Abstract
Astrocyte activation has been implicated in the pathogenesis of many neurological diseases. These reactive astrocytes are capable of producing a variety of proinflammatory mediators and potentially neurotoxic compounds, such as nitric oxide (NO), tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) and interleukin-1β (IL-1β). In this study, we examined the suppressive effects of Tetrandrine (TET) on astrocyte activation induced by lipopolysaccharide (LPS) in vitro. We found that TET decreased the release of NO, TNF-α, IL-6 and IL-1β in LPS-activated astrocytes. Also mRNA expression levels of inducible nitric oxide synthase (iNOS), macrophage inflammatory protein-1α (MIP-1α) and vascular cell adhesion molecule-1 (VCAM-1) were inhibited in TET pretreated astrocytes. Such suppressive effects might be resulted from the inhibition of nuclear factor kappa B (NF-κB) activation through downregulating IκB kinases (IKKs) phosphoration, which decreased inhibitor of nuclear factor-κB-α (IκBα) phosphoration and degradation. Our results suggest that TET acted to regulate astrocyte activation through inhibiting IKKs-IκBα-NF-κB signaling pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Astrocytes have a fundamental role in regulating brain homeostasis and development, providing metabolic and trophic support for neurons, and promoting repair processes [1]. Astrocytes also play an important role in the pathophysiology of neurodegenerative diseases [2–4]. Brain lesions observed in Alzheimer’s disease (AD), ischemic damage, autoimmune responses, infections (e.g., human immunodeficiency virus), and tumors are rapidly bordered by hypertrophic astrocytes. These reactive astrocytes can produce nitric oxide (NO) and other proinflammatory mediators, which amplify the inflammatory response [5]. Although NO has been reported to protect against neuronal cells death, it is likely that higher concentrations of NO, mainly generated by inducible nitric oxide synthase (iNOS), and exert detrimental effects on neuronal cells [6]. Astrocytes also synthesize cytokines including interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α), which contribute to the development of neurodegeneration through amplifying brain inflammation and neuronal injury [7]. The secretion of macrophage inflammatory protein-1α (MIP-1α) and vascular cell adhesion molecule-1 (VCAM-1) by activated astrocytes are also found important for the entry of T cells into the CNS parenchyma and for the manifestation of neurological disease [1, 8].
Tetrandrine (TET) is a bis-benzylisoquinoline alkaloid isolated from the roots of Han-Fang-Ji (Stephania Tetrandra S Moore). It is traditionally used in China for treating patients with arthritis, silicosis, hypertension, and inflammation; anti-tumor properties of TET have been demonstrated [9]. In addition, in vitro studies have shown that TET inhibits cellular proliferation and cytokine production in activated monocytes and T cells through suppressing inhibitor of nuclear factor-κB-α (IκBα) kinases or PKC activities [10–13]. Also, we found that TET suppresses microglial activation through inhibiting NF-κB pathway [14].
Based on the known anti-inflammatory activities of TET, we hypothesized that TET may suppress the activation of astrocytes. As described previously [15, 16], we employed LPS as an experimental tool in vitro to stimulate astrocyte activation. We found that TET pretreatment inhibited NO release, IL-1β, IL-6 and TNF-α production as well as MIP-1α and VCAM-1 expression by astrocytes. These effects of TET may be attributed to its inhibitory effect on the IκB kinases (IKKs)-IκBα-nuclear factor kappa B (NF-κB) pathway during astrocyte activation.
Materials and methods
Reagents
Tetrandrine (purity > 98%) was purchased from Huike Botanical Development (Shanxi, China). The chemical structure of TET is illustrated in Fig. 1. LPS from Escherichia coli (serotype 026: B6) was purchased from Sigma (St Louis, MO, USA). The enzyme-linked immunosorbent assay (ELISA) kits specific for rat TNF-α, IL-6 and IL-1β were purchased from R&D Systems (Minneapolis, MN, USA). Primers for real-time PCR and nucleotide oligomers were synthesized by Invitrogen (Carlsbad, CA, USA). Mouse monoclonal antibody for phospho-IκBα (Ser32/36) (5A5) and rabbit polyclonal antibodies (for IKKα, IKKβ, phospho-IKKα/β (Ser176/180), IκBα (44D4) ) were purchased from Cell Signaling Technology (Beverly, MA, USA). Rabbit polyclonal antibodies for β-actin (20–33) and HRP-conjugated goat anti-rabbit antibody were purchased from Sigma. HRP-linked antibody (H&L) anti-mouse IgG was purchased from Cell Signaling Technology.
Astrocytes culture and TET pretreatment
Primary astrocytes culture was prepared as described previously [17]. Briefly, brains were isolated from Spraque-Dawley rat (Shanghai SLAC Laboratory Animal, Shanghai, China) at postnatal d 1–3. After the meninges were carefully removed, the brains were minced mechanically. Dissociated cells were resuspended in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and seeded in 75 cm2 flasks at a density of 1 × 106 cells/ml. The cells were cultured in an incubator under 5% CO2 at 37°C, and the medium was changed every 3 d. After 7–9 d, microglia growing on the surface of adherent astrocytes were removed by shaking for 4.5 h at 180 rpm. The adherent astrocytes were tripsionized by 0.25% Tripsion-EDTA, then collected and transferred to a six-well plate at a density of 2 × 106 cells in 2 ml culture medium per well. The purity was 95–98% for astrocytes as defined by anti-glial fibrillary acid protein (GFAP) antibody (Sigma). In all the experiments, cells were pretreated with TET (15 or 30 μM) for 2 h before the addition of LPS (1 μg/ml). Control samples were pretreated with the culture medium only.
The study was conducted in accordance with the National Institute of Health Guide for the Care and Use of Laboratory Animals.
Measurement of nitrite
NO was determined by measuring the end product nitrite, using a method based on the Griess reaction. Briefly, aliquots of culture supernatant (100 μl) were mixed with 100 μl of Griess reagent at room temperature for 10 min. Absorbance was measured at 540 nm in an automated microplate reader. The concentration of nitrite was determined by reference to a standard curve of sodium nitrite. Culture medium was used as the blank.
Analysis of cytokines
TNF-α, IL-6 and IL-1β were determined with the help of ELISA kits (R&D) according to the manufacture’s instructions.
Isolation of total RNA and RT-PCR
Total RNA was isolated from cell pellets using RNeasy mini kit (Qiagen, Hilden, Germany). Genomic DNA was removed from total RNA prior to cDNA synthesis by DNase digestion using the RNase-free DNase Set (Qiagen). RNA was stored at −80°C. First-strand cDNA synthesis was performed for each RNA sample using Sensiscript RT Kit (Qiagen). Random hexamers were used to prime cDNA synthesis.
Real-time PCR
Gene expression levels of iNOS, VCAM-1, and MIP-1α mRNA were performed by real-time PCR using SYBR Green master mix (Applied Biosystems, Foster City, CA, USA). Thermocycler conditions comprised an initial holding at 50°C for 2 min, then 95°C for 10 min. Reaction mixtures were cycled 40 times at 95°C for 15 s and 60°C for 60 s. Data were collected and quantitatively analyzed on an ABI Prism 7900 sequence detection system (Applied Biosystems, USA). The β-actin gene was used as an endogenous control to normalize differences in the amount of total RNA in each sample. All quantities were expressed in the number of folds relative to the expression of β-actin.
-
β-actin: sense 5′-TTCAACACCCCAGCCATGT-3′; anti-sense 5′-GTGGTACGACCAGAGGCATACA-3′
-
iNOS: sense 5′-CGGTTCACAGTCTTGGTGAAAG-3′; anti-sense 5′-ACGCGGGAAGCCATGAC-3′
-
VCAM-1: sense 5′-TGTGAAGATGGTCGCGATCTT-3′; anti-sense 5′-CAATCTGAGCGAGCGTTTTGT-3′
-
MIP-1α: sense 5′-GACGGCAAATTCCACGAAAA-3′; anti-sense 5′-AGATCTGCCGGTTTCTCTTGG-3′
Electrophoresis mobility shift assay (EMSA)
After treatment with LPS (1 μg/ml) with or without TET (30 μM) for 24 h, astrocytes were collected. Buffer A (10 mM Hepes, pH 7.9, 1.5 mM MgCl2, 10 mM KCl, 1 mM phenylmethylsulfonyl fluoride [PMSF] and 1 mM dithiothreitol [DTT]) was then added to the cells and incubated at 4°C for 15 min, and 1.06 μl of Nonidet P-40 (10%) was added. After centrifugation, the supernatant was removed, and a high-salt solution (20 mM Hepes, pH 7.9, 25% glycerol, 420 mM NaCl, 1.5 mM MgCl2, 0.2 mM EDTA, 1 mM PMSF, and 1 mM DTT) was added to the pellet. The resuspended pellet was incubated for 60 min at 4°C, and then the supernatant was collected and used for the experiment. Protein concentrations were determined using a protein assay (Bio-Rad, Hercules, CA, USA). Synthetic double-stranded oligonucleotides for the consensus NF-κB binding sequence, 5′-AGTTGAGGGGACTTTCCCAGGC-3′ were labeled with [γ-32P] dATP using T4 polynucleotide kinase (Promega, Madison, WI, USA). The nuclear extract from cultured cells was incubated with the labeled probe in Gel Shift Binding Buffer (Promega) at 4°C for 30 min. DNA-protein complexes were resolved by electrophoresis in 4% polyacrylamide gels with 0.5 × Tris-borate buffer at 4°C and visualized by phorsphorimaging.
Immunobloting
After treatment with LPS (1 μg/ml) with or without TET (30 μM) for 3 h, astrocytes were collected. Then cells were lysed in RIPA buffer (150 mM NaCl, 10 mM Tris–HCl (pH 8.0), 1% Nonidet P-40, 0.5% deoxycholic acid, 0.1% SDS, 5 mM EDTA) containing 0.7% PMSF, 0.2% aprotinin, and 0.2% leupeptin and sodium metavanadate. Protein 40 μg aliquots for detection were mixed with an equal amount of 2 × SDS sample buffer, boiled at 100°C for 5 minutes, centrifuged, and separated by 10% SDS-PAGE. The gels were then transferred onto polyvinylidene fluoride membranes (PVDF) (Millipore, MA, USA). Membranes were blocked with 5% nonfat milk in 10 mM Tris–HCl containing 150 mM NaCl and 0.5% Tween-20 (TBST) and then washed three times with TBST. Primary antibodies for IKKα, IKKβ, phospho-IKKα/β (Ser176/180), pIκBα (Ser32/36) (5A5) and IκBα (44D4) were added at proper dilution in TBST containing 5% BSA overnight at 4°C. Membranes were washed with TBST, HRP-conjugated goat anti-rabbit IgG (Sigma) at a dilution of 1/5,000 and HRP-linked antibody (H&L) anti-mouse IgG (Cell Signaling Technology) at a dilution of 1/2,000 were added in TBST containing 5% BSA for 1 h at room temperature. For control of equal protein loading, membranes were incubated overnight with primary antibody to β-actin (Sigma) (1/1,000 in TBST containing 5% BSA), again washed extensively with TBST, and incubated for 1 h with blocking solution containing HRP-conjugated rabbit-anti-mouse IgG (1/5,000 in TBST containing 5% BSA). All the bands were visualized by ECL reagent. The intensities of pIκBα, IκBα, pIKKα/β, IKKα and IKKβ bands were quantified by Biorad-Image for Windows Program (Biorad GS-800 Calibrated Densitometer).
Statistical analysis
All data are presented as mean ± SD. Statistical comparisons between two different treatments were analyzed using the Student’s t-test. Differences among more than two groups were tested by one-way ANOVA. The level of significance was set to α = 0.05. All tests were two tailed.
Results
TET inhibited NO release and iNOS mRNA expression in LPS-activated astrocytes
When rat primary astrocytes were stimulated with LPS in vitro, a strong induction of NO production was observed. The production of NO was determined by the measurement of nitrite, a stable product of NO, which reflects accumulated NO in the medium (Fig. 2a). We can see that cultured astrocytes without LPS stimulation produced minimal NO in the supernatant. However, in response to LPS exposure (1 μg/ml) for 24 h, astrocytes released significantly higher levels of NO: from 6.273 ± 0.5047 μM to 58.27 ± 3.033 μM (p < 0.05). In addition pretreatment of astrocytes with TET significantly reduced the elevation of NO release in a dose-dependent manner. Nitrite concentration was reduced to 43.62 ± 1.514 (TET 15 μM) and 18.64 ± 1.767 (TET 30 μM) respectively. The cytotoxicity of TET was determined by lactate dehydrogenase (LDH) assay. There was no significant difference in LDH release between TET-treated and non-treated astrocytes (data not shown). Therefore, the following observed anti-inflammation effects of TET were not due to its cytotoxicity on astrocytes.
Effect of TET on LPS-induced NO release and iNOS mRNA expression in astrocytes. Primary astrocytes were incubated with TET (15 and 30 μM) for 2 h. Thereafter, astrocytes were challenged with LPS (1 μg/ml). (a) After incubation for 24 h, the culture media were collected for nitrite determination using Griess reagent. (b) After incubation for 6 h, total RNA was obtained and relative iNOS mRNA expression was measured by real-time PCR. Data are presented as mean ± SD. The experiments were repeated 5 times and the similar pattern of inhibition was observed. * p < 0.05, ** p < 0.01
Nitric oxide synthase (NOS), the enzyme responsible for synthesis of NO, exists in three isoforms: endothelial NOS (eNOS), neuronal NOS (nNOS), and iNOS. In endotoxin-stimulated immune cells, iNOS is responsible for NO production. Therefore, we investigated whether TET suppressed iNOS expression in astrocytes activated by LPS. As shown in Fig. 2b, TET down-regulated iNOS mRNA expression in LPS-activated astrocytes in a dose-dependent manner. We also examined the amount of nNOS and eNOS mRNA expression with real-time PCR, but found them undetectable in astrocytes (data not shown). These results suggest that TET regulated NO production in LPS-activated astrocytes via an iNOS-dependent pathway.
TET reduced TNF-α, IL-6 and IL-1β release from LPS-activated astrocytes
In many of the CNS diseases including AD, multiple sclerosis (MS), Parkinson’s disease (PD) and brain injury/trauma, astrocytes are responsible for the production of inflammatory cytokines [18]. In order to investigate the effects of TET on cytokine production of astrocytes, they were pretreated with TET (30 μM) for 2 h, followed by treatment with 1 μg/ml of LPS for 24 h. Supernatants were then taken for cytokine measurement. As shown in Fig. 3, TNF-α, IL-6 and IL-1β levels were increased following the incubation with LPS. While TET pretreatment significantly inhibited the generation of these cytokines by astrocytes. Therefore, TET effectively suppressed the production of proinflammatory cytokines by activated astrocytes.
Effect of TET on LPS-induced release of TNF-α, IL-6 and IL-1β by astrocytes. Primary astrocytes were pretreated with TET (30 μM) for 2 h followed by addition of LPS (1 μg/ml) for 24 h. Culture supernatants were collected and assayed for TNF-α (a), IL-6 (b) and IL-1β (c). Data are expressed as mean ± SD. Results were representative of three independent experiments. * p < 0.05; ** p < 0.01; *** p < 0.001
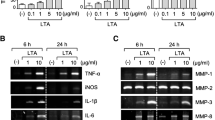
TET inhibited MIP-1α and VCAM-1 mRNA expression in LPS-activated astrocytes
As a potent source of not only cytokines, but also chemokines and adhesion molecules, astrocytes play a pivotal role in CNS inflammation and injury [18]. Therefore, we checked the expression of MIP-1α and VCAM-1 by astrocytes. As shown in Fig. 4, the expression levels of MIP-1α and VCAM-1 mRNA were potently induced after LPS stimulation, while TET significantly suppressed their expression by astrocytes.
Effect of TET on LPS-induced MIP-1α and VCAM-1 mRNA expression in astrocytes. Primary astrocytes were pretreated with TET (30 μM) for 2 h, LPS (1 μg/ml) was added. And 6 h later, total RNA was isolated. The mRNA expression of MIP-1α (a) and VCAM-1 (b) was quantified by real-time PCR. Triplicate reactions were performed on each sample. Data are presented as mean ± SD. Results were representative of three independent experiments. * p < 0.05; ** p < 0.01
TET inhibited LPS-induced activation of NF-κB through preventing IκBα degradation and phosphorylation
NF-κB pathway is initially involved in LPS-induced astrocyte activation. NF-κB regulates the expression of many proinflammatory mediators, including cytokines, chemokines and adhesion molecules [19]. Therefore, we used the EMSA assay to examine whether NF-κB activity in astrocytes were affected by TET. As shown in Fig. 5a, nuclear NF-κB binding activity was markedly increased in astrocytes stimulated with LPS. However, TET (30 μM) pretreatment dramatically inhibited LPS-induced NF-κB activation. Since degradation of IκB proteins is an essential step for NF-κB activation, we further examined the effect of TET on the LPS induced IκBα degradation (Fig. 5b). We found that TET successfully prevented IκBα degradation in LPS activated astrocytes. In addition, determination of IκBα phosphorylation by Western blotting using a phosphospecific IκBα antibody revealed the significant inhibitory effect on the LPS-induced IκBα phosphorylation in the presence of TET (Fig. 5c). These results indicated that TET prevented LPS-induced IκBα degradation through inhibiting IκBα phosphorylation, thereby interfering with one of the common steps in the signaling cascade leading to NF-κB activation.
Effect of TET on LPS-induced NF-κB activity and the degradation and phosphorylation of IκBα in astrocytes. Primary astrocytes were pretreated with TET (30 μM) for 2 h, LPS (1 μg/ml) was added. After incubation for 24 h, EMSA was performed with cell nuclear extracts to determine NF-κB activity (a). Specific competitor (SC) for EMSA consisted of a 100-fold excess of unlabeled NF-κB probe. Results were representative of three independent experiments. While after incubation for 3 h, cell pellets were collected and total cell lysates were prepared. For determination of IκBα (b) and pIκBα (c) protein levels, Western blotting assays were performed. β-actin levels were measured for the confirmation of equal amount of protein loading. Data are presented as mean ± SD. Densitometric values were representative of three independent experiments. * p < 0.05; ** p < 0.01
TET inhibited IκB kinases
IκBα is phosphorylated by the IKK complex containing catalytic subunits (IKKα and β) and the IKKγ or NF-κB essential modulator regulatory subunits at sites that trigger its ubiquitin dependent degradation [20]. Hence, we asked whether IKKα/β could be the target for TET action. According to the results of Fig. 6, we found that TET could effectively inhibit IKKs phosphorylation. These observations suggested that TET inhibition prevented NF-κB DNA binding as well as its transcriptional activity by inhibiting phosphorylation of IKKα/β activities, which indicated the possible involvement of upstream kinases in the activation of IKKs.
Effect of TET on LPS-induced IKKα and IKKβ activities in astrocytes. Primary astrocytes were pretreated with TET (30 μM) for 2 h. LPS (1 μg/ml) was added and astrocytes were further incubated for 3 h. Cell pellets were collected and total cell lysates were prepared. For determination of total IKKα and IKKβ (a) and pIKKα/β (b) protein levels, Western blotting assays were performed. β-actin levels were measured for the confirmation of equal amount of protein loading. Data are presented as mean ± SD. Densitometric values were representative of three independent experiments. ** p < 0.01
Discussion
In the present study, we are the first to demonstrate that TET-suppressed LPS-induced astrocyte activation via inhibiting NO generation, cytokines (TNF-α, IL-6 and IL-1β) secretion, as well as iNOS, MIP-1α and VCAM-1 expression. TET conferred its effects by impairing IKKs activation, consequently attenuating NF-κB binding activity, thereby leading to abrogation of LPS induced astrocyte activation. While in many of the CNS diseases, stimulated astrocytes are important cellular source of inflammatory mediators [18]. It is becoming increasingly evident that astrocytes play important roles in the modulation of brain inflammation [21, 22]. Our findings suggest that TET could be of therapeutic value in those diseases and brain damage where inflammation processes are involved.
Our data showed that TET-inhibited iNOS mRNA expression and NO production in LPS-stimulated astrocytes. NO is a diffusible gas that involves in many physiological and diverse pathological conditions. At low concentration, NO has been shown to play a role in neurotransmission and vasodilation; while at higher concentration, it is neurotoxic. In demyelinating conditions, astrocytes derived NO could contribute to oligodendrocyte degeneration and neuronal death [23]. Our present study showed that TET-inhibited iNOS expression in LPS stimulated astrocytes. Our observation of reduced NO after TET administration suggested that TET-suppressed astrocytes activation through abrogating iNOS expression and NO production.
Furthermore, our results suggested that TET modulated the production of TNF-α, IL-6 and IL-1β by astrocytes, which were secreted at a very early stage of CNS inflammation. These cytokines are elevated in most neurodegenerative diseases, and there is evidence that they play critical roles in disease pathology. For example, TNF-α is a potent inducer of cellular adhesion molecules in astrocytes [24]. It can also induce chemokines expression in astrocytes, thus promoting demyelination and oligodendrocyte injury [25–27]. IL-6 is also important for inflammatory response and is involved in reactive gliosis [28]. In addition, TNF-α and IL-6 production by astrocytes can lead to increased permeability of the blood-brain barrier (BBB), which normally severely restricts the entry of leukocytes into the CNS [29]. Also, IL-1β, a key contributor to brain inflammation, can cause sustained activation of NF-κB in astrocytes resulting in production of adhesion molecules and chemokines [7]. Therefore, TET-exerted protective effects via inhibiting TNF-α, IL-6 and IL-1β production.
We found that TET-inhibited MIP-1α and VCAM-1 mRNA expression in LPS stimulated astrocytes. MIP-1α is expressed in reactive astrocytes in a number of acute and chronic neuroinflammation conditions, inducing chemokines and cytokines production [1]. MIP-1α has been suggested to promote the recruitment of various leukocyte subtypes [30, 31]. In addition, VCAM-1 is an adhesion molecule that is important for the migration of leukocyte through BBB. VCAM-1 is also involved in the formation of destructive CNS inflammatory lesions, such as experimental autoimmune encephalomyelitis (EAE) and MS [8]. In recent EAE study based on NEMOCNS-KO, van Loo et al. suggested that VCAM-1 might be critical for T lymphocyte persistent activation [21]. We proposed that TET-inhibited the expression of MIP-1α and VCAM-1, which in turn inhibited the migration of inflammatory cells into the CNS.
NF-κB plays an essential role in inflammation, cell proliferation and apoptosis [5]. In resting cells, through masking the nuclear localization signal, NF-κB transcription factors are retained in the cytosol by inhibitory proteins, including IκBα, IκBβ, IκBɛ and IκBγ. After receiving a stimulatory signal such as LPS, the IκBα inhibitory protein is phosphorylated at both 32 and 36 serine residues by IKKs, resulting in ubiquitination and subsequent degradation by proteosome. These sequential yet highly regulated signal transduction events then cause nuclear translocation of NF-κB transcription factors from cytosol to nucleus [12]. NF-κB in the nucleus binds to the regulatory region in the gene promoter, and is involved in the induction of many cytokines, chemokines and adhesion molecules that mediate the recruitment and activation of immune cells. Now the IKK/NF-κB signaling pathway is under intensive investigation as a therapeutic target. Multiple evidences indicate that IKKβ is primarily responsible for the activation of NF-κB in response to proinflammatory stimuli, whereas IKKα is essential for epidermal differentiation and B-cell maturation [32]. Most studies have been focused on developing small molecule inhibitors to inhibit IKKβ because of its catalytic activities. During CNS injury and cerebral ischemia, inhibition of astroglial NF-κB activity reduced inflammation and improved functional recovery [33, 34]. TET had been found to intervene with NF-κB activation and nuclear translocation in vitro in several cell lines [11–13]. Our results showed that TET inhibited the activation of NF-κB. Further studies indicated that TET successfully prevented IκBα phosphorylation and degradation in activated astrocytes. Moreover, the blockade was associated with suppressed phosphorylation of IKKα and IKKβ. These subsequent molecular changes suggested that the inhibition of NF-κB transcriptional activation might account partly for the inhibition of TET. In addition, there are also reports that TET could inhibit nuclear translocation of p65 [12]. In addition, there were reports that mitogen-activated protein kinases (MAPKs) and protein kinase C (PKC) also regulate astrocyte inflammatory responses [35–37]. Whether TET can inhibit these alternative pathways in activated astrocytes need further investigation.
In conclusion, our results demonstrated for the first time that TET suppressed LPS-induced astrocyte activation and reduced the release of inflammatory mediators, including NO, cytokines, chemokines and adhesion molecules. Such suppressive effects were likely carried out through inhibition of IKKs-IκBα-NF-κB signaling pathway. Our findings offers new therapeutic targets with the potential of regulating astrocyte-mediated inflammatory diseases in the CNS.
References
Ambrosini E, Aloisi F (2004) Chemokines and glial cells: a complex network in the central nervous system. Neurochem Res 29:1017–1038. doi:10.1023/B:NERE.0000021246.96864.89
Tuppo EE, Arias HR (2005) The role of inflammation in Alzheimer’s disease. Int J Biochem Cell Biol 37:289–305. doi:10.1016/j.biocel.2004.07.009
Holley JE, Gveric D, Newcombe J, Cuzner ML, Gutowski NJ (2003) Astrocyte characterization in the multiple sclerosis glial scars. Neuropathol Appl Neurobiol 29:434–444. doi:10.1046/j.1365-2990.2003.00491.x
Volterra A, Meldoles J (2005) Astrocytes, from brain glue to communication elements: the revolution continues. Nat Rev Neurosci 6:626–640. doi:10.1038/nrn1722
Li S, Wang L, Berman MA, Zhang Y, Dorf ME (2006) RNAi screen in mouse astrocytes identifies phosphatases that regulate NF-kappaB signaling. Mol Cell 24:497–509. doi:10.1016/j.molcel.2006.10.015
Bal-Price A, Brown GC (2000) Nitric-oxide-induced necrosis and apoptosis in PC12 cells mediated by mitochondria. J Neurochem 75:1455–1464. doi:10.1046/j.1471-4159.2000.0751455.x
Moynagh PN (2005) The interleukin-1 signaling pathway in astrocytes: a key contributor to inflammation in the brain. J Anat 207:265–269. doi:10.1111/j.1469-7580.2005.00445.x
Gimenez MA, Sim JE, Russell JH (2004) TNFR1-dependent VCAM-1 expression by astrocytes exposes the CNS to destructive inflammation. J Neuroimmunol 151:116–125. doi:10.1016/j.jneuroim.2004.02.012
Jang BC, Lim KJ, Paik JH, Cho JW, Baek WK, Suh MH et al (2004) Tetrandrine-induced apoptosis is mediated by activation of caspases and PKC-delta in U937 cells. Biochem Pharmacol 67:1819–1829. doi:10.1016/j.bcp.2004.01.018
Wu SJ, Ng LT (2007) Tetrandrine inhibits proinflammatory Cytokines, iNOS and COX-2 expression in human monocytic cells. Biol Pharm Bull 30:59–62. doi:10.1248/bpb.30.59
Chen F, Sun S, Kuhn DC, Lu Y, Gaydos LJ, Shi X et al (1997) Tetrandrine inhibits signal-induced NF-kappa B activation in rat alveolar macrophages. Biochem Biophys Res Commun 231:99–102. doi:10.1006/bbrc.1997.6057
Ho LJ, Juan TY, Chao P, Wu WL, Chang DM, Chang SY et al (2004) Plant alkaloid tetrandrine downregulates IkappaBalpha kinases-IkappaBalpha-NF-kappaB signaling pathway in human peripheral blood T cell. Br J Pharmacol 143:919–927. doi:10.1038/sj.bjp.0706000
Ho LJ, Chang DM, Lee TC, Chang ML, Lai JH (1999) Plant alkaloid Tetrandrine downregulates protein kinase C-dependent signaling pathway in T cells. Eur J Pharmacol 367:389–398. doi:10.1016/S0014-2999(98)00941-8
Xue Y, Wang Y, Feng DC, Xiao BG, Xu LY (2008) Tetrandrine suppresses lipopolysaccharide-induced microglial activation by inhibiting NF-kappaB pathway. Acta Pharmacol Sin 29:245–251. doi:10.1111/j.1745-7254.2008.00734.x
Chung IY, Benveniste EN (1990) Tumor necrosis factor-alpha production by astrocytes: induction by lipopolysaccharide, IFN-gamma, and IL-1 beta. J Immunol 144:2999–3007
Monje ML, Toda H, Palmer TD (2003) Inflammatory blockade restores adult hippocampal neurogenesis. Science 302:1760–1765. doi:10.1126/science.1088417
Xu LY, Yang JS, Xiao BG (2002) TGF-beta1-conditioned glial cell-derived dendritic cells inhibit expansion of MBP-reactive T cells in vitro. Neuroreport 13:35–39. doi:10.1097/00001756-200201210-00012
Dong Y, Benveniste EN (2001) Immune function of astrocytes. Glia 36:180–190. doi:10.1002/glia.1107
Karin M, Lin A (2002) NF-κB at the crossroads of life and death. Nat Immunol 3:221–227. doi:10.1038/ni0302-221
Ghosh S, Karin M (2002) Missing pieces in the NF-κB puzzle. Cell 109(Suppl):S81–S96. doi:10.1016/S0092-8674(02)00703-1
van Loo G, De Lorenzi R, Schmidt H, Huth M, Mildner A, Schmidt-Supprian M et al (2006) Inhibition of transcription factor NF-κB in the central nervous system ameliorates autoimmune encephalomyelitis in mice. Nat Immunol 7:954–961. doi:10.1038/ni1372
Maragakis NJ, Rothstein JD (2006) Mechanisms of Disease: astrocytes in neurodegenerative disease. Nat Clin Pract Neurol 2:679–689. doi:10.1038/ncpneuro0355
Pahan K, Sheikh FG, Khan M, Namboodiri AM, Singh I (1998) Sphingomyelinase and ceramide stimulate the expression of inducible nitric-oxide synthase in rat primary astrocytes. J Biol Chem 273:2591–2600. doi:10.1074/jbc.273.5.2591
Satoh J, Kastrukoff LF, Kim SU (1991) Cytokine-induced expression of intercellular adhesion molecule-1 (ICAM-1) in cultured human oligodendrocytes and astrocytes. J Neuropathol Exp Neurol 50:215–226. doi:10.1097/00005072-199105000-00004
Hayashi M, Luo Y, Laning J, Strieter RM, Dorf ME (1995) Production and function of monocyte chemoattractant protein-1 and other beta-chemokines in murine glial cells. J Neuroimmunol 60:143–150. doi:10.1016/0165-5728(95)00064-9
Hurwitz AA, Lyman WD, Berman JW (1995) Tumor necrosis factor alpha and transforming growth factor beta upregulate astrocyte expression of monocyte chemoattractant protein-1. J Neuroimmunol 57:193–198. doi:10.1016/0165-5728(95)00011-P
Louis JC, Magal E, Takayama S, Varon S (1993) CNTF protection of oligodendrocytes against natural and tumor necrosis factor-induced death. Science 259:689–692. doi:10.1126/science.8430320
Klein MA, Moller JC, Jones LL, Bluethmann H, Kreutzberg GW, Raivich G (1997) Impaired neuroglial activation in interleukin-6-deficient mice. Glia 19:227–233. doi:10.1002/(SICI)1098-1136(199703)19:3 < 227::AID-GLIA5 > 3.0.CO;2-W
Abbott NJ (2002) Astrocyte–endothelial interactions and blood-brain barrier permeability. J Anat 200:629–638. doi:10.1046/j.1469-7580.2002.00064.x
Ajuebor MN, Das AM, Virag L, Szabo C, Perretti M (1999) Regulation of macrophage inflammatory protein-1 alpha expression and function by endogenous interleukin-10 in a model of acute inflammation. Biochem Biophys Res Commun 255:279–282. doi:10.1006/bbrc.1999.0196
Olson TS, Ley K (2002) Chemokines and chemokine receptors in leukocyte trafficking. Am J Physiol Regul Integr Comp Physiol 283:R7–R28
Shiao YJ, Lin YL, Sun YH, Chi CW, Chen CF, Wang CN (2005) Falcarindiol impairs the expression of inducible nitric oxide synthase by abrogating the activation of IKK and JAK in rat primary astrocytes. Br J Pharmacol 144:42–51. doi:10.1038/sj.bjp.0706022
Brambilla R, Bracchi-Ricard V, Hu WH, Frydel B, Bramwell A, Karmally S et al (2005) Inhibition of astroglial nuclear factor kappa B reduces inflammation and improves functional recovery after spinal cord injury. J Exp Med 202:145–156. doi:10.1084/jem.20041918
Zhang W, Potrovita I, Tarabin V, Herrmann O, Beer V, Weih F et al (2005) Neuronal activation of NF-kappaB contributes to cell death i/n cerebral ischemia. J Cereb Blood Flow Metab 25:30–40. doi:10.1038/sj.jcbfm.9600004
Bhat NR, Zhang P, Lee JC, Hogan EL (1998) Extracellular signal-regulated kinase and p38 subgroups of mitogen-activated protein kinases regulate inducible nitric oxide synthase and tumor necrosis factor-alpha gene expression in endotoxin-stimulated primary glial cultures. J Neurosci 18:1633–1641
Schumann RR, Pfeil D, Freyer D, Buerger W, Lamping N, Kirschning CJ et al (1998) Lipopolysaccharide and pneumococcal cell wall components activate the mitogen activated protein kinases (MAPK) erk-1, erk-2, and p38 in astrocytes. Glia 22:295–305. doi:10.1002/(SICI)1098-1136(199803)22:3 < 295::AID-GLIA8 > 3.0.CO;2-4
Sun LL, Cheng C, Liu HO, Shen CC, Xiao F, Qin J et al (2007) Src suppressed C kinase substrate regulates the lipopolysaccharide-induced TNF-alpha biosynthesis in rat astrocytes. J Mol Neurosci 32:16–24. doi:10.1007/s12031-007-0003-x
Acknowledgments
This work was supported by grants from the Science and Technology Commission of Shanghai Municipality (04DZ14902), Shanghai Leading Academic Discipline Project (T0206), and the Knowledge Innovation Program of the Chinese Academy of Sciences (J0171-1905).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, ST., Wang, Y., Xue, Y. et al. Tetrandrine suppresses LPS-induced astrocyte activation via modulating IKKs-IκBα-NF-κB signaling pathway. Mol Cell Biochem 315, 41–49 (2008). https://doi.org/10.1007/s11010-008-9787-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-008-9787-4