Abstract
Human papillomavirus (HPV) is considered to be a major etiological factor but is not sufficient for the development of cervical cancer. Other host factors including altered tumor suppressor gene activities might contribute to the carcinogenic process. Fragile Histidine Triad (FHIT) has been shown to play a pivotal role in carcinogenesis. Therefore, we made an attempt to find out point mutation of FHIT gene in HPV mediated cervical cancer in Indian women. 112 cases of cervical carcinoma tissue biopsies and 38 cervical scrapes samples of normal cytology were employed for this study. Herein, we report a novel mutation identified at nucleotide position 655, at codon 98 from CAT → CGT with ultimate replacement of amino acid Histidine by Arginine in cervical cancer cases. Molecular modeling was performed to predict the effect of this mutation in disease pathology. We predict that this change, His to Arg substitution in substrate-binding domain may generate catalytically inactive protein with loss of tumor suppressor activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer of the uterine cervix is the second most common gynecological cancers worldwide; but is the most common cancer among women in India [1] and it comprises about 16% of the world’s annual incidence and is the major public health problem [2]. Of the several risk factors associated with this cancer, infection with high-risk human papillomaviruses (HR-HPVs) has emerged as the major etiological factor for the development of cervical cancer. The presence of HR-HPV DNA has been found in more than 90% of cervical cancer cases. In India, HPV type 16 is the most prevalent type, accounting for more than 70% of cervical cancer cases followed by HPV type 18 and other high-risk types [1, 3]. However, infection of HPV is essential but is not sufficient for the development of cervical cancer, which implies the involvement of genetic factors [4, 5].
In cancer, the functional loss of tumor suppressor genes is one of the most common genetic alterations. A number of studies revealed frequent genetic deletion especially at chromosome 3p locus, which harbors many tumor suppressor genes including Fragile Histidine Triad (FHIT) gene [6]. This site is also reported to be the site for HPV integration [7]. Therefore, FHIT gene inactivation due to mutation, methylation, and LOH at several loci on chomosome 3p have been reported in both invasive and high-grade preinvasive cervical lesions [8, 9]. Inactivation of this gene has also been reported in various other cancers including colon, lung, breast, head and neck, and skin [10–12]. FHIT gene spans 1.8 Mb of genome region and is composed of 10 exons. It encodes a small mRNA transcript of 1.1 Kb and a protein of 16.8 kDa [13]. The reported point mutations of FHIT gene is very rare and vary from 0–5% in oral and cervical cancers [14].
Various mechanisms of tumor suppressor activity of FHIT protein have been proposed based on its crystal structure [15], but the most important one is the formation of enzyme substrate complex and the different residues in substrate-binding domain of FHIT that plays a major role for its active function [16]. However, no comprehensive study has been done to investigate its inactivation in cervical cancer. Therefore, the present study was designed to investigate a detailed evaluation of FHIT gene mutation in HPV mediated cervical cancer in North Indian population. In addition, we have done molecular modeling studies to predict the probable effect of this mutation in disease pathology.
Materials and methods
Patients and specimens
A total of 112 cases of cervical carcinoma tissue biopsies and 38 cervical scrapes samples of normal cytology of Indo-Aryan ethnicity were employed for this study. The patients were recruited from Jawaharlal Nehru Medical College & Hospital, Aligarh and other hospitals of Delhi with histopathologically confirmed cases. The patients had a mean age of 47 ± 12 years, written informed consent was obtained from all the participants and the study was carried out in accordance with the principles of Helsinki Declaration. The study was approved by the Ethics Committee of the Institute.
DNA extraction and HPV detection
Genomic DNA was extracted from fresh cervical tissue biopsy samples (patients) and cervical scrapes (control) by standard method using Proteinase K followed by Phenol/chloroform/isopropanol treatment [17].
HPV diagnosis was performed by PCR amplification using consensus primers MY09 and MY11 and further typing was done by PCR using type specific primers for HPV 16 and HPV18 [18, 19].
Polymerase chain reaction
The coding region of FHIT gene, which comprises exon 5–9, was screened for detection of mutations/polymorphism. Five sets of primers were used for this analysis, the sequences of which were adopted from the published article [20]. These primers were designed to amplify all the exonic regions as well as intron–exon boundaries. A typical PCR amplification was performed in 25 μl reaction volume containing 10 mM Tris–HCl pH 8.4, 50 mM KCl, 1.5 mM MgCl2, 200 μM of each dNTPs (dATP, dCTP, dGTP, and dTTP) (125 mM for SSCP-PCR for FHIT exons), 5 pmoles of each oligonucleotide primer, 100–500 ng of tumor DNA, and 0.5 U Taq DNA polymerase. The cycling conditions used were 95°C (5 min) initial denaturation, 94°C (0.5) min, 53°C (0.5) min, and 72°C (0.5) min for exon 5–9 with 35 cycles of amplification.
PCR-SSCP for detection of FHIT gene mutations
Single strand conformation polymorphism (SSCP) analysis was performed according to the method described by Orita et al. [21] with certain modifications [22]. The PCR products were radiolabelled for an additional 15 cycles by using 1 mCi of (α-32P) dCTP (BARC, Mumbai, India) following amplification of the FHIT exons by standard procedure. One microliter of labelled PCR product was diluted 10 times with SSCP gel loading buffer/dye containing 95% formamide, 20 mM EDTA (pH 8.0), 0.05% each of xylene cyanol, and bromophenol blue. The diluted products were denatured for 5 min at 95°C and then chilled on ice for 5 min. Three microliters of this product were subjected to non-denaturing electrophoresis in a 6% polyacrylamide sequencing gel run in 0.5 × TBE (Tris–borate EDTA) buffer. The electrophoresis was carried out at 200 V for 12 h at 17 ± 1°C in Base Ace sequencing gel apparatus (Stratagene GmbH, Heidelberg, Germany). The gel was removed on a Whatman paper and subjected to vacuum drying in gel dryer (BioRad,USA) and exposed to X-ray film at −70°C. Alteration in electrophoretic mobility of single strand DNA bands was analyzed in comparison to that of normal controls.
DNA sequencing
Direct DNA sequencing was performed on those PCR products that showed altered band mobility in SSCP along with normal controls. Fresh PCR products were prepared by PCR amplification of original tumor DNA and purified by using Qiagen PCR purification columns (Qiagen GmbH, Hilden,Germany). The mobility-shifted mutant and polymorphic bands samples were further subjected to sequencing by Macrogen Sequencing Company, Korea.
Modeling of the putative substrate-binding site
Molecular modeling was performed on silicon Graphics System using the graphics program packages PyMOL, 2002 (DeLano Scientific, Palo Alto, CA, USA.) using the atomic coordinates of Fragile Histidine Triad protein (PDB ID: 2FHI) [16]. The interaction between the substrate and substrate-binding pocket was determined by using contact/act program from CCP4 package (Collaborative Computational Project, Number 4, 1994). The mutant model (His (35) → Arg (35) was generated by using COOT package from CCP4 suite [23]. The generated coordinates were subjected to energy minimization on Swiss-PdbViewer software for correcting its stereochemical features [24]. The final model was validated on online server (http://deposit.pdb.org/validate/) which provides validation report from PROCHEK [25] and Ramachandaran Plot [26]. Energetically best-fitted model was used for structure analysis and comparison with that of wild-type protein. The ribbon diagram was plotted by using Pymol software.
Results
Detection of HPV type 16/18 in cervical cancer cases
In the studied cohort, about 83% (93/112) of the cases showed positivity for HPV infection and out of HPV positive cases, 97% (90/93) of cases were infected with HPV type16 while only 3.2% (3/93) of cases were found to be positive for HPV type 18 and 5.2% (2/38) in normal control.
FHIT gene alteration in cervical tumors
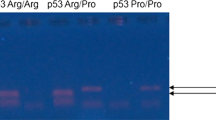
In this study, 112 cervical cancer DNA samples were analyzed for mutations in the coding region (exons 5–9) of the FHIT gene. Each exon was amplified and analyzed separately for detection of mutations. 5 tumor DNAs (4.4%) showed the altered mobility shift in PCR-SSCP for exon 6 (Fig. 1a). Figure 1b showed the partial electrophoregram of FHIT exon 6 in normal tissues. Sequencing of the DNAs with shifted band indicated a single mutation in Exon 6 (Fig. 1c). The single missense mutation occurred due to A → G transition at nucleotide position 655, at codon 98 from CAT → CGT with ultimate replacement of amino acid Histidine by Arginine. By using direct sequencing, we found evidence for the presence of another mutation, a frame shift mutation in intron 8. The frame shift mutation was due to insertion of T in intron–exon boundary (data not shown).
a–c Analysis of FHIT gene mutation in cervical cancer cases: a Representative photograph of PCR-SSCP analysis of FHIT gene in cervical tissue samples showing altered band mobility in lane 5, is the indication of mutation shown by an arrow. Lane 1, normal control and lane 2–7 cervical cancer tissue samples. (b and c), partial electropherogram of FHIT exon 6 representing the normal and mutant in cervical cancer as indicated by arrows
Structural analysis
The mutation of FHIT gene in exon 6 at nucleotide position 655 was modeled computationally on three dimensional structure in order to investigate the physiological changes occurred in substrate-binding site due to change in His35 to Arg35 in substrate-binding domain. As evident from Fig. 2a, b, the substrate-binding pocket of wild-type FHIT is sufficient to accommodate substrate in the substrate-binding pocket. The substrate-binding pocket comprises evolutionary conserved residues like Phe5, His8, Ile10, Leu25, Asn27, Val31, His35, leu37, Thr79, Gln83, Thr91, Val92, His96, His98, Arg102 and Met135. It appears that any change in these residues may lead to inactivation or decrease substrate binding of FHIT. Interestingly, we observed a significant change in one of the substrate-binding residues that is His35 which has been mutated into Arginine. The substrate-binding pocket of His35Arg is substantially narrower than native (Fig. 3a). The reason is evident from the structure of substrate-binding residues in wild-type (Fig. 2b) as well as His35Arg (Fig. 3b). ND2 and NE1 of His35 form van derwaals interaction with oxygen atoms of substrate. In addition, the main chain nitrogen forms hydrogen bond with the main chain oxygen of Val 31 (Fig. 2b). On the other hand, in His35Arg a numerous hydrogen bonded interactions have been observed for Arg35 with either substrate atoms or protein atoms which significantly narrowed the size pocket. Moreover, the side chain of Arg is much larger as compared to His which further supports the inability of substrate to bind the FHIT.
a and b: Molecular modeling of FHIT gene in cervical cancer. a substrate-binding pocket of wild-type FHIT is shown in surface diagram. The substrate analog, P1-P2-Methylene-P3-Thio-Diadenosine Triphosphate is present in the substrate-binding groove is shown in ball and stick. b structure of wild type FHIT-substrate complex. The substrate analog P1-P2-Methylene-P3-Thio-Diadenosine Triphosphate (White) and His35 are shown in ball and stick model (Yellow). Vall31 has close interaction with His35 is shown in green (ball and stick model). The hydrogen bonds are shown in dotted line
a and b: Substrate-binding pocket of FHIT His35Arg model is shown in surface diagram. a the substrate analog, P1-P2-Methylene-P3-Thio-Diadenosine Triphosphate is present in the substrate-binding groove is shown in ball and stick. b Structure of FHIT His35Arg model-substrate complex. The substrate analog P1-P2-Methylene-P3-Thio-Diadenosine Triphosphate (White) and Arg35 (Yellow) are shown in ball and stick model. Residues showing close interaction with Arg35 is shown in green (ball and stick model). The hydrogen bonds are shown in dotted line
Discussion
The extensive screening program has lowered the global incidences of cervical cancer but still cervical cancer is the second most common cancer among women worldwide [27], and the most common cancer among women in the resource poor countries including India. Early age of marriage, promiscuity, smoking, and the use of contraceptives etc. have been considered as risk factors for the development of cervical cancer but persistent HR-HPV infection has been considered to be the principal etiologic factor. In India, 85–90% cervical cancer cases are squamous cell carcinoma but only 10–15% cases are adenocarcinoma. Interestingly, in India HPV 16 is the most prevalent type both in squamous cell carcinoma as well as in adenocarcinoma while preferential occurrence of HPV 18 in adenocarcinoma is available globally [28, 29].
Cervical cancer is a suitable model to study genetic and epigenetic changes occurring during its progression because of multiple etiologies as well as prolonged well-differentiated intraepithelial lesions. However, still the role of genetic factors involved in the development of cervical carcinogenesis is poorly understood and only limited reports are available showing alteration of FHIT gene in this cancer.
The FHIT gene, a human homolog of S. pombe hydrolase enzyme prefers dinucleoside 5′, 5′′′-p1, and p3-triphosphate (Ap3A) as substrate, in contrast to 5′, 5′′′-p1, and p4-tetraphosphate (Ap4A) in case of S.pombe [30]. Thus, it is postulated that elevated levels of Ap3A (the substrate for the enzyme) activate signal transduction pathway or impair apoptotic pathway. Ap3A, in some cases can act as ATP analog and inhibit a protein kinase. In the present study, we made an attempt to predict computationally whether the FHIT function gets altered by point mutation in substrate-binding domain in cervical cancer cases from North Indian population.
Earlier studies have failed to detect any point mutation in the FHIT gene from tumors but later, evidence of such mutations were available from cell lines derived from tumors [20, 31]. Mao et al. [32] reported polymorphisms of FHIT at codons 88 and 98, a null mutation without altering the amino acid from head and neck cancer cell lines. In our study, we observed a novel single missense mutation due to A → G transition substitution at nucleotide 665, codon 98, lead to change CAT → CGT with consequent replacement of amino acid Histidine by Arginine in North Indian cervical cancer cases. However in contrast, Kannan et al. could not find any mutation in the coding regions of FHIT gene in exon 5–9 but at the ninth nucleotide upstream to the beginning of exon 9 in cervical carcinomas [14]. On the other hand, there are some reports of somatic missense mutations in FHIT gene from primary gastric cancer [33].
Earlier studies showed a link between viral integration sites and fragile sites of chromosome 3p [34]. There are two regions of the FRA3B/FHIT fragile site as flanking sites for HPV insertion point that occur within introns 4 and 5, respectively, which surround the frequently deleted exon 5 of FHIT [7]. However in contrast, reports were also available showing no apparent correlation between FHIT alteration and HPV infection suggesting FHIT gene alterations may occur independent of HPV infection [35]. As mutation in FHIT is rare event, another mechanism of inactivation of FHIT in cervical cancer cases is methylation. Our previous report showed that aberrant promoter hypermethylation of FHIT gene was highly significant (P < 0.01) for the cervical cancer cases and this late event may be associated with carcinogenesis in Indian population [8].
After determination of crystal structure of FHIT, Pace et al. proposed three different models for its anti-tumor activity. In postulation, it was proposed that the tumor suppressing function of FHIT might be due to its catabolic action to Ap3A or related substrates and/or signaling by FHIT-bound forms of these compounds which may lead to nucleotide-independent tumor suppressor function of FHIT [16]. Our observations are in good agreement with the first mechanism proposed by Pace et al. [16]. The substrate and enzyme binding might be interfered by many factors including mutations. In our study, the change from His to Arg caused an appreciable difference in the size of pocket where FHIT was unable to accommodate substrate. A similar observation was reported by Pace et al. [16] where they mutated His98 to Trp which was expected to hinder substrate binding. Formation of an enzyme–substrate complex is essential for tumor suppressor activity and the heavy side chain (Arg) substitution alleles of FHIT would be expected to lose function in parallel with a loss of its ability to bind substrate.
To our knowledge, this is the first report showing a novel naturally occurring mutation in the tumor of uterine cervix from Indian population. Our results on the mutations of the FHIT gene in squamous cell carcinoma of uterine cervix indicated that FHIT gene mutations are very rare. Although the mechanism by which FHIT gene mutations play a role in the pathogenesis of cervical cancer is not very clear, however, our mutation based structural analysis indicated that constriction in the substrate-binding pocket due to a close interactions formed by Arginine instead of Histidine in wild type at 35th position in substrate-binding domain may be one of the reason. The bulkiness of side chain of Arg further reduces the size of pocket, which is insufficient to accommodate substrate in the pocket with ultimate loss of protein function.
References
Das BC, Hussain S, Nasare V, Bharadwaj M (2008) Prospects and prejudices of human papillomavirus vaccines in India. Vaccine 26:2669–2679
Cohen J (2005) Public health. HPV’s peculiarities, from infection to disease. Science 308:619
Franceschi S, Rajkumar T, Vaccarella S, Gajalakshmi V, Sharmila A, Snijders PJ, Munoz N, Meijer CJ, Herrero R (2003) Human papillomavirus and risk factors for cervical cancer in Chennai, India: a case control study. Int J Cancer 107:127–133
Kohaar I, Thakur N, Salhan S, Batra S, Singh V, Sharma A, Sodhani P, Das BC, Sarkar DP, Bharadwaj M (2007) TNFalpha-308G/A polymorphism as a risk factor for HPV associated cervical cancer in Indian population. Cell Oncol 29:249–256
Kohaar I, Hussain S, Thakur N, Tiwari P, Nasare V, Batra S, Singh V, Bhambani S, Das BC, Sarkar DP, Bharadwaj M (2009) Association between human leukocyte antigen class II alleles and human papillomavirus-mediated cervical cancer in Indian women. Hum Immunol 70:222–229
Lea JS, Ashfaq R, Muneer S, Burbee DG, Miller DS, Minna JD, Muller CY (2004) Understanding the mechanisms of FHIT inactivation in cervical cancer for biomarker development. J Soc Gynecol Investig 11:329–337
Wilke CM, Hall BK, Hoge A, Paradee W, Smith DI, Glover TW (1996) FRA3B extends over a broad region and contains a spontaneous HPV16 integration site: direct evidence for the coincidence of viral integration sites and fragile sites. Hum Mol Genet 5:187–195
Neyaz MK, Kumar RS, Hussain S, Naqvi SH, Kohaar I, Thakur N, Kashyap V, Das BC, Husain SA, Bharadwaj M (2008) Effect of aberrant promoter methylation of FHIT and RASSF1A genes on susceptibility to cervical cancer in a North Indian population. Biomarkers 13:597–606
Wistuba II, Montellano FD, Milchgrub S, Virmani AK, Behrens C, Chen H, Ahmadian M, Nowak JA, Muller C, Minna JD, Gazdar AF (1997) Deletions of chromosome 3p are frequent and early events in the pathogenesis of uterine cervical carcinoma. Cancer Res 57:3154–3158
Ohta M, Inoue H, Cotticelli MG, Kastury K, Baffa R, Palazzo J, Siprashvili Z, Mori M, McCue P, Druck T, Croce CM, Huebner K (1996) The FHIT gene, spanning the chromosome 3p14.2 fragile site and renal carcinoma-associated t(3;8) breakpoint, is abnormal in digestive tract cancers. Cell 84:587–597
Sozzi G, Veronese ML, Negrini M, Baffa R, Cotticelli MG, Inoue H, Tornielli S, Pilotti S, De Gregorio L, Pastorino U, Pierotti MA, Ohta M, Huebner K, Croce CM (1996) The FHIT gene 3p14.2 is abnormal in lung cancer. Cell 85:17–26
Greenspan DL, Connolly DC, Wu R, Lei RY, Vogelstein JT, Kim YT, Mok JE, Munoz N, Bosch FX, Shah K, Cho KR (1997) Loss of FHIT expression in cervical carcinoma cell lines and primary tumors. Cancer Res 57:4692–4698
Croce CM, Sozzi G, Huebner K (1999) Role of FHIT in human cancer. J Clin Oncol 17:1618–1624
Kannan K, Munirajan AK, Bhuvarahamurthy V, Mohanprasad BK, Shankar P, Tsuchida N, Shanmugam G (2000) FHIT gene mutations and single nucleotide polymorphism in Indian oral and cervical squamous cell carcinomas. Oral Oncol 36:189–193
Lima CD, D’Amico KL, Naday I, Rosenbaum G, Westbrook EM, Hendrickson WA (1997) MAD analysis of FHIT, a putative human tumor suppressor from the HIT protein family. Structure 5:763–774
Pace HC, Garrison PN, Robinson AK, Barnes LD, Draganescu A, Rosler A, Blackburn GM, Siprashvili Z, Croce CM, Huebner K, Brenner C (1998) Genetic, biochemical, and crystallographic characterization of Fhit-substrate complexes as the active signaling form of Fhit. Proc Natl Acad Sci U S A 95:5484–5489
Gopalkrishna V, Aggarwal N, Malhotra VL, Koranne RV, Mohan VP, Mittal A, Das BC (2000) Chlamydia trachomatis and human papillomavirus infection in Indian women with sexually transmitted diseases and cervical precancerous and cancerous lesions. Clin Microbiol Infect 6:88–93
Saiki RK, Gelfand DH, Stoffel S, Scharf SJ, Higuchi R, Horn GT, Mullis KB, Erlich HA (1988) Primer-directed enzymatic amplification of DNA with a thermostable DNA polymerase. Science 239:487–491
Manos M, Lee K, Greer C, Waldman J, Kiviat N, Holmes K, Wheeler C (1990) Looking for human papillomavirus type 16 by PCR. Lancet 335:734
Druck T, Hadaczek P, Fu TB, Ohta M, Siprashvili Z, Baffa R, Negrini M, Kastury K, Veronese ML, Rosen D, Rothstein J, McCue P, Cotticelli MG, Inoue H, Croce CM, Huebner K (1997) Structure and expression of the human FHIT gene in normal and tumor cells. Cancer Res 57:504–512
Orita M, Iwahana H, Kanazawa H, Hayashi K, Sekiya T (1989) Detection of polymorphisms of human DNA by gel electrophoresis as single-strand conformation polymorphisms. Proc Natl Acad Sci U S A 86:2766–2770
Katiyar S, Hedau S, Jain N, Kar P, Khuroo MS, Mohanta J, Kumar S, Gopalkrishna V, Kumar N, Das BC (2005) p53 gene mutation and human papillomavirus (HPV) infection in esophageal carcinoma from three different endemic geographic regions of India. Cancer Lett 218:69–79
Emsley P, Cowtan K (2004) Coot: model-building tools for molecular graphics. Acta Crystallogr D Biol Crystallogr 60:2126–2132
Guex N, Peitsch MC (1997) SWISS-MODEL and the Swiss-PdbViewer: an environment for comparative protein modeling. Electrophoresis 18:2714–2723
Laskowski RA, Moss DS, Thornton JM (1993) Main-chain bond lengths and bond angles in protein structures. J Mol Biol 231:1049–1067
Ramachandran GN, Sasisekharan V (1968) Conformation of polypeptides and proteins. Adv Protein Chem 23:283–438
Parkin DM, Bray F (2006) Chapter 2: The burden of HPV-related cancers. Vaccine 24(Suppl 3):S11–S25
Das BC, Gopalkrishna V, Das DK, Sharma JK, Singh V, Luthra UK (1993) Human papillomavirus DNA sequences in adenocarcinoma of the uterine cervix in Indian women. Cancer 72:147–153
Iwasawa A, Nieminen P, Lehtinen M, Paavonen J (1996) Human papillomavirus DNA in uterine cervix squamous cell carcinoma and adenocarcinoma detected by polymerase chain reaction. Cancer 77:2275–2279
Barnes LD, Garrison PN, Siprashvili Z, Guranowski A, Robinson AK, Ingram SW, Croce CM, Ohta M, Huebner K (1996) Fhit, a putative tumor suppressor in humans, is a dinucleoside 5′, 5′′′-P1, p3-triphosphate hydrolase. Biochemistry 35:11529–11535
Thiagalingam S, Lisitsyn NA, Hamaguchi M, Wigler MH, Willson JK, Markowitz SD, Leach FS, Kinzler KW, Vogelstein B (1996) Evaluation of the FHIT gene in colorectal cancers. Cancer Res 56:2936–2939
Mao L, Fan YH, Lotan R, Hong WK (1996) Frequent abnormalities of FHIT, a candidate tumor suppressor gene, in head and neck cancer cell lines. Cancer Res 56:5128–5131
Gemma A, Hagiwara K, Ke Y, Burke LM, Khan MA, Nagashima M, Bennett WP, Harris CC (1997) FHIT mutations in human primary gastric cancer. Cancer Res 57:1435–1437
Yoshino K, Enomoto T, Nakamura T, Nakashima R, Wada H, Saitoh J, Noda K, Murata Y (1998) Aberrant FHIT transcripts in squamous cell carcinoma of the uterine cervix. Int J Cancer 76:176–181
Yoshino K, Enomoto T, Nakamura T, Sun H, Ozaki K, Nakashima R, Wada H, Saitoh J, Watanabe Y, Noda K, Murata Y (2000) FHIT alterations in cancerous and non-cancerous cervical epithelium. Int J Cancer 85:6–13
Acknowledgments
The authors are thankful to Dr. Rajyashri Sharma, Department of Obstetrics and Gynecology, JNMC, Aligarh, for providing clinical samples. This study was done under core fund of ICPO (ICMR), Noida.
Author information
Authors and Affiliations
Corresponding author
Additional information
Md. Kausar Neyaz and Showket Hussain contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Neyaz, M.K., Hussain, S., Hassan, M.I. et al. Novel missense mutation in FHIT gene: interpreting the effect in HPV-mediated cervical cancer in Indian women. Mol Cell Biochem 335, 53–58 (2010). https://doi.org/10.1007/s11010-009-0240-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-009-0240-0