Abstract
Alterations in lipid metabolism and genetic predisposition are major risk factors for coronary artery disease (CAD). Variations in genes involved in lipid metabolism may act synergistically to confer risk or protection against CAD. The objective of the present study was to determine such interactions in variants of apolipoprotein E and apolipoprotein A1 genes. One hundred and forty subjects with clinically confirmed CAD and 100 unrelated normal subjects participated in the study. Multiple regression analysis was used to relate lipid and apolipoprotein profiles with genotypes. Odd ratios were calculated for various combinations of ApoE and ApoA1 genotypes. Prevalence of ApoE ‘E4’ and ApoA1 ‘A’ and ‘T’ alleles was significantly higher in patients than controls. Serum apolipoprotein E and apolipoprotein A1 levels were significantly lower in CAD patients than controls. When lipid parameters were related to genotypes, the polymorphisms associated to various markers were in agreement with previous reports. ApoE 2/4 genotype in combination with either ApoA1 heterozygous GA or CT genotype conferred higher risk of CAD. E3 allele in homozygous or heterozygous state in combination with ApoA1+83 CC genotype conferred highest protection (P < 0.05). Thus, it appears that ApoE and ApoA1 gene variants may act synergistically to associate with risk and protection against CAD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathogenesis of coronary artery disease (CAD) is associated with multiple genetic and environmental risk factors. Several candidate genes related with lipid and lipoprotein metabolism have been studied for their association with the CAD. There is a wealth of literature on the ApoE and ApoAI polymorphism particularly for their effects on lipid profiles and CAD risk. Multiple genetic variations in apolipoprotein E and apolipoprotein A1 have been shown to influence lipoprotein metabolism and the plasma concentration of total cholesterol (TC), LDL cholesterol, apo B, and apo E, and confer risk for CAD. Apolipoprotein E is involved in cholesterol transport and is encoded by a polymorphic gene. Three common alleles designated E2, E3, and E4 code for three apo E isoforms E2, E3, and E4. ApoE4 has been found to be associated with higher plasma cholesterol levels, increased risk for CAD and subjects with E4/4 genotype showed an earlier onset of the disease [1–4]. However, association between CAD and ApoE gene variants has been found to be inconsistent and vary in different ethnic populations [5, 6].
Two polymorphisms of ApoA1 gene namely G to A substitution at −75 bp of transcription start site and C to T substitution at +83 bp have been implicated in susceptibility to CAD and shown to influence plasma lipid levels [7, 8]. Individuals carrying the A1 allele have been shown to have higher concentrations of ApoA1 and HDL-C [9–14]; however, the results have been inconsistent and inconclusive, with few studies reporting either no association [15–17] or negative association [18] between Apo1 alleles and plasma lipids.
Participation of single genes in a pathogenesis of complex diseases such as atherosclerosis and CAD is relatively small, but coexistence of several polymorphic variants of candidate genes may have higher impact on disease etiology. Several recent studies have shown that combinatorial effects of candidate genes may be better predictors of disease risk than the individual genes [19–21]. Although, ApoE and ApoAI gene variants are known to modulate plasma lipid levels and have been found to be associated with CAD, the co-occurrence of ApoE and ApoA1 gene polymorphisms on risk of CAD and lipid levels has not been evaluated. The present study was carried out: (a) to study the independent influence of ApoE and ApoA1 genotypes on lipids and apolipoprotein E and apolipoprotein A1 levels among Asian Indian patients of North Indian origin with premature CAD and (b) to determine combined impact of co occurrence of ApoE and ApoA1 polymorphisms on the risk of CAD and on serum lipid levels.
Materials and methods
Study population
The study was carried out on North Indian Punjabi population. The study subjects comprised of 140 clinically confirmed CAD patients (age <50 years), attending the cardiology Out Patients Department of Nehru Hospital at PGIMER, Chandigarh. One hundred age- and sex-matched subjects with normal clinical examination, normal ECG, negative stress test, and with no family history of CAD or diabetes were recruited as controls. The study was approved by the Institute Ethics Committee and an informed consent was obtained from all the subjects enrolled in the study. An overnight fasting venous blood sample was obtained and processed for biochemical estimations and genomic DNA isolation.
Biochemical analysis
Serum TC, triglycerides (TG), and high-density cholesterol (HDL) were measured using commercial kits (Accurex, India). The value of low-density lipoprotein was determined using Friedwald’s equation LDL − C = TC − (HDL + TG/5). Serum ApoA1 and ApoE were determined using their respective kits (Spinreact, Spain and Diiachi, Tokyo).
ApoE genotyping
ApoE genotyping was done by the method of Wenham et al. [22]. PCR was performed in a 25 μl reaction mixture containing 100 ng DNA, 2.0 mM Mg2+, 0.2 mM dNTP, and 1 U Taq DNA polymerase. The amplification protocol consisted of an initial denaturation at 95°C for 5 min, followed by 28 cycles of denaturation, primer annealing, and extension at 94, 60, and 72°C for 1 min each and final extension at 72°C for 5 min. An aliquot of 20 μl of amplified product was digested with 2 units Hha1 at 37°C for 15 h. The digested products were visualized on 12% polyacrylamide gel following silver staining (Fig. 1).
ApoA1 genotyping
ApoA1 genotyping was done as described by Paul et al. [12]. PCR was performed in 25 μl containing 100 ng DNA, 2.5 mM Mg2+, 0.2 mM dNTP, and 1 U Taq DNA polymerase. The amplification protocol consisted of an initial denaturation at 95°C for 5 min, followed by 35 cycles of denaturation, primer annealing, and extension at 94, 62, and 72°C for 1 min each and final extension at 72°C for 5 min. An aliquot of 20 μl of amplified product was digested with 2.5 units Msp1 at 37°C for 15 h. The digested products were visualized on 12% polyacrylamide gel following silver staining (Fig. 2).
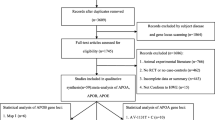
Statistical analysis
Allelic frequencies were estimated by a gene count method and were tested for Hardy-Weinberg equilibrium. Differences of allele and genotype frequencies were compared using the χ2 test. The student t-test was used to compare means, and ANOVA was used with Tukey post hoc comparison. In order to estimate the risk of CAD, odd ratios were calculated by multiple logistic regression analysis after age and sex adjustments. When the number of subjects in the group was less than ten, the Fisher’s correction was used. Statistical significance was set at P < 0.05. For two- and three-way interactions, Bonferroni correction was applied and P < 0.016 was considered significant. All statistical analyses were performed using SPSS (Statistical Package for Social Sciences) for windows (Version 10).
Results
The demographic characteristics of the patients and control subjects are given in Table 1. HDL-Cholesterol, ApoE, and ApoA1 were significantly decreased (P < 0.05), and TG levels were significantly increased in patients as compared to controls (P < 0.05). Multiple logistic regression analysis of known predictors of CAD confirmed the independent role of age (OR 1.36, 95% CI 1.03–1.80, P < 0.05), male gender (OR 0.001, 95% CI 0.00–0.29, P < 0.05), plasma ApoA1 (OR 0.001, 95% CI 0.00–0.03, P < 0.05) and plasma ApoE (OR 0.02, 95% CI 0.00–0.24, P < 0.05) as risk factors for CAD in our population. Smoking was also found to be significantly associated with risk of CAD (P < 0.05).
Genotypes
The percentage prevalence of genotypes and allele frequencies of ApoE and ApoA1 are given in Tables 2 and 3. Prevalence of ApoE 4/4 genotype, ApoA1-75 AA, and ApoA+83 TT genotypes was significantly higher in patients as compared to controls (P < 0.05). ApoE 4/4 genotype was associated with higher risk of the disease (OR 3.11, 95% CI, P < 0.05). Percentage prevalence of E2 (21.07%) and E4 allele (49.29%) was also significantly higher in patients as compared to controls (11.50%, 31%). ApoA1-75 ‘AA’ and ApoA+83 ‘TT’ genotypes showed higher odds ratio (Table 2), associated with increased risk of CAD. For ApoA1−75 and +83 polymorphisms, the prevalence of ‘A’ and ‘T’ alleles was significantly higher in patients (52.14%, 42.14%) as compared to controls (29.50%, 8%) (P < 0.05). An analysis of ApoA1 diplotypes showed that individuals with AA/TT (OR 8.44), GA/CT (OR 30.53), and AA/CT (OR 14.60) diplotypes had higher risk of CAD (Table 4).
Apolipoprotein E, apolipoprotein AI genotypes, and lipid levels
Associations of ApoA1 and ApoE genotypes with lipid profile and apolipoprotein levels are shown in Table 5. Patients with ApoE 3/3 and ApoE 3/4 genotypes had significantly lower HDL-C levels than controls. HDL-C levels were also significantly lower in patients with ApoA1 AA and CC genotypes (P < 0.05). Patients with ApoA1−75 GG and +83 CC genotypes had higher TG levels than controls. Cholesterol levels were found to be higher in patients with E4/4 genotype as compared to patients with E2/2 genotype. LDL levels were also significantly higher in patients with E4/4 genotype compared to patients with E3/3 genotype. Apolipoprotein A1 was found to be significantly associated with ‘A’ allele among patients but not in controls.
Synergistic effect of ApoE and ApoA1 gene polymorphisms
Subgroups were formed according to the ApoE and ApoA1 polymorphisms. Both two- and three-way interactions were analyzed. Genotype combinations conferring protection and risk to CAD were identified. Only those combinations which were significantly associated with either risk or protection of CAD are shown (Tables 6 and 7). ApoE 2/4 genotype in combination with heterozygous Msp1 −75 (GA) or +83 bp (CT) ApoA1 genotypes showed odd ratio of 5.88 and 19.46, respectively, indicating association with significantly increased risk of CAD (P < 0.05). This significance was abolished for E2/4 and GA genotypes after Bonferroni correction. ApoE 3/4 genotype in combination with heterozygous C/T genotype of ApoA1 also showed increased risk of CAD (OR 6.02, P < 0.001).
Three-way interaction between ApoE genotypes in combination with ApoA1 diplotypes showed that ApoE3/4 genotype in combination with ApoA1 GG/CC diplotype was most prevalent in controls (OR 0.06, CI 95%, P < 0.001). E3 allele in homozygous or heterozygous state in combination with ApoA1+83 CC genotype conferred highest protection (P < 0.05).
Discussion
The prevalence and mortality rates of CAD have been known to be higher in Indians than the Western population. Most data on lipid levels in Indians have been obtained from studies on migrant Asian Indians. There are insufficient data on lipid profile and other conventional risk factors in Indian patients living within India. We observed normal cholesterol, LDL-C, decreased HDL-C, and raised TG levels in our patient group with premature CAD. Our results are in agreement with those reported earlier for Asian Indians [23] indicating that CAD occurs at much lower levels of TC and low-density lipoprotein cholesterol in northern Indians than other populations, and high triglyceride and low high-density lipoprotein levels are more of a universal phenomenon in this population. The absence of traditional dyslipidemia among Indian patients has also prompted studies on role of non-traditional risk factors in CAD in Asian Indians. Low serum levels of ApoAI and ApoE have been proposed to be independent risk factors for CAD and may initiate atherosclerosis, especially in patients with no major risk factors [24]. We too observed significantly lower levels of ApoAI and ApoE in our patients and found that higher ApoA1 and ApoE levels were protective against CAD in our subjects (ApoA1 OR 0.001, 95% CI 0.00–0.03, P < 0.05; ApoE OR 0.02, 95% CI 0.00–0.24, P < 0.05). Our results suggest that quantitation of apolipoproteins could be another useful parameter to identify subjects at risk of CAD and may assume importance in the definite subset of Indian patients with normal levels of cholesterol and LDL-C and an early-onset of CAD.
Genetic variations at the ApoE locus have been found to influence the risk of CAD and myocardial infarction (MI) in different ethnic populations. In India, data on association between ApoE polymorphism and CAD are limited and inconclusive. Conflicting studies indicating an increased prevalence of ApoE4 allele in patients [25] and a lack of association between genotype prevalence and CAD have been reported [26]. These conflicting reports could be due to regional variations in genotype frequencies among the populations studied or small sample size in these studies [27, 28]. We found a significant higher prevalence of ApoE4/4 genotype compared to controls and E4 allele to be associated with higher risk of the disease in our patients who were all from northern India and were selected on the basis of rigid clinical phenotype of early onset of disease. Our study confirms a positive association of E4/4 genotype with higher risk of premature CAD in our patients similar to those observed in other ethnic groups.
Studies in several different populations have shown varied association of ApoAI polymorphisms and risk of CAD [29–32]. A higher but non-significant prevalence of ApoA1-75 ‘A’ allele has been reported in CAD patients of north Indian origin [19]. We observed significantly higher frequency of ApoA1-75 AA and ApoA+83 TT genotypes in CAD patients and co-occurrence of these genotypes further increased the risk of CAD as indicated by higher odd ratio (OR 8.44). Our results are similar to those reported by Wang et al. [17] who also found homozygous AA and TT genotypes to be associated with CAD in Australian Caucasian population.
ApoE and ApoAI gene variants may influence serum lipid and lipoprotein metabolism; for example, ApoE4 isoform, which has a higher affinity for LDL-receptor, could lead to increased TC, LDL-C, and apo B levels by down regulating these receptors. We observed higher cholesterol and LDL-C levels in patients with ApoE4/4 genotypes. These results are similar to those reported earlier in other populations [33–36] and confirm the strong influence of ApoE4 allele on increased cholesterol levels. However, none of the ApoE genotypes was found to be associated with the raised TG in the present study, whereas a strong association between TG and ApoE4 genotype has been reported in Caucasian population. It appears that genes such as lipoprotein lipase and ApoC3 that are also known to modulate TG levels may be playing a more dominant role in modulating TG levels in our population [37].
Besides ApoE, ApoAI polymorphisms were also seen to influence plasma ApoAI concentrations in the present study. We observed higher serum ApoAI levels in patients carrying ‘A’ allele. An association between ApoAI ‘A’ allele and higher concentrations of ApoA1 and HDL-C has been reported in Caucasian populations [9, 10, 32]. However, we did not observe any association between HDL-C and ApoAI genotypes, which could be either due to ethnic or environmental differences as Asian Indians tend to have lower HDL-C levels [38].
Since ApoE and ApoAI alleles showed significant association with the risk of CAD and were found to influence plasma lipid levels, we also examined the combined effects of genetic polymorphisms in these two genes on the risk of CAD. We observed that individuals with ApoE4 allele in association with ApoA1 ‘A’ and ‘T’ alleles were more susceptible to CAD. Moreover we also observed that ApoE3 allele in combination with ApoA1 ‘G’ allele was protective against CAD. Although ApoA1 ‘A’ and ApoE4 alleles have been shown to be associated with increased susceptibility to CAD, ours is the first study showing the additive effects of these genotypes on susceptibility to CAD. A synergistic effect between ApoE and AGT polymorphisms and MI has been also observed [39] which has been attributed to higher cholesterol levels in patients with AGT-TT + ApoE4 allele carriers. Zak et al. [21] have also reported a considerably higher frequency of contemporaneous carriers of two or three proatherosclerotic variants of candidate genes in CAD patients. Thus, it appears that co-occurrence of polymorphic alleles of genes involved in the disease process may increase the risk of the disease.
Conclusions
Our results indicate that aggregate effects of candidate gene loci such as ApoE and ApoAI could significantly contribute to increased risk of CAD even though individual effect of these gene variations on the disease may be small. If studies based on other populations confirm our results, simultaneous genotyping of ApoE and ApoA1 polymorphisms could identify individuals at a higher risk of developing CAD.
References
Davignon J, Gregg RE, Sing CF (1988) Apolipoprotein E polymorphism and atherosclerosis. Arteriosclerosis 8:1–21
Ilveskoski E, Perola M, Lehtimaki T, Laippala P, Savolainen V, Pajarinen J, Penttila A, Lalu KH, Mannikko A, Liesto KK, Koivula T, Karhunen PJ (1999) Age-dependent association of apolipoprotein E genotype with coronary and aortic atherosclerosis in middle-aged men: an autopsy study. Circulation 100:608–613
Van Bockxmeer FM, Mamotte CD (1992) Apolipoprotein epsilon 4 homozygosity in young men with coronary heart disease. Lancet 340:879–880
Wilson PW, Schaefer EJ, Larson MG, Ordovas JM (1996) Apolipoprotein E alleles and risk of coronary disease. A meta-analysis. Arterioscler Thromb Vasc Biol 16:1250–1255
Lenzen HJ, Assmann G, Buchwalsky R, Schulte H (1986) Association of apolipoprotein E polymorphism, low-density lipoprotein cholesterol, and coronary artery disease. Clin Chem 32:778–781
Utermann G, Hardewig A, Zimmer F (1984) Apolipoprotein E phenotypes in patients with myocardial infarction. Hum Genet 65:237–241
Ordovas JM, Civeira F, Genest J Jr, Craig S, Robbins AH, Meade T, Pocovi M, Frossard PM, Masharani U, Wilson PW et al (1991) Restriction fragment length polymorphisms of the apolipoprotein A-I, C-III, A-IV gene locus. Relationships with lipids, apolipoproteins, and premature coronary artery disease. Atherosclerosis 87:75–86
Wile DB, Barbir M, Gallagher J, Myant NB, Ritchie CD, Thompson GR, Humphries SE (1989) Apolipoprotein A-I gene polymorphisms: frequency in patients with coronary artery disease and healthy controls and association with serum apo A-I and HDL-cholesterol concentration. Atherosclerosis 78:9–18
Jeenah M, Kessling A, Miller N, Humphries S (1990) G to A substitution in the promoter region of the apolipoprotein AI gene is associated with elevated serum apolipoprotein AI and high density lipoprotein cholesterol concentrations. Mol Biol Med 7:233–241
Meng QH, Pajukanta P, Valsta L, Aro A, Pietinen P, Tikkanen MJ (1997) Influence of apolipoprotein A-1 promoter polymorphism on lipid levels and responses to dietary change in Finnish adults. J Intern Med 241:373–378
Pagani F, Sidoli A, Giudici GA, Barenghi L, Vergani C, Baralle FE (1990) Human apolipoprotein A-I gene promoter polymorphism: association with hyperalphalipoproteinemia. J Lipid Res 31:1371–1377
Paul-Hayase H, Rosseneu M, Robinson D, Van Bervliet JP, Deslypere JP, Humphries SE (1992) Polymorphisms in the apolipoprotein (apo) AI-CIII-AIV gene cluster: detection of genetic variation determining plasma apo AI, apo CIII and apo AIV concentrations. Hum Genet 88:439–446
Saha N, Tay JS, Low PS, Humphries SE (1994) Guanidine to adenine (G/A) substitution in the promoter region of the apolipoprotein AI gene is associated with elevated serum apolipoprotein AI levels in Chinese non-smokers. Genet Epidemiol 11:255–264
Xu CF, Angelico F, Del Ben M, Humphries S (1993) Role of genetic variation at the apo AI-CIII-AIV gene cluster in determining plasma apo AI levels in boys and girls. Genet Epidemiol 10:113–122
Barre DE, Guerra R, Verstraete R, Wang Z, Grundy SM, Cohen JC (1994) Genetic analysis of a polymorphism in the human apolipoprotein A-I gene promoter: effect on plasma HDL-cholesterol levels. J Lipid Res 35:1292–1296
Civeira F, Pocovi M, Cenarro A, Garces C, Ordovas JM (1993) Adenine for guanine substitution −78 base pairs 5′ to the apolipoprotein (APO) A-I gene: relation with high density lipoprotein cholesterol and APO A-I concentrations. Clin Genet 44:307–312
Wang XL, Liu SX, McCredie RM, Wilcken DE (1996) Polymorphisms at the 5′-end of the apolipoprotein AI gene and severity of coronary artery disease. J Clin Invest 98:372–377
Matsunga A, Sasaki J, Mori T (1995) Apolipoprotein A1 gene promoter polymorphism in patients with coronary heart disease and healthy controls. Nutr Metab Cardiovasc Dis 5:269
Chhabra S, Narang R, Krishnan LR, Vasisht S, Agarwal DP, Srivvastava LM, Manchana SC, Das N (2003) Apolipoprotein A1-75 G/A and Apolipoprotein c3 Sst1 Polymorphisms in the risk assessment of coronary artery disease. Trends Clin Biochem Lab Med 186–193
Salah D, Bohnet K, Gueguen R, Siest G, Visvikis S (1997) Combined effects of lipoprotein lipase and apolipoprotein E polymorphisms on lipid and lipoprotein levels in the Stanislas cohort. J Lipid Res 38:904–912
Zak I, Balcerzyk A, Sarecka B, Niemiec P, Ciemniewski Z, Dylag S (2005) Contemporaneous carrier-state of two or three “proatherosclerotic” variants of APOE, ICAM1, PPARA and PAI-1 genes differentiate CAD patients from healthy individuals. Clin Chim Acta 362:110–118
Wenham PR, Price WH, Blandell G (1991) Apolipoprotein E genotyping by one-stage PCR. Lancet 337:1158–1159
Goel PK, Bharti BB, Pandey CM, Singh U, Tewari S, Kapoor A, Garg N, Sinha N (2003) A tertiary care hospital-based study of conventional risk factors including lipid profile in proven coronary artery disease. Indian Heart J 55:234–240
Francis MC, Frohlich JJ (2001) Coronary artery disease in patients at low risk–apolipoprotein AI as an independent risk factor. Atherosclerosis 155:165–170
Ashavaid TF, Todur SP (2001) Study of lipoprotein (a) levels and apolipoprotein E polymorphism in subjects at risk for CHD. AACC Mol Pathol Div 13:2
Luthra K, Bharghav B, Chabbra S, Das N, Misra A, Agarwal DP, Pandey RM, Srivastava LM (2002) Apolipoprotein E polymorphism in Northern Indian patients with coronary heart disease: phenotype distribution and relation to serum lipids and lipoproteins. Mol Cell Biochem 232:97–102
Balgir PP, Kaur M (2003) Restriction isotyping of apolipoprotein E among populations of Punjab, northwestern India. Hum Biol 75:771–776
Thelma BK, Juyal RC, Dodge HH, Pandav R, Chandra V, Ganguli M (2001) APOE polymorphism in a rural older population-based sample in India. Hum Biol 73:135–144
Kamboh MI, Aston CE, Nestlerode CM, McAllister AE, Hamman RF (1996) Haplotype analysis of two APOA1/MspI polymorphisms in relation to plasma levels of apo A-I and HDL-cholesterol. Atherosclerosis 127:255–262
Minnich A, DeLangavant G, Lavigne J, Roederer G, Lussier-Cacan S, Davignon J (1995) G–>A substitution at position −75 of the apolipoprotein A-I gene promoter. Evidence against a direct effect on HDL cholesterol levels. Arterioscler Thromb Vasc Biol 15:1740–1745
Sigurdsson G Jr, Gudnason V, Sigurdsson G, Humphries SE (1992) Interaction between a polymorphism of the apo A-I promoter region and smoking determines plasma levels of HDL and apo A-I. Arterioscler Thromb 12:1017–1022
Talmud PJ, Ye S, Humphries SE (1994) Polymorphism in the promoter region of the apolipoprotein AI gene associated with differences in apolipoprotein AI levels: the European Atherosclerosis Research Study. Genet Epidemiol 11:265–280
Eichner JE, Kuller LH, Ferrell RE, Meilahn EN, Kamboh MI (1990) Phenotypic effects of apolipoprotein structural variation on lipid profiles. III. Contribution of apolipoprotein E phenotype to prediction of total cholesterol, apolipoprotein B, and low density lipoprotein cholesterol in the healthy women study. Arteriosclerosis 10:379–385
Eto M, Watanabe K, Makino I (1989) Increased frequencies of apolipoprotein epsilon 2 and epsilon 4 alleles in patients with ischemic heart disease. Clin Genet 36:183–188
Luc G, Bard JM, Arveiler D, Evans A, Cambou JP, Bingham A, Amouyel P, Schaffer P, Ruidavets JB, Cambien F et al (1994) Impact of apolipoprotein E polymorphism on lipoproteins and risk of myocardial infarction. The ECTIM Study. Arterioscler Thromb 14:1412–1419
Stengard JH, Zerba KE, Pekkanen J, Ehnholm C, Nissinen A, Sing CF (1995) Apolipoprotein E polymorphism predicts death from coronary heart disease in a longitudinal study of elderly Finnish men. Circulation 91:265–269
Chhabra S, Narang R, Krishnan LR, Vasisht S, Agarwal DP, Srivastava LM, Manchanda SC, Das N (2002) Apolipoprotein C3 SstI polymorphism and triglyceride levels in Asian Indians. BMC Genet 3:9
Das S (2004) Presidential oration 2003 lipids, diabetes and coronary artery disease in Indians. Int J Diab Dev Countries 24:87
Batalla A, Alvarez R, Reguero JR, Hevia S, Iglesias-Cubero G, Alvarez V, Cortina A, Gonzalez P, Celada MM, Medina A, Coto E (2000) Synergistic effect between apolipoprotein E and angiotensinogen gene polymorphisms in the risk for early myocardial infarction. Clin Chem 46:1910–1915
Acknowledgments
Financial support to this work was provided by Indian Council for Medical Research (ICMR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rai, T.S., Khullar, M., Sehrawat, B.S. et al. Synergistic effect between apolipoprotein E and apolipoprotein A1 gene polymorphisms in the risk for coronary artery disease. Mol Cell Biochem 313, 139–146 (2008). https://doi.org/10.1007/s11010-008-9751-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-008-9751-3