Abstract
The aim of the study was to find out whether administration of selenium (Se) will protect the immature heart against ischemia/reperfusion.
The control pregnant rats were fed laboratory diet (0.237 mg Se/kg diet); experimental rats received 2 ppm Na2SeO3 in the drinking water from the first day of pregnancy until day 10 post partum. The concentration of Se in the serum and heart tissue was determined by activation analysis, the serum concentration of NO by chemiluminescence, cardiac concentration of lipofuscin-like pigment by fluorescence analysis. The 10 day-old hearts were perfused (Langendorff); recovery of developed force (DF) was measured after 40 min of global ischemia. In acute experiments, 10 day-old hearts were perfused with selenium (75 nmol/l) before or after global ischemia. Sensitivity to isoproterenol (ISO, pD50) was assessed as a response of DF to increasing cumulative dose.
Se supplementation elevated serum concentration of Se by 16%. Se increased ischemic tolerance (recovery of DF, 32.28 ± 2.37 vs. 41.82 ± 2.91%, P < 0.05). Similar results were obtained after acute administration of Se during post-ischemic reperfusion (32.28 ± 2.37 vs. 49.73 ± 4.40%, P < 0.01). The pre-ischemic treatment, however, attenuated the recovery (23.08 ± 3.04 vs. 32.28 ± 2.37%, P < 0.05). Moreover, Se supplementation increased the sensitivity to the inotropic effect of ISO, decreased cardiac concentration of lipofuscin-like pigment and serum concentration of NO.
Our results suggest that Se protects the immature heart against ischemia/reperfusion injury. It seems therefore, that ROS may affect the function of the neonatal heart, similarly as in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The immature mammalian heart is more resistant to oxygen deprivation than that of the adult, but the mechanisms of this difference have not yet been satisfactorily clarified. As the mammalian fetus lives at an oxygen partial pressure corresponding to the altitude of 8000 m, newborn animals exhibit a number of physiological reactions similar to adaptive mechanisms known from hypoxia-tolerant animals, e.g., lower energy demand, greater anaerobic glycolytic capacity, changes in the ATP catabolic pathways, calcium handling, and sensitivity to oxygen free radicals [for rev. see 1]. Neonatal tolerance to oxygen deprivation seems to be primarily based on the ability to maintain tissue aerobiosis as long as possible [2].
The neonatal period seems to be critical also for the development of possibilities of cardiac protection against oxygen deprivation. In this regard, the two most potent protective mechanisms have been described: long-lasting adaptation to chronic hypoxia [3, 4], and short-lasting adaptation, called "ischemic preconditioning” [5]. We have shown previously that both protective phenomena are absent in rats at birth and that the enhanced post-ischemic recovery of the contractile function only develops during the second postnatal week [6, 7]. It seems, therefore, that decreasing tolerance to ischemia during early postnatal life is counteracted by the development of endogenous protection [7]. The protective pathways may differ during ontogenetic development, particularly in neonates; mitochondrial KATP channels and NO seem to be involved in the protective mechanism of adaptation to chronic hypoxia but not in the mechanism of ischemic preconditioning in this developmental period [7].
Tolerance to ischemic injury is not the only factor governing the recovery of the myocardium following an ischemic insult. One area yet to be explored relates to the possible ontogenetic differences in the consequences of ischemia/reperfusion injury. Severe myocardial ischemia leads to a decrease in the activity of antioxidant enzymes such that the burst of oxygen radical species suddenly produced upon reperfusion of ischemic tissue can have detrimental effects. On this basis it has been suggested that any intervention able to maintain or ideally to increase the activity of antioxidant enzymes could limit the alterations concomitant with reperfusion of ischemic myocardium [8]. Oxyradicals are generated from different sources: intracellular, mainly as a side product of restored mitochondrial metabolism and extracellular, partly coming with oxygenated blood and partly from degranulation of the inflammatory cells (e.g., neutrophils and macrophages) [9]. It has been suggested that the extent of free radical production on reperfusion may be related to the degree of injury sustained during the preceding ischemic insult [10]. Southworth et al. [11] have shown that mature guinea-pig hearts produced more reactive oxygen species than immature heart on reperfusion; they have concluded that the immature heart may be at less risk from the free radical component of ischemia/reperfusion injury than the adult myocardium. In this connection the question arises whether elevated level of antioxidants might increase tolerance to ischemia in the immature heart despite the fact that the amount of oxygen radicals is relatively low.
For this purpose we have selected selenium as an essential micronutrient with antioxidant function. It is incorporated into proteins that protect against oxidative stress [12]. The family of selenoproteins includes glutathione peroxidases, i.e., redox enzymes that take the advantage of the chemical properties of selenium to remove free radicals by reduced glutathione and thus to form oxidized glutathione [13]. In this connection it is necessary to mention that Se supplementation had a protective effect on ischemia/reperfusion injury in adult experimental animal species: it improved the recovery of cardiac function [14, 15], decreased ultrastructural changes [16], increased the expression of glutathione related enzymes [17], and partially affected the antioxidant capacity of the tissues together with an effect on gene transcription level [18]. In addition, Se supplementation prevented the hypoxia/reoxygenation injury of the isolated neonatal cardiomyocytes [19, 20]. Moreover, it has been found that selenium causes an NO-related increase of inotropic response of adult cardiac muscle to the beta-adrenergic stimulation by isoproterenol [21].
The aim of the present study was, therefore, to find out whether Se supplementation may improve post-ischemic recovery of the cardiac contractile function and inotropic responsiveness to beta-adrenergic catecholamines in 10 day-old neonatal rats, i.e., at the time when endogenous protective mechanisms are already – at least partially – developed; the selenium metabolism at this developmental period was studied previously [22].
Methods
The study was conducted in accordance with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH publication No. 85–23, revised 1996).
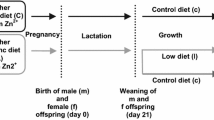
Animal model
A total of eight pregnant female Wistar rats were used throughout the experiments. They had free access to water and standard laboratory diet (ST 1 Bergman, 237 μg Se/kg diet); the food and water intake was measured daily. Starting from day 1 after conception to day 10 post partum the experimental group of pregnant rats (Se, n = 4,) was supplemented by 2 ppm of selenium (Na2SeO3, Merck) in drinking water, the control group (C, n = 4,) remained without treatment. The degree of Se supplementation was chosen in order to avoid extreme values, which might be toxic [22–24]. The offspring (a total of 104 neonates) were investigated on day 10 of postnatal life. All animals were weighed and killed by decapitation. Serum was collected for determination of Se and of the sum of NO and its oxidation products (NOx). Each experimental group of neonates was composed of at least three different nests.
Assessment of heart function
After killing the animals by cervical dislocation, the chest was quickly opened and a stainless steel cannula (with an external diameter of 0.80 mm) was inserted into the aorta. The heart was rapidly excised, the atria were removed and the ventricles were perfused in the Langendorff mode under constant pressure, corresponding to the mean arterial blood pressure for the given developmental stage [25, 26], i.e., 73 cm H2O. The hearts were perfused with a Krebs–Henseleit solution containing (mmol/l): NaCl 118.0; KCl 4.7; CaCl2 1.25; MgSO4 1.2; NaHCO3 25.0; KH2PO4 1.2; glucose 7.0 and mannitol 1.1. The solution was saturated by a mixture of 95% O2 and 5% CO2 (pH 7.4) and temperature was maintained at 37°C. The hearts were electrically stimulated at a rate of 220 beats/min using silver electrodes attached to the base of the heart. The stimulation was performed with pulses of alternating polarity, 1 ms duration, and voltage set at 50% above the threshold level. The resting force was gradually increased by means of a micromanipulator to the level at which the developed force (DF) was approximately 80% of the maximum force reached at optimum preload. The contractile function of these isolated hearts was measured using an isometric force transducer connected by a glass fiber, two-arm titanium lever and silk suture (0.7 metric) to the apex of the heart. DF (g) was evaluated automatically from the force signal using an on-line computer [6, 7, 27].
Determination of cardiac tolerance to ischemia
After a period of stabilization, baseline values of DF were recorded. The hearts of offspring from Se mothers (Se, n = 8) were then perfused for additional 10 min with Krebs–Henseleit solution and then exposed to 40 min of sustained global ischemia followed by reperfusion up to maximum recovery of DF (the last value of DF before its decay). The hearts of neonates from C mothers were divided into three groups: the hearts in the first group (n = 8) were perfused as the Se hearts; the second group (n = 8) was after period of stabilization perfused for additional 10 min with Krebs–Henseleit solution supplemented with selenium (Na2SeO3) in a final concentration of 75 nmol · l−1. This pre-ischemic perfusion was followed by the sustained global ischemia of 40 min and reperfusion with the Krebs–Henseleit solution (without Se) up to maximum recovery. The hearts in the last group (n = 8) were perfused similarly as in the first group but they were reperfused with Krebs–Henseleit solution with selenite (Na2SeO3) in a final concentration of 75 nmol · l−1 [20] again up to maximum recovery (post-ischemic reperfusion). In all groups of hearts, the DF was recorded after stabilization, before ischemia and in 3 min intervals during reperfusion up to maximum recovery. Cardiac tolerance to ischemia was determined as the maximum recovery of DF expressed as the percentage of baseline values (Fig. 1).
Estimation of inotropic responsiveness to isoproterenol
After a period of stabilization, the 10 day-old isolated hearts from Se (n = 7) and C (n = 7) litters were perfused with Krebs–Henseleit solution, supplemented cumulatively with (−)-isoproterenol (+)bitartrate salt dihydrate (Sigma-Aldrich) (ISO) over a range of concentrations 1.0 × 10−10–1.0 × 10−6 M and dose response of DF was determined. Increase in contractile force induced by each concentration of agonist was expressed as a percentage of the maximum response produced by ISO in the same sample. pD2 is defined as the negative logarithm of the molar concentration of ISO needed to produce a half maximum response.
Determination of Se in biological samples
Short-term irradiation mode of instrumental neutron activation analysis (INAA) based on analytical response of gamma line (162.0 keV) of short-lived radio nuclide 77mSe (17.5 s) was applied for selenium determination in the laboratory diet (ST 1 Bergman, n = 3), and blood serum and heart from 10 day-old offspring from Se supplemented (n = 16) and control litters (n = 12). Lyophilized samples and elemental standards were wrapped and sealed in a polyethylene foil. The activation of samples and elemental standards was carried out in the core of the experimental light water nuclear reactor LWR-15 (Nuclear Physics Institute, Řež near Prague) using the pneumatic irradiation facility (Nuclear Research Institute, Acad. Sci. of the Czech Republic) at the working regime: irradiation in a neutron flux 8 × 1013 cm−2/s for 10 s, decay time 20 s, and accumulation of gamma spectrum for 30 s. Computerized gamma-ray spectrometry equipped with an HPGe detector (FWHM 1.8 keV, relative efficiency 27%) was applied for spectrometric measurement of induced activity of 77mSe. The concentration of Se was determined using the comparator mode. The standards of Se were prepared from pure stoichiometric compounds (Na2SeO3, pro analysi, LACHEMA and/or elemental Se) and Merck Selenium Standard Solution. Accuracy of described procedure was assured by means of Certified Reference Material, A-13 (freeze the dried animal serum) prepared by International Atomic Energy Agency; the certified value of which is 0.24 ± 0.08 mg Se/kg and the value obtained by described procedure was 0.23 ± 0.02 mg/kg (n = 2) for samples of >200 mg weight.
Determination of NOx in the blood serum
NO production was quantified by measuring the sum of NO and its oxidation products (NOx) in blood serum (C n = 8, Se n = 8). NOx in the sample (0.1 ml) was first converted to NO by acidic (1 M HCl) reduction by vanadium (0.1 M VCl3) at 90°C [28, 29]. NO was then stripped from the sample by a steady flow of helium into a chemiluminescence NO analyzer (CLD 77 AM, Eco Physics, Dürnten, Switzerland) for detection. Sodium nitrate was used for calibration.
Determination of lipofuscin-like pigment (marker of oxidative stress) in the heart
A total of 50 mg pre-weighed, minced, frozen heart was added to 4 ml of chloroform-methanol mixture (2:1, v/v) and extracted for 1 h on a motor-driven shaker. After extraction, 1 ml of distilled water was added, mixed, and the mixture was centrifuged (400 g, 10 min). After centrifugation, the lower chloroform phase was separated and used for measurements. Three-dimensional fluorescence spectra were measured on the spectrofluorometer Aminco Bowman series 2 (ChromSpec company, Prague). The excitation spectra were measured in the range of 250–400 nm for emission wavelengths adjusted between 350 and 500 nm. The quantitative estimation of LFP was based on the excitation and emission maxima found in 3D spectral arrays. Fluorophores with fluorescence characteristics 355/440 nm (excitation/emission) were chosen. The fluorometer was calibrated with the standard No. 5 of the instrument manufacturer and the LFP concentration was expressed in relative fluorescence units (rfu) per mg of tissue net weight. To study changes in the composition of LFP, synchronous fluorescence spectra in the range of 300–500 nm with constant difference between excitation and emission of 25 or 50 nm were used [30, 31].
Statistical analysis
The results are expressed as means ± SEM. Each observation was obtained from at least seven heart preparations in each group. Differences in the recovery of contractile function among the groups were evaluated using two-, and one-way analysis of variance. For preliminary analysis, three-way analysis of variance was used. For pair wise mean comparisons the Student-Newman–Keuls multiple range test was applied. All the used programs belong to BMDP Statistical Software, University of California. Differences were considered as statistically significant when P < 0.05.
Results
General effects
The total food and water intake was comparable in both groups of pregnant mothers. The control group received a total of 0.220 mg Se/rat/ (diet only), whereas Se-supplemented group 0.594 mg Se/rat/ (0.243 in the diet, 0.351 in the drinking water), i.e., 2.7 times more. Se supplementation did not affect the growth of 10 day-old offspring: body and heart weight were not different from the control group (Table 1). The concentration of Se in the serum was in Se fed sucklings significantly increased; on the other hand, the concentration in the heart tissue remained unchanged (Fig. 2). In addition, the serum concentration of NOx in Se fed group was significantly decreased (Fig. 3).
Effect of Se perfusion on cardiac tolerance to ischemia
Acute addition of selenite to the perfusion medium during the pre-ischemic period had no effect on the baseline values of DF (percentage of baseline value: C 95.0 ± 1.7 and Se 103.0 ± 4.2), but significantly decreased the post-ischemic recovery of this parameter (Figs. 4 and 5). On the other hand, the addition of Se during reperfusion significantly improved the recovery of DF (Figs. 4 and 5).
Effect of acute addition of Se into Krebs–Henseleit solution on the recovery of developed force (DF) after global ischemia (expressed as a percentage of baseline values) in 10 day-old rats; C, controls (n = 8); Se pre-isch, pre-ischemic perfusion with selenium (n = 8); Se post-isch, post-ischemic perfusion with Se (n = 8); means ± SEM, *P < 0.05
Effect of acute addition of Se into Krebs–Henseleit solution on the time-course of recovery of developed force (DF) after global ischemia (expressed as a percentage of baseline values) in 10 day-old rats; controls (n = 8, full circles), pre-ischemic perfusion with selenium (n = 8, empty squares) and post-ischemic perfusion with Se (n = 8, full squares); means ± SEM, *P < 0.05
Effect of Se supplementation on cardiac tolerance to ischemia
Se supplementation (Se group) had no effect on baseline values of DF (Table 1); however, cardiac tolerance to global ischemia, as judged from the recovery of contractile function, was significantly increased (Fig. 6). Moreover, Se supplementation increased the sensitivity of the isolated perfused immature rat heart to the positive inotropic effect of isoproterenol (Fig. 7) and decrease the significantly concentration of lipofuscin-like pigment in the hearts of the 10 day-old rats (Fig. 8).
Discussion
Our results show that Se supplementation as well as acute administration of selenite during reperfusion significantly improved post-ischemic recovery of the cardiac contractile function in 10 day-old neonatal rats. On the other hand, acute pre-ischemic perfusion with selenite significantly impaired the recovery of the contractile function. Surprisingly, the protective effect was attained in spite of the fact that the cardiac concentration of selenium was not significantly increased in Se-supplemented rats, similarly as in the study of Pucheu et al. [16] and Huang et al. [32].
Se supplementation significantly increased selenium concentration in the blood serum of 10 day-old offspring, indicating placental and milk selenium transfer [33, 34]. Selenium supplementation did not significantly modify the basic functional characteristics of isolated perfused normoxic neonatal rat heart. This suggests that any difference in the post-ischemic recovery of cardiac function might be related to differences in myocardial susceptibility to ischemia/reperfusion according to trace element status.
Our results are concordant with those obtained in various studies demonstrating the protective effect of selenium supplementation during ischemia/reperfusion in the adult isolated perfused heart [14–18]. With the exception of Turan et al. [18], all studies were based on chronic supplementation of selenium in the diet. Only Turan et al. [18] observed a protective effect of selenium after acute addition of selenium into the perfusion medium, but the trace element was present during pre- as well as post-ischemic perfusion. On the other hand, we were able to distinguish between the effect of pre- and post-ischemic perfusion with selenium; protective was only the post-ischemic one. The explanation may be only hypothetical; the presence of the substance with an antioxidant properties during pre-ischemic perfusion may probably limit the number of oxygen radicals, that are essential for endogenous protection [35].
The protective effect of selenium is obviously the result of its antioxidant role. It is believed to be related to its ability to form covalent links with intracellular proteins and reduced glutathione. Pucheu et al. [16] have shown that Se supplementation significantly increased the activity of antioxidant enzymes, particularly glutathione peroxidase. This enzyme appears to play a key role in the degradation of oxygen radicals in the cytosol of cardiac myocytes, because myocytes do not have peroxisomes that contain catalase. The attenuation of glutathione peroxidase activity and scavenging effect of selenoproteins could account for the increase in oxygen radicals—elicited myocardial cell damage [36]. According to Venardos et al. [15, 17], selenium lowered the levels of protein carbonyls as well as lipid peroxides and significantly up-regulated the cardiac mRNA expression of thioredoxin and glutathione related enzymes. Moreover, Turan et al. [18] have suggested that selenium protects the heart against ischemia/reperfusion injury due to its action on the redox state and deactivation of nuclear factor (NF-κB). We have observed that Se supplementation reduced significantly the concentration of the lipofuscin-like pigment which represents the final oxidative product. It can be, therefore, concluded that Se supplementation may provide an effective method for reducing oxidative damage induced by ischemia/reperfusion not only in the adult but also in the immature heart.
The protective effect of selenite was demonstrated despite the fact that the immature myocardium produces less oxygen radicals over a range of ischemic duration than the adult heart does; however these differences had no impact on the recovery of coronary flow or contractile function in the adult and immature guinea-pig heart [11]. It is evident that the immature heart has a less developed antioxidant defense than the mature one [37]; hence, the balance between ROS and antioxidants may be similar in both with no developmental difference in oxidative stress. Nevertheless, ROS production is only one of a number of factors that might play a role in mediating developmental differences in post-ischemic recovery of the contractile function.
We observed that chronic selenium supplementation significantly increased the sensitivity of the isolated perfused immature heart to the positive inotropic effect of the beta-mimetic catecholamine, isoproterenol. A similar effect was described in the adult rat myocardium, the dose used was, however, in the range of toxic effects [38]. On the other hand, Gomez et al. [21] have observed that chronic selenium deficiency has a completely opposite effect, which correlated with the increased expression and activity of NOS and increased nitrite/nitrate levels in the heart. This would be in a good agreement with our finding of significantly decreased plasma concentration of NO in selenium-supplemented animals.
The increased inotropic response to catechoalmine stimulation observed in this study can be likely explained by a decreased NO concentration in selenium supplemented animals and the known effects of NO on myocardial function [39]. NO stimulates myocardial soluble guanylate cyclase to produce cGMP, which affects two major target proteins. A small increase in cGMP levels predominantly inhibits phosphodiesterase III, whereas high cGMP levels activate cGMP-dependent protein kinase. Accordingly, low (submicromolar) NO concentrations improve myocardial contraction, whereas high (submilimolar) NO concentrations decrease contractility [21]. Another possibility to explain the effect of NO on catecholamine-induced inotropic response could be a direct interaction between NO and catecholamines. However, there is no conclusive evidence that this process plays any role in vivo [40].
The mechanism by which selenium influences iNOS cardiac expression is, unfortunately, unknown. In this connection it is possible to mention the results of Kim et al. [41]; they have shown that lipopolysacharide-activated human T-cells with relatively high concentrations of selenite inhibited NF-κB binding and decreased NO production. Similarly, Turan et al. [18] observed that total NF-κB in the cardiac muscle was reduced by selenium. They suppose that selenium deficiency or excess affects the signal transduction pathway of the beta adrenoreceptors, protein kinase A and calcium channels present in the cardiac tissue.
In conclusion, selenium protects the immature heart against ischemia/reperfusion injury, both after supplementation or acute perfusion after ischemia, most likely by its antioxidative action. The pre-ischemic perfusion with Se had, however, the adverse effect. This suggests that ROS are produced in the immature heart; their increase or decrease may contribute to impairing or improving the function of the neonatal heart, similarly as in adults. The increased sensitivity to the inotropic effect of ISO in the Se-supplemented rats points to a possible influence of Se on the function of beta-adrenoceptors.
Abbreviations
- Se:
-
Selenium
- ROS:
-
Radical oxygen species
- I/R:
-
Ischemia reperfusion
- DF:
-
Developed force
- ISO:
-
Isoproterenol
- NF-κB:
-
Nuclear factor-κB
- cGMP:
-
Cyclic guanosine monophosphate
- iNOS:
-
Inducible nitric oxide synthase
- LFP:
-
Lipofuscin-like pigment
- rfu:
-
Relative fluorescence unit
References
Ostadal B, Ostadalova I, Dhalla NS (1999) Development of cardiac sensitivity to oxygen deficiency: comparative and ontogenetic aspects. Physiol Rev 79:635–659
Singer D (1999) Neonatal tolerance to hypoxia: a comparative-physiological approach. Comp Biochem Physiol A Mol Integr Physiol 123:221–234
Hurtado A (1960) Some clinical aspects of life at high altitudes. Ann Intern Med 53:247–258
Poupa O, Krofta K, Prochazka J, Turek J (1966) Acclimatization to simulated high altitude and acute cardiac necrosis. Fed Proc 25:1243–1246
Murry CE, Jennings RB, Reimer KA (1986) Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 74:1124–1136
Ostadalova I, Ostadal B, Kolar F, Parratt JR (1998) Tolerance to ischemia and ischemic preconditioning in neonatal rat heart. J Mol Cell Cardiol 30:857–865
Ostadalova I, Ostadal B, Jarkovska D, Kolar F (2002) Ischemic preconditioning in chronically hypoxic neonatal rat heart. Pediatr Res 52:561–567
Bolli R (1998) Causative role of oxyradicals in myocardial stunning: a proven hypothesis. A brief review of the evidence demonstrating a major role of reactive oxygen species in several forms of postischemic dysfunction. Basic Res Cardiol 93:156–162
Dhalla NS, Elmoselhi AB, Hata T, Makino N (2000) Status of myocardial antioxidants in ischemia-reperfusion injury. Cardiovasc Res 47:446–456
Henry TD, Archer SL, Nelson D (1993) Postischemic oxygen radical production varies with duration of ischemia. Am J Physiol 264:H1478–H1484
Southworth R, Shattock MJ, Hearse DJ, Kelly FJ (1998) Developmental differences in superoxide production in isolated quinea-pig hearts during reperfusion. J Mol Cell cardiol 30:1391–1399
Sunde RA (1994) Intracellular glutathione peroxidases-structure, regulation, and function. In: Burk RF (ed) Selenium in biology and human health. Springer-Verlag, New York, pp. 45–78
Burk RF, Hill KE, Motley AK (2003) Selenoprotein metabolism and function: evidence for more than one function for selenoprotein. J Nutr 133(5Suppl 1):1517S–15120S
Poltronieri R, Cevese A, Sbarbati A (1992) Protective effect of selenium in cardiac ischemia and reperfusion. Cardioscience 3:155–160
Venardos K, Harrison G, Headrick J, Perkins A (2004) Selenium supplementation and ischemia-reperfusion injury in rats. Redox Rep 9:317–320
Pucheu S, Coudray C, Tresallet N, Favier A, de Leiris J (1995) Effect of dietary antioxidant trace element supply on cardiac tolerance to ischemia-reperfusion in the rat. J Mol Cell Cardiol 27:2303–2314
Venardos K, Ashton K, Headrick J, Perkins A (2005) Effects of dietary selenium on post-ischemic expression of antioxidant mRNA. Mol Cell Biochem 270:131–138
Turan B, Saini HK, Zhang M, Prajapati D, Elimban V, Dhalla NS (2005) Selenium improves cardiac function by attenuating the activation of NF-kappaB due to ischemia-reperfusion injury. Antioxid Redox Signal 7:1388–1397
Hollander JM, Lin KM, Scott BT, Dillmann WH (2003) Overexpression of PHGPx and HSP60/10 protects ischemia/reoxygenation injury. Free Radic Biol Med 35:742–751
Bordoni A, Biagi PL, Angeloni C, Leoncini E, Danesi F, Hrelia S (2005) Susceptibility to hypoxia/reoxygenation of aged rat cardiomyocytes and its modulation by selenium supplemenmtation. J Agric Food Chem 53:490–494
Gomez RM, Levander OA, Sterin-Borda L (2003) Reduced inotropic heart response in selenium-deficient mice relates with inducible nitric oxide synthase. Am J Physiol Heart Circ Physiol 284:H442–H448
Ostadalova I, Babicky A, Kopoldova J (1982) Ontogenetic changes in selenite metabolism in rats. Arch Toxicol 49:247–252
Ostadalova I, Babicky A, Obenberger J (1978) Cataract induced by administration of a single dose of sodium selenite to sucklings rats. Experientia 34:222
Spallholz JE (1997) Free radical generation by selenium compounds and their prooxidant toxicity. Biomed Environ Sci 10:260–270
Litchfield JB (1958) Blood pressure in infant rats. Physiol Zool 31:1–6
Zicha J, Kunes J, Jelinek J (1986) Experimental hypertension in young and adult animals. Hypertension 8:1096–1104
Ostadalova I, Kolar F, Ostadal B, Rohlicek V, Rohlicek J, Prochazka J (1993) Early postnatal development of contractile performance and responsiveness to Ca2+, verapamil and ryanodine in the isolated rat heart. J Mol Cell Cardiol 25:733–740
Hampl V, Walters CL, Archer S (1996) Determination of nitric oxide by the chemiluminescence reaction with ozone In: Feelisch M, Stamler JS (eds). Methods in nitric oxide research, Wiley, Chichester, pp. 310–318
Michelakis ED, Archer SL (1998) The measurement of NO in biological systems using chemiluminiscence. In: Titheradge MA (ed) Nitric oxide protocols, Humana Press, Totowa, NJ, USA, pp. 111–127
Goldstein BD, McDonagh EM (1976) Spectrofluorescent detection of in vivo red cell lipid peroxidation in patients treated with diaminodiphenylsulfone, J Clin Investig 57:1302–1307
Wilhelm J, Herget J (1999) Hypoxia induces free radical damage to rat erythrocytes and spleen: analysis of the fluorescent end-products of lipid peroxidation, Inter J Biochem and Cell Biol 31:671–681
Huang Y, Bai H, Zhang Z (1999) Mechanism of selenium protecting against free radical damages during myocardial ischemia/reperfusion in rats. Zhonghua Yi Xue Za Zhi 79:852–856
Allen JC, Miller WJ (1981) Transfer of selenium from blood to milk in goats and noninterference of copper with selenium metabolism. J Dairy Sci 64:814–821
Enjalbert F, Lebreton P, Salat O, Schelcher F (1999) Effects of pre- or postpartum selenium supplementation on selenium status in beef cows and their calves. J Anim Sci 77:223–229
Shattock MJ, Mukaida M, Baghai M, Awad W, Chambers DJ, Alphonso N, Austin CB, Anderson DR (2004) KATP channels and preconditioning in the neonatal heart: are they up to the job? J Mol Cell Cardiol 37:365–366
Igarashi J, Nishida M, Hoshida S, Yamashita N, Kosaka H, Hori M, Kuzuya T, Tada M (1998) Inducible nitric oxide synthase augments injury elicited by oxidative stress in rat cardiac myocytes. Am J Physiol 274:C245–252
Das DK, Engelman RM, Flansaas D, Otani OJ (1987) Developmental profiles of protective mechanisms of heart against peroxidase injury. Basic Res Cardiol 82:36–50
Turan B, Hotomaroglu O, Kilic M, Demirel-Yilmaz E (1999) Cardiac dysfunction induced by low and high diet antioxidant levels comparing selenium and vitamin E in rats. Regul Toxicol Pharmacol 29:142–150
Kojda G, Kottenberg K (1999) Regulation of basal myocardial function by NO. Cardiovasc Res 41:514–523
Klatt P, Cacho J, Crespo MD, Herrera E, Ramos P (2000) Nitric oxide inhibits isoproterenol-stimulated adipocyte lipolysis through oxidative inactivation of the β-agonist. Biochem J 351:485–493
Kim YM, Bombeck CA, Billiar TR (1999) Nitric oxide as a bifunctional regulator of apoptosis. Circ Res 84:253–256
Acknowledgements
The authors thank Mrs. M. Peskova for technical assistance.
This work was supported by grant No. 1M0510 of the Czech Ministry of Education, Youth and Physical Education, by grant No. AV 0Z 50110509 and by grant AV 0Z 40310501.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ostadalova, I., Vobecky, M., Chvojkova, Z. et al. Selenium protects the immature rat heart against ischemia/reperfusion injury. Mol Cell Biochem 300, 259–267 (2007). https://doi.org/10.1007/s11010-006-9391-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-006-9391-4