Abstract
Objectives The United States is one of only three countries worldwide with no national policy guaranteeing paid leave to employed women who give birth. While maternity leave has been linked to improved maternal and child outcomes in international contexts, up-to-date research evidence in the U.S. context is needed to inform current policy debates on paid family leave. Methods Using data from Listening to Mothers III, a national survey of women ages 18–45 who gave birth in 2011–2012, we conducted multivariate logistic regression to predict the likelihood of outcomes related to infant health, maternal physical and mental health, and maternal health behaviors by the use and duration of paid maternity leave. Results Use of paid and unpaid leave varied significantly by race/ethnicity and household income. Women who took paid maternity leave experienced a 47% decrease in the odds of re-hospitalizing their infants (95% CI 0.3, 1.0) and a 51% decrease in the odds of being re-hospitalized themselves (95% CI 0.3, 0.9) at 21 months postpartum, compared to women taking unpaid or no leave. They also had 1.8 times the odds of doing well with exercise (95% CI 1.1, 3.0) and stress management (95% CI 1.1, 2.8), compared to women taking only unpaid leave. Conclusions for Practice Paid maternity leave significantly predicts lower odds of maternal and infant re-hospitalization and higher odds of doing well with exercise and stress management. Policies aimed at expanding access to paid maternity and family leave may contribute toward reducing socio-demographic disparities in paid leave use and its associated health benefits.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Generous maternity leave benefits have been associated with lower rates of infant and child mortality and positive indicators for maternal mental health, breastfeeding, and childhood vaccination in international contexts. This study adds to the existing field of knowledge by examining (1) the associations between maternity and health in the U.S. context and (2) differentiating between paid and unpaid maternity leave. Out findings suggest use and duration of paid maternity leave to be associated with lower odds of maternal and infant re-hospitalization and positive maternal health behaviors, providing important information for policymakers considering implementing national paid family policies in the U.S.
Introduction
Labor force participation in the United States has increased significantly among women with young children, from 34% in 1976 to 61% in 2015 (Juhn and Potter 2006; U.S. Bureau of Labor Statistics 2016). Maternal employment may contribute positively to maternal and child health by improving women’s physical and mental health and preventing the loss of wages and health insurance coverage after childbirth (Hill et al. 2005; Jou et al. 2016; Repetti et al. 1989). Due to competing demands from work and family, however, many women face barriers in returning to paid work after childbirth, creating persistent gender inequalities in career trajectory and income (Glass 2004; Hegewisch and Gornick 2011). These disparities may in turn reduce the resources women have available to invest in their own and their children’s health (Grossman 1972; McGovern et al. 1997; Chatterji and Markowitz 2012).
One potential strategy for improving health outcomes among reproductive-age women and their children is to ensure women access to paid leave after the birth or adoption of a child. Paid leave allows women time to recover physically from childbirth and to care for their infants without risking employment or income loss. All but three countries worldwide have implemented national paid maternity leave policies: Papua New Guinea, Suriname, and the U.S. (WORLD Policy Analysis Center 2015). Maternity leave in the U.S. is guaranteed only through the Family and Medical Leave Act (FMLA), which requires large employers to make 12 weeks of unpaid, job-protected leave available each year for qualified medical or family reasons, including caring for newborn children (The Family and Medical Leave Act of 1993, as amended to 2009).
Many U.S. workers do not meet the eligibility criteria for the FMLA, which applies only to employers with over 50 employees and employees who worked at least 1250 h during the previous 12 months (U.S. Department of Labor, 1993). Additionally, the FMLA does not include provisions for paid leave. In 2015, only 13% of U.S. workers reported having paid family leave available, and 12% had no leave (Perez and Groshen 2015). Access to family leave, which includes both maternity leave and less commonly available benefits such as paternity and family caregiving leave, varies across socio-demographic lines. In 2015, over 20% of low-income and part-time workers reported having no family leave available, and paid family leave was available to only 4% of workers in the lowest income decile and 5–7% of workers in the construction, transportation, and service sectors (Perez and Groshen 2015). Even with unpaid leave available, many women may not be able to afford taking extended leaves of absence from work without pay. In 2012, over 2.8 million U.S. workers refrained from taking needed family or medical leave due to economic concerns (Klerman et al. 2014).
Existing research suggests positive associations between maternity leave and infant health, including reduced neonatal and child mortality, low birth weight, and premature birth; improved developmental outcomes; and longer breastfeeding duration (Berger et al. 2005; Rossin 2011; Ruhm 2000). Some maternal mental health benefits are also associated with paid leave, including lower likelihood of exhibiting depressive symptoms or psychological distress (Aitken et al. 2015; Dagher et al. 2014). Evidence on maternal physical health is more limited. One systematic review found positive relationships between leave duration and maternal mental health, but little evidence on maternal physical health or health behaviors (Andres et al. 2016). A study of California women found a 6-week increase in paid leave availability to be associated with improvements in self-rated health; others have found no association between maternity leave duration and backache, sleep deprivation, or overall health status (Killien et al. 2001; Staehelin et al. 2007).
Several factors limit the current research on paid maternity leave and health. Few studies distinguish between paid and unpaid leave, which can affect resource availability and leave duration. Most existing studies have geographically or demographically homogeneous study populations, limiting their generalizability (Andres et al. 2016). The few nationally-representative studies conducted largely use data collected over two decades ago (Aitken et al. 2015; Staehelin et al. 2007). Policy developments since, including the passage of the FMLA in 1993 and subsequent state-level policy changes, have likely influenced women’s access to and experiences of maternity leave.
This study examines the associations between paid maternity leave and maternal/infant health, using data from a national survey of women who gave birth in 2011–2012. As paid family leave policies gain increasing prominence in both federal and local jurisdictions—including New York and San Francisco, which passed state- and city-wide leave legislation in June 2016 (Domonoske 2016)—our results are expected to inform current policy debates by providing empirical evidence on the potential associations between paid maternity leave and the health of women and infants.
Methods
Data and Study Population
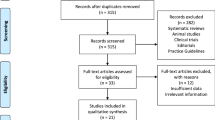
This study uses data from Listening to Mothers III (LTM3), a national survey of women ages 18–45 who gave birth to singleton infants in U.S. hospitals from July 2011–June 2012 (N = 2400). Commissioned by Childbirth Connection and administered by Harris Interactive, the survey consisted of two waves: the core survey, fielded October–December 2012 via internet (N = 2400), and a follow-up survey administered January–April 2013 (N = 1072). Respondents were recruited from four of Harris Interactive’s ongoing survey panels using a probability-based quota sampling method until a nationally representative base sample was obtained. For most socio-demographic characteristics, including age, race/ethnicity, and level of education, the full study sample from both surveys closely mirrors the national population of U.S. women who gave birth in 2011–2012 (Monte and Ellis 2014). Further details on survey methodology, including validation of survey measures, may be found in the survey report (Declercq et al. 2013).
Participants were instructed to complete the web-based core survey; respondents who did so were then invited to complete the follow-up survey at least 3 months after the initial core survey. On average, respondents were 14.3 months postpartum at the time of the follow-up survey. To account for potential biases associated with internet use or the likelihood of responding to the follow-up survey, propensity score weighting was applied to the dataset, along with survey weighting for demographic variables such as age, race/ethnicity, geographic region, educational attainment, and household income to more accurately reflect the target population. The final sample consisted of 700 women who indicated in the follow-up survey that they were working part- or full-time during pregnancy.
Measurement
Use and duration of paid maternity leave were the main predictors. Respondents were asked, “Did the employer you worked for during your pregnancy have a paid maternity leave benefit?”, with answer choices being, “Yes, but I didn’t take any paid leave”; “Yes, and I took paid leave”; “No, my employer did not have such a policy”; and “Not sure.” Separately, they were also asked whether their employer had an unpaid maternity leave benefit. To represent paid leave use, we constructed a dummy variable indicating whether respondents took paid maternity leave (either alone or in combination with unpaid leave) or not (i.e., taking either unpaid leave only or no leave). Another dummy variable was created to compare respondents who took partially- or fully-paid leave to respondents who took unpaid leave only.
Due to evidence suggesting a non-linear relationship between maternity leave duration and maternal health (Dagher et al. 2014), we coded paid leave duration as a 4-category variable from an open-ended question asking respondents, “For how many weeks did you receive paid leave?” Responses were categorized as 0, 1–6, 7–12, and more than 12 weeks of paid leave use, with cutoff points based on observational distribution, national initiatives regarding leave, policy considerations, and consistent with prior studies (Aitken et al. 2015; Andres et al. 2016; 115th Congress of the United States). Women who took no paid leave were included in the “0 weeks” category.
Infant health outcomes included health status, re-hospitalization, and well- and sick-child visits. Respondents were asked “Overall, how would you rate the health of your baby?”, with responses condensed from a 4-point Likert scale into a dichotomous variable indicating whether infants were in “excellent” health. Re-hospitalization, a key health care quality metric (Society for Maternal-Fetal Medicine et al. 2016), was coded from a question asking whether respondents’ newborns had had a medical problem causing an overnight hospital stay since birth. Respondents were also asked the number of “…‘well’ and ‘sick’ visits [their child had] had at a health care provider’s office” since birth. For well-child visits, we created a dummy variable indicating whether the minimum number of visits by age recommended by the American Academy of Pediatrics was met (American Academy of Pediatrics 2014). For sick-child visits, the number of visits was divided by the child’s age in months and a dummy variable created indicating whether the number of visits by age exceeded the distributional median.
Indicators for maternal health included re-hospitalization, physical pain, depressive symptoms, and use of mental health care. The two physical health indicators were coded from a yes/no question on re-hospitalization since giving birth and another on whether pain interfered with routine activities in the first 2 months postpartum. Mental health measures included a dichotomous variable indicating whether respondents saw a mental health professional at any point after childbirth and another representing depressive symptomology.Footnote 1
Four outcome indicators for maternal health behaviors were coded from a question asking respondents, “Thinking about the past 2 weeks, how well do you think you are doing with each of the following? (1) Getting enough exercise; (2) Eating a healthy diet; (3) Managing stress; and (4) Getting enough sleep.” Responses were given on a five-item Likert scale from 1 “Not at all well” to 5 “Extremely well,” which were then collapsed into dummy variables indicating whether or not the respondent was doing “Very” or “Extremely” well for each of the four behaviors.
Covariates included age, race/ethnicity, level of education, household income, Census region, marital status, mode of delivery, parity, pregnancy complexity, low birthweight, and number of months since birth. Pregnancy complexity refers to respondents who, prior to becoming pregnant, had been obese (BMI ≥ 30 kg/m2), taking medication for depression or high blood pressure, or diagnosed with Type 1 or 2 diabetes. Number of months since childbirth ranged from 7 to 21 months.
Analysis
One-way tabulation was used to describe sample characteristics and two-way tabulation with design-based F-tests used to identify significant differences in paid leave use and duration by socio-demographic and birth-related characteristics. Logistic and multinomial logit regression models were used to estimate the likelihood of each maternal and infant health outcome, as predicted by paid leave. To address potential selection bias, we applied propensity score weights to each regression model. Propensity scores for the main predictors were estimated based on factors expected or demonstrated to differ by exposure, including age, household income, full-time (versus part-time) work status, share of child care responsibilities with a partner (equal versus unequal share), and whether respondents’ employers met their needs for pregnancy-related accommodations (Jou et al. 2016). Weights were then created by taking the inverse of the propensity scores. All regression models were adjusted for the covariates listed above and run using both the propensity score weights and the original survey weights to determine whether results differed significantly due to selection based on observed variables. All analyses were conducted using Stata 11.2 (StataCorp, College Station, TX).
Results
Of the 700 women in the study population, 50% took fully- or partially-paid maternity leave, 20% took unpaid leave only, and 30% took no leave (Table 1). Over three-fourths (77%) of respondents rated their infants as being in excellent health. Prevalence of overnight re-hospitalization was similar for respondents (12%) and their infants (10%). Around one-third of women rated themselves as doing well with each of the four health-related behaviors, with adequate sleep (29%) being least common and stress management (38%) being most.
Compared to the overall U.S. population of women who gave birth in 2012, women in the study sample tended to be slightly older, more highly educated, and non-Hispanic white (Table 2). Around 23% of respondents were between ages 18 and 24, 28% were 25–29 and 30–34, and 20% were 35 or older. Non-Hispanic white women comprised nearly two-thirds of the study sample (63%), followed by Hispanic or Latina women (18%), non-Hispanic black women (13%), and women of other or multiple races/ethnicities (6%). Nearly half (45%) of the respondents had a Bachelor’s or graduate degree, and 40% were in the top income bracket of $75,301 and above. Leave use differed significantly by race/ethnicity and income, with fewer non-Hispanic black women taking either paid or unpaid leave (p = 0.042) and fewer lower- and middle-income women taking paid leave (p = 0.028). Leave duration varied by age and income, with shorter lengths of paid leave more common among women ages 18–24 (p = 0.003) and women in the lowest income bracket (p = 0.013).
Maternity leave use significantly predicted infant and maternal health outcomes (Table 3). Women who took partially- or fully-paid leave experienced a nearly 50% reduction in the odds of having had their infants hospitalized (AOR 0.53; 95% CI 0.3–1.0), having been hospitalized themselves (AOR 0.49; 95% CI 0.3–0.9), and having seen a mental health care provider (AOR 0.53; 95% CI 0.3–0.9) since childbirth, compared to women who did not take paid maternity leave. Compared to women who took only unpaid leave, women taking paid leave had 1.76 and 1.78 times the odds of reporting themselves as doing very or extremely well with exercise (95% CI 1.1–3.0) and stress management (95% CI 1.1–2.8), respectively, during the 2 weeks prior to survey.
Duration of paid leave significantly predicted health outcomes (Table 4). Women who took over 12 weeks of leave saw a nearly 75% decrease in the odds of having had their infant re-hospitalized (AOR 0.26; 95% CI 0.1–0.9) and having seen a mental health professional (AOR 0.28; 95% CI 0.1–1.0) since giving birth, compared to women who took no paid leave. No significant differences were found between women taking 12 or fewer weeks and women taking no paid maternity leave.
Discussion
Our analysis indicates that use and duration of paid maternity leave is associated with positive indicators of maternal and infant health, including lower likelihood of maternal and infant re-hospitalization and maternal mental health care use. These results support previous findings showing maternity leave to be associated with decreased infant mortality and improved maternal vitality and life satisfaction (Andres et al. 2016; Berger et al. 2005). By differentiating between paid and unpaid leave, we build on earlier work by highlighting unique associations between paid maternity leave and maternal and infant health, which may not manifest when the only leave available is unpaid. Additionally, we find paid leave use to be associated with higher odds of positive health behaviors such as exercise and stress management when compared to the use of unpaid-only leave. Previous studies have addressed changes in health behaviors among women pre- and post-partum and described dietary and sleep patterns among women during the first years after childbirth (Grace et al. 2006; Xiao et al. 2016). Ours is among the first to explore the potential associations between maternity leave and health-related behaviors among women who recently gave birth. We also build upon previous literature by examining outcomes among a diverse study population in terms of education and income level, race/ethnicity, and geographic region, which more closely resembles the socio-demographic characteristics of the total population of U.S. women who gave birth in 2011–2012. Doing so allows the findings from this study to be generalized beyond a single location or demographic group to the broader population of U.S. women of childbearing age and enables subgroup analyses that highlight disparities in access to paid maternity leave. Our analysis also finds paid leave over 12 weeks to be associated with lower likelihood of infant re-hospitalization and maternal mental health care use. This finding aligns with earlier research showing paid maternity leave to predict increased uptake of recommended childhood vaccinations, which may prevent serious illness and hospitalization, along with studies associating paid leave duration positively with maternal mental health (Hajizadeh et al. 2015; Staehelin et al. 2007). Infant re-hospitalizations are most commonly due to acute respiratory, infectious, gastrointestinal, and chronic respiratory disease, while common causes of maternal re-hospitalization include postpartum or wound infections, pulmonary conditions, and surgical complications (Underwood et al. 2007; Bashiri et al. 2003). Paid leave not only provides women with compensated time to recover from childbirth, but may also allow them to seek prompt care for their infants and themselves upon initial presentation of illness, which may prevent complications that require hospital re-admission. While our finding on maternal mental health use does not differentiate between respondents who experienced decreased need for mental health care and respondents forgoing needed care, women who took over 12 weeks of paid leave tended overwhelmingly to be high-income, making financial constraint an unlikely barrier to mental health care use. Instead, women with higher-income positions may have workplace responsibilities that prevent them from taking needed time to seek mental health care. Given the lack of significant association between paid leave and the likelihood of exhibiting depressive symptoms, our findings do not contradict existing evidence on the benefits of longer leave duration for maternal mental health.
These findings have potentially important policy implications, especially as discourse on work-family balance gains increasing prominence in the U.S. In the 2015 State of the Union address, former President Barack Obama highlighted the U.S. as “the only advanced country on Earth that doesn’t guarantee paid sick leave or paid maternity leave to our workers” and called for “new action to help states adopt paid leave laws” (U.S. White House 2015). In February 2017, policymakers re-introduced the Family and Medical Insurance Leave (FAMILY) Act (S.1810/H.R.3712) in the U.S. Senate, under which joint payroll contributions would fund up to 12 weeks of paid leave for all eligible workers in the U.S. (115th Congress of the United States). This study provides current, empirical evidence of significant associations between paid maternity leave and positive indicators for maternal and infant health in the U.S. Maternity leave policies may also generate health care cost savings, especially with regard to re-hospitalizations. Each instance of maternal re-hospitalization adds $1700–3000 to the costs of childbirth; for pre-term infants, average annual costs of re-hospitalization exceed $40 million nationally, with an average per-infant cost of $15,100 (Declercq et al. 2007; Russell et al. 2007; Underwood et al. 2007). Together with research from international contexts, these findings highlight the need to consider policies and incentives designed to increase women’s access to paid maternity leave and to address issues of equity.
Guaranteed access to maternity leave may also reduce the disparities in leave use documented in this study. Our findings show that higher percentages of non-Hispanic Black and Hispanic women take no maternity leave compared to non-Hispanic White women. Moreover, women in the lowest income group tend to take no leave, while women with mid-level incomes tend to take unpaid-only and women in the highest income group tend to take partially- or fully-paid leave. Similar patterns of racial/ethnic and socioeconomic disparity are reflected in maternal/infant health outcomes. Mortality rates for infants born to African-American women (12.4 per 1000 births) were nearly twice the national average (6.4 per 1000 births) in 2009 (Matthews and MacDorman 2012). The relative risk of neonatal mortality in the most socioeconomically deprived groups compared to the least deprived groups has increased from 36 to 43% higher from 1985 to 2000 (Singh and Kogan 2007). Policies that increase access to maternity leave, including more lenient criteria to qualify for FMLA and some length of paid leave guaranteed to vulnerable groups such as women of color and lower-income women, may support the reduction of these socio-demographic disparities. Further research on policy effects should explicitly examine the equity impacts of efforts to expand leave access.
Several states have implemented recent legislation providing paid family leave and subsequently seen higher take-up rates, especially among workers with lower-wage jobs (Milkman and Appelbaum 2013). Though mandated benefits may have unintended consequences such as decreased wages for women (Gruber 1994), recent studies suggest that women with access to paid maternity leave work more hours, with a corresponding wage increase (Rossin-Slater et al. 2013). Maternity leave is strongly associated with women’s return to the labor force following childbirth, which reduces loss of employment-related earnings long-term (Hegewisch and Gornick 2011). In states with paid family leave policies, employers avoid incurring the direct costs of financing paid leave due to funding structures that shift costs to employees through a small increase to payroll tax (around 1%). As a result, a majority of employers in states such as California have reported no increase in costs associated with paid leave mandates, while a small percentage (9%) reported cost savings due to reduced employee turnover (Milkman and Appelbaum 2013). Given the success of state policies in encouraging paid leave use while remaining cost-effective to employers, federal measures may expand access to paid maternity and family leave without incurring substantial costs or widening the gender wage gap. Federal policy may also be more effective in reducing geographic disparities in leave availability, especially in states with a higher percentage of small employers or households below the poverty level.
Limitations
These findings should be considered relative to their limitations. While the LTM3 provides unique data on women’s health and employment around the time of childbirth, it lacks detailed information about respondents’ occupation, employer size, and length of tenure, which may determine whether women have maternity leave available. Though we use household income as a proxy for these attributes, future surveys should include specific information on the conditions of women’s employment in addition to detailed health indicators. Additionally, the characteristics of women who do and do not take leave are likely to differ systematically, affecting health outcomes independently of maternity leave. By calculating the propensity of respondents to take paid leave and conducting our analyses using both survey and propensity score weights, we aimed to account for any significant differences in observed characteristics between these two groups. There could, however, remain unobserved characteristics that we were not able match on. Our study also focuses on maternity leave, as women are most commonly the primary caregivers for infants and young children in the U.S. Given the implications for gender equality, we recommend more detailed data collection and research efforts addressing paid leave among fathers and other non-maternal caregivers.
The directionality of association between maternity leave use and maternal/infant health may be uncertain, especially in cases where severe illness or complications during pregnancy or birth necessitate leave. The Pregnancy Discrimination Act of 1978 requires employers to extend temporary disability benefits to employees with pregnancy- or childbirth-related conditions; in many states, medical complications in pregnancy or childbirth allow women to request extended temporary disability benefits (U.S. Equal Employment Opportunity Commission 2015). Women who experience complications may therefore have better access to postpartum leave. While our models are adjusted for several birth-related characteristics that may affect women’s decisions regarding leave use, we recommend further study into these factors.
Several additional limitations may be attributed to the nature of the dataset. As a survey, the LTM3 contains data derived from retrospective self-report, which introduces potential recall bias. Because the data are cross-sectional, we were not able to draw any causal inferences regarding the impact of paid maternity leave policies on health outcomes. Future research should focus on data collection and analysis approaches that allow for longitudinal study designs. Moreover, our measures of maternal health behaviors were based on self-perceived performance in the areas of diet, exercise, sleep, and stress management, rather than standardized measures of these dimensions, which may introduce imprecision in the construct being measured. While we recognize the importance of self-perception in health status and behaviors, we recommend the inclusion of standard health behavior measures in future data collection efforts.
Conclusion
Consistent with international findings, we find maternity leave use and duration in the U.S. to have positive associations with maternal and infant health. In particular, the use of paid maternity leave is associated with lower likelihood of maternal and infant re-hospitalization and positive maternal health behaviors such as exercise and stress management. Policies that expand access to paid leave may contribute toward not only cost savings in terms of reduced healthcare utilization and improved employee retention, but also immediate and longer-term improvements in the health of women and children. As national policy debates continue to address work-family balance, this study aims to serve as a basis for future data collection and analysis efforts on issues related to family leave and health throughout the lifespan.
Notes
Respondents were coded as having depressive symptoms if they indicated feeling “little interest or pleasure in doing things” or “down, depressed, or hopeless” either “More than half the days” or “Nearly every day” during the two weeks prior to the survey.
References
115th Congress of the United States. Family and Medical Insurance Leave Act, S.1810/H.R.3712 C.F.R. (2017).
Aitken, Z., Garrett, C. C., Hewitt, B., Keogh, L., Hocking, J. S., & Kavanagh, A. M. (2015). The maternal health outcomes of paid maternity leave: A systematic review. Social Science & Medicine, 140, 32–41.
American Academy of Pediatrics. (2014). Periodicity schedule: Schedule of screenings & assessments recommended at each well-child visit from infancy through adolescence. Retrieved 12 February, 2015, from http://www.aap.org/en-us/professional-resources/practice-support/Pages/PeriodicitySchedule.aspx.
Andres, E., Baird, S., Bingenheimer, J. B., & Markus, A. R. (2016). Maternity leave access and health: A systematic narrative review and conceptual framework development. Maternal Child Health Journal, 20, 1178–1192.
Bashiri, A., Smolin, A., Sheiner, E., Zelingher, J., & Mazor, M. (2003). Maternal rehospitalization after singleton term vaginal delivery. The Journal of Maternal-Fetal & Neonatal Medicine, 14(5), 344–348.
Berger, L. M., Hill, J., & Waldfogel, J. (2005). Maternity leave, early maternal employment, and child health and development in the US. The Economic Journal, 115, F29-F47.
Chatterji, P., & Markowitz, S. (2012). Family leave after childbirth and the mental health of new mothers. Journal of Mental Health Policy and Economics, 15(2), 61–76.
Dagher, R. K., McGovern, P. M., & Dowd, B. E. (2014). Maternity leave duration and postpartum mental and physical health: Implications for leave policies. Journal of Health Politics, Policy, and Law, 39(2), 369–416.
Declercq, E. R., Barger, M., Cabral, H. J., Evans, S. R., Kotelchuck, M., Simon, C., … Heffner, L. J. (2007). Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstetrics & Gynecology, 109(3), 669–677.
Declercq, E. R., Sakalar, C., Corry, M. P., Applebaum, S., & Herrlich, A. (2013). Listening to Mothers III: Pregnancy and Birth. New York: Childbirth Connection.
Domonoske, C. (2016, 6 April). A big week for parents: New York State, San Francisco establish paid-leave laws. Retrieved 30 April, 2016, from http://www.npr.org/sections/thetwo-way/2016/04/06/473226596/a-big-week-for-parents-new-york-state-san-francisco-establish-paid-leave-laws.
Glass, J. (2004). Blessing or curse? Work-family policies and mother’s wage growth over time. Work and Occupations, 31(3), 367–394.
Grace, S. L., Williams, A., Stewart, D. E., & Franche, R.-L. (2006). Health-promoting behaviors through pregnancy, maternity leave, and return to work: Effects of role spillover and other correlates. Women & Health, 43(2), 51–72.
Grossman, M. (1972). On the concept of health capital and the demand for health. Journal of Political Economy, 80(2), 223–255.
Gruber, J. (1994). The incidence of mandated maternity benefits. American Economic Review, 84(3), 622–641.
Hajizadeh, M., Heymann, J., Strumpf, E., Harper, S., & Nandi, A. (2015). Paid maternity leave and childhood vaccination uptake: Longitudinal evidence from 20 low-and-middle-income countries. Social Science & Medicine, 140, 104–117.
Hegewisch, A., & Gornick, J. C. (2011). The impact of work-family policies on women’s employment: A review of research from OECD countries. Community, Work & Family, 14(2), 119–138.
Hill, J., Waldfogel, J., Brooks-Gunn, J., & Han, W.-J. (2005). Maternal employment and child development: A fresh look using newer methods. Developmental Psychology, 41(6), 833–850.
Jou, J., Kozhimannil, K. B., Blewett, L. A., McGovern, P. M., & Abraham, J. M. (2016). Workplace accommodations for pregnant employees: Associations with women’s access to health insurance coverage after childbirth. Journal of Occupations and Environmental Medicine, 58(6), 561–566.
Juhn, C., & Potter, S. (2006). Changes in labor force participation in the United States. Journal of Economic Perspectives, 20(3), 27–46.
Killien, M. G., Habermann, B., & Jarrett, M. (2001). Influence of employment characteristics on postpartum mother’s health. Women & Health, 33(1–2), 63–81.
Klerman, J. A., Daley, K., & Pozniak, A. (2014). Family and medical leave in 2012: Technical report. In J. Simonetta (Ed.). Cambridge, MA: Abt Associates, Inc.
Matthews, T. J., & MacDorman, M. F. (2012). Infant mortality statistics from the 2009 period linked birth/infant death data set. National Vital Statistics Report, 61(8):1–26.
McGovern, P., Dowd, B., Gjerdingen, D., Moscovice, I., Kochevar, L., & Lohman, W. (1997). Time off work and the postpartum health of employed women. Medical Care, 35(5), 507–521.
Milkman, R., & Appelbaum, E. (2013). Unfinished business: Paid family in California and the future of U.S. work-family policy. Ithaca, NY: Cornell University Press.
Monte, L., & Ellis, R. (2014). Fertility of women in the United States: 2012 (pp. 1–26). Washington DC: United States Census Bureau, U.S. Department of Commerce.
Perez, T. E., & Groshen, E. L. (2015). National Compensation Survey: Employee benefits in the United States, March 2015. Washington DC: U.S. Department of Labor.
Repetti, R. L., Matthews, K. A., & Waldron, I. (1989). Employment and women’s health: Effects of paid employment on women’s mental and physical health. American Psychologist, 44(11), 1394–1401.
Rossin, M. (2011). The effects of maternity leave on children’s birth and infant health outcomes in the United States. Journal of Health Economics, 30, 221–239.
Rossin-Slater, M., Ruhm, C. J., & Waldfogel, J. (2013). The effects of California’s paid family leave program on mothers’ leave-taking and subsequent labor market outcomes. The Journal of Policy Analysis and Management, 32(2), 224–245.
Ruhm, C. J. (2000). Parental leave and child health. Journal of Health Economics, 19, 931–960.
Russell, R. B., Green, N. S., Steiner, C. A., Meikle, S., Howse, J. L., Poschman, K., … Petrini, J. R. (2007). Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics, 120(1), e1–e9.
Shapiro-Mendoza, C. K., Tomashek, K. M., Kotelchuck, M., Barfield, W., Weiss, J., & Evans, S. Risk factors for neonatal morbidity and mortality among “healthy,” late preterm newborns. Seminars in Perinatology, 30(2), 54–60.
Singh, G. K., & Kogan, M. D. (2007). Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the United States, 1969–2001. Pediatrics, 119(4), e928–e939.
Society for Maternal-Fetal Medicine, Bailit, J. L., Gregory, K. D., Srinivas, S., Westover, T., Grobman, W.A., & Saade, G.R. (2016). Society for Maternal-Fetal Medicine (SMFM) special report: Current approaches to measuring quality of care in obstetrics. American Journal of Obstetrics & Gynecology, 215(3), B8–B16.
Staehelin, K., Bertea, P. C., & Stutz, E. Z. (2007). Length of maternity leave and health of mother and child - a review. International Journal of Public Health, 52, 202–209.
The Family and Medical Leave Act of 1993, as amended to 2009 (1993).
U.S. Bureau of Labor Statistics. (2016, 22 April). Employment status of mothers with own children under 3 years old by single year of age of youngest child and marital status, 2014–2015 annual averages. Economic News Release. Retrieved 15 September, 2016, from http://www.bls.gov/news.release/famee.t06.htm.
U.S. Equal Employment Opportunity Commission. (2015). Pregnancy discrimination. Retrieved 26 February, 2015, from http://www.eeoc.gov/laws/types/pregnancy.cfm.
U.S. White House (2015, 20 January). Remarks by the President in State of the Union Address, January 20, 2015. Retrieved 30 January, 2015, from http://www.whitehouse.gov/the-press-office/2015/01/20/remarks-president-state-union-address-january-20-2015.
Underwood, M. A., Danielsen, B., & Gilbert, W. M. (2007). Cost, causes and rates of rehospitalization of preterm infants. Journal of Perinatology, 27, 614–619.
WORLD Policy Analysis Center. (2015). Is paid leave avilable for mothers of infants? Retrieved 12 September, 2016, from http://worldpolicycenter.org/policies/is-paid-leave-available-for-mothers-of-infants.
Xiao, R. S., Moore Simas, T. A., Pagoto, S. L., Person, S. D., Rosal, M. C., & Waring, M. E. (2016). Sleep duration and diet quality among women within 5 years of childbirth in the United States: A cross-sectional study. Maternal Child Health Journal, 20, 1869–1877.
Acknowledgements
This project was supported by a Health Services Research Dissertation Award from the Agency for Healthcare Research and Quality (1R36 HS023950-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jou, J., Kozhimannil, K.B., Abraham, J.M. et al. Paid Maternity Leave in the United States: Associations with Maternal and Infant Health. Matern Child Health J 22, 216–225 (2018). https://doi.org/10.1007/s10995-017-2393-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-017-2393-x