Abstract
We have previously demonstrated that protein kinase CK2 is a potent suppressor of apoptosis in cells subjected to diverse mediators of apoptosis. The process of apoptosis involves a complex series of molecules localized in various cellular compartments. Among the various proteins that modulate apoptotic activity are inhibitors of apoptosis proteins (IAPs) which are elevated in cancers and have been proposed to block caspase activity. We have examined the impact of CK2 signal on these proteins in prostate cancer cells. Cellular IAPs demonstrate distinct localization and responsiveness to altered CK2 expression or activity in the cytoplasmic and nuclear matrix fractions. Modulation of cellular CK2 by various approaches impacts on cellular IAPs such that inhibition or downregulation of CK2 results in reduction in these proteins. Further, IAPs are also reduced when cells are treated with sub-optimal concentrations of chemical inhibitors of CK2 combined with low or sub-optimal levels of apoptosis-inducing agents (such as etoposide) suggesting that downregulation of CK2 sensitizes cells to induction of apoptosis which may be related to attenuation of IAPs. Decreased IAP protein levels in response to apoptotic agents such as TNFα or TRAIL were potently blocked upon forced overexpression of CK2 in cells. Together, our results suggest that one of the modes of CK2-mediated modulation of apoptotic activity is via its impact on cellular IAPs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CK2 (formerly casein kinase II) is a ubiquitous protein serine/threonine kinase that has a large number of potential substrates, and as such is implicated in a variety of cellular processes including cell growth and proliferation and survival [1–5]. The levels of CK2 are generally high in proliferating cells, and analogous to this property is its consistently observed elevation in a variety of cancers [1, 3]. A role for CK2 in cell proliferation has been known for a long time, whereas the distinct nature of its involvement in the cancer cell phenotype was not well understood. However, the demonstration that CK2 was also a potent suppressor of apoptosis [2, 6] pointed to an important link of the kinase to the cancer cell phenotype given that cancer cells characteristically demonstrate not only enhanced proliferation, but also reduced cell death [e.g., 7]. Following our original observations, it has become apparent that CK2 has a broad role in suppression of apoptosis induced by various mechanisms including that mediated by removal of growth factors, treatment of cells with chemical agents/drugs, and receptor-mediated apoptosis [8–11]. We have previously documented that CK2-mediated suppression of apoptosis impacts on several downstream targets in the apoptotic machinery including Bax, Bcl-2, Bcl-xL, NF-κB, cytochrome c, and caspase activity; importantly, it appears that these events may be downstream of an initial production of intracellular H2O2 in response to downregulation of CK2 [8, 9, 12, 13]. Because IAPs have been implicated in modulation of apoptotic activity in cells [14–18], we have here investigated their response to altered CK2 status by employing androgen-sensitive (ALVA-41) and androgen-insensitive (PC-3) prostate cancer cells. Our results show that downregulation of CK2 results in reduction of various IAPs, whereas overexpression of CK2 results in blocking their loss suggesting a potential locus for CK2-mediated suppression of apoptosis.
Materials and methods
Cell lines and reagents
Androgen-sensitive ALVA-41 and androgen-insensitive PC-3 prostate cancer cell lines were employed for these experiments. ALVA-41 cells were grown in RPMI-1640 (Invitrogen/GIBCO, Carlsbad, CA) supplemented with 6% FBS and 2 mM L-glutamine, whereas PC-3 cells were maintained in RPMI-1640 supplemented with 10% FBS and 2 mM L-glutamine. The following inhibitors of CK2 were employed: Apigenin, TBB from Calbiochem (San Diego, CA), and MNA (a kind gift of Dr. L.A. Pinna, University of Padova). Etoposide and rabbit anti-lamin A antibody were purchased from Sigma-Aldrich (St Louis, MO). Sources of various other antibodies and reagents employed were as follows: rabbit anti-SOD1, and mouse anti-actin were from Santa Cruz Biotechnology (Santa Cruz, CA); TRAIL, TNFα, mouse anti-cytochrome c, goat anti-XIAP, rabbit anti-cIAP1, and goat anti-cIAP2 were from R & D Systems (Minneapolis, MN); and rabbit anti-survivin was from Cell Signaling (Denver, CO).
Treatment of cells, preparation of cell fractions, and immunoblot analysis
Treatment of cells with various inhibitors of CK2 or apoptosis-inducing agents was carried out as described previously [8, 9, 12, 13, 19]. To achieve overexpression of CK2α, pcDNA6-CK2α expression vector was employed; the details of transfection are the same as described previously [8, 9, 12, 13, 19]. Additional pertinent information is provided in the figure legends. Preparation of cell lysates, and preparation of nuclear matrix and cytoplasmic fractions from cells following various treatments, and immunoblot analysis for expression of various proteins was carried out precisely as described previously [8, 9, 12, 13, 19].
Measurement of CK2 and caspase activities
Measurement of CK2 activity in cells treated with various inhibitors was carried out by employing a CK2 assay kit (MBL, Woburn, MA) as described previously [19]. Assay of caspase activity using the fluorescent assay caspase substrate (BioMol, Plymouth, PA) was carried out as detailed previously [8, 13, 19].
Results
Inhibition of CK2 activity and induction of apoptosis in prostate cancer cells by chemical inhibitors of CK2
In previous work, we have documented that induction of apoptosis in cells is blocked by overexpression of CK2, whereas modest downregulation of CK2 sensitizes cells to low levels of apoptosis-inducing agents [8, 9]. Since it appears that caspase activation is involved in induction of apoptosis mediated by downregulation of CK2, and cellular inhibitor of apoptosis proteins such as cIAPs, XIAP, and survivin are involved in blocking caspase action [14, 15, 17, 18], we have investigated the effects of CK2 modulation on these proteins in prostate cancer cells. As a first step, we have analyzed the effect of two of the chemical inhibitors (TBB and apigenin) on CK2 activity in both the androgen-sensitive (ALVA-41) and androgen-insensitive (PC-3) cells in cell culture. The results in Table 1 show that both the CK2 inhibitors tested at a concentration of 80 μM caused a time-dependent inhibition of the cellular CK2 activity with ALVA-41 cells showing somewhat greater sensitivity compared with PC-3 cells. Significant induction of apoptosis is observed at similar concentrations of CK2 inhibitors; a representative experiment employing 80 μM TBB is shown in Fig. 1 demonstrating caspase-3 activation in ALVA-41 cells treated with TBB.
Response of IAPs in prostate cancer cells following modulation of CK2 activity by various methods
We have previously shown that moderate downregulation of CK2 activity in cells results in their sensitization to apoptosis-inducing agents such as TRAIL [9]. As a step to further identify the downstream targets in the apoptosis machinery that respond to CK2 modulations, we examined the effects of manipulating CK2 by different strategies on IAPs expression in prostate cancer cells (Fig. 2). The results in Fig. 2 show the effects of 20 μM apigenin, 40 μM TBB (both CK2 inhibitors), 20 μM etoposide (DNA damaging apoptosis-inducing agent), and 100 μM TNFα without cycloheximide (a ligand for receptor-mediated apoptosis); it may be noted that these concentrations represent sub-optimal levels required for production of their respective effects in prostate cancer cells [9]. Figure 2a demonstrates that at the suboptimal concentrations, TBB, TNFα, and etoposide produce a moderate reduction in the immunoreactive levels of cIAP1, cIAP2, and survivin, the exception being that treatment with TNFα alone resulted in somewhat increased expression of survivin. However, when 40 μM TBB is combined with either 20 μM etoposide or 100 μM TNFα there is a marked further reduction in the levels of cIAP1, cIAP2, and survivin. Analogous changes are observed in the increased levels of cytochrome c under the same conditions reflecting the induction of apoptosis. The results in Fig. 2b based on the effects of apigenin (20 μM) in place of TBB confirm the results shown in Fig. 2a concerning the amplified reduction in IAPs expression following dual treatment which includes a CK2 inhibitor. Together, these data suggest that downregulation of CK2 activity results in reduction in IAPs in these cells. In order to establish whether overexpression of CK2 results in the opposite effect on IAPs, a representative experiment is shown in Fig. 3 employing concentrations of TRAIL (50 ng/ml) and TNFα (20 ng/ml plus 20 μM cycloheximide) which are known to induce apoptosis in prostate cancer cells [9]. The results show that the immunoreactive level of cIAP2 is markedly reduced when cells are treated with TRAIL or TNFα. However, when CK2 expression is increased by prior transfection of the PC-3 cells with pcDNA6-CK2α expression plasmid, there is complete reversal of the effects of TRAIL or TNFα on cIAP2 level examined. These data suggest a protective role of overexpression of CK2 on cIAP2 on steady state protein levels.
Effects of various apoptosis-inducing agents on IAPs in ALVA-41 prostate cancer cells. ALVA-41 cells were treated with 40 μM TBB, 20 μM apigenin, 20 μM etoposide, and 100 μM TNFα without cycloheximide; all of these concentrations of the various agents are sub-optimal for their respective effects (CK2 inhibition or induction of apoptosis). Panel (a)shows the effects of TBB, etoposide, and TNFα alone, and effect of etoposide plus CK2 inhibitor TBB or TNFα plus TBB; panel (b) shows a similar experiment except that apigenin rather than TBB is employed as the CK2 inhibitor. Cells were treated for a period of 24 h prior to preparation of the cell lysates. Panel ( a) shows immunoblots of cIAP1, cIAP2, survivin, and cytochrome c. Panel (b) shows immunoblots of cIAP2, survivin, and cytochrome c. Equal protein loading is confirmed by immunoblotting for β-actin
Effect of apoptotic signals on cIAP2 levels in PC-3 prostate cancer cells in the presence or absence of CK2 overexpression. Overexpression of CK2 was achieved in PC-3 cells by employing the pcDNA6-CK2α expression plasmid (treated for a period of 48 h). Control cells or cells expressing pcDNA6-CK2α were treated with 50 ng/ml of TRAIL or 20 ng/ml of TNFα (plus 30 μg/ml of cycloheximide) (these agents induce apoptosis at these concentrations). Equal quantities of cell lysates were immunoblotted for cIAP2. The results show that loss of cIAP2 in cells treated with TRAIL or TNFα was completely blocked in cells overexpressing CK2α
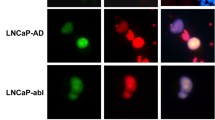
Response of IAPs in subcellular fractions following treatment of cells with inhibitors of CK2
Since IAPs are located in different cell compartments [e.g., 16, 20], we investigated the effect of treating cells with CK2 inhibitors on cytoplasmic and nuclear localized IAPs. The data in Fig. 4 indicate that control cells fractionated into the cytoplasmic and nuclear matrix fractions demonstrated distinct distribution of survivin, XIAP, and cIAP2, and that following treatment with CK2 inhibitor TBB there was a differential response of IAPs in these subcellular fractions. For example, in ALVA-41 cells, survivin protein in the cytoplasmic fraction was dramatically reduced compared with that in the nuclear matrix. In the case of PC-3 cells, both the cytoplasmic and nuclear matrix-associated survivin demonstrated significant reduction in response to TBB. The level of XIAP in ALVA-41 and PC-3 cells was greater in the cytoplasmic fraction compared with that in the nuclear matrix. The reduction in cytoplasmic and nuclear matrix XIAP was marked in response to TBB treatment in ALVA-41 cells, whereas its reduction in PC-3 cells was moderate. cIAP2 was found to be localized largely in the nuclear matrix fraction in both the ALVA-41 and PC-3 cells, and its response to treatment of cells with TBB was more dramatic in the ALVA-41 cells compared with that in PC-3 cells although the reduction in the latter was also significant. Figure 5 shows the effects of MNA (another CK2 inhibitor tested at 80 μM concentration) on cIAP2, cIAP1, XIAP, and survivin in ALVA-41 and PC-3 cells. In accordance with the result in Fig. 4, cIAP2 was predominantly found in the nuclear matrix fraction and demonstrated a dramatic reduction in response to MNA treatment in both types of prostate cancer cells. Both cIAP1 and XIAP were localized predominantly in the cytoplasmic fraction, and demonstrated a marked reduction in their levels in response to MNA in both types of cells. Data on effect of MNA on survivin expression were also similar to those for TBB shown in Fig. 4. Together, these results suggest that IAPs are dramatically influenced by the status of CK2 activity in the cells, and further these proteins demonstrate distinct distribution in the cell and that their responsiveness to CK2 status may also differ depending on their cellular locale.
Effect of CK2 inhibitor TBB on levels of IAPs in cytoplasmic and nuclear matrix fractions of prostate cancer cells. ALVA-41 and PC-3 cells were treated with 80 μM TBB for 24 h and subjected to cytoplasmic (Cy) and nuclear matrix (NM) fractionation as indicated under Materials and methods. These fractions were subjected to immunoblot analysis for survivin, XIAP, and cIAP2 as shown. Protein loading was confirmed by inclusion of a β-actin immunoblot
Effect of CK2 inhibitor MNA on levels of IAPs in cytoplasmic and nuclear matrix fractions of prostate cancer cells. All details are essentially the same as for Fig. 4, except that MNA at 80 μM was employed as the inhibitor of CK2 in ALVA-41 and PC-3 cells treated for a period of 24 h prior to isolation of the cytoplasmic (Cy) and nuclear matrix (NM) fractions. Equal amounts of protein were subjected to immunoblot analysis for cIAP2, cIAP1, XIAP, and survivin. The fidelity of the cytoplasmic and nuclear matrix fractions was confirmed by analysis of SOD1 (a cytoplasmic marker) and lamin A (a marker for nuclear compartment). β-actin was included as a protein loading control
Discussion
A consistent feature of cancer cells is that they exhibit deregulation of both proliferation and cell death [e.g., 7]. For example, in the case of prostate cancer it is suggested that reduced apoptotic activity rather than increased proliferation plays an important role in its progression [21]. Accordingly, cellular apoptotic machinery has attracted considerable attention as a potential target for designing therapeutic approaches. Apoptosis or programmed cell death in cells is regulated through activation of a complex series of pathways and molecules, and likewise its inhibition also appears to incorporate a number of potential mechanisms [e.g., 14, 15, 17, 18, 22]. One aspect of cell survival control was recognized with the observation that protein kinase CK2, known to have a role in cell proliferation in normal and cancer cells [1, 3], was also capable of suppressing cell death mediated by diverse agents suggesting the potential involvement of several pathways [2, 6, 8, 23]. For example, it has been documented that CK2 influences apoptosis associated with removal of growth factors [24, 25], chemical agents [6, 19], physical agents [26, 27], and death receptor ligands [8, 9, 11]. Thus, it would appear that CK2 has a global role in regulating apoptotic activity in cells [8]. Since CK2 has been found to be elevated in various cancers that have been examined [1, 3], its involvement in suppression of apoptosis (besides its role in cell proliferation) provided an important link of CK2 signaling to the cancer phenotype and eventually to its potential as a target for cancer therapy [2, 9, 10, 25, 28].
Among the diverse mechanisms that appear to be involved in mediating repression of apoptosis in cells [14, 15, 18], we have been interested in examining the influence of CK2 on downstream targets in the apoptotic machinery. Our previous studies have indicated involvement of several molecules that are impacted by CK2, including generation of intracellular ROS (reactive oxygen species such as H2O2) in response to downregulation of CK2 and influence on molecules such as Bcl-2, Bcl-xL, Bax, NFκB, and FLIP [8, 9, 20]. The present study has demonstrated that IAPs are also influenced by manipulation of the CK2 status in the cells. IAPs including cIAP1, cIAP2, XIAP, and survivin have been implicated in suppression of apoptosis by blocking caspase activity in addition to other potential effects in the cell [e.g., 14, 15, 18]. Our studies indicate that approaches to inhibit CK2 activity or reduce CK2 levels (by chemical inhibitors or inducers of apoptosis) result in a significant reduction in the immunoreactive protein levels of various IAPs. Considering the consistent elevation of CK2 in cancers [1, 3], the present results are germane to the observed elevation of various IAPs in cancer cells including prostate cancer [14, 15, 17, 29]. Of note, our observations on the effects of CK2 status on survivin agree with a previous study [29]; however, we have noted that the cytoplasmic component of survivin is significantly more sensitive to manipulation of CK2 levels in the cell. It has been previously noted that survivin localized in the nuclear and cytoplasmic fractions may exert distinct functions such as promotion of mitotic activity by the nuclear survivin or blocking of apoptosis by the cytoplasmic survivin [e.g., 20]. Since CK2 promotes cell proliferation and suppresses apoptosis, our results imply that this signal may exert dual effects in the cell through cytoplasmic and nuclear survivin. Accordingly, our data hint that CK2 may have an important role in regulating the cytoplasmic survivin function in addition to the other IAPs as targets for modulation of apoptotic activity in cancer cells.
It is noteworthy that the effect of altering CK2 on IAPs in prostate cancer cells was apparent in both the androgen-sensitive and androgen-insensitive cells which is consistent with our other observations indicating that CK2 functions are analogous in prostate cancer cells regardless of their phenotype [25]. The increased responsiveness of the androgen-sensitive compared with androgen-insensitive cells may relate to the observation that androgen receptor-mediated transcriptional activity is modulated by CK2 [30]. The mechanism by which CK2 influences IAPs in cancer cells is not fully understood, although our preliminary studies suggest that CK2 alters expression of survivin message (data not shown) analogous to the previous observation [29] that linked survivin expression to CK2-mediated activity in Wnt signaling. However, it is not clear if the alteration in other IAPs relate to changes at the message level in response to manipulation of CK2 status since preliminary studies did not indicate a change in the message level of cIAP1, cIAP2, or XIAP (data not shown). These studies are currently underway in our laboratory. In this regard, a recent report demonstrating that fibronectin protection of TNFα-induced apoptosis is via the AKT/survivin pathway [31] is of special note since CK2-mediated phosphorylation of a site in AKT may have a role in its activity [32]. Also, germane to these considerations is the observation that AKT is involved in stabilization of X-linked inhibitor of apoptosis protein [33].
In addition to the present observations on IAPs as potential targets of CK2 effects on apoptotic activity, a number of other molecules and pathways that may be involved in CK2-mediated suppression of apoptosis have also been identified, including, e.g., phosphorylation of IκBα and NFκB [34–36], Wnt signaling [37], Bid [38], Max [39], Faf1 [40], and the caspase-inhibiting protein ARC [41]. Together, these observations support the notion that CK2 may exert a global effect on the apoptosis machinery in the cell [8, 25, 42]. Thus, while it has been proposed that IAPs and especially survivin [14, 15] may be useful targets for cancer therapeutics, we have considered that CK2 which is a remarkable nodal molecule with its impact on a wide range of cellular activities may be an even more attractive target for cancer therapy [10, 25, 28, 42].
In conclusion, we have presented data that provide novel information on the impact of CK2 on IAPs. Downregulation of CK2 results in loss of cellular IAPs in a distinct manner, and overexpression of CK2 protects IAPs from such downregulation induced by apoptotic signals. Considering that CK2 is deregulated in all the cancers that have been examined, and that IAPs have also been found to be elevated in several cancers, we propose that therapies directed at downregulation of CK2 could additionally produce a targeted downregulation of IAPs thereby facilitating a potent induction of apoptosis.
Abbreviations
- CK2:
-
Acronym for the former name casein kinase II
- CK2α:
-
CK2 catalytic subunit α
- CK2β:
-
CK2 regulatory subunit β
- IAPs:
-
Inhibitor of apoptosis proteins such as cIAP1, cIAP2, XIAP, survivin
- TBB:
-
4,5,6,7-Tetrabromobenzotriazole
- MNA:
-
1,8-Dihydroxy-4-nitro-anthracene-9,10-dione
- TRAIL:
-
Tumor necrosis factor-related apoptosis inducing ligand
- TNFα:
-
Tumor necrosis factor α
- FBS:
-
Fetal bovine serum
References
Tawfic S, Yu S, Wang H, Faust R, Davis A, Ahmed K (2001) Protein kinase CK2 signal in neoplasia. Histol Histopathol 16:573–582
Ahmed K, Gerber DA, Cochet C (2002) Joining the cell survival squad: an emerging role for protein kinase CK2. Trends Cell Biol 12:226–230. doi:10.1016/S0962-8924(02)02279-1
Guerra B, Issinger O-G (1999) Protein kinase CK2 and its role in cellular proliferation, development and pathology. Electrophoresis 20:391–408. doi:10.1002/(SICI)1522-2683(19990201)20:2 ≤ 391::AID-ELPS391 ≥ 3.0.CO;2-N
Pinna LA (2002) Protein kinase CK2: a challenge to canons. J Cell Sci 115:3873–3878. doi:10.1242/jcs.00074
Duncan JS, Litchfield DW (2008) Too much of a good thing: the role of protein kinase CK2 in tumorigenesis and prospects for therapeutic inhibition of CK2. Biochim Biophys Acta 1784:33–47
Guo C, Yu S, Davis AT, Green JE, Ahmed K (2001) A potential role of nuclear matrix-associated protein kinase CK2 in protection against drug-induced apoptosis in cancer cells. J Biol Chem 276:5992–5999. doi:10.1074/jbc.M004862200
Evan GI, Vousden KH (2001) Proliferation, cell cycle, and apoptosis in cancer. Nature 411:342–348. doi:10.1038/35077213
Wang G, Ahmad KA, Ahmed K (2005) Modulation of receptor mediated apoptosis by CK2. Mol Cell Biochem 274:201–205. doi:10.1007/s11010-005-2952-0
Wang G, Ahmad KA, Ahmed K (2006) Role of CK2 in regulation of tumor necrosis factor-related apoptosis inducing ligand-induced apoptosis in prostate cancer cells. Cancer Res 66:2242–2249. doi:10.1158/0008-5472.CAN-05-2772
Unger GM, Davis AT, Slaton JW, Ahmed K (2004) Protein kinase CK2 as regulator of cell survival: implications for cancer therapy. Curr Cancer Drug Targets 4(1):77–84. doi:10.2174/1568009043481687
Izeradjene K, Douglas L, Delaney A, Houghton JA (2005) Casein kinase II (CK2) enhances death-inducing signaling complex (DISC) activity in TRAIL-induced apoptosis in human colon carcinoma cell lines. Oncogene 24:2050–2058. doi:10.1038/sj.onc.1208397
Wang G, Unger G, Ahmad KA, Slaton JW, Ahmed K (2005) Downregulation of CK2 induces apoptosis in cancer cells—a potential approach to cancer therapy. Mol Cell Biochem 274:77–84. doi:10.1007/s11010-005-3077-1
Ahmad KA, Wang G, Ahmed K (2006) Intracellular hydrogen peroxide production is an upstream event in apoptosis induced by down-regulation of casein kinase 2 in prostate cancer cells. Mol Cancer Res 4:331–338. doi:10.1158/1541-7786.MCR-06-0073
Reed JC (2002) Apoptosis-based therapies. Nat Rev Drug Discov 2:111–121. doi:10.1038/nrd726
Altieri DC (2008) Survivin, cancer networks and pathway-directed drug discovery. Nat Rev Cancer 8:61–70. doi:10.1038/nrc2293
McEleny KR, Watson RWG, Coffey RNT, O’Neill AJ, Fitzpatrick JM (2002) Inhibitors of apoptosis proteins in prostate cancer cell lines. Prostate 51:133–140. doi:10.1002/pros.10061
Krajewska M, Krajewski S, Banares S, Huang X, Turner B, Bubendorf L et al (2003) Elevated expression of inhibitor of apoptosis proteins in prostate cancer. Clin Cancer Res 9:4914–4925
Bortner CD, Cidlowski JA (2002) Cellular mechanisms for the repression of apoptosis. Annu Rev Pharmacol Toxicol 42:259–281. doi:10.1146/annurev.pharmtox.42.083101.143836
Ahmad KA, Harris NH, Johnson AD, Lindvall HNC, Wang G, Ahmed K (2007) Protein kinase CK2 modulates apoptosis induced by resveratrol and epigallocatechin-3-gallate in prostate cancer cells. Mol Cancer Ther 6:1006–1012. doi:10.1158/1535-7163.MCT-06-0491
Stauber RH, Mann W, Knauer SK (2007) Nuclear and cytoplasmic survivin: molecular mechanism, prognostic, and therapeutic potential. Cancer Res 67:5999–6002. doi:10.1158/0008-5472.CAN-07-0494
Kyprianou N, Bruckheimer EM, Guo Y (2000) Cell proliferation and apoptosis in prostate cancer: significance in disease progression and therapy. Histol Histopathol 15:1211–1223
Sun X-M, MacFarlane M, Zhuang J, Wolf BB, Green DR, Cohen GM (1999) Distinct caspase cascades are initiated in receptor-mediated and chemical-induced apoptosis. J Biol Chem 274:5053–5060. doi:10.1074/jbc.274.8.5053
Wang H, Davis A, Yu S, Ahmed K (2001) Response of cancer cells to molecular interruption of the CK2 signal. Mol Cell Biochem 227:167–174. doi:10.1023/A:1013112908734
Yu S, Wang H, Davis A, Ahmed K (2001) Consequences of CK2 signaling to the nuclear matrix. Mol Cell Biochem 227(1/2):67–71. doi:10.1023/A:1013156721938
Wang G, Ahmad KA, Unger G, Slaton JW, Ahmed K (2006) CK2 signaling in androgen-dependent and -independent prostate cancer. J Cell Biochem 99:382–391. doi:10.1002/jcb.20847
Davis AT, Wang H, Zhang P, Ahmed K (2002) Heat shock mediated modulation of protein kinase CK2 in the nuclear matrix. J Cell Biochem 85:583–591. doi:10.1002/jcb.10158
Yamane K, Kinsella TJ (2005) CK2 inhibits apoptosis and changes its cellular localization following ionizing radiation. Cancer Res 65:4362–4367. doi:10.1158/0008-5472.CAN-04-3941
Ahmad KA, Wang G, Slaton J, Unger G, Ahmed K (2005) Targeting CK2 for cancer therapy. Anticancer Drugs 16:1037–1044. doi:10.1097/00001813-200511000-00001
Tapia JC, Torres VA, Rodriguez DA, Leyton L, Quest AFG (2006) Casein kinase 2 (CK2) increases survivin expression via enhanced β-catenin-T cell factor/lymphoid enhancer binding factor-dependent transcription. Proc Natl Acad Sci USA 103:15079–15084. doi:10.1073/pnas.0606845103
Götz C, Bachmann C, Montenarh M (2007) Inhibition of protein kinase CK2 leads to a modulation of androgen-receptor dependent transcription in prostate cancer cells. Prostate 67:125–134. doi:10.1002/pros.20471
Fornaro M, Plescia J, Chheang S, Tallini G, Zhou Y-M, King M et al (2003) Fibronectin protects prostate cancer cells from tumor necrosis factor-α-induced apoptosis via the Akt/survivin pathway. J Biol Chem 278:50402–50411. doi:10.1074/jbc.M307627200
Di Maira G, Salvi M, Arrigoni G, Marin O, Sarno S, Brustolon F et al (2005) Protein kinase CK2 phosphorylates and upregulates Akt/PKB. Cell Death Differ 12:668–677. doi:10.1038/sj.cdd.4401604
Dan HC, Sun M, Kaneko S, Feldman RI, Nicosia SV, Wang HG et al (2004) Akt phosphorylation and stabilization of X-linked inhibitor of apoptosis protein (XIAP). J Biol Chem 279:5405–5412. doi:10.1074/jbc.M312044200
Pando MP, Verma IM (2000) Signal-dependent and–independent degradation of free and NF-κB-bound IκBα. J Biol Chem 275:21278–21286. doi:10.1074/jbc.M002532200
Wang D, Westerheide SD, Hanson JS, Baldwin AS Jr (2000) Tumor necrosis factor α-induced phosphorylation of Rel/p65 on Ser529 is controlled by casein kinase II. J Biol Chem 275:32592–32597. doi:10.1074/jbc.M001358200
Romieu-Mourez R, Landesman-Bollag E, Seldin DC, Traish AM, Mercurio F, Sonenshein GE (2001) Roles of IKK kinase and protein kinase CK2 in activation of NF-κB in breast cancer. Cancer Res 61:3810–3818
Seldin DC, Landesman-Bollag E, Farrago M, Currier N, Lou D, Dominquez I (2005) CK2 as a positive regulator of Wnt signaling and tumorigenesis. Mol Cell Biochem 274:2532–2538. doi:10.1007/s11010-005-3078-0
Desagher S, Osen-Sand A, Montessuit S, Magnenat E, Vilbois F, Hochmann A et al (2001) Phosphorylation of Bid by casein kinase 1 and 2 regulates its cleavage by caspase 8. Mol Cell 8:601–611. doi:10.1016/S1097-2765(01)00335-5
Krippner-Heidenreich A, Talanian RV, Sekul R, Kraft R, Thole H, Ottleben H et al (2001) Targeting of the transcription factor Max during apoptosis: phosphorylation-regulated cleavage by caspase-5 at an unusual glutamic acid residue in position P1. Biochem J 358:705–715. doi:10.1042/0264-6021:3580705
Olsen BB, Jesson V, Hojrup P, Issinger O-G, Boldyreff B (2003) Protein kinase CK2 phosphorylates the Fas-associated factor Faf1 in vivo and influences its transport into the nucleus. FEBS Lett 546:218–222. doi:10.1016/S0014-5793(03)00575-1
Li PF, Li J, Muller EC, Otto A, Dietz R, von Horsdorf R (2002) Phosphorylation by protein kinase CK2: a signaling switch for the caspase-inhibiting protein ARC. Mol Cell 10:247–258. doi:10.1016/S1097-2765(02)00600-7
Ahmad KA, Wang G, Unger G, Slaton J, Ahmed K (2008) Protein kinase CK2—a key suppressor of apoptosis. Adv Enzyme Regul 48 (in press). doi:10.1016/j.advenzreg.2008.04.002
Acknowledgments
This work is supported in part by funds from USPHS Research Grant CA-15062 awarded by the National Cancer Institute, Department of Health and Human Services, and in part by the Medical Research Fund of the U.S. Department of Veterans Affairs. We deeply appreciate the critical comments of Dr. J. Trembley during preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, G., Ahmad, K.A., Harris, N.H. et al. Impact of protein kinase CK2 on inhibitor of apoptosis proteins in prostate cancer cells. Mol Cell Biochem 316, 91–97 (2008). https://doi.org/10.1007/s11010-008-9810-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-008-9810-9