Abstract
Introduction The home and school environments play important roles in influencing children’s health behaviours. However, their simultaneous influence on childhood obesity has not yet been examined. We explore the relationship of the home and school environments with childhood obesity, to determine whether this relationship is mediated by children’s fruit and vegetable intake and physical behaviours. Methods This study uses baseline data from 9 to 11 year old children, their parents and school principals (matched data n = 2466) from the Obesity Prevention and Lifestyle Project. Child-reported behaviours, parent-reported home environment and principal-reported school environment data were collected via questionnaires. Trained researchers measured children’s height and weight, and Body Mass Index (BMI, kg/m2) was calculated. Structural equation modelling was used to assess the relationship of the home and school environments with children’s fruit and vegetable intake, physical activity behaviours, and children’s BMI. Result The home diet environment was positively associated with child diet (β = 0.18, p < 0.001). The home physical activity environment had the largest inverse association with BMI (β = − 0.11, p < 0.001), indirectly through child physical activity (β = 0.28 ,p < 0.001). Schools’ healthy eating policy implementation was significantly associated with child diet (β = 0.52, p < 0.05), but physical activity policy was not associated with child activity (β = − 0.007, p > 0.05). The school environment was not associated with child BMI. Discussion The home environment had a stronger association with healthier child behaviours, compared to the school environment. These findings suggest that future childhood obesity interventions targeting healthier home environments and supporting parents can promote healthier child eating and physical activity behaviours.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
The home and school environments play important roles in influencing children’s health behaviours. However, limited evidence currently exists examining the direct and indirect effect of both the home and school environments on children’s weight status. Our study found that the home environment had a stronger association with children’s health behaviours than the school environment. Parents in particular may be promoters of their children’s behaviours, and thus weight, through the home environment.
Introduction
Childhood overweight and obesity affects one-quarter of all children in Australia (Australian Institute of Health and Welfare 2015), with a linear increase in prevalence persisting in some Australian states (Ho et al. 2017). Excess weight gain is a leading public health concern as it contributes to many health consequences (World Health Organization 2004).
A diet high in fruit and vegetables together with being physically active are known to be important for preventing weight gain (World Health Organization 2004). Yet high proportions of children are not meeting the recommended intake of fruit and vegetables (Department of Health and Ageing, Australian Food and Grocery Council, & Department of Agriculture Fisheries and Forestry 2007) according to the Australian Dietary Guidelines (ADG) (National Health and Medical Research Council 2013) and a minority are meeting the Australian Physical Activity Guidelines (Australian Bureau of Statistics 2013). Thus, the importance of targeting both diet and physical activity behaviours for long-term obesity prevention is evident.
Swinburn’s Ecological Model of Obesity proposes that environmental factors underpin diet and physical activity behaviours and indirectly affect weight status (Swinburn et al. 1999). A recent Cochrane review found that obesity prevention interventions have commonly targeted the school environment (Waters et al. 2011). Schools deliver education when children have the greatest receptivity for attitudinal and behavioural change, thus the school environment is a logical focus for efforts to encourage healthy behaviours. Although research has shown that schools can have a positive effect on children’s diet and physical activity behaviours and weight status (Jaime and Lock 2009; van Sluijs et al. 2007), Australian children aged 10–11 years spend approximately 26% of their day at school, a portion second to the time spent at home (50%) (Mullan 2013). Furthermore, recent research indicates that children are at an increased risk of gaining weight when they are out of school (school-holidays) than when they are in school (Franckle et al. 2014), demonstrating that school environments alone cannot solve the childhood obesity crisis.
Parents are the ‘gatekeepers’ of the home and have a central role in creating the environments which shape their children’s diet (Birch et al. 2007; Klesges et al. 1986) and physical activity behaviours (Klesges et al. 1986). Further, success of school intervention for healthy eating were shown to be reliant on the degree of family involvement (Krølner et al. 2009). Similarly, strong evidence exists that interventions involving both school and family are most successful for increasing physical activity (Kriemler et al. 2011; van Sluijs et al. 2007). Thus, both the home and school are promising environments for policy and strategy development (Waters et al. 2011).
Most studies investigating environmental influences on obesity include children and adolescents, thus limited conclusions can be made due to the developmental differences between these age groups. Therefore to our knowledge, the combined influence of the school and home environments on diet and physical activity behaviours and weight status of older primary school children (9–11 years) is still unclear. Additionally, there is limited evidence examining the direct effect of both the home and school environments on children’s weight status. The need for strong conceptual and analytical models to increase our understanding of the mechanisms that influence childhood obesity, through examining the moderators and mediators of the built environment (Ball et al. 2006; Baranowski 2004; Ding and Gebel 2012; Waters et al. 2011), has been acknowledged. Therefore this study aims to explore the influence of the home and school environments on children’s diet and physical activity behaviours and Body Mass Index (BMI).
Methods
Participants and Recruitment
This study uses baseline data from the Obesity Prevention and Lifestyle (OPAL) Evaluation Project (Leslie et al. 2015). OPAL was a state-funded, multi-site, community-based childhood obesity prevention program, initiated in 2009, and implemented in 20 local government areas across South Australia (SA), based on the Ensemble, Prévenons l’Obésité Des Enfants approach (Borys et al. 2012). Details of the OPAL evaluation have been reported (Bell et al. 2016). Briefly 20 selected intervention (OPAL communities) and 20 matched comparison communities in SA were invited to participate. OPAL communities were selected based on level of disadvantage using Socio-Economic Index for Areas (SEIFA), childhood obesity, household education, child population and local government readiness for participation. Comparison communities were matched as closely as possible to each OPAL community on the basis of maternal education, geographical location, Index of Relative Social Advantage (IRSD: a component of SEIFA based on a basket of income- and education-related measures), and population density of 0–18 year olds.
Baseline data were collected between November 2011 and August 2013. Recruitment details have been reported (Leslie et al. 2015). Briefly, all schools (n = 428) within eligible communities were invited to participate via a mailed information pack and a follow-up phone call to the principal. Upon agreement, information packs for parents of eligible children were delivered to the school and distributed to students. Principals of the targeted schools and parents of children in Years 4–6 each completed a questionnaire. Students in Years 4–6 whose parents gave consent and who themselves gave assent completed a questionnaire and had anthropometric measures taken. The sample for this study consists of predominantly 9–11 year old children, matched with their parents and school principals (n = 2466).
All procedures involving human subjects were approved by the relevant human research ethics committees from the Flinders University Social and Behavioural Sciences Ethics Committee, the South Australian Department of Health Human Research Ethics Committee, the Aboriginal Health Council Human Research Ethics Committee, the Department of Education and Child Development, and Catholic Education, South Australia.
Demographics
Children’s socio-demographic data including age, gender and locality were collected via questionnaires. Locality was classified as metropolitan or rural based on the child’s school location. The school’s Index of Community Socio-Educational Advantage (ICSEA: a scale of socio-educational advantage that is computed for schools)(Australian Curriculum Assessment and Reporting Authority 2013) was used as a measure of students’ socio-economic status (SES). ICSEA values range from approximately 500 (representing very disadvantaged) to approximately 1300 (representing very advantaged)(Australian Curriculum Assessment and Reporting Authority 2013). These scores were categorised into quintiles of disadvantage.
Child’s Weight Status
Anthropometric measures were conducted by trained researchers using the International Society for the Advancement of Kinanthropometry protocol (Stewart et al. 2011). Children’s height and weight were determined as the mean of two measures or the median of three measures if the first two measures differed by more than 0.5 cm or 0.5 kg respectively. BMI [weight(kg)/height(m)2] was calculated and weight status was determined using the International Obesity Taskforce BMI cut-points (Cole et al. 2000). Weight status was categorised into four groups: underweight (< 18.5 kg/m2), healthy weight (18.5–24.9 kg/m2), overweight (≥ 25.0 kg/m2) and obese (≥ 30.0 kg/m2).
Child Behaviours—Child Reported Diet and Physical Activity
Dietary data were estimated from four questions regarding the number of fruit (1 questionnaire item) and vegetable (3 questionnaire items) serves consumed the previous day. These questions were based on an existing valid and reliable tool (Bennett et al. 2009). Standard serve sizes used in the ADG (National Health and Medical Research Council 2013) were provided as a guide. For this study, total vegetable intake referred to all potato (excluding fried potato) and other vegetables and legumes. Individual responses greater than nine serves were identified as unrealistic and removed (< 1%). A score for fruit and vegetable intake was given to each child based on the following: 0 = did not have any fruit or vegetables, 1 = had some fruit or vegetables but less than recommended, 2 = met guidelines (had at least two serves of fruit or five serves of vegetables). Scores for each food group were summed to give the child’s overall healthy diet score (range 0–4).
Children reported the number of days (0–7) in the previous week that they were physically active for a total of 60 min or more per day, in accordance with the Australian Physical Activity and Sedentary Behaviour Guidelines(Department of Health 2014a). This question was based on validated items of the Health Behaviour of School Children Study (Roberts et al. 2009). Responses (range 0–7) were used to determine the child’s overall healthy physical activity score.
Home Environment—Primary Carer (parent) Reported Diet and Physical Activity
Table 1 describes the questionnaire items used to assess the home diet environment (HDE) and home physical activity environment (HPAE). The HDE was assessed using 11 items and responses were categorised into three variables (Table 1). Scores from these variables were summed to give a continuous score (range 0–43), where a higher score represents a healthier HDE. Seventeen items were used to assess the HPAE with items categorised into four variables (Table 1). Individual scores from these variables were summed to give a continuous score (range 0–21), where a higher score represents a healthier HPAE.
School Environment—Principal Reported Diet and Physical Activity
Table 2 describes the questionnaire items used to assess the School Diet Environment (SDE) and school physical activity environment (SPAE). The SDE was assessed using a 19-item variable on healthy eating policy implementation. Responses for each item were on a 4-point Likert scale (0 = not applicable, 1 = not too well, 2 = OK or 3 = very well). Five of these items, (1) setting adequate time for children to eat; (2) distributing information to parents about healthy eating; (3) involving parents in school’s healthy eating decisions; (4) supporting breastfeeding; and (5) linking with outside organisations) were considered not directly related to the school environment or healthy eating and were therefore removed. Fourteen items, described in Table 2, were subsequently used. Responses were summed to give a continuous score (range 0–42), where a higher score indicates a healthier SDE.
The SPA was assessed as per the SDE. Physical activity policy implementation was assessed using 13 items on a 4-point Likert scale (0 = not applicable, 1 = not too well, 2 = OK or 3 = very well). Four of these items, (1) communication with parents for school physical activity decisions; (2) linking with outside organisations; (3) making school grounds available for external clubs; and (4) including guidelines for electronics use in the curriculum) were considered not directly related to the school environment or physical activity and were therefore removed. Nine items, described in Table 2, were subsequently used. These values were summed to give a continuous score (range 0–27), where a higher score indicates a healthier SPAE.
While many of the items assessing the home and school environments were derived from previously validated questionnaires (Wilson et al. 2013), the psychometric properties of the final tools have not been determined.
Statistical Analyses
Data management and statistical analyses were performed using IBM SPSS version 22.0 (SPSS Inc., Chicago, IL, USA) and STATA version 14.0 (StataCorp LP, College Station, TX, USA). Means and standard deviations (SD) for discrete and continuous data were calculated and categorical variables are presented as percentages. Data normality was visually checked using frequency histograms and normal Q-Q plots. For not-normally distributed data, median and interquartile ranges (IQR) were reported.
Structural Equation Modelling
A two-step approach for structural equation modelling was used to examine the associations between the home and school environments and children’s diet and physical activity behaviours, and BMI. First, confirmatory factor analysis (CFA) was used to test two measurement models to determine how well the observed variables from the home environment fit within the latent variables, the HDE and the HPAE. The HDE had three indicators: (1) parental knowledge of fruit and vegetable guidelines, (2) parental intake of fruit and vegetables, and (3) parental behaviours associated with feeding routines. The HPAE had four indicators: (1) parental knowledge of physical activity guidelines, (2) parental encouragement of physical activity, (3) parental physical activity practices and (4) physical activity item availability in the home.
Secondly, the structural equation model (SEM) was used to assess the direct and indirect relationship between home and school environments on children’s diet and physical activity behaviours, and BMI. Child BMI was used to represent child weight status, the overall child healthy eating score was used to represent child diet, and the overall physical activity score was used to represent child physical activity behaviour. The model was adjusted for child age, gender, locality, and SES. In a separate model, the direct association between the school environments and child BMI was tested, adjusting for child age.
Models were estimated with maximum likelihood estimation and assessed using goodness-of-fit indices: Chi-squared test (X 2), appropriate fit corresponding with the root mean square error of approximation (RMSEA) and its 90% confidence interval with values < 0.05, and the standardised root mean residual (SRMR) of less than 0.08 (Dermody et al. 2015). Standardised regression weights with p values were represented in our models. The level of significance was set at p < 0.05.
Results
Characteristics of the Sample
Of the school principals invited to participate, 43% completed questionnaires. Of the eligible parents and children, 21 and 20%, respectively, completed questionnaires and provided anthropometric measures (children only). Child, parent and principal data were linked and 2466 cases were found in the matched data (Fig. 1).
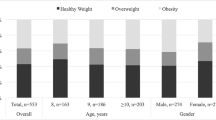
Child characteristics are shown in Table 3. Children were on average 10.6 years of age and approximately half (52%) were female. One-fifth (20.5%) of the children were overweight or obese, and the mean ICSEA score was 1015.
Children’s Diet and Physical Activity Behaviour
Children’s diet and physical activity behaviours are shown in Table 4. Although two-thirds (67%) of children met the recommended serves of fruit, only 17% consumed five or more vegetable serves. Nearly three-quarters of children had a healthy diet score of 2 (24.8%) or 3 (45.3%) (out of 4). For physical activity, one-third (33%) of children participated in more than 60 min of activity the previous day.
The Home and School Environments
Of all parents, 30% knew the recommended intake of both fruit and vegetables for children (Table 4). Few parents (8%) met the recommended intake of both fruit and vegetables for adults. Most children (82%) reported that their parents encouraged them to do physical activity. Three quarters (74%) of parents knew the physical activity guidelines and 9% of both parents met the adult guidelines for physical activity. Median scores for parental behaviours associated with feeding routines (how often they promoted healthy eating habits) and physical activity item availability at home are reported in Table 4.
Of the 182 schools in this study, few (6.4%) did not implement healthy eating or physical activity policies. Policy implementation scores are shown in Table 4.
Structural Equation Modelling (SEM)
To develop the latent constructs HDE and HPAE, two measurement models were generated (Figs. 2, 3). From the three observed variables related to the HDE, parental dietary intake had the highest factor loading (0.78) with the HDE (Fig. 2). For the HPAE, parental physical activity knowledge had the highest loading (0.56) of the four observed variables (Fig. 3).
After excluding cases due to missing data in the HDE, HPAE, SDE and SPAE, 1725 cases were available for the SEM. Model goodness-of-fit was acceptable (X 2 = 426.3, p < 0.001, RMSEA = 0.048[0.044–0.053], SRMR = 0.043). After adjusting for confounders (age, gender, locality, SES), a more positive HDE was directly associated with a healthier child diet (0.18 ,p < 0.001), but not child BMI. The HPAE had a positive association with child physical activity (0.28, p < 0.001), which was inversely correlated with BMI (− 0.11, p < 0.001) (Fig. 4). Conversely, although healthy eating policy in schools was significantly related to child diet (0.52, p < 0.05), implementing a physical activity policy was not associated with child physical activity behaviours (Fig. 4). In a separate model (Fig. 5), there was no relationship between school environments (as measured by implementation of healthy eating and physical activity policies) and child BMI (adjusted for child’s age).
Discussion
To our knowledge, this study is the first to have undertaken structural equation modelling to simultaneously examine the association of the home and school environments on primary school-aged children’s diet, activity behaviours and weight status. A healthier home environment was positively associated with healthier child diet and physical activity behaviours. The association of the home environment with healthier child behaviours was stronger than the association of the school environment, however there were no significant direct associations between the home and school environments and child BMI. A positive home environment was associated with parental knowledge of physical activity guidelines and parental intake of fruit and vegetables. An indirect association of child’s physical activity with BMI, via the HPAE was found, suggesting that a positive HPAE may be protective against childhood obesity.
Of all HDE components, parental intake of fruit and vegetables had the strongest association with child diet. This finding aligns with studies which found parental intake of fruit and vegetables to be positively associated with children’s intake (Blanchette and Brug 2005; Wyse et al. 2015). Similarly, a review showed that the extent to which parents practice healthy eating is positively associated with children’s eating behaviours(Ventura and Birch 2008), suggesting that interventions targeting parental fruit and vegetable consumption may improve children’s consumption. However limited research has examined the relationship between the home environment and child weight status. Therefore this study presents new findings. Child fruit and vegetable intake were not associated with BMI, consistent with a previous study conducted on children and adolescents (Field et al. 2003). A possible explanation is that only examining fruit and vegetable intake may not predict overall energy intake. Thus targeting only fruit and vegetable intake in interventions may not suffice for weight change and targeting other food group intake, in addition to physical activity, may result in better outcomes.
Of all HPAE components, parental knowledge of physical activity guidelines had the strongest association with child physical activity. Limited evidence exists to support this finding. However, a recent study conducted to understand parental concerns about children’s diet, activity and weight, found that parents were aware of the benefits of physical activity but thought children can meet the recommended 60 min of physical activity daily without support(Slater et al. 2010). Interestingly, of the HPAE components, parental physical activity encouragement was the next strongest association with child physical activity. Previous research supports this, as parental role modelling, rules around sedentary behaviour, and parental support for physical activity are important in improving children’s physical activity and weight over 5 years (Crawford et al. 2010). Thus, interventions that consider the importance of parental responsibility for children’s activity levels are warranted.
Our results showed healthier child physical activity behaviours may be a better predictor of lower BMI than diet. This association between physical activity and BMI is supported by previous cross-sectional (Abbott and Davies 2004) and cohort studies (Jago et al. 2005; Moore et al. 2003; Trost et al. 2003) that found increased physical activity to be associated with decreased BMI in preschool and primary school aged children. One longitudinal study (Jago et al. 2005) in particular found physical activity, but not dietary factors, to be a strong predictor of children’s BMI as they grew older. These results further emphasise the need to focus on increasing physical activity levels to curb obesity.
Implementing a healthy eating policy at school was weakly associated with child’s diet but no such association was observed between implementing physical activity policy and child’s physical activity. Further, we found no significant relationship between implementing healthy eating or physical activity policies and BMI. Interestingly, many countries are applying policies that follow the World Health Organization Nutrition-Friendly Schools Initiative (World Health Organization 2009), an internationally proposed school program to promote healthy eating and physical activity. A possible explanation of our findings may be that other aspects of the school environment (for example, staff awareness of policy implementation) were not examined. Nonetheless, previous research has elucidated that family involvement in school-based interventions is of importance to tackle childhood obesity. One study (Blanchette and Brug 2005) found school-based interventions that included parental involvement as a factor showed the most promise for fruit and vegetable intake among children. These results are in accord with a systematic review (Nixon et al. 2012) which concluded that interventions comprising high levels of parental involvement appeared most effective in reducing weight, and improving diet and physical activity behaviours in young children. Evidently, involving families in school-based interventions is warranted.
The strengths of this study are the large community-based sample and the objective anthropometric measures collected. The selection of relatively disadvantaged communities in metropolitan and rural regions provides insight on the need for family-based obesity prevention strategies in these communities. The application of SEM allowed exploration of the many moderators of health behaviours, thus our model can form the basis for future hypotheses generations. Our findings however must be considered within the limitations of this study. Although the majority of items in the current questionnaires were sourced from previously validated questionnaires, the psychometric properties of the compiled tools were not tested. Generalisability is limited because of the low participant response rates (~ 20% children and parents; ~40% principals). Due to the cross-sectional nature of this study, we were not able to determine causality between current BMI, child health behaviours and the measured environments (e.g. if the child’s current BMI was a consequence of the parents’ behaviours or whether the child’s BMI resulted in changes in the parents’ behaviours). Parents can also influence the school environment, however this correlation was not accounted for in our model, and therefore the two environments were treated as independent variables. Diet data were based on one day’s intake and thus do not reflect a usual eating pattern. As only fruit and vegetable intakes were used in this study to represent children’s diet, our results must be considered with caution as this alone does not reflect total energy intake. Residual confounding should be acknowledged, as there may be other factors which could have influenced our results (e.g. family structure). Lastly, other aspects of the home and school environments were not included (for example, sedentary behaviour of children and principal/teacher knowledge of fruit and vegetable serve guidelines) that may have improved the model’s goodness-of-fit indices. Nevertheless our findings are consistent with the social ecological framework (Swinburn et al. 1999), and provide important insight into the relationship between the home and school environments and children’s health behaviours. Our findings support other literature that family involvement in childhood obesity interventions is essential (Blanchette and Brug 2005; Crawford et al. 2010; Ventura and Birch 2008; Wyse et al. 2015). Childhood obesity has a complex aetiology and needs continuous research to unravel its complexities. Applying SEM has portrayed the significance of examining multiple factors which may be associated with childhood obesity. Thus continuous application of the SEM approach in future research is encouraged.
Our findings contribute to the evidence that the home environment plays an important role in determining diet and physical activity behaviours of primary school-aged children. Our model of the direct and indirect relationships with child BMI showed that a more positive home environment, specifically related to physical activity, can be protective of childhood obesity. Public health professionals and researchers can use these findings to engage families in future interventions and educate parents on the importance of supporting children’s total food intake and physical activity. Focusing on these aspects may be a promising strategy to tackle childhood obesity.
References
Abbott, R. A., & Davies, P. S. W. (2004). Habitual physical activity and physical activity intensity: Their relation to body composition in 5.0-10.5-y-old children. European journal of clinical nutrition, 58(2), 285–291.
Australian Bureau of Statistics. (2013). Australian Health Survey: Physical Activity, 2011–2012. Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/462FBA87B642FCA4CA257BAC0015F3CE?opendocument.
Australian Curriculum Assessment and Reporting Authority. (2013). Guide to understanding 2013 Index of Community Socio-educational Advantage (ICSEA) values. Retrieved from http://www.acara.edu.au/verve/_resources/Guide_to_understanding_2013_ICSEA_values.pdf.
Australian Institute of Health and Welfare. (2015). Overweight and obesity: Who is overweight? In Australian Institute of Health and Welfare (Ed.). Australia.
Ball, K., Timperio, A., & Crawford, D. (2006). Understanding environmental influences on nutrition and physical activity behaviors: Where should we look and what should we count? International Journal of Behavioral Nutrition and Physical Activity, 3(1), 33.
Baranowski, T. (2004). Why combine diet and physical activity in the same international research society? International Journal of Behavioral Nutrition and Physical Activity, 1(1), 2.
Bell, L., Ullah, S., Olds, T., Magarey, A., Leslie, E., Jones, M., … ,Cobiac, L. (2016). Prevalence and socio-economic distribution of eating, physical activity and sedentary behaviour among South Australian children in urban and rural communities: Baseline findings from the OPAL evaluation. Public health, 140, 196–205. https://doi.org/10.1016/j.puhe.2016.06.022.
Bennett, C., de Silva-Sanigorski, A., Nichols, M., Bell, A., & Swinburn, B. (2009). Assessing the intake of obesity-related foods and beverages in young children: Comparison of a simple population survey with 24 h-recall. International Journal of Behavioral Nutrition and Physical Activity, 6, 71. https://doi.org/10.1186/1479-5868-6-71.
Birch, L., Savage, J., & Ventura, A. (2007). Influences on the Development of Children’s Eating Behaviours: From Infancy to Adolescence. Canadian journal of dietetic practice and research: A publication of Dietitians of Canada = Revue canadienne de la pratique et de la recherche en dietetique : une publication des Dietetistes du Canada, 68(1), s1-s56.
Blanchette, L., & Brug, J. (2005). Determinants of fruit and vegetable consumption among 6–12-year-old children and effective interventions to increase consumption. Journal of Human Nutrition and Dietetics, 18(6), 431–443. https://doi.org/10.1111/j.1365-277X.2005.00648.x.
Borys, J., Le Bodo, Y., Jebb, S., Seidell, J., Summerbell, C., Richard, D., …, Swinburn, B. (2012). EPODE approach for childhood obesity prevention: Methods, progress and international development. Obesity Reviews, 13(4), 299–315. https://doi.org/10.1111/j.1467-789X.2011.00950.x.
Cole, T., Bellizzi, M., Flegal, K., & Dietz, W. (2000). Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ (Clinical Research ed.), 320(7244), 1240.
Crawford, D., Cleland, V., Timperio, A., Salmon, J., Andrianopoulos, N., Roberts, R., …, Ball, K. (2010). The longitudinal influence of home and neighbourhood environments on children’s body mass index and physical activity over 5 years: The CLAN study. International Journal of Obesity, 34(7), 1177–1187.
Department of Health. (2014a). Australia’s Physical Activity & Sedentary Behaviour Guidelines for Children (5–12 years). Canberra.
Department of Health. (2014b). Australia’s Physical Activity and Sedentary Behaviour Guidelines for Adults (18–64 years). Canberra.
Department of Health and Ageing, Australian Food and Grocery Council, & Department of Agriculture Fisheries and Forestry. (2007). Australian national children’s nutrition and physical activity survey, Canberra.
Dermody, S. S., Wright, A. G. C., Cheong, J., Miller, K. G., Muldoon, M. F., Flory, J. D., …, Manuck, S. B. (2015). Personality Correlates of Midlife Cardiometabolic Risk: The explanatory role of higher-order factors of the five-factor model. Journal of Personality. https://doi.org/10.1111/jopy.12216.
Ding, D., & Gebel, K. (2012). Built environment, physical activity, and obesity: What have we learned from reviewing the literature? Health & Place, 18(1), 100–105. https://doi.org/10.1016/j.healthplace.2011.08.021.
Field, A. E., Gillman, M. W., Rosner, B., Rockett, H. R., & Colditz, G. A. (2003). Association between fruit and vegetable intake and change in body mass index among a large sample of children and adolescents in the United States. International Journal of Obesity & Related Metabolic Disorders, 27(7), 821–826. https://doi.org/10.1038/sj.ijo.0802297.
Franckle, R., Adler, R., & Davison, K. (2014). Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: A systematic review. Preventing Chronic Disease, 11, E101. https://doi.org/10.5888/pcd11.130355.
Ho, N., Olds, T., Schranz, N., & Maher, C. (2017). Secular trends in the prevalence of childhood overweight and obesity across Australian states: A meta-analysis. Journal of Science and Medicine in Sport, 20(5), 480–488. https://doi.org/10.1016/j.jsams.2016.09.014.
Jago, R., Baranowski, T., Baranowski, J. C., Thompson, D., & Greaves, K. A. (2005). BMI from 3 to 6[thinsp]y of age is predicted by TV viewing and physical activity, not diet. International Journal of Obesity and Related Metabolic Disorders, 29(6), 557–564.
Jaime, P., & Lock, K. (2009). Do school based food and nutrition policies improve diet and reduce obesity? Preventive Medicine, 48(1), 45–53. https://doi.org/10.1016/j.ypmed.2008.10.018.
Klesges, R. C., Malott, J. M., Boschee, P. F., & Weber, J. M. (1986). The effects of parental influences on children’s food intake, physical activity, and relative weight. International Journal of Eating Disorders, 5(2), 335–345.
Kriemler, S., Meyer, U., Martin, E., van Sluijs, E., Andersen, L., & Martin, B. (2011). Effect of school-based interventions on physical activity and fitness in children and adolescents: A review of reviews and systematic update. British Journal of Sports Medicine, 45(11), https://doi.org/10.1136/bjsports-2011-090186.
Krølner, R., Due, P., Rasmussen, M., Damsgaard, M., Holstein, B., Klepp, K., & Lynch, J. (2009). Does school environment affect 11-year-olds’ fruit and vegetable intake in Denmark? Social Science & Medicine, 68(8), 1416–1424. https://doi.org/10.1016/j.socscimed.2009.01.022.
Leslie, E., Magarey, A., Olds, T., Ratcliffe, J., Jones, M., & Cobiac, L. (2015). Community-based obesity prevention in Australia: Background, methods and recruitment outcomes for the evaluation of the effectiveness of OPAL (Obesity Prevention and Lifestyle). Advances in Pediatric Research. https://doi.org/10.12715/apr.2015.2.23.
Moore, L., Gao, D., Bradlee, M., Cupples, L., Sundarajan-Ramamurti, A., Proctor, M.,,…, Ellison, R. (2003). Does early physical activity predict body fat change throughout childhood? Preventive Medicine, 37(1), 10–17.
Mullan, K. (2013). The Longitudinal Study of Australian Children (LSAC) Annual Statistical Report 2013: Time use and children’s social and emotional wellbeing and temperament. Retrieved from http://www.growingupinaustralia.gov.au/pubs/asr/2013/ch4asr2013.pdf.
National Health and Medical Research Council. (2013). Eat for health: Australian dietary guidelines Canberra, A.C.T: National Health and Medical Research Council.
Nixon, C., Moore, H., Douthwaite, W., Gibson, E., Vogele, C., Kreichauf, S., … ,Summerbell, C. (2012). Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4-6-year-olds: A systematic review. Obesity Reviews, 13(Suppl 1), 106–117. https://doi.org/10.1111/j.1467-789X.2011.00962.x.
Roberts, C., Freeman, J., Samdal, O., Schnohr, C., de Looze, M., Gabhainn, N. S., …, Rasmussen, M. (2009). The Health Behaviour in School-aged Children (HBSC) study: Methodological developments and current tensions. International Journal of Public Health, 54(2), 140–150. https://doi.org/10.1007/s00038-009-5405-9.
Slater, A., Bowen, J., Corsini, N., Gardner, C., Golley, R., & Noakes, M. (2010). Understanding parent concerns about children’s diet, activity and weight status: An important step towards effective obesity prevention interventions. Public Health Nutrition, 13(08), 1221–1228. https://doi.org/10.1017/S1368980009992096. doi.
Stewart, A., Marfell-Jones, M., Olds, T., & De Ridder, J. (2011). International Standards for Anthropometric Assessment. New Zealand: Lower Hutt.
Swinburn, B., Egger, G., & Raza, F. (1999). Dissecting obesogenic environments: The development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine, 29(6), 563–570. https://doi.org/10.1006/pmed.1999.0585.
Trost, S., Sirard, J., Dowda, M., Pfeiffer, K., & Pate, R. (2003). Physical activity in overweight and nonoverweight preschool children. International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity, 27(7), 834–839.
van Sluijs, E., McMinn, A., & Griffin, S. (2007). Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ: British Medical Journal, 335(7622), 703–703. https://doi.org/10.1136/bmj.39320.843947.BE.
Ventura, A., & Birch, L. (2008). Does parenting affect children’s eating and weight status? The International Journal of Behavioral Nutrition and Physical Activity, 5, 15–15. https://doi.org/10.1186/1479-5868-5-15.
Waters, E., de Silva-Sanigorski, A., Hall, B., Brown, T., Campbell, K., Gao, Y., …, Summerbell, C. (2011). Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews, 12, CD001871. https://doi.org/10.1002/14651858.CD001871.pub3.
Wilson, A., Magarey, A., & Mastersson, N. (2013). Reliability of questionnaires to assess the healthy eating and activity environment of a child’s home and school. Journal of Obesity, 2013, 720368. https://doi.org/10.1155/2013/720368.
World Health Organization. (2004). Global strategy on diet, physical activity and health. France.
World Health Organization. (2009). School policy framework: Implementation of the WHO global strategy on diet. Physical Activity and Health, 9, 557–564.
Wyse, R., Wolfenden, L., & Bisquera, A. (2015). Characteristics of the home food environment that mediate immediate and sustained increases in child fruit and vegetable consumption: Mediation analysis from the Healthy Habits cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 1–9. https://doi.org/10.1186/s12966-015-0281-6.
Acknowledgements
We thank the schools and families for their participation in the OPAL program, the OPAL Evaluation team for their contribution to the project and SA Health for allowing Flinders University use of the OPAL data. SU formulated the research question and designed the study. SU and JH analysed the data, and JH drafted the manuscript as part of her Honours project. SU, AM and LB provided academic supervision and support in all aspects of the study analysis and writing. EL provided support in the study writing and reviewed the manuscript. All five authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Haddad, J., Ullah, S., Bell, L. et al. The Influence of Home and School Environments on Children’s Diet and Physical Activity, and Body Mass Index: A Structural Equation Modelling Approach. Matern Child Health J 22, 364–375 (2018). https://doi.org/10.1007/s10995-017-2386-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-017-2386-9