DAPI bound to dsDNA is 358 nm, and the emission maximum is 461 nm. DAPI can be excited with a xenon or mercury-arc lamp or with a UV laser. DAPI may be used in flow cytometry systems utilizing UV excitation sources.
The percentage of apoptosis as determined by DAPI staining. Apoptotic nuclei were counted in at lest 10 different high power fields per experiment and the percentage of apoptosis was calculated as apoptotic cells to total cells in each high power field (* P < 0.01, Ad-640 + FFA vs. FFAs & Ad-DEST + FFA; ** P < 0.01, Ad-640 + FFA versus normal group; ▲: P < 0.01, FFAs vs. normal group; n = 3)
DAPI staining showed that in the FFA group (0.75 mM) (Fig. 6b) there was typical apoptotic morphology of chromatin condensation at the nuclear periphery, nuclear fragmentation, and apoptotic bodies. There was almost no apoptotic in the control group (Fig. 6a, the normal cell), however, when cells were treated with FFA + Ad-640(MOI 50) for 72 h (Fig. 6c), typical apoptotic morphology was less evident than the FFA group, but the apoptotic morphology was almost as clear as the FFA group when treated with FFA + Ad-DEST(MOI 50) for 72 h (Fig. 6d).
Discussion
We constructed an RNAi adenovirus targeting GSK3β and used it to infect HUVECs. Our results indicated that RNAi adenovirus can exert effective inhibition of GSK3β expression with MOI 25–50. Meanwhile, at MOI 50 the protein level of β-catenin was significantly increased. The GSK3β protein level decreased 48 h after infection. Up-regulation of the level of β-catenin protein could be observed as early as 72 h after infection. β-catenin continued to accumulate until 144 h after infection. Infection of blank virus (Ad-DEST) had no effects on the expression of the target genes. Taken together, these experiments demonstrated that our RNAi adenovirus could effectively inhibit GSK3β expression for at least 6 days. Further, inhibition of GSK3β expression resulted in accumulation of β-catenin in cells and thus up-regulated the activity of Wnt/GSK3β/β-catenin pathway.
Currently, it is thought that endothelial apoptosis is one of the key events leading to atherosclerosis during the progress of chronic vascular complications in diabetes. For diabetic patients, long-term hyperglycemia and high-level cycling FFAs are important environmental factors that cause endothelial damage. Michaela et al. reported that the treatment of endothelial cells with FFA composed of 0.5 mM oleic acid and 0.25 mM palmitic acid caused apoptosis within 48 h. The effect was more pronounced after 72 h and dependent on treatment time and concentration [8, 9]. In the second part of our study, we presented the effect on HUVECs of FFA at three different concentrations (0.5, 0.75, and 1.0 mM) after 72 h of treatment. Flow cytometry analysis revealed that the proportion of apoptotic cells in the FFA group was significantly higher than that of the normal control group. The BrdU experiment indicated that the proliferation of HUVECs treated with 0.75 mM FFA was significantly lower than normal control cells. Our results demonstrated that the treatment of 0.75 mM FFA (0.5 mM oleic acid and 0.25 mM palmitic acid) for 72 h could induce apoptosis and inhibit proliferation of HUVECs. Therefore, we cultured cells with 0.75 mM FFA in the following experiment for further studies.
We first examined the effect of the RNAi adenovirus on the apoptosis and proliferation of HUVECs under normal culture conditions. These results suggested that under normal culture conditions, suppression of GSK3β expression could promote proliferation in endothelial cells while having no effect on apoptosis. Subsequently, we examined the effect of RNAi adenovirus on the apoptosis and proliferation of HUVECs under high FFA conditions. The BrdU assay indicated that the proliferation of cells in the Ad-640 + FFA group was increased, compared with that of the FFA and Ad-DEST + FFA groups. The results of Annexin V-FITC/PI showed that after the treatment with FFA (0.75 mM), the proportion of apoptotic cells was greatly increased to 27.8% compared with only 1.04% in the control group, but when cells were treated with FFA + Ad-640(MOI 50) for 48 h, the proportion of apoptotic cells was dramatically decreased to 8.92%. The results of DAPI showed that when cells were treated with FFA + Ad-640(MOI 50), the typical apoptotic morphology was less evident than the FFA group, but it was almost as clear as the FFA group when cells were treated with FFA + Ad-DEST. These results indicated that FFA had significant toxicity to HUVECs. On the other hand, up-regulation of the Wnt signaling pathway through suppression of GSK3β protein expression in HUVECs cultured under high FFA conditions might alleviate the inhibition of proliferation and induction of apoptosis mediated by FFA.
Recent studies have demonstrated that the Wnt signaling pathway is closely related to the proliferation and apoptosis of endothelial cells [4, 6, 10, 11]. Our results showed that suppression of GSK3β in HUVECs under FFA culture could promote cell proliferation without completely abolishing the inhibitory effect of FFAs. Meanwhile, suppression of GSK3β in HUVECs under FFA culture could inhibit apoptosis without completely abolishing the induction effect of FFA. We concluded that RNAi adenovirus targeting GSK3β could partially protect HUVECs under high FFA level. High FFA-induced apoptosis in endothelial cells is a complicated process involving multiple factors and signaling pathways. As the Wnt/GSK3β/β-catenin pathway is one of many such pathways, its up-regulation results in only partial protection from high FFA-treated HUVECs. Our RNAi experiments demonstrated that the canonic Wnt/GSK3β/β-catenin pathway participated in the endothelial cell apoptosis process induced by high FFA. We inferred that high FFA might induce activation of GSK3β and subsequent phosphorylation as well as inactivation of β-catenin(9). Alternatively, high FFA might induce conformational change in cellular factors associated with β-catenin(1). In either scenario, the Wnt-mediated survival signal was blocked and thus caused apoptosis of the endothelial cells. After the GSK3β expression was suppressed by our RNAi adenovirus in HUVECs, the protein level of β-catenin was increased thereby activating the Wnt signaling pathway while alleviating the inhibitory effect of FFA on the Wnt pro-survival function. This could promote cell proliferation through enhancement of the expression of down-stream pro-survival genes such as VEGF(4), or cross-talk with other pro-survival signaling pathways involving PI3-Kinase/Akt(4) and NF-κB [12]. It is established that Wnt signaling participates in the endothelial damage caused by high FFA, but the detailed mechanisms are still not clear. How our RNAi adenovirus protects endothelial cells through activating Wnt pathway warrants further investigation.
Various signaling pathways have been implicated in endothelial damage. Identification of key factors in those pathways has become a hot research topic with expectation for the discovery of novel therapeutic targets and techniques for interventional treatment of diabetes [13, 14]. Our study revealed an important protective effect resulting from suppressing GSK3β, a critical factor in the canonic Wnt signaling pathway. Therefore, GSK3β could be a novel candidate of treatment target for diabetic chronic vascular complications [7].
References
Ho FM, Lin WW, Chen BC et al (2006) High glucose-induced apoptosis in human vascular endothelial cells is mediated through NF-kappaB and c-Jun NH2-terminal kinase pathway and prevented by PI3 K/Akt/eNOS pathway. Cell Signal 18(3):391–399
Ho FM, Liu SH, Liau CS et al (2000) High glucose–induced apoptosis in human endothelial cells is mediated by sequential activations of c-Jun NH2-terminal kinase and caspase-3. Circulation 101:2618–2624
Miho N, Ishida T, Kuwaba N et al (2005) Role of the JNK pathway in thrombin-induced ICAM-1 expression in endothelial cells. Cardiovasc Res 68(2):289–298
Carsten S, Henrike M, Edward R et al (2005) Glycogen-synthase K-inase3β/β-catenin axis promotes angiogenesis through activation of vascular endothelial growth factor signaling in endothelial cells. Circ Res 96:308–318
Yoshihiro T, Tomohiro O, Naoko K et al (2005) Developmental regulation of Wnt/ß-catenin signals is required for growth plate assembly, cartilage integrity, and endochondral ossification. J Biol Chem 280(19):19185–19195
Zhang F, Cheng J, Hackett NR (2004) Adenovirus E4 gene promotes selective endothelial cell survival and angiogenesis via activation of the vascular endothelial-cadherin/Akt signaling pathway. J Biol Chem 279(12):11760–11766
Choi SE, Kang Y, Jang HJ et al (2007) Involvement of glycogen synthase kinase-3beta in palmitate-induced human umbilical vein endothelial cell apoptosis. J Vasc Res 44(5):365–374 Epub 2007 May 4
Schaeffer G, Frank SL, Spitaler MM et al (2003) Intercellular signalling within vascular cells under high D-glucose involves free radical-triggered tyrosine kinase activation. Diabetologia 46:773–783
Artwohl M, Roden M, Waldhausl W et al (2004) Free fatty acids trigger apoptosi and inhibit cell cycle progression in human vascular endothelial cells. FASEB J 18(1):146–148
Hanai J, Dhanaba M, Karumanchi SA (2002) Endostatin causes G1 arrest of endothelial cells through inhibition. J Biol Chem 277(19):16464–16469
Liu Z, Hbener JF (2008) Glucagon-like peptide-1 activation of TCF7L2-dependent Wnt signaling enhances pancreatic beta-cell proliferation. J Biol Chem 283(13):8723–8735
Chen H, Yang S, Yang Z et al (2007) Inhibition of GSK-3beta decreases NF-kappaB-dependent gene expression and impairs the rat liver regeneration. J Biochem Cell 102(5):1281–1289
Sheu ML, Ho FM, Yang RS et al (2005) High glucose induces human endothelial cell apoptosis through a phosphoinositide-3-kinase-regulated cyclooxygenase-2 pathway. Arterioscler Thromb Vasc Biol 25(3):539–545
Nakagami H, Morishita R, Yamamoto K et al (2001) Phosphorylation of p38 mitogen-activated protein kinase downstream of bax-caspase-3 pathway leads to cell death induced by high D-glucose in human endothelial cells. Diabetes 50:1472–1481
Acknowledgments
This study was supported by Grant C071002 and 2009Y0011 for natural science foundation from Fujian province of China and grant from the Ministry of Health of the People’s Republic of China (WKJ 2005-2-021). We thank the members of Department of Molecular Medicine Research Center lab of Fujian Medical University, specifically Drs Lin.
Disclosure
The authors disclose this apparent conflict.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors Penli Zhu, Gang Chen, Tingting You, Jin Yao, and Qiqin Jiang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhu, P., Chen, G., You, T. et al. High FFA-induced proliferation and apoptosis in human umbilical vein endothelial cell partly through Wnt/β-catenin signal pathway. Mol Cell Biochem 338, 123–131 (2010). https://doi.org/10.1007/s11010-009-0345-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-009-0345-5