Abstract
Objective This study examined associations between pregnant women’s report of obstetric provider GWG advice, self-reported adherence to such advice, and GWG. Methods Healthy pregnant women (N = 91) who started obstetric care prior to 17 weeks of gestation completed assessments between 30 and 34 weeks of gestation. These included survey (questions on receipt of and adherence to provider GWG advice, and demographics) and anthropometric measures. GWG data were abstracted from electronic health records. Analyses included Chi square and Mann–Whitney tests, and binary and multivariate logistic regressions. Results The cohort’s median age was 28 years, 68% of women were White, 78% had a college education, 50.5% were overweight or obese before the pregnancy, and 62.6% had GWGs above the Institute of Medicine-recommended ranges. Sixty-seven percent of women reported having received GWG advice from their obstetric providers and, of those, 54.1% reported that they followed their provider’s advice. Controlling for race, education and pre-pregnancy BMI, receipt of GWG advice was marginally associated with increased odds of excessive weight gain (OR 2.52, CI 0.89–7.16). However, women that reported following the advice had lower odds of excessive GWG (OR 0.18, CI 0.03–0.91) and, on average, gained 11.3 pounds less than those who reported following the advice somewhat or not at all. Conclusions Frequency of GWG advice from obstetric providers is less than optimal. When given and followed, provider advice may reduce the risk of excessive GWG. Research to understand factors that facilitate providers GWG advice giving and women’s adherence to providers’ advice, and to develop interventions to optimize both, is needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Excessive gestational weight gain (GWG) increases risk of adverse maternal and neonatal outcomes. Few studies have examined the influence of provider advice on excessive GWG. There is a need to study the influence of provider advice on GWG in a prospective manner and using the most recent 2009-IOM recommendations. Our study revealed that provider advice was associated with higher odds of excessive weight gain but self-reported adherence to such advice was associated with lower odds. Our findings highlight the need to formulate strategies to increase provider GWG advice and adherence to it among pregnant women.
Introduction
Excessive gestational weight gain (GWG) increases risk for maternal and child obesity (Amorim et al. 2007; Linne et al. 2004; Oken et al. 2007), pregnancy and labor/delivery complications (Fortner et al. 2009; Jensen et al. 2005; Kieffer et al. 2001; Stotland et al. 2004), adverse neonatal outcomes (Heddersin et al. 2010; Jensen et al. 2005; Stotland et al. 2006), and poor quality of life (Amador et al. 2008). Despite these risks, almost one-half of women in the U.S. experience excessive GWG, with the prevalence of this problem being greater among socioeconomically disadvantaged and minority women (Deputy et al. 2015; Olson and Strawderman 2003).
The Institute of Medicine (IOM) updated body mass index (BMI) specific evidence-based recommendations for GWG ranges in 2009 (Rasmussen and Yaktine 2009). However, existing research suggests that pregnant women may receive little guidance from their obstetric providers regarding GWG (Cogswell et al. 1999; Ferrari and Siega-Riz 2013; Liu et al. 2016; McDonald et al. 2011; Stotland et al. 2005; Wrotniak et al. 2015). Given that health care providers’ advice is an important factor in the initiation of health behavior change among patients overall, including advice about weight (Bish et al. 2005; Dorsey and Songer 2011; Galuska et al. 1999; Loureiro and Nayga 2006; Thande et al. 2009; Zapka et al. 2009), understanding the association between obstetric provider advice and GWG may help inform future interventions. However, few studies have examined this association and their findings have been mixed. Four studies have reported that provider advice consistent with guidelines is associated with adequate GWG (Cogswell et al. 1999; Herring et al. 2012; Liu et al. 2016; Stotland et al. 2005), while three other studies found no association between provider advice and GWG (Ferrari and Siega-Riz 2013; Phelan et al. 2011; Wrotniak et al. 2015). Differences in criteria used for determining adequacy of GWG may explain these mixed findings as five of the seven studies assessed adequacy of GWG based on earlier (1990) guidelines (Cogswell et al. 1999; Ferrari and Siega-Riz 2013; Liu et al. 2016; Phelan et al. 2011; Stotland et al. 2005). Such guidelines did not provide an upper limit for recommended GWG for obese women, instead encouraging these women to gain at least 15 pounds, whereas the revised guidelines recommend a 20 pound maximum (Committee on Nutritional Status During Pregnancy, Institute of Medicine, Eds. Nutrition During Pregnancy: Part I: Weight Gain, Part II: Nutrient Supplements., 1990; Rasmussen and Yaktine 2009). In the absence of an upper cap for recommended GWG for obese women, studies that used the 1990 guidelines applied the recommended GWG range for overweight women (i.e., 15 to 25lbs) to obese women (Cogswell et al. 1999; Ferrari and Siega-Riz 2013; Liu et al. 2016; Phelan et al. 2011; Stotland et al. 2005). Thus, in accordance with current guidelines, those studies misclassify obese women with regards to meeting or not meeting the GWG recommendations. Furthermore, two of the seven aforementioned studies did not assess provider GWG advice prospectively but instead assessed recall of GWG advice retrospectively (i.e., post-partum) (Liu et al. 2016; Wrotniak et al. 2015), which may engender recall bias. Thus, there is a need to study the association of provider advice and adherence to GWG guidelines prospectively and using the latest (2009) IOM recommendations.
The aims of this study were to examine provider GWG advice and adherence to the advice received, in a sample of pregnant women who were participants in the Pregnancy and Post-partum Observational Dietary Study (PPODS) (MooreSimas et al. 2015). Specifically, we explored associations between provider GWG advice, adherence to the advice, and total and excessive GWG. We hypothesized that both receipt of provider advice and adherence to advice would be associated with lower total GWG and greater odds of adherence to IOM GWG guidelines.
Methods
Study Design and Participants
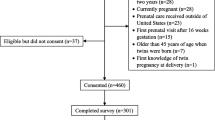
The present study uses baseline data from the PPODS study, a prospective cohort study designed to elucidate risks and protective factors for GWG and post-partum weight loss [described elsewhere; (MooreSimas et al. 2015)]. In brief, participants were enrolled from obstetric clinics at a large tertiary care hospital in central Massachusetts. Eligibility criteria included: age 18–45 years, singleton gestation, able to communicate in English, start of prenatal care prior to 17 weeks of gestation, no use of medications that affect weight, and no history of diabetes, bariatric surgery, alcohol or substance abuse or evidence of systemic disease (i.e., HIV, hepatitis, autoimmune disease) or eating disorders. Screening eligibility occurred proactively from August 2011 to November 2012 following gestational diabetes screening (n = 942). Records of 888 women without gestational diabetes were abstracted for further eligibility by full medical chart review. Of these, 443 were ineligible (i.e., substance abuse, non-English speaking, pre-natal care initiated > 17 weeks of gestation). Of the remaining 445, a total of 279 women were approached by a research assistant (the remainder that were eligible were missed due to logistics) and 110 women were interested and agreed to participate. Participants were consented in writing prior to completing study assessments. This study was approved by the Institutional Review Board of the University of Massachusetts Medical School.
Measures
Data from baseline assessments and participants’ medical charts were used. The baseline assessment was administered at 28–34 weeks of gestation (before the fetus has reached the period of higher weight gain) (American Pregnancy Association 2016).
Socio-demographics and Covariates
Demographic variables were assessed via survey questions and included age, race, ethnicity, educational attainment, and work status. Educational attainment was measured by the highest level of education achieved. Work status was dichotomized into employed (full or part-time) and not working (unemployed, homemaker and full-time student).
Gravidity was assessed by survey and categorized as being multigravida or not. Height was measured at the time of the baseline study visit and pre-pregnancy weight was abstracted from the first pre-natal visit record. Pre-pregnancy BMI was calculated as pre-pregnancy weight (kg)/height (m2), and categorized according to WHO criteria: underweight (< 18.5 kg/m2), healthy weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥ 30 kg/m2)(Rasmussen and Yaktine 2009).
Provider’s GWG Advice
Recall of provider GWG advice was assessed through a single yes/no question that asked: “Since becoming pregnant, has your doctor, nurse or midwife given you any advice on how much weight you should gain during your pregnancy?.”
Adherence to Provider GWG Advice
Adherence to provider GWG advice was assessed by a question that asked about the participant’s efforts to follow the GWG advice received: “To what extent have you followed such advice?” Response options were “not at all”, “somewhat” and “very much”. For this analysis, responses regarding adherence to advice were dichotomized as “not at all/somewhat” and “very much” because only 2 participants reported not following the advice at all.
Gestational Weight Gain (GWG)
GWG was studied as a continuous variable (in pounds). Total GWG was calculated by subtracting pre-pregnancy weight from the documented weight at the last pre-natal visit. Adherence to GWG recommendations was calculated based on pre-pregnancy BMI and in accordance to the 2009 IOM guidelines. Accordingly, recommended GWG ranges are: 28–40 lbs for women with underweight pre-pregnancy BMI, 25–35 for women with normal pre-pregnancy BMIs, 15–25 lbs for women with overweight pre-pregnancy BMIs, and 11–20 lbs for women with pre-pregnancy obesity (Rasmussen and Yaktine 2009). GWG adherence status was classified as inadequate (below recommended range), appropriate (within recommended range), or excessive (above recommended range). Since only ten participants (10.2%) had inadequate GWG, this variable was dichotomized into inadequate/adequate GWG versus excessive GWG for our analyses.
Statistical Analyses
This analysis only included participants with complete data on recollection of physician GWG advice (13 participants with missing data), covariates (9 participants with missing data), and outcome, for a total of sample of 91 individuals. Descriptive statistics include median (P25 and P75) for continuous variables and frequencies and percentages for categorical variables. The Chi square test was used for categorical variables and Mann–Whitney test for continuous variables to compare socio-demographics, obstetrics, and weight characteristics between participants that received and did not receive GWG advice from their providers. Mann–Whitney and Chi square tests were also used to contrast total GWG and adherence to IOM-guidelines by adherence to provider GWG advice status. Linear regression was performed to assess associations between (1) provider GWG advice status and total GWG, and (2) adherence to provider GWG advice and total GWG. In addition, logistic regression was used to assess associations between (1) receipt of provider GWG advice and experiencing excessive GWG, and (2) adherence to provider GWG advice and experiencing excessive GWG. Linear regression models were adjusted a-priori for variables taken from the literature namely, race, education, gestational age at last prenatal visit and pre-pregnancy BMI. Logistic regression models were adjusted for race, education and pre-pregnancy BMI. Statistical significance was set at the 0.05 level. The SPSS program version 20 was used for all analyses.
Results
Of a total sample of 110 participants, 91 had complete data on exposures, covariates, and outcome variables. The median age of the sample was 28 years. About two-thirds of the sample was of White race, and slightly over one quarter self-identified as Latina (Table 1). Three-fourths of the sample had some college education or a higher educational level, another three-fourths were employed and approximately two-thirds were multigravida. Half of the sample had a pre-pregnancy BMI in the overweight or obese range. The median gestational age at the last prenatal visit was 39 weeks and the median GWG was 34 pounds, with almost two-thirds of the participants experiencing excessive GWG (Table 2).
Approximately two-thirds of the sample received provider GWG advice (Table 1). Socio-demographic and obstetrics characteristics were similar in those that received provider GWG advice compared to those that did not. Among participants that recalled receiving GWG advice from their provider, only one-half reported adhering to such advice.
Total GWG was similar among participants that received provider GWG advice and those who did not (Table 2). However, a greater proportion of the participants that received provider GWG advice had excessive GWG compared to participants who had GWG within the IOM-recommended ranges (Table 2). In adjusted regression analyses, provider GWG advice was not significantly associated with total GWG or with excessive GWG (Table 3). Results remained similar in analyses excluding participants with inadequate weight gain (data not shown).
Total GWG was significantly different between women that reported following provider GWG advice compared to those who reported somewhat following the advice or not following it at all (Table 2), with women that reported following provider GWG advice gaining less weight. Similarly, there were significant differences in adherence to IOM-recommended GWG ranges between women who reported following provider GWG advice and those who followed it somewhat or not at all, with almost half of the participants that reported following the advice having GWG within the IOM-recommended ranges compared to only one-tenth of those who reported somewhat following the advice or not at all (Table 2). In adjusted regression analyses, women that reported following provider GWG advice gained on average 11 lbs. less than those who reported somewhat following the advice or not at all (Table 3). In addition, women who reported following provider GWG advice were 82% less likely to experience excessive GWG (Table 3). Results remained similar in analyses excluding participants with inadequate weight gain (data not shown).
Discussion
In this sample of pregnant women, receipt of provider GWG advice and adherence to such advice were less than optimal. Contrary to our first hypothesis, we failed to find a positive association between provider GWG advice and our two outcomes: total GWG and adherence to GWG guidelines. However, participant’s self-reported adherence to GWG advice did show a significant negative association with total GWG with above-guideline GWG, as hypothesized.
These findings confirm prior reports that the occurrence of GWG advice from obstetric providers is less than ideal. Our finding that two-thirds of participants received provider GWG advice is in the upper range of rates of provider advice reported in prior studies where between 36–81% of women reported receiving such advice (Cogswell et al. 1999; Ferrari and Siega-Riz 2013; Herring et al. 2012; Liu et al. 2016; Phelan et al. 2011; Stotland et al. 2005; Wrotniak et al. 2015). The variability in rates of advice may be associated with the design of the studies. Variability in reported rates of advice may also be due to differences in timing of data collection and timing of advice. The study that reported the highest rate of provider GWG advice (Liu et al. 2016) collected data in post-partum women whereas other studies (Ferrari and Siega-Riz 2013; Herring et al. 2012; Phelan et al. 2011; Stotland et al. 2005) have collected data prospectively during early or mid pregnancy. Providers may be giving GWG advice later in pregnancy (due to response to identified non-adherence) and so it may not be captured when asked during early pregnancy (Liu et al. 2016). Thus, the high rate of advice in our study may be associated with our assessment of GWG advice later in pregnancy.
The variability in rates of advice may also be associated with patient, provider, and health care system factors, not assessed as part of this study. Differences in provider advice in studies of women with varying demographic characteristics have been previously documented. For example, a study by Herring and colleagues that reported the lowest rate of provider GWG advice (36%) included a sample largely composed of African American women (83%) most of whom had an educational level of high school or less (87%) (Herring et al. 2012). In contrast, our sample was largely White with a higher educational level. At the provider and system levels, a recent study found that 55.7% of residents in Obstetrics/Gynecology and Family Medicine training programs across the U.S. (n = 660) were not aware of the 2009 IOM-guidelines for GWG, which are the foundation for GWG counseling (Moore Simas et al. 2013). A tendency by providers to adopt a “reactive” approach by waiting for the patient to bring up concerns (Duthie et al. 2013), rather than proactively addressing GWG with all women, also may limit advice. Another factor that may affect provider advice is their concern about consequences of the advice. For example, in a qualitative study providers reported that they were concerned that the advice may cause anxiety and frustration to patients if guideline-centered goals are not successfully achieved (Stotland et al. 2010). Additionally, some providers report limited provider self-efficacy about the impact of their advice on their patients’ GWG (Stotland et al. 2010). Health care system factors such as limited time of obstetric visits that may limit opportunities to discuss GWG may be another barrier to provider GWG advice as this has been an issue on weight gain counseling in primary care clinical settings (Yarnall et al. 2003). All these factors may add up to explain the suboptimal frequency of provider GWG advice and may serve as potential intervention targets to optimize provider GWG counseling.
Our findings highlight the problem of non-adherence to IOM recommendations for GWG, and are in line with evidence from previous research and surveillance systems showing that approximately half of women gain weight in excess of IOM recommended ranges (Hernandez 2012; Deputy et al. 2015). We did not find a significant association between provider GWG advice and participants’ total GWG and excessive GWG, however our study was limited because we were not able to confirm receipt of provider advice and relied on a self-reported measure. Our results are in agreement with two prior studies that reported no association between provider advice and excessive GWG (Ferrari and Siega-Riz 2013; Phelan et al. 2011; Wrotniak et al. 2015) whereas others have reported opposite results (Cogswell et al. 1999; Herring et al. 2012; Liu et al. 2016; Stotland et al. 2005). The benefits of provider GWG advice warrant further research using randomized trial designs.
Our study revealed that, among women who reported receiving GWG advice, adherence to such advice was suboptimal, with only half of the women stating that they adhered to the advice. Our study did not examine factors that may affect adherence to provider GWG advice, however other studies provide potential insights into factors that may play a role. For example, social and cultural norms including the belief that a pregnant woman needs to “eat for two” are common and well accepted by society (Kraschnewski and Chuang 2014). Such norms may lead a woman to question advice about curtailing GWG. Factors associated with the advice itself also limit its influence, such as lack of specificity of the advice. For example, one study showed that although providers reported providing nutrition counseling to their pregnant patients, women perceived that the advice offered was too general (Duthie et al. 2013). Our study did not assess these factors. Lastly, the delivery method selected for giving advice may limit adherence to it. In one study, women in the third trimester of pregnancy reported receiving advice though nutrition handouts but reported that the information in the handout was not discussed by the provider, which also could limit adherence (Duthie et al. 2013). Ultimately, numerous factors may potentially explain the low adherence rates to provider GWG advice in our study.
Our results evidence favorable outcomes for women that indicated following their provider GWG advice over women who reported somewhat following the advice or not following it at all: they had less total GWG and greater odds of adhering to the IOM-recommended GWG range. Consistent with our findings, one other study that evaluated adherence to advice and GWG reported that women who followed their provider GWG advice had lower risk of experiencing excessive GWG (RR 0.87, 95% CI 0.78–0.98) (Ferrari and Siega-Riz 2013). These results suggest that just providing GWG advice is not enough and highlight the need for design and implementation of novel strategies that facilitate recognition, recollection, relatability and adherence to provider GWG advice.
Our study has some strengths and limitations. The relatively small sample size may have limited us in identifying statistical significance for analyses with the total GWG outcome. In addition, initial exclusion criteria of the study and other sample characteristics may limit generalizability of findings to non-English speaking women, pregnant adolescents, women with history of diabetes and other systemic diseases, those who did not seek early prenatal care, and low-education/socioeconomically disadvantaged women. Lastly, our exposure measures were self-reported and thus we were not able to validate them. However, the study has important strengths. Compared to a previous study that assessed women’s recall of GWG advice at four months post-partum (Liu et al. 2016), our study reduces the possibility of recall bias by assessing GWG advice during pregnancy. Additionally, while it is important to replicate study findings in a larger sample and diverse populations of pregnant women, our findings point to potential targets of intervention in future trials.
In conclusion, this study characterized the frequency of provider GWG advice and adherence to such advice in a sample of women, and examined the association of these variables with total GWG and GWG adherence status. Although recall of provider GWG advice was not associated with adherence to GWG recommendations, adherence to advice was associated with favorable weight outcomes. Thus, there is a need to promote delivery of provider advice on GWG and to further encourage adherence to such advice to lower the risk of excessive GWG.
References
Amador, N., Juarez, J., Guizar, J., & Linares, B. (2008). Quality of life in obese pregnant women: A longitudinal study. American Journal of Obstetrics and Gynecology, 198(2), 203.e1–203.e5.
American Pregnancy Association. (2016). Fetal Development: Third Trimester. Retrieved February 5, 2018, from http://americanpregnancy.org/while-pregnant/third-trimester/.
Amorim, A., Rossner, S., Neovius, M., Lourenco, P., & Linne, Y. (2007). Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity (Silver Spring, Md.), 15(5), 1278–1286.
Bish, C., Blanck, H., Serdula, M., Marcus, M., Kohl, H., & Khan, L. (2005). Diet and physical activity behaviors among Americans trying to lose weight: 2000 behavioral risk factor surveillance system. Obesity Research, 13(3), 596–607.
Cogswell, M., Scanlom, K., Fein, S., & Schive, L. (1999). Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstet Gynecol, 94(4), 616–622.
Committee on Nutritional Status During Pregnancy, Institute of Medicine (Eds.). Nutrition during pregnancy: Part I: Weight Gain, Part II: Nutrient Supplements. (1990). Washington, D.C.: National Academy Press.
Deputy, N., Sharma, A., Kim, S., & Hinkle, S. (2015). Prevalence and characteristics associated with gestational weight gain adequacy. Obstetrics and Gynecology, 125(4), 773–781.
Dorsey, R., & Songer, T. (2011). Lifestyle behaviors and physician advice for change among overweight and obese adults with prediabetes and diabetes in the United States, 2006. Preventing Chronic Disease, 8(6), A132.
Duthie, E., Drew, E., & Flynn, K. (2013). Patient-provider communication about gestational weight gain among nulliparous women: a qualitative study of the views of obstetricians and first-time pregnant women. BMC Pregnancy Childbirth. https://doi.org/10.1186/1471-2393-13-231.
Ferrari, R., & Siega-Riz, A. (2013). Provider advice about pregnancy weight gain and adequacy of weight gain. Maternal and Child Health Journal, 17(2), 256–264.
Fortner, R., Pekow, P., Solomon, C., Markenson, G., & Chasan-Taber, L. (2009). Prepregnancy body mass index, gestational weight gain, and risk of hypertensive pregnancy among Latina women. American Journal of Obstetrics and Gynecology, 200(2), 167.e1–167.e7.
Galuska, D., Will, J., Serdula, M., & Ford, E. (1999). Are health care professionals advising obese patients to lose weight? JAMA, 282(16), 1576–1578.
Heddersin, M., Gunderson, E., & Ferrara, A. (2010). Gestational weight gain and risk of gestational diabetes mellitus. Obstetrics and Gynecology, 115(5), 597–604.
Hernandez, D. (2012). Gestational weight gain as a predictor of longitudinal body mass index transitions among socioeconomically disadvantaged women. Journal of Women’s Health, 21(10), 1082–1090.
Herring, S., Nelson, D., Davey, A., Klotz, A., Dibble, L., Oken, E., & Foster, G. (2012). Determinants of excessive gestational weight gain in urban, low-income women. Womens Health Issues, 22(5), e439–e446.
Jensen, D., Ovesen, P., Beck-Nielsen, H., Molsted-Pedersen, L., Sorensen, B., Vinter, C., & Damm, P. (2005). Gestational weight gain and pregnancy outcomes in 481 obese glucose-tolerant women. Diabetes Care, 28(9), 2118–2122.
Kieffer, E., Carman, W., Gillespie, B., Nolan, G., Worley, S., & Guzman, J. (2001). Obesity and gestational diabetes among African-American women and Latinas in Detroit: Implications for disparities in women’s health. Journal of the American Medical Women’s Association, 56(4), 181–187.
Kraschnewski, J., & Chuang, C. (2014). Eating for two”: Excessive gestational weight gain and the need to change social norms. Womens Health Issues, 24(3), e257–e259.
Linne, Y., Dye, L., Barkeling, B., & Rossner, S. (2004). Long-term weight development in women: A15-year follow-up of the effects of pregnancy. Obesity Research, 12(7), 1166–1178.
Liu, J., Whitaker, K., Yu, S., Chao, S., & Lu, M. (2016). Association of provider advice and pregnancy weight gain in a predominantly hispanic population. Womens Health Issues, 26(3), 321–328.
Loureiro, M., & Nayga, R. J. (2006). Obesity, weight loss, and physician’s advice. Social Science and Medicine, 62(10), 2458–2468.
McDonald, S., Pullenayegum, E., Taylor, V., Lutsiv, O., Good, C., Hutton, E., & Sword, W. (2011). Despite 2009 guidelines, few women report being counseled correctly about weight gain during pregnancy. American Journal of Obstetrics and Gynecology, 205(4), e1–e6.
Moore Simas, T., Waring, M., Sullivan, G., Lio, X., Rosal, M., Hardy, J., & Berry, R. (2013). Institute of medicine 2009 gestational weight gain guideline knowledge: Survey of obstetrics/gynecology and family medicine residents of the United States. Birth, 40(4), 237–246.
MooreSimas, T., Corvera, S., Lee, M., Zhang, N., Leung, K., Olendzki, B., … Rosal, M. (2015). Understanding multifactorial influences on the continuum of maternal weight trajectories in pregnancy and early postpartum: Study protocol, and participant baseline characteristics. BMC Pregnancy Childbirth, 15, 71.
Oken, E., Taveras, E., Kleinman, K., Rich-Edwards, J., & Gillman, M. (2007). Gestational weight gain and child adiposity at age 3 years. American Journal of Obstetrics and Gynecology, 196(4), 322 e1–e8.
Olson, C., & Strawderman, M. (2003). Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weightgain. Journal of the American Dietetic Association, 103(1), 48–54.
Phelan, S., Phipps, M., Abrams, B., Darroch, F., Shaffner, A., & Wing, R. R. (2011). Practitioner advice and gestational weight gain. Journal of Women’s Health, 20(4), 585–591.
Rasmussen, K. M., & Yaktine, A. L. (2009). Weight gain during pregnancy: Examining the guidelines. Washington, D.C.: Institute of Medicine and National Research Council of the National Academies.
Stotland, N., Cheng, Y., Hopkins, L., & Caughey, A. (2006). Gestational weight gain and adverse neonatal outcome among term infants. Obstetrics and Gynecology, 13(3), 635–643.
Stotland, N., Gilbert, P., Bogetz, A., Harper, C., Abrams, B., & Gerbert, B. (2010). Preventing excessive weight gain in pregnancy: How do prenatal care providers approach counseling? Journal of Women’s Health, 19(4), 807–814.
Stotland, N., Haas, J., Brawarsky, P., Jackson, R., Fuentes-Afflick, E., & Escobar, G. (2005). Body mass index, provider advice, and target gestational weight gain. Obstetrics and Gynecology, 105(3), 633–638.
Stotland, N., Hopkins, L., & Caughey, A. (2004). Gestational weight gain, macrosomia, and risk of cesarean birth in nondiabetic nulliparas. Obstetrics and Gynecology, 104(4), 671–677.
Thande, N., Hurstak, E., Sciacca, R., & Giardina, E. (2009). Management of obesity: A challenge for medical training and practice. Obesity, 17(1), 107–113.
Wrotniak, B., Dentice, S., Mariano, K., Salaam, E., Cowley, A., & Mauro, E. (2015). Counseling about weight gain guidelines and subsequent gestational weight gain. Journal of Women’s Health, 24(10), 819–824.
Yarnall, K., Pollak, K., Ostbye, T., Krause, K., & Michener, J. (2003). Primary care: Is there enough time for prevention. American Journal of Public Health, 93(4), 635–641.
Zapka, J., Lemon, S., Estabrook, B., & Rosal, M. (2009). Factors related to weight loss behavior in a multiracial/ethnic workforce. Ethnicity and Disease, 19(2), 154–160.
Acknowledgements
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR000161, NIH/NIMHD (Grant #1 P60 MD006912-02), the CDC (Grant # U48 DP001933) and NIH-National Institute of General Medical Science (Grant # 5 R25 GM113686-02). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Lopez-Cepero, A., Leung, K., Moore Simas, T. et al. Association Between Obstetric Provider’s Advice and Gestational Weight Gain. Matern Child Health J 22, 1127–1134 (2018). https://doi.org/10.1007/s10995-018-2497-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2497-y