Abstract
Two of the most potent vasoconstrictors, endothelin-1 (ET-1) and angiotensin II (Ang II), are upregulated in fructose hypertensive rats. It is unknown whether an interrelationship exists between these peptides that may contribute to the development of fructose-induced hypertension. The objective of this study was to investigate the existence of an interaction between the endothelin and renin angiotensin systems that may play a role in the development of fructose-induced hypertension. High fructose feeding and treatment with either bosentan, a dual endothelin receptor antagonist, or with L-158,809, an angiotensin type 1 receptor antagonist, were initiated simultaneously in male Wistar rats. Systolic blood pressure, fasted plasma parameters, insulin sensitivity, plasma Ang II, and vascular ET-1-immunoreactivity were determined following 6 weeks of high fructose feeding. Rats fed with a high fructose diet exhibited insulin resistance, hyperinsulinemia, hypertriglyceridemia, hypertension, and elevated plasma Ang II. Treatment with either bosentan or L-158,809 significantly attenuated the rise in blood pressure with no effect on insulin levels or insulin sensitivity in fructose-fed rats. Bosentan treatment significantly reduced plasma Ang II levels, while L-158,809 treatment significantly increased vascular ET-1-immunoreactivity in fructose-fed rats. Thus, treatment with the endothelin receptor antagonist prevented the development of fructose-induced hypertension and decreased plasma Ang II levels. These data suggest that ET-1 contributes to the development of fructose-induced hypertension through modulation of Ang II levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The metabolic syndrome is a clustering of cardiovascular risk factors. Key components of this syndrome include abdominal obesity, dyslipidemia, insulin resistance, and hypertension. The most accepted and unifying hypothesis proposes that insulin resistance is the major common underlying metabolic abnormality that contributes to the pathogenesis of the metabolic syndrome [1, 2]. In both humans and animal models, insulin resistance/hyperinsulinemia has been suggested to contribute causally toward the development of hypertension [3].
The fructose hypertensive rat (FHR) represents a model of acquired systolic hypertension in which starch present in standard laboratory rat chow is substituted with fructose. Rats fed with a high fructose diet exhibited several features observed in the metabolic syndrome, such as insulin resistance, hyperinsulinemia, hypertriglyceridemia, and hypertension [4]. This animal model is utilized to study the relationship between the metabolic disturbances and hypertension independent of obesity or genetic contributions. Increased production and/or activity of vasoactive mediators, such as endothelin-1 (ET-1) [5–7], angiotensin II (Ang II) [8–10], and thromboxane A2 (TxA2) [11], have been proposed as mechanisms that may mediate the link between insulin resistance/hyperinsulinemia and hypertension.
The endothelin (ET) system and the renin angiotensin system (RAS) are two of the most potent vasopressor mechanisms identified to date [12]. The ET system consists of 21 amino acid ET peptides and their receptors, ETA and ETB. ET-1 is the major peptide primarily produced by endothelial cells and is preferentially released toward vascular smooth muscle cells to produce sustained increases in vascular tone [13]. The RAS maintains cardiovascular homeostasis by regulating fluid and electrolyte balance, as well as vascular tone. The active component of the RAS is Ang II, a potent vasoconstrictor, which exerts its actions through AT1 or AT2 receptors. Most of the well-known functions of Ang II are mediated through AT1 receptors [14].
In conditions where both systems are activated, interrelationships between them have been proposed to contribute to the development of hypertension. For instance, chronic infusion of subpressor doses of both Ang II and ET-1 induced significant increases in systolic blood pressure (SBP), whereas a subpressor dose of either Ang II or ET-1 had no effect in conscious rats, leading the authors to suggest that the combined actions of both peptides may be involved in blood pressure regulation [15]. In fructose-fed rats, it has been reported that blood pressure was reduced by a greater degree in the presence of a combination treatment consisting of an ACE inhibitor, trandolapril, and an ET receptor antagonist, LU-135252, as compared to either treatment alone [16]. However, whether an interrelationship exists between these systems that contribute to the development of hypertension in fructose-fed rats is currently unknown.
The aim of this study was to investigate and define the existence of an interaction between the ET system and RAS that may play a role in the development of hypertension in insulin resistant fructose-fed rats. We determined the effects of a dual ET receptor antagonist, bosentan, or an AT1 receptor antagonist, L-158,809, on plasma levels of insulin, glucose, triglycerides, SBP, and insulin sensitivity. In addition, we assessed the effect of bosentan treatment on plasma Ang II levels and the effect of L-158,809 treatment on vascular ET-1-immunoreactivity (ET-1-ir). We hypothesized that both the ET system and RAS contribute to the development of hypertension in fructose-fed rats and that these systems are interconnected. Our data suggest that fructose-induced hypertension is dependent on the ability of ET-1 to modulate Ang II levels.
Materials and methods
Animals and experimental design
Forty-eight male Wistar rats were obtained from Charles River Laboratories (St-Constant, Quebec) at 5 weeks of age and randomly divided into six experimental groups: control vehicle-treated (C, n = 8), control bosentan-treated (CB, n = 8), control L-158,809-treated (CL, n = 8), fructose vehicle-treated (F, n = 8), fructose bosentan-treated (FB, n = 8), and fructose L-158,809-treated (FL, n = 8).
At 6 weeks of age, fasted (5 h) plasma parameters (glucose, insulin and triglycerides) and SBP were measured in all groups. At 7 weeks of age, rats in fructose-fed groups (F, FB, and FL) were started on a 60% fructose diet (Teklad Laboratory Diets, Madison, WI) for 6 weeks, whereas rats in control groups (C, CB, and CL) were maintained on standard laboratory rat chow containing 30% carbohydrate in the form of starch for the same period. Bosentan (CB and FB) or L-158,809 (CL and FL) treatment was initiated concurrently at a dose of 100 mg/kg or 1 mg/kg, respectively, suspended in 1% gum arabic administered via daily oral gavage for the duration of the study. The dose of bosentan and L-158,809 was chosen based on effective blood pressure lowering as reported in previous studies [5, 17–19]. Rats were housed on a 12-h light–dark cycle and received food and water ad libitum. At the end of the study, rats from all groups were euthanized with an overdose of pentobarbital (65 mg/kg, i.p.). Superior mesenteric arteries were isolated, cleaned of adherent connective tissue, and fixed in formalin to assess vascular ET-1-ir. This investigation conforms to the Canadian Council on Animal Care Guidelines on the Care and Use of Experimental Animals. All protocols were approved by the University of British Columbia Animal Care Committee.
Blood pressure measurement
Prior to obtaining blood pressure measurements, rats were preconditioned to the procedure. SBP was measured in conscious rats using the indirect non-invasive tail-cuff method without external preheating as previously described [4].
Oral glucose tolerance test and insulin sensitivity index
Following 6 weeks of study, all rats were fasted overnight (15 h) and subjected to an oral glucose tolerance test (OGTT). A 40% glucose solution was prepared and administered by oral gavage (1 g/kg) to conscious animals. Blood samples were obtained at 0, 10, 20, 30, 60, and 90 min following the glucose challenge. Plasma was separated and stored at −20°C until further analysis. The insulin sensitivity index (ISI) was calculated for each animal using data obtained from the OGTT and applied to the formula of Matsuda and DeFronzo [20], where ISI = 100/square root [(mean plasma glucose × mean plasma insulin) × (fasting plasma glucose × fasting plasma insulin)]. Values obtained with this methodology correlate highly with results obtained from the euglycemic hyperinsulinemic clamp technique [20].
Blood collection
Five hour fasted blood samples were collected from the tail vein for determination of plasma glucose, insulin, and triglyceride levels. Plasma samples were separated, aliquoted, and stored at −20°C until further analysis. At termination, blood was collected via cardiac puncture and placed into plastic tubes containing 0.44 mM ο-phenanthroline, 25 mM EDTA, 1 mM p-hydroxymercuribenzoic acid, and 0.12 mM pepstatin A for determination of plasma Ang II levels. Plasma samples were separated and stored at −20°C until analysis.
Immunohistochemistry and image analysis
Superior mesenteric arteries were embedded in paraffin and cut into 10-μm thick sections on a vibratome. Sections were mounted on slides, deparaffinized, and immunostained for ET-1-ir. Briefly, sections were incubated in 5% normal goat serum for 1 h at room temperature. Sections were incubated overnight in a humid atmosphere at 4°C with a rabbit anti-ET-1 antibody (1:500, Peninsula Laboratories; T4495, San Carlos, CA) diluted in phosphate buffered saline (PBS) containing 1% normal goat serum. Following three washes in PBS, sections were incubated with an Alexa 594-conjugated goat anti-rabbit IgG antibody (1:1600 diluted in PBS, Molecular Probes; A11037, Eugene, OR) for 90 min at room temperature. Negative controls were stained by omitting the primary antibody incubation. Immunoreactivity was not detected in the absence of primary antibody. Fluorescent images were captured using an Olympus Fluoview BX61 confocal microscope and analyzed using the Image Pro Analyzer 6.2 software. For semi-quantitative analysis of vascular ET-1-ir, the area of interest was chosen by outlining the intimal and medial layers of each section. Vascular ET-1-ir was evaluated within the area of interest and was based on the amount of immunopositive staining expressed as a proportion of the total area of interest.
Biochemical measurements
Plasma glucose levels were determined using a Beckman Glucose Analyzer II (Beckman, Fullerton, CA). Plasma triglycerides were measured using an enzymatic calorimetric assay from Boehringer Mannheim (Germany). Plasma insulin levels were determined using a radioimmunoassay kit from Linco Research (St. Charles, MO). Plasma Ang II levels were measured using an enzyme immunoassay kit from Cedarlane (Hornby, Ontario).
Reagents
All chemicals were of reagent grade and were purchased from Sigma (St. Louis, MO). Bosentan was a generous gift from Actelion Ltd. (Allschwil, Switzerland). L-158,809 was a generous gift from Merck Research Laboratories (Rahway, NJ).
Statistical analysis
All data are expressed as mean ± SEM. Statistical analysis of all data was performed using the Number Cruncher Statistical Software 2000 (NCSS, Kaysville, UT). Data with multiple time points were analyzed by General Linear Model ANOVA and inter-group comparisons of dependent variables were analyzed by one-way ANOVA. Given that we were interested in comparing either bosentan or L-158,809 treatment against vehicle-treated animals and not bosentan treatment against L-158,809 treatment, animals from the C and F groups were used to analyze the effects of bosentan treatment against vehicle-treatment, as well as the effects of L-158,809 treatment against vehicle-treatment. For all results, the Newman–Keuls test for post-hoc analysis was applied. A value of P < 0.05 was taken as the level of significance.
Results
General characteristics
General characteristics of rats following 6 weeks of bosentan or L-158,809 treatment are summarized in Tables 1 and 2, respectively. Body weight did not differ among the experimental groups. Food intake was slightly, but significantly, reduced in fructose-fed (F, FB, and FL) animals as compared to control (C, CB, and CL) animals. In addition, food intake was significantly reduced in the CL group as compared to the C group. Fasted plasma insulin levels of the F and FL groups were significantly elevated as compared to the C and CL groups. Fasted plasma glucose levels were slightly, but significantly, elevated in fructose-fed animals as compared to control animals. Treatment with either bosentan or L-158,809 had no effect on glucose or insulin levels in either fructose-fed or control animals. Fasted plasma triglycerides were significantly elevated in the F group. Chronic bosentan treatment significantly reduced elevated levels of triglycerides in fructose-fed rats, while chronic L-158,809 treatment had no effect.
Blood pressure
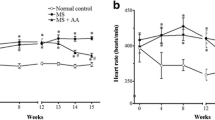
SBP was significantly elevated in the F group following 6 weeks of high fructose feeding (Fig. 1). Chronic treatment with either bosentan or L-158,809 significantly attenuated the increase in blood pressure in fructose-fed rats. Treatment with either bosentan or L-158,809 had no effect on blood pressure in the control rats.
OGTT responses
Plasma glucose and insulin profiles following an oral glucose challenge are shown in Figs. 2 and 3, respectively. High fructose feeding or treatment with either bosentan or L-158,809 had no effect on the glucose area under the curve (AUC). The insulin AUC of the F and FL groups were significantly elevated as compared to the C and CL groups. Comparisons of the ISI demonstrated that high fructose feeding significantly impaired insulin sensitivity (Fig. 4). Chronic treatment with either bosentan or L-158,809 did not alter insulin sensitivity in either control or fructose-fed animals.
Plasma Ang II
Plasma Ang II levels were significantly elevated following 6 weeks of high fructose feeding (Fig. 5). Chronic bosentan treatment completely prevented the increase in plasma Ang II levels in fructose-fed rats, while it had no effect in control animals. In contrast, treatment with L-158,809 resulted in significantly elevated plasma Ang II levels in both control and fructose-fed rats.
ET-1-ir microscopy and semi-quantitative analysis
Semi-quantitative analysis of vascular ET-1-ir in superior mesenteric arteries revealed significant elevations in the proportion of ET-1-ir in animals in the CL and FL groups as compared to arteries from the C and F groups (Fig. 6). Vascular ET-1-ir was slightly increased in arteries from fructose-fed rats, although this difference did not reach the statistical significance.
a Representative fluorescence images of immunohistochemical expression of ET-1 in superior mesenteric arteries from animals following 6 weeks of L-158,809 treatment. Arrows indicate positive immunostaining for ET-1 within the intimal and medial layers. b Semi-quantitative analysis of vascular ET-1-ir from animals following 6 weeks of L-158,809 treatment. Values are expressed as mean ± SEM, n = 8. ^P < 0.05 versus C, F
Discussion
In this study, treatment with either a dual ET receptor antagonist or an AT1 receptor antagonist prevented the development of hypertension, indicating that both the ET system and RAS play important roles in the development of fructose-induced hypertension. Chronic blockade of the ET system normalized Ang II levels, while blockade of the RAS increased ET-1-ir. These data suggest there is an interaction between the ET system and RAS, and that ET-1 may exert its effect through the RAS. To the best of our knowledge, this is the first study that has concurrently investigated the role of both the ET system and RAS in hypertension in fructose-fed rats. We have demonstrated that ET-1 contributes to the development of fructose-induced hypertension through modulation of Ang II levels.
The results of this study extend previous reports showing that blood pressure regulation is dependent on an interrelationship between the ET system and RAS. Studies in normotensive [21] and hypertensive dogs [22] and various rat models of experimental hypertension [23–25] have shown a greater hypotensive effect under conditions where both the ET system and RAS were antagonized as compared to the effect seen with antagonists of either system alone. Furthermore, treatment of rats with an ET receptor antagonist prevented the development of hypertension induced by Ang II infusion [26, 27], while treatment with an ACE inhibitor prevented the development of hypertension induced by ET-1 infusion [28]. Although these studies provide evidence for a potential link between the ET system and RAS in the maintenance of normal or elevated blood pressure, the nature of this interaction has been unclear. Our data suggest that in the setting of fructose-induced hypertension, elevations in Ang II are dependent on the actions of ET-1.
Recently, we demonstrated that bosentan treatment prevented the increase in cyclooxygenase 2 expression and normalized elevated levels of plasma thromboxane B2, a stable metabolite of TxA2, in fructose-fed rats [29]. These findings suggest that ET-1 also acts upstream of TxA2, a concept that has been previously suggested [30]. Further evidence suggests that ET-1 stimulates oxidative stress, another mediator thought to contribute to the pathogenesis of hypertension [31]. In DOCA-salt hypertension, selective blockade of ETA receptors normalized vascular superoxide production [32] and decreased plasma thiobarbituric acid reacting substances, a marker of systemic oxidative stress [33]. Given that oxidative stress is another proposed mechanism of fructose-induced hypertension [34], a potential role for ET-1 in stimulating oxidative stress in fructose-fed rats remains to be clarified. 
Superior mesenteric arteries from animals in the CL and FL groups showed significant increases in vascular ET-1-ir as compared to arteries from animals in the C and F groups. As expected, chronic blockade of the AT1 receptor resulted in significant elevations in plasma Ang II. As well, significant increases in vascular ET-1-ir were observed in both control and fructose-fed rats treated with L-158,809, suggesting a potential positive feedback loop between Ang II and ET-1. We believe that during chronic blockade of the AT1 receptor, elevations in Ang II result in a compensatory increase in ET-1 (inset). Arteries from animals in the F group showed a slight increase in vascular ET-1-ir as compared to arteries from animals in the C group, although this increase did not reach the statistical significance, perhaps due to the sample size and larger variability observed in the F group. Taken together, our results provide further evidence that ET-1 may play a central role in the development of fructose-induced hypertension through modulation of various vasoactive mediators.
Interestingly, we did not observe improvements in insulin sensitivity in fructose-fed rats treated with L-158,809, a finding that differs from previously published reports. Treatment with either an ACE inhibitor or AT1 receptor antagonist have previously been reported to reduce elevated insulin levels and/or improve insulin sensitivity in fructose-fed rats [9, 10]. The reasons for this discrepancy are unclear, but may be due to differences in the duration of fructose feeding/drug treatment or due to dose-dependent effects of the various drugs used.
Hypertriglyceridemia, and not insulin resistance/hyperinsulinemia, has been proposed to be a causal link in the development of fructose-induced hypertension [35]. Our data do not support this hypothesis given that the development of hypertension was attenuated in fructose-fed animals chronically treated with either bosentan or L-158,809, despite the presence of hypertriglyceridemia in fructose-fed animals treated with L-158,809. Similar observations have been made in fructose-fed rats treated with the AT1 receptor antagonists, losartan [36] or TCV-116 [37], or thromboxane synthase inhibitor, dazmegral [11]. Furthermore, a reduction in elevated triglycerides levels did not reduce the elevated blood pressure in fructose-fed rats [38, 39], supporting the concept of a triglyceride-independent component involved in the development of fructose-induced hypertension.
Conflicting reports exist on the interrelationship between ET-1 and Ang II. These differences may be due to the use of in vitro versus in vivo experiments, the use of different animal models of experimental hypertension, the duration of treatment, acute versus chronic effects of receptor blockade, or species differences that may exist in the regulation of the ET system and/or RAS. Although we were able to demonstrate a relationship between these two systems, this study was limited in its ability to determine whether the ET system affects the RAS through direct or indirect mechanisms. Bosentan may act to suppress Ang II levels by preventing the actions of ET-1 on ACE activity and aldosterone production given that previous reports demonstrated that ET-1 stimulates ACE activity [40, 41] and increases aldosterone production [42]. Alternatively, bosentan may indirectly affect Ang II levels by decreasing blood pressure and subsequently reducing the activation of the RAS. The compensatory increase in Ang II, secondary to L-158,809 treatment, may regulate vascular ET-1 expression at various levels of the RAS. Ang II has been shown to stimulate transcription of the prepro-ET-1 gene [12], increase the activity of the ET converting enzyme [40], and the release of ET-1 from vascular smooth muscle cells [43] and endothelial cells [44]. As it remains unclear where the specific site(s) of interaction(s) may occur, further investigation on the exact nature of this relationship is required.
In conclusion, results from this study demonstrate that either dual ET receptor antagonism or AT1 receptor blockade prevented the development of fructose-induced hypertension with no effects on insulin levels or insulin sensitivity. Chronic blockade of ET receptors resulted in normalized Ang II levels, while AT1 receptor blockade upregulated the levels of vascular ET-1. These data suggest that both the ET system and RAS are crucial players in the development of fructose-induced hypertension, with ET-1 contributing its effects through modulation of Ang II.
References
Reaven GM (1988) Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 37:1595–1607. doi:10.2337/diabetes.37.12.1595
Ginsberg HN (2000) Insulin resistance and cardiovascular disease. J Clin Invest 106:453–458. doi:10.1172/JCI10762
Reaven GM (1991) Insulin resistance, hyperinsulinemia, and hypertriglyceridemia in the etiology and clinical course of hypertension. Am J Med 90:7S–12S. doi:10.1016/0002-9343(91)90028-V
Hwang IS, Ho H, Hoffman BB, Reaven GM (1987) Fructose-induced insulin resistance and hypertension in rats. Hypertension 10:512–516
Verma S, Bhanot S, McNeill JH (1995) Effect of chronic endothelin blockade in hyperinsulinemic hypertensive rats. Am J Physiol 269:H2017–H2021
Verma S, Skarsgard P, Bhanot S, Yao L, Laher I, McNeill JH (1997) Reactivity of mesenteric arteries from fructose hypertensive rats to endothelin-1. Am J Hypertens 10:1010–1019. doi:10.1016/S0895-7061(97)00107-6
Juan CC, Fang VS, Hsu YP, Huang YJ, Hsia DB, Yu PC, Kwok CF, Ho LT (1998) Overexpression of vascular endothelin-1 and endothelin-A receptors in a fructose-induced hypertensive rat model. J Hypertens 16:1775–1782. doi:10.1097/00004872-199816120-00010
Erlich Y, Rosenthal T (1995) Effect of angiotensin-converting enzyme inhibitors on fructose induced hypertension and hyperinsulinaemia in rats. Clin Exp Pharmacol Physiol Suppl 22:S347–S349. doi:10.1111/j.1440-1681.1995.tb02949.x
Iyer SN, Katovich MJ (1996) Effect of acute and chronic losartan treatment on glucose tolerance and insulin sensitivity in fructose-fed rats. Am J Hypertens 9:662–668. doi:10.1016/0895-7061(96)00035-0
Higashiura K, Ura N, Takada T, Li Y, Torii T, Togashi N, Takada M, Takizawa H, Shimamoto K (2000) The effects of an angiotensin-converting enzyme inhibitor and an angiotensin II receptor antagonist on insulin resistance in fructose-fed rats. Am J Hypertens 13:290–297. doi:10.1016/S0895-7061(99)00174-0
Galipeau D, Arikawa E, Sekirov I, McNeill JH (2001) Chronic thromboxane synthase inhibition prevents fructose-induced hypertension. Hypertension 38:872–876
Rossi GP, Sacchetto A, Cesari M, Pessina AC (1999) Interactions between endothelin-1 and the renin-angiotensin-aldosterone system. Cardiovasc Res 43:300–307. doi:10.1016/S0008-6363(99)00110-8
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415. doi:10.1038/332411a0
Widdop RE, Jones ES, Hannan RE, Gaspari TA (2003) Angiotensin AT2 receptors: cardiovascular hope or hype? Br J Pharmacol 140:809–824. doi:10.1038/sj.bjp.0705448
Yoshida K, Yasujima M, Kohzuki M, Kanazawa M, Yoshinaga K, Abe K (1992) Endothelin-1 augments pressor response to angiotensin II infusion in rats. Hypertension 20:292–297
Ezra-Nimni O, Ezra D, Peleg E, Munter K, Rosenthal T (2003) Trandolapril and endothelin antagonist LU-135252 in the treatment of the fructose-induced hypertensive, hyperinsulinemic, hypertriglyceridemic rat. Am J Hypertens 16:324–328. doi:10.1016/S0895-7061(03)00003-7
Clozel M, Breu V, Gray GA, Kalina B, Loffler BM, Burri K, Cassal JM, Hirth G, Muller M, Neidhart W et al (1994) Pharmacological characterization of bosentan, a new potent orally active nonpeptide endothelin receptor antagonist. J Pharmacol Exp Ther 270:228–235
Gillies LK, Werstiuk ES, Lee RM (1998) Cross-over study comparing effects of treatment with an angiotensin converting enzyme inhibitor and an angiotensin II type 1 receptor antagonist on cardiovascular changes in hypertension. J Hypertens 16:477–486. doi:10.1097/00004872-199816040-00009
Tamura T, Said S, Andersen SM, McCune SA, Mochizuki S, Gerdes AM (2002) Temporal regression of myocyte hypertrophy in hypertensive, heart failure-prone rats treated with an AT1-receptor antagonist. J Card Fail 8:43–47. doi:10.1054/jcaf.2002.32030
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470. doi:10.2337/diacare.22.9.1462
Gomez-Alamillo C, Juncos LA, Cases A, Haas JA, Romero JC (2003) Interactions between vasoconstrictors and vasodilators in regulating hemodynamics of distinct vascular beds. Hypertension 42:831–836. doi:10.1161/01.HYP.0000088854.04562.DA
Massart PE, Hodeige DG, Van Mechelen H, Charlier AA, Ketelslegers JM, Heyndrickx GR, Donckier JE (1998) Angiotensin II and endothelin-1 receptor antagonists have cumulative hypotensive effects in canine Page hypertension. J Hypertens 16:835–841. doi:10.1097/00004872-199816060-00015
Pollock DM, Derebail VK, Yamamoto T, Pollock JS (2000) Combined effects of AT(1) and ET(A) receptor antagonists, candesartan, and A-127722 in DOCA-salt hypertensive rats. Gen Pharmacol 34:337–342. doi:10.1016/S0306-3623(00)00079-3
Ikeda T, Ohta H, Okada M, Kawai N, Nakao R, Siegl PK, Kobayashi T, Miyauchi T, Nishikibe M (2000) Antihypertensive effects of a mixed endothelin-A- and -B-receptor antagonist, J-104132, were augmented in the presence of an AT1 -receptor antagonist, MK-954. J Cardiovasc Pharmacol 36:S337–S341
Bohlender J, Gerbaulet S, Kramer J, Gross M, Kirchengast M, Dietz R (2000) Synergistic effects of AT(1) and ET(A) receptor blockade in a transgenic, angiotensin II-dependent, rat model. Hypertension 35:992–997
d’Uscio LV, Moreau P, Shaw S, Takase H, Barton M, Luscher TF (1997) Effects of chronic ETA-receptor blockade in angiotensin II-induced hypertension. Hypertension 29:435–441
Herizi A, Jover B, Bouriquet N, Mimran A (1998) Prevention of the cardiovascular and renal effects of angiotensin II by endothelin blockade. Hypertension 31:10–14
Mortensen LH, Fink GD (1992) Captopril prevents chronic hypertension produced by infusion of endothelin-1 in rats. Hypertension 19:676–680
Jiang J, Tran L, Vasudevan H, Xia Z, Yuen VG, McNeill JH (2007) Endothelin-1 blockade prevents COX2 induction and TXA2 production in the fructose hypertensive rat. Can J Physiol Pharmacol 85:422–429. doi:10.1139/Y06-088
Lariviere R, Moreau C, Rodrigue ME, Lebel M (2004) Thromboxane blockade reduces blood pressure and progression of renal failure independent of endothelin-1 in uremic rats. Prostaglandins Leukot Essent Fatty Acids 71:103–109. doi:10.1016/j.plefa.2003.12.021
Pollock DM (2005) Endothelin, angiotensin, and oxidative stress in hypertension. Hypertension 45:477–480. doi:10.1161/01.HYP.0000158262.11935.d0
Callera GE, Touyz RM, Teixeira SA, Muscara MN, Carvalho MH, Fortes ZB, Nigro D, Schiffrin EL, Tostes RC (2003) ETA receptor blockade decreases vascular superoxide generation in DOCA-salt hypertension. Hypertension 42:811–817. doi:10.1161/01.HYP.0000088363.65943.6C
Callera GE, Tostes RC, Yogi A, Montezano AC, Touyz RM (2006) Endothelin-1-induced oxidative stress in DOCA-salt hypertension involves NADPH-oxidase-independent mechanisms. Clin Sci (Lond) 110:243–253. doi:10.1042/CS20050307
Delbosc S, Paizanis E, Magous R, Araiz C, Dimo T, Cristol JP, Cros G, Azay J (2005) Involvement of oxidative stress and NADPH oxidase activation in the development of cardiovascular complications in a model of insulin resistance, the fructose-fed rat. Atherosclerosis 179:43–49. doi:10.1016/j.atherosclerosis.2004.10.018
Si X, Webb RC, Richey JM (1999) Bezafibrate, an anti-hypertriglyceridemic drug, attenuates vascular hyperresponsiveness and elevated blood pressure in fructose-induced hypertensive rats. Can J Physiol Pharmacol 77:755–762. doi:10.1139/cjpp-77-10-755
Navarro-Cid J, Maeso R, Perez-Vizcaino F, Cachofeiro V, Ruilope LM, Tamargo J, Lahera V (1995) Effects of losartan on blood pressure, metabolic alterations, and vascular reactivity in the fructose-induced hypertensive rat. Hypertension 26:1074–1078
Chen S, Noguchi Y, Izumida T, Tatebe J, Katayama S (1996) A comparison of the hypotensive and hypoglycaemic actions of an angiotensin converting enzyme inhibitor, an AT1a antagonist and troglitazone. J Hypertens 14:1325–1330. doi:10.1097/00004872-199611000-00011
Galipeau D, Verma S, McNeill JH (2002) Female rats are protected against fructose-induced changes in metabolism and blood pressure. Am J Physiol Heart Circ Physiol 283:H2478–H2484
Fujioka Y, Masai M, Tsuboi S, Okumura T, Morimoto S, Tsujino T, Ohyanagi M, Iwasaki T (2003) Troglitazone reduces activity of the Na+/H+ exchanger in fructose-fed borderline hypertensive rats. Hypertens Res 26:111–116. doi:10.1291/hypres.26.111
Barton M, Carmona R, Ortmann J, Krieger JE, Traupe T (2003) Obesity-associated activation of angiotensin and endothelin in the cardiovascular system. Int J Biochem Cell Biol 35:826–837. doi:10.1016/S1357-2725(02)00307-2
Barton M, Carmona R, Krieger JE, Goettsch W, Morawietz H, d’Uscio LV, Lattmann T, Luscher TF, Shaw S (2000) Endothelin regulates angiotensin-converting enzyme in the mouse kidney. J Cardiovasc Pharmacol 36:S244–S247
Nussdorfer GG, Rossi GP, Belloni AS (1997) The role of endothelins in the paracrine control of the secretion and growth of the adrenal cortex. Int Rev Cytol 171:267–308. doi:10.1016/S0074-7696(08)62590-5
Sung CP, Arleth AJ, Storer BL, Ohlstein EH (1994) Angiotensin type 1 receptors mediate smooth muscle proliferation and endothelin biosynthesis in rat vascular smooth muscle. J Pharmacol Exp Ther 271:429–437
Emori T, Hirata Y, Ohta K, Shichiri M, Marumo F (1989) Secretory mechanism of immunoreactive endothelin in cultured bovine endothelial cells. Biochem Biophys Res Commun 160:93–100. doi:10.1016/0006-291X(89)91625-2
Acknowledgements
The authors thank Drs. G Kargacin, U Kumar, and L Marzban for consultation in the immunohistochemistry and Dr. CB Verchere for use of the microscope. Thanks to Drs. M Clozel and M Iglarz from Actelion Pharmaceuticals Ltd. and Dr. R Schwartz from Merck Research Laboratories for the generous gift of bosentan and L-158,809, respectively. The technical assistance of Dr. L Yao, P Rajput, K Potter, and VG Yuen is gratefully acknowledged. This project was supported by the Heart and Stroke Foundation of British Columbia and Yukon. LTT was a recipient of a Graduate Research Scholarship in Pharmacy from the Health Research Foundation of Canada’s Research-Based Pharmaceutical Companies and the Canadian Institute for Health Research and a Pacific Century Graduate Scholarship from the University of British Columbia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tran, L.T., MacLeod, K.M. & McNeill, J.H. Endothelin-1 modulates angiotensin II in the development of hypertension in fructose-fed rats. Mol Cell Biochem 325, 89–97 (2009). https://doi.org/10.1007/s11010-008-0023-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-008-0023-z