Abstract
Introduction
Autism mandates are laws that require commercial insurers to cover certain evidence-based treatments for Autism Spectrum Disorder (ASD). The purpose of this study was to review state variability in autism insurance mandates and the benefits they cover and to discuss recommendations for research and policy to improve ASD services across states.
Methods
Data were extracted from 2001 to 2020 from all 50 states plus the District of Columbia (N = 51) from policy text. News articles and websites of ASD advocacy organizations were also reviewed to ensure inclusion of the most recent policy changes. Descriptive statistics and heatmaps were used to characterize the autism mandate landscape and visualize variability in benefit parameters across states.
Results
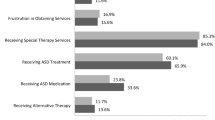
Autism mandates vary greatly in benefit parameters across US states, but there is a common set of benefits that most states have adopted. These include coverage of provider-recommended ASD services except for medical equipment, coverage up to an age limit of 18 to 21, an annual dollar limit of $36,000 with no restriction on the number of hours or visits, no lifetime cap on benefits, and requirement of BCBA® certification or its equivalent for providers of ABA.
Discussion
There is a need for continued research evaluating the impact of autism mandates and benefit parameters on access to care, service utilization, and clinical outcomes for the ASD population. Stakeholder engagement and understanding the impact of autism mandates on clinical and patient-centered outcomes may provide direction for policy advocacy and public health initiatives.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Autism mandates are laws requiring commercial insurers to cover certain evidence-based treatments for Autism Spectrum Disorder (ASD). These laws exist in all US states, but states vary in benefits covered. This paper provides a current overview of the autism mandate landscape in US states, illuminating geographic differences in coverage and opportunities for research and policy advocacy that may improve outcomes for individuals with ASD.
Introduction
Autism Spectrum Disorder (ASD) affects approximately 2.6% of children between the ages of three and 17 years in the United States (US) (Baio et al. 2018; Xu et al. 2019). Although ASD can occur alone, it commonly occurs among children with other comorbidities such as developmental, psychiatric, genetic, chromosomal, or neurologic disorders (Soke et al. 2018). Estimates from the Autism and Developmental Disabilities Monitoring Network (ADDM) suggest that 83% of children with ASD have a co-occurring developmental disorder, while 10% of children with ASD have a co-occurring psychiatric disorder (Levy et al. 2010). There is also high risk for co-morbid medical conditions for this population (Davignon et al. 2018). Given these high comorbidity rates, children with ASD often have complex medical, behavioral, and social needs, and requiring intensive and expensive care. Medical costs for children with ASD are estimated to be four to six times greater than costs for children without ASD, and intensive behavioral interventions can cost as much as $60,000 per year, per child (Buescher et al. 2014; Shimabukuro et al. 2008).
Historically, commercial insurers have excluded ASD services or provided minimal coverage, making it difficult for families to access and afford care. Insurers have argued that ASD treatment costs are too high and there is insufficient evidence for the efficacy of behavioral treatment, such as Applied Behavior Analysis (ABA) (Bouder et al. 2009; Rogers and Vismara 2008). To address this gap, some states have implemented Home- and Community-Based Services (HCBS) (i.e., services offered outside of institutional care settings) Medicaid waivers, which encourage community-based care and cover ASD services regardless of income at varying degrees across states (Graaf and Snowden 2020; Velott et al. 2016). Additionally, some states interpreted the federal Mental Health Parity and Addiction Equity Act (2008) such that they required insurers to cover ASD services on parity grounds (Bilaver and Jordan 2013). These policy efforts have had mixed success. Evidence suggests that (1) Medicaid waivers disproportionately benefitted high-income households and did not fully ameliorate unmet need for ASD services and (2) parity laws had mixed or minimal impact on service access (Bilaver and Jordan 2013; Leslie et al. 2017; Stuart et al. 2017). Current estimates suggest that approximately 30% of US children with a diagnosis of ASD still do not receive needed behavioral or medication treatment services, due to a variety of child and family factors including lack of insurance (Wilson et al. 2018; Xu et al. 2019).
In response to the continued gaps in access to care for many youth with ASD and the high public-sector burden of ASD services, all 50 US states and the District of Columbia have passed laws requiring commercial insurance plans to cover ASD services, often referred to as autism mandates (Autism Speaks, n.d.). Autism mandates are laws intended to increase access to community- and home-based service settings for youth with ASD, make ASD treatment a mandatory component of commercial health insurance benefits, and, in some states, provide for intensive early intervention in school, community, or healthcare settings. Treatment for ASD is often multifaceted, so autism mandates generally require coverage for a variety of evidence-based interventions including ABA, physical therapy, occupational therapy, speech therapy, psychological care, medications, and other clinically appropriate treatments. ABA is widely considered the primary evidence-based treatment for ASD. ABA is a scientifically validated approach to understanding behavior, how it is affected by the environment, and using those principles to improve communication, function, and behavior for youth with ASD (Molko 2018). However, many children require additional medical, mental health, and pharmacological services to address comorbidities.
There is wide variability in the kind, amount, and extent of service coverage across US states. The first autism insurance mandate in the US was passed in Indiana in 2001 and was relatively generous in benefits (Indiana Resource Center for Autism, n.d.). The mandate required commercial insurers to cover treatment prescribed by a physician for individuals with ASD or pervasive developmental disorder with no annual or lifetime dollar or visit limits and a requirement for parity with physical illness coverage. The Indiana law remains one of the more generous mandates, and while some states followed Indiana’s example and established comparable benefits, other state mandates require significantly lower levels of coverage (Autism Speaks, n.d.).
A growing body of research on autism mandates has suggested that mandating private insurance coverage of certain ASD treatment services can relieve some of the public-sector burden of ASD care and increase utilization of ASD services, albeit often shifting costs to commercial insurers and patients (Candon et al. 2018; Saloner and Barry 2017; Stein et al. 2012; Wang et al. 2013). The number of children receiving services as a result of a given autism mandate appears to increase with each year the law is in place, and mandates have been associated with both increased rates of ASD diagnosis and service utilization (Barry et al. 2017; Candon et al. 2018; Mandell et al. 2016).
Autism mandates hold promise for addressing the unmet needs of youth with ASD and increasing access to care. However, there may be additional or different benefits available to those covered by commercial insurance mandates than those covered by Medicaid waivers. Some state mandates offer exemptions or waivers for small group and individual plans, excluding children covered by those plans from benefits. States also vary considerably in the kind and generosity of benefits offered under their autism mandates. Furthermore, an increase in awareness and reporting of ASD (Hansen et al. 2015) has contributed to ASD diagnosis rates rising from 0.6% of children diagnosed in 2000 to 2.6% of children diagnosed in 2016, creating additional demand for ASD services. As a result of a combination of these and other factors, despite the implementation of insurance mandates in all 50 states, the treated prevalence of ASD is still much lower than community prevalence estimates. Many privately insured children with ASD remain undiagnosed or are treated only through publicly funded systems with unmet need for services (Mandell et al. 2016; Xu et al. 2019).
There is no consensus or evidence-based standard for the parameters of state autism mandates regarding the kind, amount, or duration or services to be covered. Autism mandates must balance the competing needs of stakeholder groups including payers, providers, and patients. Private payers are challenged by increased diagnosis rates and corresponding higher costs under the mandates (Boulder et al. 2009). To manage costs, commercial insurers may offer low reimbursement rates for ASD services, deny claims for ASD services, limit provider networks, or attempt to manage costs in other ways that reduce access to services. Likewise, providers face challenges of compliance with provider licensure requirements, and may lack knowledge of services covered by mandates and service capacity. Patients and families face high cost-sharing, difficulty findings providers, lack of information, and lack of coverage for all services (Baller et al. 2016). Future policy efforts to improve the effectiveness of mandates must consider the needs of payers, providers, and patients and seek consensus on parameters are responsive to the goals and needs of all parties. Given the lack of evidence about optimal benefit parameters for autism mandates, better understanding the range of benefits covered by autism mandates in the US is a first step towards consensus and equity in service coverage (Johnson et al. 2014). Prior studies have characterized the parameters of autism mandates in a limited number of states and reviewed policy processes preceding the mandates, but given the rapidly evolving autism mandate policy environment, a current review of the autism mandate landscape is needed (Callaghan and Sylvester 2019; Douglas et al. 2017). This study addresses that gap by describing state variability in parameters of autism insurance mandates in all 50 states—including age limits, benefit generosity, and provider requirements—and discussing recommendations for research and policy to improve ASD services across states.
Methods
Sample and Data
This descriptive study derived data from the policy text of all 50 states and the District of Columbia (N = 51) directly from state legislative websites. The data were extracted in January 2020 to include all autism mandates and changes to mandates from 2001 when the first mandate was passed in Indiana until the present. Statutes and regulations related to private insurance coverage of ASD, ASD insurance parity, state-level behavioral interventionist licensing boards, and ASD-related insurance bulletins were included. General parity laws without specific provisions for ASD and laws related to public coverage (e.g., Medicaid) of ASD services were excluded. We also reviewed government websites, insurance commissioner websites, ASD foundation and advocacy organizations, and news articles reporting on the passage of the mandates for each state to ensure that the most recent data were captured (American Speech-Language-Hearing Association, n.d.; Autism Speaks, n.d.; National Conference of State Legislatures 2017). In all cases, these non-policy sources confirmed that the most recent data were included in the analysis.
A range of mandate parameters were extracted, including effective date, age limits, dollar benefit limits, lifetime benefit limits, hour- or session-based benefit limits, provider licensure requirements, treatment prescriber requirements, services covered (ABA, pharmacy, psychiatry, psychology, therapeutic are, rehabilitative care, equipment), and employer exemptions (e.g., exemptions for small group plans or if ASD service coverage would increase insurance premiums prohibitively). We noted specific numeric parameters when applicable and used a dichotomous yes/not specified (NS) coding scheme for the presence or absence of non-numeric parameters. Parameters absent in the policy text were coded as NS, but this designation does not necessarily mean that the benefit is excluded in practice.
We measured the generosity of autism mandates using a new coding scheme based on the presence of an insurance mandate, age restrictions on benefits, spending caps on benefits, and adjustments for inflation (Callaghan and Sylvester 2019). States were given one point for the presence of an autism mandate that was restricted by both age (under 18 only) and spending caps (below the median benefit spending cap); two points for the presence of an autism mandate that were generous in terms of age limits (some adults included) or spending caps (above the median benefit spending cap); three points for the presence of a mandate that had no age limits and was over the median benefit spending cap; and four points for the presence of a mandate with no age or spending limits whatsoever. States lost an additional half-point if they had a spending limit that was not adjusted for inflation. Descriptive statistics, frequencies, and heatmaps were used to characterize the current autism mandate landscape and visualize the overall generosity of autism mandates across states. The full dataset with state-specific details about autism mandate parameters is available in Supplement 1.
Results
The overall mean state generosity score was 2.34 (range 0.5–4), with the choropleth in Fig. 1 illustrating variation across states, using a 1–4 point index of the presence of an insurance mandate, age restrictions on benefits, spending caps on benefits, and adjustments for inflation.
Generosity of US Private Autism Insurance Mandates, 2001–2020. This map shows the generosity of autism mandates in US states, based on a 1–4 point index. States were given one point for the presence of an autism mandate that was restricted by both age (under 18 only) and spending caps (below the median benefit spending cap); two points for the presence of an autism mandate that were generous in terms of age limits (some adults included) or spending caps (above the median benefit spending cap); three points for the presence of a mandate that had no age limits and was over the median benefit spending cap; and four points for the presence of a mandate with no age or spending limits whatsoever. State lost an additional half-point if they had a spending limit that was not adjusted for inflation
Age Limits
Age limits, the age at which individuals are no longer eligible for mandate benefit, may limit access to ASD care. Many states also require higher dollar benefits for younger children or exclude adults from benefits altogether, making access more difficult for families with older children or adult family members with ASD. Seventeen states do not impose an age limit on when benefits expire and provide coverage for both children and adults with ASD. The most common age limits at which individuals are no longer eligible for benefits is 18, 21, or 22 years (21 states have one of these age limits). Seven states—Maine, Tennessee, Connecticut, Ohio, Rhode Island, South Carolina, and Arizona—end benefits between the ages of 10 and 17, while one state (Mississippi) limits benefits at age eight.
Treatment Services Covered
There are a range of treatment services that may be covered by autism mandates, including ABA (ABA was sometimes defined under rehabilitative care and sometimes defined independently; see Supplement 1 for details), pharmacy care, psychiatric care, psychological care, therapeutic care (defined in all 51 mandates as speech, occupational, and physical therapy), rehabilitative care (defined in some cases as ABA and in others more generally as behavioral treatment), and medical equipment. Mandates requiring coverage of a broader range of services and specify coverage of ABA—which tends to be more expensive—may be more beneficial to families in addressing the complex care needs of a child with ASD. Almost all mandates provide coverage for ABA, with three states (South Carolina, Indiana, Wisconsin) not specifying ABA coverage in their mandates (this omission does not mean that ABA would never be covered in those states). Most mandates provide for psychiatric care, psychological care, pharmacy care, and therapeutic services (speech, physical, and occupational therapy). Eleven states specify coverage of rehabilitative care, under which ABA is classified. Some mandates specify a service list, while others provide for whatever services are deemed necessary by a physician, psychologist, or other licensed healthcare provider without a clear definition of “medical necessity.”
Benefit Limits
Many autism mandates place limits on the quantity of ASD services private insurers are required to provide in terms of maximum annual treatment costs, hours of therapy, number of therapy sessions, or lifetime maximum treatment costs. These limits can have implications for care access and clinical condition; the limits set by state autism mandates may not necessarily align with the amount of treatment recommended by healthcare providers. Only one state (Florida) imposes a lifetime benefit of $200,000. Kansas, Mississippi, Nebraska, and Oklahoma have an annual limit on number of service hours, generally 25 h per week. Ohio is the only state that sets an annual number of session limits. All other states allow for the amount of services deemed appropriate by a provider. Given the intensity and corresponding high cost of ABA, some states that have an annual benefit limit, most commonly a dollar limit of $36,000 annually (range $25,000 to $72,000 per year). Some states have annual dollar limits that vary by the child's age, with decreasing benefits as the child ages. Twenty-eight states have no annual dollar limit.
Provider Requirements
The kinds of healthcare professionals authorized to prescribe and provide treatment can affect both care access and care quality. There are differences among mandates in strict provider requirements versus allowing a broader range of health professionals to prescribe and provide treatment. Thirty-three states require ABA providers to be a Board Certified Behavior Analyst® (BCBA®) by the Behavior Analyst Certification Board or an equivalent level of provider, typically when the state has their own state-issued license or certification for behavioral analysts. A majority of states require a physician or psychologist to be the treatment prescriber, including testing, diagnosis, and subsequent treatment services (though the prescribed services may be provided by others). Some states are less restrictive and allow other health professionals including clinical social workers, therapists, nurse practitioners, licensed professional counselors, or physician assistants to prescribe and provide treatment.
Discussion
Autism insurance mandates have become widespread in the US and are now present in all 50 states and the District of Columbia. There is heterogeneity in the type, amount, and duration of benefits provided by the mandates across states. While prior studies have examined mandate parameters for a limited number of states, this study provides a current picture of the US autism mandate landscape (Callaghan and Sylvester 2019; Douglas et al. 2017; Douglas et al. 2017). A majority of mandates now require coverage for provider-recommended ASD services including ABA, services up to age 18 or 21 for both children and adults, no lifetime benefit limits, and few restrictions on hours or sessions per year. Slightly less than half of states continue to set an annual dollar limit on benefits.
Given evidence from Medicaid enrollees about positive outcomes associated with public insurance benefits, research regarding the impact of commercial insurance autism mandates on access, service utilization, and clinical outcomes continues to be needed. Understanding the impact of autism mandates on clinical and patient-centered outcomes is particularly important; a recent study of age limits in autism mandates found decreased service utilization and lower costs associated with more stringent limits, but the clinical impact of these findings remains unknown (Kennedy-Hendricks et al. 2018). The decreases in service utilization found in this study could have resulted from barriers to service, clinical improvement and a decreased need for services, or a shift of service location to schools. Research on autism mandates should include continued exploration of the clinical impact of age and other benefit parameters.
State autism insurance mandates are rapidly evolving, and there is a paucity of research on their effects. Studies examining the presence or absence of a mandate found early evidence to suggesting that mandates decrease unmet need among youth with ASD and increase service utilization (Candon et al. 2018; Saloner and Barry 2017). However, studies have not yet explored the effect of mandate parameters, and policy components often influence the effectiveness of policies. Furthermore, studies should examine to what extent the effects of mandates vary across communities, as contextual factors such as rurality, health care infrastructure, educational levels can influence the impact of policies.
Few studies to date have examined clinical or functional status outcomes and tend to rely on service utilization as a proxy for met need and subsequent improved function (Barry et al. 2017; Candon et al. 2018; Kennedy-Hendricks et al. 2018). There are challenges to using such measures to assess the clinical impact of ASD mandates because of the heterogeneity of treatment intensity recommendations and the need for tailored care. Treatment intensity can vary greatly based on the age and needs of the individual with ASD, as well as by provider type and provider beliefs about treatment (Heidgerken et al. 2005; Zwaigenbaum et al. 2015). Geographic availability of service providers may also affect service utilization rates, a contributing factor that is unrelated to clinical need (McBain et al. 2019). This limitation of existing studies of mandates should lead to caution in interpreting the clinical impact of autism mandates. Extending this work to include patient-centered functional status outcomes is a needed to improve our understanding of the effectiveness of insurance mandates.
There is also a need to study long-term service needs and outcomes for adolescents and adults with ASD because benefits rarely extend past young adulthood—and, in some cases, end in early childhood—and there are likely unmet service needs among adolescents and adults with ASD. Studies should consider long-term functional status outcomes such as living situation, participation in the community, physical health, and personal relationships as indicators of successful treatment in childhood (Molko 2018). Finally, future studies should examine state-by-state coverage of ASD services from all insurance sources including public insurance, parity laws, and private insurance mandates. Such an analysis would be useful for identifying geographic areas in need of greater access to ASD care and better accounting for the impact of private autism mandate limits, such as employer exemptions and waivers.
There are several limitations to this study that should be considered in interpreting the results. Our analysis derived data from policy text regarding private insurance autism mandates. It does not include all possible ways that ASD services are covered by insurance (e.g., Medicaid, parity laws) and it is possible that the application or interpretation of laws differs from the policy text in real-world practice. We were unable to assess actions that may be occurring within states to facilitate or impede the intended effects of the mandates and their implementation, and we do not know the extent or impact of employer exemptions and waivers from the current analysis. Replication analyses will be necessary to track changes in the autism mandate landscape. Our study has strengths as well. To our knowledge, this is the first study to characterize current autism mandates in all 50 states and the District of Columbia. We derived data from multiple sources and quantified some benefit parameters that have not previously been described (Douglas et al. 2017).
US states have an ongoing opportunity to make more informed policy choices and improve the effectiveness of their policies by learning what autism mandate parameters appear to be most effective and efficient in states that have implemented them. Currently, there is a lack of guidance for structuring autism mandates optimally so that they achieve the public health and policy goals of states. Stakeholders from payer, provider, and patient may benefit from consensus building around autism mandates and related issues, such as treatment quality standards and outcome measures across states. A more robust evidence base around autism mandates has potential to improve geographic parity across states in access to ASD services and public health outcomes for youth. In the absence of an evidence base and established standards from stakeholders and experts, payers and policymakers dictate how services are provided without the needed input of experts, clinicians, and families and without taking patient-centered outcomes into account (Molko 2018). As autism mandates continue to evolve, involving key stakeholders in policy refinement may improve the efficacy and reach of ASD mandates.
References
American Speech-Language-Hearing Association. (n. d.). State insurance mandates for autism spectrum disorder. Retrieved from https://www.asha.org/Advocacy/state/States-Specific-Autism-Mandates/.
Autism Speaks (n. d.) State insurance reform laws. Retrieved from https://www.autismspeaks.org/advocacy/insurance/faqs-state-autism-insurance-reform-laws.
Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., et al. (2018). Prevalence of Autism Spectrum Disorder among children aged 8 years – Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. Morbidity and Mortality Weekly Report,67(6), 1–23.
Baller, J. B., Barry, C. L., Shea, K., Walker, M. M., Ouellette, R., & Mandell, D. S. (2016). Assessing early implementation of state autism insurance mandates. Autism,20(7), 796–807.
Barry, C. L., Epstein, A. J., Marcus, S. C., Kennedy-Hendricks, A., Candon, M. K., Xie, M., et al. (2017). Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Affairs,36(10), 1754–1761.
Bilaver, L. A., & Jordan, N. (2013). Impact of state mental health parity laws on access to autism services. Psychiatric Services,64(10), 967–973.
Bouder, J. N., Spielman, S., & Mandell, D. S. (2009). Brief report: Quantifying the impact of autism coverage on private insurance premiums. Journal of Autism and Developmental Disorders,39(6), 953–957.
Buescher, A. V., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics,168(8), 721–728.
Callaghan, T., & Sylvester, S. (2019). Autism spectrum disorder, politics, and the generosity of insurance mandates in the United States. PLoS ONE,14(5), e0217064.
Candon, M. K., Barry, C. L., Epstein, A. J., Marcus, S. C., Kennedy-Hendricks, A., Xie, M., et al. (2018). The differential effects of insurance mandates on health care spending for children’s Autism Spectrum Disorder. Medical Care,56(3), 228–232.
Davignon, M. N., Qian, Y., Massolo, M., & Croen, L. A. (2018). Psychiatric and medical conditions in transition-aged individuals with ASD. Pediatrics,141(Supplement 4), S335–S345.
Douglas, M. D., Benevides, T. W., & Carretta, H. (2017). Analyzing state autism private insurance mandates for allied health services: A pilot study. OTJR Occupation, Participation and Health,37(4), 218–226.
Graaf, G., & Snowden, L. (2020). Medicaid waiver adoption for youth with complex behavioral health care needs: An analysis of state decision-making. Journal of Disability Policy Studies. https://doi.org/10.1177/1044207319897058.
Hansen, S. N., Schendel, D. E., & Parner, E. T. (2015). Explaining the increase in the prevalence of autism spectrum disorders: The proportion attributable to changes in reporting practices. JAMA Pediatrics,169(1), 56–62.
Heidgerken, A. D., Geffken, G., Modi, A., & Frakey, L. (2005). A survey of autism knowledge in a health care setting. Journal of Autism and Developmental Disorders,35(3), 323–330.
Indiana Resource Center for Autism (n.d.). Indiana's health insurance mandate for Autism Spectrum Disorders (ASDs) and Pervasive Developmental Disorders (PDDs). Retrieved from https://www.iidc.indiana.edu/pages/Indianas-Health-Insurance-Mandate-for-Autism-Spectrum-Disorders-and-Pervasive-Developmental-Disorders-PDDs.
Johnson, R. A., Danis, M., & Hafner-Eaton, C. (2014). US state variation in autism insurance mandates: Balancing access and fairness. Autism,18(7), 803–814.
Kennedy-Hendricks, A., Epstein, A. J., Mandell, D. S., Candon, M. K., Marcus, S. C., Xie, M., et al. (2018). Effects of state autism mandate age caps on health service use and spending among adolescents. Journal of the American Academy of Child & Adolescent Psychiatry,57(2), 125–131.
Leslie, D. L., Iskandarani, K., Dick, A. W., Mandell, D. S., Yu, H., Velott, D., et al. (2017). The effects of Medicaid home and community-based services waivers on unmet needs among children with autism spectrum disorder. Medical Care,55(1), 57.
Levy, S. E., Giarelli, E., Lee, L. C., Schieve, L. A., Kirby, R. S., Cunniff, C., et al. (2010). Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. Journal of Developmental & Behavioral Pediatrics,31(4), 267–275.
Mandell, D. S., Barry, C. L., Marcus, S. C., Xie, M., Shea, K., Mullan, K., et al. (2016). Effects of autism spectrum disorder insurance mandates on the treated prevalence of autism spectrum disorder. JAMA Pediatrics,170(9), 887–893.
McBain, R. K., Kareddy, V., Cantor, J. H., Stein, B. D., & Yu, H. (2019). Systematic Review: United States Workforce for Autism-Related Child Healthcare Services. Journal of the American Academy of Child & Adolescent Psychiatry.,59, 113–119.
Molko, R. (2018). Autism matters: Empowering investors, providers, and the autism community to advance autism services. Charleston, SC: ForbesBooks.
National Conference of State Legislatures. (2017). Autism and insurance coverage. Retrieved from https://www.ncsl.org/research/health/autism-and-insurance-coverage-state-laws.aspx.
Rogers, S. J., & Vismara, L. A. (2008). Evidence-based comprehensive treatments for early autism. Journal of Clinical Child & Adolescent Psychology,37(1), 8–38.
Saloner, B., & Barry, C. L. (2017). Changes in spending and service use after a state autism insurance mandate. Autism,23, 167–174.
Soke, G. N., Maenner, M. J., Christensen, D., Kurzius-Spencer, M., & Schieve, L. A. (2018). Prevalence of co-occurring medical and behavioral conditions/symptoms among 4- and 8-year-old children with Autism Spectrum Disorder in selected areas of the United States in 2010. Journal of Autism and Developmental Disorders,48, 1–14.
Stein, B. D., Sorbero, M. J., Goswami, U., Schuster, J., & Leslie, D. L. (2012). Impact of a private health insurance mandate on public sector autism service use in Pennsylvania. Journal of the American Academy of Child & Adolescent Psychiatry,51(8), 771–779.
Shimabukuro, T. T., Grosse, S. D., & Rice, C. (2008). Medical expenditures for children with an autism spectrum disorder in a privately insured population. Journal of Autism and Developmental Disorders,38(3), 546–552.
Stuart, E. A., McGinty, E. E., Kalb, L., Huskamp, H. A., Busch, S. H., Gibson, T. B., et al. (2017). Increased service use among children with autism spectrum disorder associated with mental health parity law. Health Affairs,36(2), 337–345.
Velott, D. L., Agbese, E., Mandell, D., Stein, B. D., Dick, A. W., Yu, H., et al. (2016). Medicaid 1915 (c) Home-and Community-Based Services waivers for children with autism spectrum disorder. Autism,20(4), 473–482.
Wang, L., Mandell, D. S., Lawer, L., Cidav, Z., & Leslie, D. L. (2013). Healthcare service use and costs for autism spectrum disorder: A comparison between Medicaid and private insurance. Journal of Autism and Developmental Disorders,43(5), 1057–1064.
Xu, G., Strathearn, L., Liu, B., O’brien, M., Kopelman, T. G., Zhu, J., et al. (2019). Prevalence and treatment patterns of autism spectrum disorder in the United States, 2016. JAMA Pediatrics,173(2), 153–159.
Zwaigenbaum, L., Bauman, M. L., Choueiri, R., Kasari, C., Carter, A., Granpeesheh, D., et al. (2015). Early intervention for children with autism spectrum disorder under 3 years of age: Recommendations for practice and research. Pediatrics,136(Supplement 1), S60–S81.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choi, K.R., Knight, E.A., Stein, B.D. et al. Autism Insurance Mandates in the US: Comparison of Mandated Commercial Insurance Benefits Across States. Matern Child Health J 24, 894–900 (2020). https://doi.org/10.1007/s10995-020-02950-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-020-02950-2