Abstract
Objectives This study seeks to further the work exploring adverse childhood experiences (ACEs) by proposing a novel approach to understanding the impact of ACEs through applying advanced analytical methods to examine whether combinations of ACEs differentially impact child health outcomes. Methods Using National Survey of Children’s Health data, we use latent class analysis to estimate associations between classes of ACEs and child health outcomes. Results Class membership predicts child poor health, with differences found for specific ACE combinations. A subgroup of children exposed to poverty and parental mental illness are at higher risk for special healthcare needs than all other groups, including children exposed to 3 or more ACEs. Conclusions Different combinations of ACEs carry different risk for child health. Interventions tailored to specific ACEs and ACE combinations are likely to have a greater effect on improving child health. Our findings suggest children who experience specific ACE combinations (e.g., poverty and parental mental illness) are at particularly high risk for poor health outcomes. Therefore, clinicians should routinely assess for ACEs to identify children exposed to the most problematic ACE combinations; once identified, these children should be given priority for supportive interventions tailored to their specific ACE exposure and needs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
A substantial body of research has shown ACEs are detrimental to child health and negatively affect health outcomes in adulthood. Additionally, this research established that experiencing more than one ACE has a cumulative, negative effect on a variety of health outcomes. The current study extends this work by examining ACE combinations and their associations with child health. Through understanding the impact of ACE combinations, clinicians and practitioners in various disciplines can direct intervention and prevention strategies to address the specific ACEs reported and prioritize interventions for children who report the most-problematic combinations.
Introduction
Felitti et al. (1998) seminal study on adverse childhood experience (ACEs) was the first rigorous examination of the impact of traumatic events experienced during childhood on health status in adulthood. Among several groundbreaking findings, their study found ACEs were common among the general population. The survey respondents were largely White and middle class; more than half of the sample (N = 9508) reported exposure to at least one ACE category, and one-quarter reported exposure to two or more ACE categories. Additionally, Felitti et al. found a strong graded relationship between the extent of ACE exposure (i.e., number of ACE categories experienced) and negative health outcomes in adulthood ranging from heart disease to cancer to skeletal fractures. The findings from this study—known as the CDC-Kaiser ACE study—and the proliferation of studies that replicated and extended this work led to a wider understanding of the long-lasting effects of childhood experiences, profoundly impacting medicine, public health, and social work.
The majority of ACE research has taken a cumulative risk approach and continued to use an additive count measure in studies of ACEs and health (e.g., Anda et al. 1999; Dong et al. 2003, 2004; Dube et al. 2001; Ramiro et al. 2010). Such research has shown a strong link between the accumulation of ACEs and negative health outcomes, but has generally treated the different ACE categories as having equivalent health risks. When translating these findings to clinical settings, clinicians might find it helpful to know which ACE category a child experienced, from which the clinician can draw insights to tailor interventions to a patient’s needs. However, the existing research has not explored whether specific ACE categories represent different levels of risk or whether certain ACE combinations or “constellations” confer different outcomes. To help advance the translation of ACE research to practice, the present study proposes a new approach for understanding the impact of ACEs on child health outcomes.
ACEs and Health
The CDC-Kaiser ACE study included ten categories of adverse experiences: emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, witnessing violence against the mother, household member with mental illness, household substance abuse, parental separation/divorce, and household member with history of incarceration. The literature broadly supports the connection between ACEs and negative health outcomes. Exposure to four or more ACE categories was associated with significantly elevated risk levels for substance abuse, mental illness, sexually transmitted infections, cigarette smoking, and obesity in adulthood. Additionally, a significant graded relationship was found between the number of ACE categories a child experienced and serious illnesses in adulthood. Similarly, other researchers using data from the CDC-Kaiser ACE study have found a graded relationship between ACEs and other negative health outcomes, including paternity in teen pregnancy (Anda et al. 2002) and suicidality (Dube et al. 2001). Further, Dong et al. (2004) showed exposure to one ACE category significantly increased the likelihood of exposure to additional ACE types. Researchers using adapted versions of the ACE questionnaire have reported finding similar graded relationships between the extent of ACE exposure and multiple health risks (Ramiro et al. 2010).
Cumulative Risk
Across disciplines, researchers have asserted hypotheses related to the accumulation of risk and its negative impact on a variety of outcomes (for a review of cumulative risk factor exposure and child development, see Evans et al. 2013). Numerous studies have detected a linear relationship such that each additional risk factor (e.g., child maltreatment, parental domestic violence) worsens child outcomes (e.g., behavior; Appleyard et al. 2005; Rutter 1979; Sameroff 2000). This hypothesis appears to hold for the connection between ACEs and negative adult health outcomes given the evidence of graded relationships described above.
This epidemiologic research has limitations when translated to clinical settings, particularly in guiding work with trauma-exposed children. When clinicians lack knowledge about how ACE combinations differentially affect health outcomes, they are limited to a “one size fits all” approach when providing services. This approach assumes all individuals exposed to a given number of ACEs will receive equal benefit from a given intervention regardless of the distinct nature of the trauma experienced. Examining the impact of ACE combinations on health outcomes holds promise toward enabling clinicians to provide interventions tailored to individual needs.
Alternate Approaches to Understanding ACEs
Although much of the existing ACE research has examined the cumulative effect of exposure to multiple ACEs, a sizable number of studies have investigated the associations of separate ACEs with health outcomes. Studies have found that each ACE was independently associated with self-reports of poor health outcomes, including adolescent and adult smoking behavior (Anda et al. 1999; Font and Maguire-Jack 2016), suicidality (Dube et al. 2001), depression, binge drinking, obesity, and self-reported health status (Font and Maguire-Jack 2016). However, Dietz et al. (1999) found unintended pregnancy in adulthood was associated with only three of the original ACE categories: emotional and physical abuse, and witnessing domestic violence. A study using a variation of the original ACE categories found physical and sexual abuse, witnessing parental marital conflict, parental psychopathology, poor parent–child relationship, and low parental education attainment were individually associated with adult self-reports of overall poor health, pain, and high rates of healthcare use (Chartier et al. 2010).
Understanding the impact of individual ACEs is essential for targeted screening and for informing the selection of interventions for patients. Equally important, given that exposure to one ACE significantly increases the likelihood of experiencing at least one more ACE (Dong et al. 2004), clinicians must also understand the impact of ACEs in various combinations. However, no available studies have examined the impact of ACE combinations on child health outcomes.
ACEs in Practice Settings
As dissemination of the findings from the CDC-Kaiser ACE study has continued, the study questionnaire (or variations) has been used with increasing frequency in population health and clinical settings. Many states now include ACE questions in their Behavioral Risk-Factor Surveillance System surveys (see Bynum et al. 2010), allowing states to systematically track ACE prevalence over time, and providing researchers with new data to explore the connections between ACEs and health outcomes. Additionally, many studies have called for universal ACE screening to guide clinical interventions (e.g., Injury Prevention Center n.d.; Wisconsin Children’s Trust (2014). Although the ACE questionnaire has potential as a useful clinical tool, a summary ACE score alone is insufficient to guide intervention efforts; clinicians must also understand the impact of ACEs separately and in specific combinations to fully understand the effect of ACEs on health.
Current Study
The current study sought to extend the prior work on ACEs in two important ways. First, using latent class analysis, we provide an alternative measure of the prevalence of unobserved subgroups of ACEs. Second, we intentionally focused on the association of these combinations of ACEs on childhood health outcomes. By understanding the differential impact of ACE combinations, professionals can tailor intervention strategies to address exposure to specific ACEs. Despite a large body of research on the impact of ACEs on adult health, only limited information is available on the more-immediate impact of ACEs on child health. We sought to address this critical gap because understanding how child health outcomes are effected by ACE exposure is essential for enhancing intervention and prevention strategies that aim to improve child health outcomes.
Methods
This study had two methodological aims. The first aim, was to use latent class analysis (LCA) to examine whether children could be grouped into unobserved subpopulations (latent classes) based on each child’s observed (i.e., reported) ACEs. Given that numerous prior studies have found strong correlations between individual ACEs, we hypothesized that unobserved latent classes of ACE clusters would exist in this sample. As an exploratory LCA, we had no specific hypotheses regarding the number of classes or class membership profiles. The second aim was, once we specified a LCA model, to assess predictive validity of class membership by examining the association between latent classes and child health outcomes using regression models. Since classes emerged through the first study aim, we had no specific a priori hypotheses regarding the relationship between classes and health outcomes.
Data and Measures
Survey Data
Data were obtained from the 2011/2012 National Survey of Children’s Health (NSCH), which was conducted by the National Center for Health Statistics State and Local Area Integrated Telephone Survey program (Centers for Disease Control and Prevention 2013). The NSCH was designed to assess the physical and emotional health of children (0–17 years) and identify factors related to child well-being. Survey respondents were parents or guardians, who provided responses for one child in their household randomly chosen as the survey subject. The NSCH is a cross-sectional telephone survey using random-digital-dial for both landline (list-assisted) and cell-phone (independent) numbers. Surveys were administered from July 2011 through January 2012. Sampling weights adjust for nonresponse and unequal selection bias. Using weighted data, national and state-specific results are representative of all noninstitutionalized children. The NSCH screened 847,881 households for eligibility. Of these households, 187,422 reported age-eligible children in the home, and 95,677 of households completed the survey in one of six languages (about 1800 per state).
Variable Selection Approach
There were three types of variables used in this study: predictors of class membership (child/parent characteristics and other sociodemographic variables); measures of class membership (the ACEs); and outcomes of class membership (child health outcomes). The predictors of class membership are identified in Table 1 to describe the NSCH sample. The NSCH asks about nine ACEs, which we use as measures of class membership: extreme economic hardship, parental divorce/separation, parental incarceration, witness to domestic violence in the home, victim/witness of neighborhood violence, lived with anyone with a drug or alcohol problem, lived with anyone with a mental illness or was suicidal, parent/guardian death, and treated unfairly due to race/ethnic group (discrimination). Dichotomous yes/no responses are used to measure each ACE with two exceptions: responses for economic hardship and discrimination were first measured using 4-point scale (very often, somewhat often, rarely, never) and then dichotomized (yes/no). Although similar to the CDC-Kaiser ACE questionnaire, the NSCH survey differs in two ways: the NSCH added a question on racial discrimination and did not assess child abuse and neglect. The survey first introduces this module by stating “I’d like to ask you some questions about events that have happened during [subject child’s] life.” The items also state either “Since [subject child] was born…” or “Did [subject child] ever…” indicating that these items were meant to assess lifetime ACE exposure.
Prior studies using NSCH data have consistently found a link between ACE exposure and childhood health status (Bethell et al. 2014; Moore and Ramirez 2016; Slopen et al. 2016). The present study used three measures of childhood health as outcomes of class membership: general health status, special healthcare need, and chronic health condition. The first measure asked parents to use a 5-point scale (poor to excellent) to describe their child’s health; we combined responses to create a dichotomous general health status variable (fair/poor vs. good/very good/excellent). The second measure, special healthcare needs, was included in NSCH as a screener to assess use of health services for physical, emotional, and behavioral health needs. Last, the NSCH asked whether a healthcare provider had diagnosed the child as having one or more chronic physical health conditions (e.g., asthma, diabetes, cerebral palsy) or behavioral health conditions (e.g., depression, anxiety, learning disability). We created a dichotomous chronic condition variable to identify the presence of diagnosed conditions.
Analysis
Aim 1 Analysis: Latent Class Analysis
The first step in the LCA was to fit the ACEs data to a series of models specified with increasing numbers of latent classes using Mplus 7.4 (Muthén and Muthén 1998–2012). Next, we used a model selection process to identify the model with the best fit to the data. Models were compared using Akaike’s information criterion, Bayesian information criterion (BIC), sample-size adjusted BIC, model interpretability, and the accuracy of classification using the entropy value. We followed Nylund et al. (2007) recommendation that the BIC is the best empirical justification for number of classes. Although the bootstrap likelihood ratio test (BLRT) would have been ideal to assess the improvement in model fit, this test is not available for complex survey designs, such as the NSCH.
A unique consideration of our LCA analysis was the approach used to handle the 54% of the sample that reported zero ACEs. This no ACEs group did not represent a latent class because the respondents had not experienced any ACEs; however, we chose to keep these observations in the sample to maintain the structure of the complex survey design and to preserve the no ACEs group for use as the reference group in the subsequent regression analyses.
Aim 2 Analysis: Multivariate Regression to Assess Predictive Validity
Following the LCA, we used the posterior probabilities of class membership to assign a class membership to each respondent. We then conducted a series of regression analyses with three child health outcomes as the dependent variable: reported child poor health, special healthcare need, and chronic health condition. Each health outcome was regressed on the latent class as an independent variable. For comparison purposes, each health outcome was also regressed on the cumulative ACE score as an independent variable, yielding a total of six regression models. The models were adjusted to control for a set of nine covariates, including the child’s race, age, gender, premature birth; family income (above or below the federal poverty line); number of children in the home; family structure; and the mother’s education and health status. The purpose of this modeling approach was to determine whether ACE latent class membership was associated with child health outcomes. Further, this side-by-side model comparison helps assess the utility of these two different approaches to analyzing the association between ACEs and child health.
Results
Sample Characteristics
Descriptive statistics for the weighted sample are presented in Table 1. As a nationally representative study, the demographic profile of the NSCH sample is reflective of the U.S. population of noninstitutionalized children. The average age of study children was 8.6 years (range: 0–18 years). The majority of the sample was White (53%), with large proportions of Hispanic (24%) and Black (14%) children. Most children lived in a home with two parents (biological or adoptive; 66%) and more than 76% of children had at least one sibling in the home. Although most mothers reported educational attainment beyond a high-school diploma (64%), an estimated 22% of the children lived below the federal poverty line.
The prevalence of ACEs in the NSCH sample has been reported in detail elsewhere (e.g., Bethell et al. 2014; Moore and Ramirez 2016; Slopen et al. 2016). To summarize, more than half of the children in the sample had zero ACEs (52%) or reported only one ACE (25%). The most prevalent type of ACE was financial hardship (21%) whereas the least prevalent was parental death (5%).
Aims 1 Results: Latent Class Analysis Results
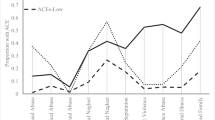
We measured class membership using seven of nine ACE indicators. Two indicators (parent/guardian death and discrimination) did not meaningfully differentiate latent classes, so we removed these indicators to improve model parsimony and interpretation. We assessed model fit for 2-class through 10-class models. Fit statistics for class comparison indicated the 7-class solution had the best model fit (see Table 2). The BIC was lowest for the 7-class model; prior studies indicate the BIC is the best indicator of fit for this type of analysis (Nylund et al. 2007). Class interpretability was also seen in the 7-class model, and this model’s entropy score (0.71) indicated greater precision in class prediction than either the 6-class or 8-class model. Figure 1 displays the proportion of each measure of class membership (ACE) in each class identified.
The final model contained seven classes: Class 1—0–1 ACE (76%); Class 2—1–2 ACEs (11%); Class 3—Domestic violence, no mental illness (3%); Class 4—Mental illness and poverty (1%); Class 5—Substance use and incarceration (2%); Class 6–Substance use, no incarceration (4%); and Class 7—High ACEs (≥ 3 ACEs; 2%).
Child and parent characteristics for each class are presented in Table 2. All characteristics were significantly associated (p < .05) with class membership, with the exception of child gender and premature birth. Children in Classes 1, 2, 4, and 7 tended to be older than the sample mean and other latent classes. Children in Class 1 (0–1 ACE) were the youngest group by 2 years. Compared with other race/ethnicities, Whites were overrepresented in Class 6 (substance use, no incarceration; 66%). Similarly, Hispanics were overrepresented in Class 3 (domestic violence, no mental illness; 35%). All groups except Class 1 (0–1 ACE) and Class 6 (substance use, no incarceration) were more likely to report living below the federal poverty line. Generally, the number of children in the home did not vary between classes; however, 23% of the total sample reported being the only child in the home, whereas only 2% of Class 7 (High ACEs) reported only child status. More than three-quarters of Class 1 reported living in a two-parent home (77%), with all other classes less likely to live in a two-parent home; notably, only 14% of Class 7 (High ACEs) reported living in a two-parent home (χ2 = 17.2, p < .001). Mothers in Class 4 (mental illness, poverty) reported the worst health, with 37% of these mothers indicating poor health.
Aim 2 Results: Multivariate Regression Results
When controlling for covariates, the cumulative number of ACEs was a significant predictor of the three health indicators: child poor health status, special healthcare need, and chronic health condition (p < .001; see Table 3). We then examined the association of the health indicators with the latent classes, using Class 1 (0–1 ACE) as the reference group (see Table 4). The indicators were predicted at varying levels dependent on class membership. A significant increased risk of parent-reported poor child health (p < .05) was found for children in Class 7 (High ACEs), Class 2 (1–2 ACEs), and Class 4 (mental illness, poverty). As compared with the reference group (Class 1, 0–1 ACE), all other classes had an increased risk of experiencing a chronic health condition (p < .05). Similarly, with the exception of Class 3 (domestic violence, no mental illness) all classes had elevated risk for special healthcare needs (p < .05), with the highest risk found for children in Class 4 (mental illness, poverty; p < .001; adjusted odds ratio [AOR] 3.10), and a slightly higher effect than Class 7 (High ACEs; AOR = 2.95).
Post-hoc Sensitivity Analysis
We selected 7-class solution because of the low BIC, face validity, class interpretability, and predictive validity in the regression models. We also explored other class solutions to assess the implications of alternative model selection. The 4-class solution also had support based on the Lo-Mendell-Rubin (LMR) test. The 4-class solution was similar to the 7-class solution in that there were 0–1 ACE and High ACEs classes that were very similar to the low and high ACE classes identified in the 7-class solution. The other two classes in the 4-class solution had moderate levels of ACEs and were characterized as either having mainly clusters of family-level ACEs (e.g., substance use, mental illness) or community-level ACEs (e.g., discrimination, poverty). Similar to the 7-class solution, the 4-class solution had similar results in predicting child health outcomes. That is, the High ACEs class had the worse health outcomes, but the combination of ACEs in the moderate ACE classes had different impacts on child health. Similar patterns were identified for the 5-class and 6-class models.
In addition to the empirical justification, the 7-class model is also further justified by reflecting more of the nuances of the variation in the moderate ACE clusters. In the 4-class solution, the two moderate-ACE classes were distinguished largely by parental substance use. Alternatively, in the 7-class solution, Class 5 (Substance use and incarceration) and Class 6 (Substance use, no incarceration) were differentiated, in terms of ACE profile, primarily in whether the parent was also incarcerated. Knowing whether a child experiences parental substance use alone, or in combination with incarceration, is likely a meaningful distinction in terms of the experience of the child, the impact on well-being, and intervention strategies. Taken together, these findings indicate that although the 7-class solution was the best fit for this data, the broader implication is that regardless of the number of classes, the combination of ACEs matters.
Discussion
Felitti et al. (1998) innovative work created a new understanding of the importance of childhood experiences on physical and behavioral health. The acknowledgment that trauma experienced during childhood can have lifelong consequences has shifted conversations among scholars in many fields. Findings from the CDC-Kaiser ACE study have also changed clinical practice, with many clinics and hospitals now including an ACE assessment in their clinical protocol. The current study advances this conversation as it examined whether various ACE combinations have differential impacts on health outcomes by using person-centered analyses. Our study identified that while exposure to a high number of ACEs was associated with poor health outcomes, certain combinations of ACEs are associated with more deleterious outcomes than other combinations. This finding provides a better understanding of which ACE combinations present greater risks to health and has the potential to inform the selection and tailoring of clinical interventions for individuals.
Considerable research has shown the cumulative effects of ACE exposure are detrimental to health outcomes (Felitti et al. 1998; Anda et al. 2002; Dube et al. 2001; Dong et al. 2003). The research indicates ACE exposure increases likelihood of negative health outcomes, and that exposure to more categories of ACEs increases the negative effects on health (Felitti et al. 1998). Our study not only supports these prior findings but also found class membership predicted child health outcomes of interest (child poor health, special healthcare need, and chronic health condition) with varying risk. This finding demonstrates an important connection between ACE combinations and differential effects on health; this information has not been available from studies that used a simple, continuous ACE measure. Our findings suggest that it is not only the number of ACEs that is related to health outcomes, but specific combinations of ACEs can be important when comparing individuals with moderate levels of ACEs.
The study identified several important distinctions between latent group membership related to health outcomes. For example, as compared with children who reported 1 or no ACE, we found a significantly greater likelihood for poor health among children who reported high ACEs (≥ 3 ACEs), moderate ACEs (1–2 ACEs), or the combination of mental illness and poverty ACEs. This finding indicates that the combination of caregiver mental illness and poverty has similar association to poor health as having three or more ACEs. Additionally, although most classes had an increased risk of experiencing a special healthcare need, we found children exposed to domestic violence but not mental illness (Class 3) were not at an increased risk for poor health as compared to Class 1 (0–1 ACE). Last, a finding that further emphasizes the differential health risk of class groups was that the class exposed to ACEs of mental illness and poverty (Class 4) had the highest risk of experiencing a special healthcare need—an effect higher than even that of the high ACE class. This last finding is especially important because the extant research suggested that children with multiple ACE exposures were most at risk; however, our work suggests that important qualitative differences exist in these childhood experiences depending on the types and combination of ACEs. Overall, these findings have important clinical implications given that the prior research suggests directing more intensive interventions to highest ACE groups; in contrast, the findings of the current study may suggest triaging intensive interventions to children who experience a combination of poverty and a parent with mental illness, regardless of additional ACE exposure.
Important socioeconomic differences (race, income, and maternal education) appear to correspond with class membership, suggesting the likelihood of group differences beyond the differing experiences of ACEs. For example, as compared with nearly a quarter of the NSCH sample who reported being the only child in the home, only a very small proportion of children in the high ACE class reported only child status (2%). Additionally, children in the referent class (0–1 ACE) were significantly more likely than all other classes to report living in a two-parent home. These findings highlight the nuanced pattern of ACE indicators that would be unavailable in a cumulative index.
Our study supports prior findings that the cumulative index of ACEs was highly predictive of all studied child health outcomes. Cumulative risk is an important phenomenon that holds across numerous populations, including a nationally representative sample of children. Screening for ACEs is a quick and accessible way to identify children who may be at greatest risk for poor health outcomes. Indeed, understanding a child’s ACE score provides clinicians an easy metric for targeting prevention and intervention. However, a count number of ACEs provides little information regarding how best to intervene. For example, an ACE score of three likely does not provide enough useful information for a clinician to suggest or select an appropriate evidence-informed intervention. Knowing not only the count of ACEs but understanding the compilation of ACEs is needed for both intervention development and deployment. As this study identified the combination of caregiver mental illness and poverty as particularly impactful on child health, it would be helpful for a clinician to know these specific ACE indicators to select an evidence-informed intervention to address caregiver mental health. Future research may identify that specific interventions are more effective in reducing child health problems for different groupings of ACE indicators. Understanding ACE constellations can help clinicians select appropriate and effective interventions for the individual child and family needs.
These findings should be considered in light of several limitations. First, as a cross-sectional study, it is not possible to determine the true causal order of ACEs and health status. However, since the NSCH asks about lifetime ACE exposure and current health status, there is some indication that temporality is implied such that ACEs preceded the measured health outcomes. Nevertheless, temporality is a necessary but not sufficient condition for establishing causality, and we have been careful not to suggest that these findings are causal. Second, binary variables may hide further nuance in the experience of ACEs in terms of frequency or developmental timing of the adverse experience. Last, the latent class memberships were based on posterior probabilities, and assigning children to their highest probability class may increase associations and attenuate standard errors.
Conclusions for Practice
The current study suggests that LCA is a helpful method for teasing out the pathways by which ACE exposure negatively affects health outcomes. Cumulative number of ACEs is a useful measure to identify and triage patient populations based on a broad dimension of risk. However, as greater numbers of clinicians begin to routinely assess ACEs, it will be essential to pinpoint specific interventions for patients presenting with exposure to specific ACEs or combinations of ACEs. Identifying the classes at elevated risk for poor outcomes can help guide the selection of interventions to improve population health.
References
Anda, R. F., Chapman, D. P., Felitti, V. J., Edwards, V., Williamson, D. F., Croft, J. B., & Giles, W. H. (2002). Adverse childhood experiences and risk of paternity in teen pregnancy. Obstetrics & Gynecology, 100(1), 37–45. doi:10.1097/00006250-200207000-00007.
Anda, R. F., Croft, J. B., Felitti, V. J., Nordenberg, D., Giles, W. H., Williamson, D. F., & Giovino, G. A. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA: The Journal of the American Medical Association, 282, 1652–1658. doi:10.1001/jama.282.17.1652.
Appleyard, K., Egeland, B., van Dulmen, M., & Sroufe, L. A. (2005). When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry, 46, 235–245. doi:10.1111/j.1469-7610.2004.00351.x.
Bethell, C. D., Newacheck, P., Hawes, E., & Halfon, N. (2014). Adverse childhood experiences: Assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs, 33, 2106–2115. doi:10.1377/hlthaff.2014.0914.
Bynum, L., Griffin, T., Riding, D. L., Wynkoop, K. S., Anda, R. F., Edwards, V. J., … Croft, J. B. (2010). Adverse childhood experiences reported by adults—five states, 2009. Morbidity and Mortality Weekly Report, 59, 1609–1613. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5949a1.htm.
Center, Injury Prevention, Phoenix Children’s Hospital. (n.d.). Overcoming adverse childhood experiences: Creating hope for a healthier Arizona. Retrieved from http://childhealthdata.org/docs/drc/arizona-aces-efinal.pdf?Status=Master.
Centers for Disease Control and Prevention. (2013). National Survey of Children’s Health. Retrieved from https://www.cdc.gov/nchs/slaits/nsch.htm.
Chartier, M., Walker, J., & Naimar, B. (2010). Separate and cumulate effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse & Neglect, 34, 454–464. doi:10.1016/j.chiabu.2009.09.020.
Dietz, P. M., Spitz, A. M., Anda, R. F., Williamson, D. F., McMahon, P. M., Santelli, J. S., … Kendrick, J. S. (1999). Unintended pregnancy among adult women exposed to abuse or household dysfunction during their childhood. JAMA: The Journal of the American Medical Association, 282, 1359–1364. doi:10.1001/jama.282.14.1359.
Dong, M., Anda, R. F., Dube, S., Giles, W., & Felitti, V. J. (2003). The relationship of exposure to childhood sexual abuse to other forms of abuse, neglect, and household dysfunction during childhood. Child Abuse & Neglect, 27, 625–639. doi:10.1016/S0145-2134(03)00105-4.
Dong, M., Anda, R. F., Felitti, V. J., Dube, S. R., Williamson, D. F., Thompson, T. J., … Giles, W. H. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28, 771–784. doi:10.1016/j.chiabu.2004.01.008.
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA: The Journal of the American Medical Association, 286, 3089–3096. doi:10.1001/jama.286.24.3089.
Evans, G. W., Li, D., & Whipple, S. S. (2013). Cumulative risk and child development. Psychological Bulletin, 139, 1342–1396. doi:10.1037/a0031808.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. doi:10.1016/S0749-3797(98)00017-8.
Font, S. A., & Maguire-Jack, K. (2016). Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse & Neglect, 51, 390–399. doi:10.1016/j.chiabu.2015.05.013.
Moore, K. A., & Ramirez, A. N. (2016). Adverse childhood experience and adolescent well-being: Do protective factors matter? Child Indicators Research, 9(2), 299–316. doi:10.1007/s12187-015-9324-4.
Muthén, L. K., & Muthén, B. O. (1998–2012). Mplus user’s guide (7th edn.). Los Angeles, CA: Muthén&Muthén
Nylund, K. L., Asparouhov, T., & Muthén, B. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14, 535–569. doi:10.1080/10705510701575396.
Ramiro, L., Madrid, B., & Brown, D. (2010). Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse & Neglect, 34, 842–855. doi:10.1016/j.chiabu.2010.02.012.
Rutter, M. (1979). Protective factors in children’s responses to stress and disadvantage. In M. W. Kent & J. E. Rolf (Eds.), Primary prevention of psychopathology. Vol.3: Social competence in children (pp. 49–74). Hanover, NH: University of New England Press.
Sameroff, A. J. (2000). Dialectical processes in developmental psychopathology. In A. Sameroff, M. Lewis & S. Miller (Eds.), Handbook of developmental psychopathology (2nd edn., pp. 23–40). New York, NY: Kluwer Academic/Plenum. doi:10.1007/978-1-4615-4163-9_2.
Slopen, N., Shonkoff, J. P., Albert, M. A., Yoshikawa, H., Jacobs, A., Stoltz, R., & Williams, D. R. (2016). Racial disparities in child adversity in the US: Interactions with family immigration history and income. American Journal of Preventive Medicine, 50(1), 47–56. doi: 10.1016/j.amepre.2015.06.013.
Wisconsin Children’s Trust Fund. (2014). Wisconsin ACE brief: 2011 and 2012 data. Retrieved from https://preventionboard.wi.gov/Pages/OurWork/Publications.aspx.
Acknowledgements
The authors would like to thank Diane Wyant from the University of North Carolina at Chapel Hill for her support in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lanier, P., Maguire-Jack, K., Lombardi, B. et al. Adverse Childhood Experiences and Child Health Outcomes: Comparing Cumulative Risk and Latent Class Approaches. Matern Child Health J 22, 288–297 (2018). https://doi.org/10.1007/s10995-017-2365-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-017-2365-1