Abstract
Objectives To improve clinical practice and increase postpartum visit Type 2 diabetes mellitus (T2DM) screening rates in women with a history of gestational diabetes mellitus (GDM). Methods We recruited clinical sites with at least half of pregnant patients enrolled in Medicaid to participate in an 18-month quality improvement (QI) project. To support clinical practice changes, we developed provider and patient toolkits with educational and clinical practice resources. Clinical subject-matter experts facilitated a learning network to train sites and promote discussion and learning among sites. Sites submitted data from patient chart reviews monthly for key measures that we used to provide rapid-cycle feedback. Providers were surveyed at completion regarding toolkit usefulness and satisfaction. Results Of fifteen practices recruited, twelve remained actively engaged. We disseminated more than 70 provider and 2345 patient toolkits. Documented delivery of patient education improved for timely GDM prenatal screening, reduction of future T2DM risk, smoking cessation, and family planning. Sites reported toolkits were useful and easy to use. Of women for whom postpartum data were available, 67 % had a documented postpartum visit and 33 % had a postpartum T2DM screen. Lack of information sharing between prenatal and postpartum care providers was are barriers to provision and documentation of care. Conclusions for Practice QI and toolkit resources may improve the quality of prenatal education. However, postpartum care did not reach optimal levels. Future work should focus on strategies to support coordination of care between obstetrical and primary care providers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Up to 70 % of women with gestational diabetes will develop Type 2 diabetes mellitus (T2DM). Postpartum and lifelong screening is recomended for timely identification of T2DM among women with a history of GDM. Low post-partum visit rates represent missed opportunities for screening for T2DM, providing prevention messages, and referral to early treatment. This project used quality improvement principles to improve clinic practices and rates of both postpartum visits and T2DM screening.
Purpose
In the United States, approximately 28 million persons have diabetes—triple the number from 3 decades ago—of whom 13.4 million are women (CDC 2014). An estimated 30 % of these women previously had gestational diabetes mellitus (GDM) (Cheung 2003), which is characterized by abnormal carbohydrate metabolism first identified in pregnancy (ACOG 2013). GDM affects up to 9.2 % of pregnancies (DeSisto 2015) with increasing prevalence (Bardenheier 2015). While GDM typically resolves after pregnancy, women with a history of GDM remain at high risk for developing type 2 diabetes mellitus (T2DM). The highest risk period for T2DM incidence among these women is immediately postpartum (Feig 2008), with incidence estimated to be 3–24 % in the first year postpartum and up to 50 % in the first 5 years (Bellamy 2009). Overall, between 50 and 70 % of women with GDM develop T2DM at some point in life (ACOG 2013), making lifelong monitoring critical to adequately capturing the risk of diabetes.
Both the American Diabetes Association (ADA) (ADA 2013) and American College of Obstetricians and Gynecologists (ACOG) (ACOG 2013) guidelines recommend that women with a history of GDM have a postpartum visit and be screened for persistent hyperglycemia and/or T2DM 6–12 weeks after delivery and subsequently, every 1–3 years. Lifelong screening enables ongoing prevention messaging, timely diagnosis of pre-diabetes and T2DM, and referral for early treatment. T2DM development in women with GDM history can prevented or delayed by lifestyle modifications and breastfeeding (Ratner 2008; Gunderson 2015). Despite this, reported postpartum screening rates are sub-optimal, ranging from 20 to 60 % (Yarrington 2015). Screening is lower among women who are low income and who have more severe GDM (Hunt 2008). Providers often lack knowledge of the extent of T2DM risk in women with GDM history (Rodgers 2014; Ko 2013a), and both women with GDM history and providers admit to not having adequate patient education materials and community resources to reduce risk (Rodgers 2014; Ko 2013a, b; Weber 2015). However, both prenatal and primary care providers (PCP) have expressed a desire for patient-centered materials and local community resources (Oza-Frank 2014).
The Ohio Gestational Diabetes Postpartum Care Learning Collaborative (referred to as the Collaborative in the remainder of this paper) was formed in January 2014 as a quality improvement initiative. The primary objectives of the intervention were to increase postpartum visit rates and postpartum T2DM screening rates among women following a GDM pregnancy. Secondary objectives were to educate women with GDM on T2DM risk and risk reduction methods. To support these objectives, toolkits were developed and tested. Patient toolkits were designed to increase the delivery of and expand the content of prenatal education. Provider toolkits were designed to improve clinical care and office work flow for timely GDM and postpartum T2DM screening. This paper describes the intervention and the observed impact on quality improvement indicators of care provision.
Description
The Social and Behavioral Sciences Institutional Review Board (IRB) at the Ohio State University determined this initiative to be a quality improvement activity that did not require IRB review. The work was conducted in accord with prevailing ethical principles.
The Collaborative consisted of clinical and public health subject matter experts, state health department leadership in both chronic disease and maternal and child health, quality improvement experts, and pilot site teams. To ensure consensus about root causes and effective strategies, all members of the Collaborative participated in development of a key driver diagram for the quality improvement project (Fig. 1). Key drivers included standardization of clinical guidelines in GDM management; increased access to maternal health services; coordination of care; and promotion of a culture of safety and improvement. A key driver of particular focus in this pilot was the increased awareness of risks and benefits of optimal management of GDM and risk reduction for T2DM among pregnant women, nurses, diabetes educators, office staff and obstetric care providers, both physicians and midwives.
Pilot Sites
We recruited clinical sites (N = 15) with at least half of pregnant patients enrolled in Medicaid, as the population had higher rates and was of interest to the state. Twelve sites remained engaged throughout the project period. Recruitment aimed for representation across size of annual GDM patient population (small: <200; medium: 200–500; and large: >500) and geography (Fig. 2). Recruited sites were suggested by public health or clinical subject matter experts or were known to the quality improvement experts from participation in prior projects. Each site team included at least one physician, nurse, and administrative staff member. Some teams also included a diabetes educator. Team sizes ranged from three to seven individuals but did not correlate with site size. All participation was voluntary; no financial incentives were offered.
Project Components
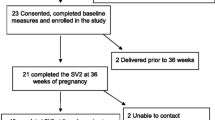
This 18-month project utilized three components: (1) development of educational and clinical care toolkits for providers and patients (see online Appendix), (2) rapid cycle data feedback to promote engagement and monitor progress, and (3) monthly learning sessions, facilitated by clinical subject-matter experts, to provide training on specific topics, answer questions, and facilitate discussion among pilot sites. The first 6 months were spent in development of the patient and provider toolkits and site recruitment. The next 12 months were spent engaged in data collection, learning sessions and quality improvement work itself (Fig. 3).
Toolkit Development and Evaluation
Provider and patient toolkits were developed to serve as resources to support clinical practice change and increase patient awareness of GDM. Toolkit development was informed by a literature review and state-specific data. State data sources included a data book with quantitative GDM-related data compiled from six sources (Oza-Frank 2011), quantitative data on provider knowledge and practices from a survey of obstetric and primary care providers (PCPs) (Oza-Frank 2014; Ko 2013a, b; Rodgers 2014) and qualitative data from focus groups with women with a history of GDM (Oza-Frank 2015; Weber 2015). Four frontline obstetrical providers, including maternal-fetal medicine physicians specializing in diabetes with pregnancy, a registered dietician/epidemiologist, and public health professionals contributed to the development of the provider toolkits. State public health experts compiled an inventory of state and local resources for T2DM risk reduction.
The provider toolkit was a three pocket folder with work sheets and tools for office flow and postpartum care, resources for GDM management, and general prenatal resources. The included patient care algorithms were adapted from ACOG (ACOG 2013). Two separate patient toolkits were single-ring bound 5 × 7 inch booklets. One patient booklet was intended for pregnant women considered at high-risk of developing GDM as defined by the presence of one or more of these risk factors: prior history of GDM, known impaired glucose metabolism, polycystic ovarian syndrome, body mass index greater than or equal to 30, or prior child with a birth weight greater than ten pounds. The booklet contained general prenatal care information including a broad overview of GDM and maintenance of a healthy lifestyle. The second patient toolkit was directed toward pregnant women with a GDM diagnosis and contained resources specific to GDM education and management during pregnancy, prevention of T2DM, and postpartum care. Patient booklets were written at a fourth to fifth grade reading level and made available in English and Spanish.
Feedback on the clinical toolkit and consumer resources were solicited from practice sites quarterly throughout this pilot. At project completion sites were asked to complete a 20-question toolkit survey (see online Appendix 2). The three sites with wireless capability administered a short questionnaire to a convenience sample of patients to determine patient satisfaction with their care and resources provided. Patients were asked if they had a diagnosis of GDM, whether they received the patient toolkit, and what they learned.
Quality Improvement Data Collection and Feedback Loops
The Model of Improvement (Langley 2009) championed by the Institute for Healthcare Improvement guided this project. This model uses rapid Plan-Do-Study-Act cycles to test a change or group of changes in selected measures on a small scale in a brief period of time, such as days rather than months. Observed improvements in key measures guide whether the tested change is adopted within clinics and expanded beyond test sites. If the change is unsuccessful, it is abandoned and another possible change is tested. Aggregate data allow sites to monitor progress relative to peers and to established targets. Thus, rapid feedback of site-specific and aggregate data is a key principle of quality improvement methods.
Quality improvement measures for this project are listed in Table 1. Sites performed monthly chart reviews to collect data on these measures. Each site was asked to review up to 20 charts for women between 33 and 36 weeks gestation with a GDM diagnosis who was treated that month. Reviewing this number of charts took approximately 2–3 h, which was a manageable commitment for most sites. When possible, sites were encouraged to select women eligible for or enrolled in Medicaid, or women who were uninsured. Additionally, for any woman whose chart had been reviewed during her prenatal period, postpartum data were collected on the following measures: (a) delivery date, (b) attendance at postpartum visit (yes or no), (c) date of postpartum visit, and (d) receipt of oral glucose tolerance test.
Data on quality improvement measures were entered directly into a secure, web-based data portal, developed on the SAS 9.3 Enterprise Business Intelligence (EBI) platform. No identifiable private health information was entered. Monthly, aggregate trend data were shared through monthly learning sessions and site-specific data through coaching calls. Sites could also access customizable reports on the portal.
Monthly Learning Sessions and Individual Coaching
The Collaborative was anchored by monthly learning sessions. Within a 1-hour webinar format, sessions included a discussion of toolkit resources, best practices for treating women diagnosed with GDM and a review of aggregate data on key quality improvement measures to identify areas for improvement to accelerate change. Quality improvement experts held up to four optional individual coaching calls with each project team quarterly to provide site-specific technical assistance. Calls focused on site-specific data and needs such as data entry and use of resources.
Results
Fifteen practices were recruited to participate; twelve remained actively engaged throughout the project period. Active engagement was defined as participating in the pre-work call, submitting at least 7 of 10 months of data collection, and participating in at least seven of ten technical assistance calls. For the three sites that discontinued participation, the primary reason was inability to commit time (3–5 h monthly) and resources. Nine of the sites participated in at least two of the four coaching calls, with seven participating in three or more calls.
More than seventy provider toolkits and 2345 patient toolkits (845 prenatal and 1500 GDM) were disseminated. Seventeen respondents (including obstetricians, nurse practitioners, nurses, and diabetes educators) from the twelve pilot sites completed the toolkit survey at project completion. All respondents reported the provider toolkit was easy or somewhat easy to use and that they would continue to use at least one toolkit resource after project completion. Most sites (92 %) responded that resources within the provider toolkit were helpful or very helpful when treating patients. Recommendations for toolkit improvements included a need for additional instruction on when to use each tool or handout and when to provide the education to the clients (e.g. specific weeks of gestation). Respondents also requested more emphasis on glucose testing postpartum, and the addition of guidance and resources to facilitate care coordination with PCPs postpartum.
All but one site reported that the patient toolkit resources were helpful in providing GDM-related education to patients, and they would likely continue utilizing the patient resources after project completion. Sites responded that patient resources were easy to use, included valuable information on educational topics such as blood sugar monitoring, the impact of the diagnosis on mom and baby, and the importance of postpartum screening. However, information gained qualitatively during coaching calls pointed to a preference for and perceived usefulness of the GDM booklet over the general prenatal booklet. This information was reinforced by distribution; some sites used only the GDM booklet and returned their prenatal booklet.
Within the three sites that surveyed patients there were 83 respondents. Among them, 91 % reported that the GDM resources provided were either helpful or very helpful. Among patients with a diagnosis of GDM, 99 % indicated they would attend their postpartum visit, with 87 % responding that they would probably or definitely receive an oral glucose tolerance test (OGTT) test to determine their risk for T2DM.
For the quality improvement measures, nine to ten submissions were received monthly from the twelve participating sites over 11 months of reporting measures. These submissions represented prenatal data on more than 700 women, of whom 259 were diagnosed with GDM and had delivery recorded by the end of the project. Aggregate baseline and follow up findings for all measures are displayed in Table 1. Figure 4 displays an example of a trend chart for the measure of receipt of prenatal education on the risk of T2DM.
For all indicators of prenatal education, baseline measures were between 90 and 100 % of reviewed charts. Prenatal nutrition and weight gain education measures were already achieving approximately 100 % completion at baseline, which was maintained throughout the project period. Education on breastfeeding and exercise was slightly over 90 % at baseline and 100 % at follow-up. Improvement was seen for the three education measures that had lower baseline rates. Among reviewed charts at baseline and at month eleven, rates of prenatal education on T2DM risk were 67 and 100 %; family planning use (including spacing births) were 63 and 86 %; and smoking cessation were 40 and 90 %. For the measure of timeliness of prenatal GDM screening, 87 % of reviewed charts at baseline indicated screening prior to 28 weeks gestation and 95 % at project completion. The measure of a scheduled follow-up appointment following GDM diagnosis did not have baseline data available, as the follow-up appointment was a new process for many sites. At project end, 59 % of reviewed charts indicated a scheduled 30-minute follow-up appointment within 4-weeks of GDM diagnosis. Of women with a delivery recorded, 69 % had a completed postpartum visit. Of women who returned for their postpartum visit, 40 % had a documented T2DM screen.
Recommendations for Future Practice
This paper describes an approach to improving care to prevent T2DM in a high-risk population through quality improvement methodology supported by provider and patient toolkits. The primary objectives of the initiative were to increase postpartum visits and postpartum T2DM screening in women following a GDM pregnancy. Secondary objectives were to increase patient education regarding T2DM and risk reduction methods. A complement of chart review data on quality improvement measures, records of site engagement, and surveys of practitoner and patient satisfaction supports the conclusion that this was a well-received initiative that improved delivery prenatal education and may have improved post-partum care receipt. Although numerous studies have identified major barriers to postpartum screening, we found few US studies (Ferrara 2012; Vesco 2012; Yarrington 2015) that have evaluated interventions to increase postpartum screening rates. Several were conducted within the same health maintenance organization, minimizing generalizability, and few used multimodal methods, a critical component for facilitating change in clinical practice. Strategies to date have relied either on the use of nurses for direct patient contact or on interventions utilizing the electronic medical record (Yarrington 2015).
Prior research has shown that resources to support clinical care for women with GDM both prenatally and postpartum are lacking and desired by practitioners (Oza-Frank 2014); that finding was supported by the Collaborative’s experience recruiting sites for participation in this initiative. We easily recruited sites as providers were eager to acquire tools to help them address this topic. This initiative appeared to meet at least some of that need as evidenced by high participation in the learning sessions, uptake of toolkits, and provider satisfaction with toolkits.
The Collaborative identified awareness of risks and benefits of optimal GDM management and risk reduction for T2DM as a key driver for improved postpartum care and improvements in education were a secondary objective of the initiative. Prenatal education on health behaviors and postpartum risks is believed to influence a woman’s behaviors and health care utilization postpartum (Hildebrand 2014; Hale 2014). Within participating sites measures of prenatal education on these topics appear to have improved. High rates of prenatal education on all topics were achieved at the end of the project period, based on chart review data reported on key measures. For some measures such as smoking cessation and family planning, the improvements appear to be large and may demonstrate potential for the use of quality improvement methods to address prenatal care.
The primary objective of this initiative was improvement of postpartum care. At project end, among women with GDM who had delivered 69 % had a record of a postpartum visit, slightly higher than rates of 20–60 % identified in recent studies (Yarrington 2015). However, rates remained suboptimal. Among the same women in this project, 40 % had a record of postpartum T2DM screening. While well within the wide range of published rates, it indicates a need for significant improvement beyond what was achieved in this pilot project.
Reasons for missed postpartum care are numerous and the content of toolkits and learning sessions attempted to address many of them. Participating sites expressed particular frustration and desire for strategies when attempting to assure postpartum care for women who would receive that care from another provider. This is consistent with prior survey findings that showed both obstetricians/gynecologists (OB/GYNs) and PCPs identified care coordination as a barrier to improving postpartum screening and care among women with GDM (Ko 2013b; Rodgers 2014). Care coordination is (http://www.ahrq.gov/professionals/prevention-chronic-care/improve/coordination/index.html) the deliberate organization of patient care activities and the sharing information among all participants in a patient’s care to achieve safer and more effective care. In the context of the postpartum T2DM screen, care coordination is challenged by the lack of a clear responsible provider for ordering and administering the test (OB/GYN or PCP). OB/GYNs are primarily responsible for diagnosing GDM and are often the sole healthcare provider for women during their reproductive years (Rayburn 2014). Although OB/GYNs are less likely than PCPs to conduct a postpartum screening (Stormo 2014), the transition to a PCP is inconsistent and variable. Furthermore, the results of the test must be given to the provider who will deliver appropriate follow-up care depending on the test results.
The findings presented are subject to limitations. First, while our primary objective was to improve postpartum care, we were not able to capture baseline information on postpartum care and missing postpartum data was common. Missing postpartum data likely biased downward the observed rates of postpartum visits and postpartum T2DM screen. Postpartum data could be missing when a woman either received postpartum care after the end of he 11 months of data collection or when she received care from a provider other than the participating prenatal care site. In this project, five sites provided only prenatal care, while delivery and postpartum care were handled by other providers. Two of the sites that did not provide postpartum care attempted to obtain postpartum data from other providers, however their success was mixed. Second, when interpreting these findings it must be noted that the initiative was designed as a quality improvement initiative to produce measurable improvements within the participating sites, and not to produce generalizable findings.
Lessons learned from this pilot were used by the Collaborative to develop a second phase with three notable changes. First, the patient toolkit was updated to be inclusive of only one booklet focused on women diagnosed with GDM and incorporates some information from the general pregnancy booklet. Second, emphasis was added to care coordination within the provider toolkit resources (e.g., a letter template for communicating with the PCP), learning session content, and key measures (i.e., a measure of use of at least one care coordination strategy was developed). Care coordination strategies include ordering the OGTT screen during the delivery hospitalization, mailing a reminder postcard about the OGTT, and direct communication to the PCP regarding diagnosis and care recommendations. Third, efforts were made to improve the completeness of postpartum data, such as phone or fax follow up with the alternate provider. The Collaborative faced challenges receiving postpartum care data on women cared for by sites that don’t provide postpartum care. Rather than exclude theses sites new strategies to obtain data will be implemented. This model of care delivery is common for Ohio women with GDM (who may be referred to specialists for prenatal care only and referred back to their general obstetric provider or PCP following delivery) and improving care within this delivery care model cannot be ignored.
This pilot quality improvement project demonstrated improvements in prenatal education and high acceptance of provider and patient toolkit resources. However, reported rates of postpartum visits and screening for T2DM suggest that additional strategies are necessary to support increased utilization of postpartum care. While much remains to be learned about how to optimize postpartum care for high risk women, this work has produced resources that support clinicians in providing care consistent with current guidelines and describe a promising approach to supporting change. The toolkit and learning session content can be freely accessed at http://www.ohiogdm.com. Future practice will build on the lessons learned, with an emphasis on care coordination, and aim to improve measurement of postpartum outcomes.
References
American College of Obstetricians and Gynecologists. (2013). Practice bulletin number 137: Gestational diabetes mellitus. Obstetrics and Gynecology, 122(Supplement 2 Part 1), 406–416.
American Diabetes Association. (2013). Standards of medical care in diabetes—2013. Diabetes Care, 36 (Supplement 1), S11–S66.
Bardenheier, B. H., Imperatore, G., Gilboa, S. M., Geiss, L. S., Saydah, S. H., Delvin, H. M., … Gregg, E. W. (2015). Trends in gestational diabetes among hospital deliveries in 19 U.S. states, 2000–2010. American Journal of Preventive Medicine, 49(1), 12–19.
Bellamy, L., Casas, J. P., Hingorani, A. D., & Williams, D. (2009). Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet, 373, 1773–1779.
Care Coordination. (content last updated July 2016). At Agency for Healthcare Research and Quality, Rockville, MD online. Retrieved from http://www.ahrq.gov/professionals/prevention-chronic-care/improve/coordination/index.html.
Centers for Disease Control and Prevention. (2014). National diabetes statistics report: Estimates of diabetes and its burden in the United States, 2014. Accessed November 10, 2015, from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf.
Cheung, N. W., & Byth, K. (2003). Population health significance of gestational diabetes. Diabetes Care, 26(7), 2005–2009.
DeSisto, C. L., Kim, S. Y., & Sharma, A. J. (2015). Prevalence estimates of gestational diabetes mellitus in the United States, pregnancy risk assessment monitoring system (PRAMS), 2007–2010. Preventing Chronic Disease, 11, 130415. doi:10.5888/pcd11.130415.
Feig, D. S., Zinman, B., Wang, X., & Hux, J. E. (2008). Risk of development of diabetes mellitus after diagnosis of gestational diabetes. Canadian Medical Association, 179(3), 229–234.
Ferrara, A., Hedderson, M. M., Ching, J., Kim, C., Peng, T., & Crites, Y. M. (2012). Referral to telephonic nurse management improves outcomes in women with gestational diabetes. American Journal of Obstetrics and Gynecology, 206(6), 491–495.
Gunderson, E. P., Hurston, S. R., Ning, X., Lo, J. C., Crites, Y., Walton, D., … Quesenberry, C. P. (2015). Lactation and progression to type 2 diabetes mellitus after gestational diabetes mellitus: A prospective cohort study. Annals of Internal Medicine, 163(12), 889–898.
Hale, N., Picklesheimer, A. H., Billings, D. L., & Covington-Kolb, S. (2014). Impact of centering pregnancy group prenatal care on postpartum family planning. American Journal of Obstetrics and Gynecology, 210(1), 1–7. doi:10.1016/j.ajog.2013.09.001.
Hildebrand, D. A., McCarthy, P., Tipton, D., Merriman, C., Schrank, M., & Newport, M. (2014). Innovative use of influential prenatal counseling may improve breastfeeding initiation rates among WIC participants. Journal of Nutrition Education and Behavior, 46(6), 458–466.
Hunt, K. L., & Conway, D. L. (2008). Who returns for postpartum glucose screening follow gestational diabetes mellitus? American Journal of Obstetrics and Gynecology, 198, 404.e1–404.e6.
Ko, J. Y., Dietz, P. M., Conrey, E. J., Rodgers, L., Shellhaas, C., Farr, S. L., & Robbins, C. L. (2013a). Gestational diabetes mellitus and postpartum care practices of nurse-midwives. Journal of Midwifery and Women’s Health, 8(1), 33–40.
Ko, J. Y., Dietz, P. M., Conrey, E. J., Rodgers, L., Shellhaas, C., Farr, S. L., & Robbins, C. L. (2013b). Strategies associated with higher postpartum glucose tolerance screening rates for gestational diabetes mellitus patients. Journal of Women’s Health, 22(8), 681–686.
Langley, G. L., Moen, R., Nolan, K. M., Nolan, T. W., Norman, C. L., & Provost, L. P. (2009). The improvement guide: A practical approach to enhancing organizational performance (2nd Ed.). San Francisco, CA: Jossey-Bass Publishers.
Oza-Frank, R., Bouchard, J., Conrey, E., Shellhaas, C., & Weber, M.B. (2015). Health care experiences of low-income women with gestational diabetes and suggestions for improving care [abstract]. Diabetes, 64(Supplement 1), A672.
Oza-Frank, R., Ko, J. Y., Wapner, A., Rodgers, L., Bouchard, J., & Conrey, E. J. (2014). Improving care for women with a history of gestational diabetes: A provider perspective. Maternal and Child Health Journal, 18(7), 1683–1690.
Oza-Frank, R., Shellhaas, C., Wapner, A., & Conrey, E. (2011). Gestational diabetes in Ohio: 2006–2008. Ohio Department of Health. Accessed November 10, 2015, from https://www.odh.ohio.gov/~/media/ODH/ASSETS/Files/prams%20-%20pregnancy%20risk%20assessment%20monitoring%20program/Reports%20and%20Fact%20Sheets/ohiogdm_databook_oct_2011.pdf.
Ratner, R. E., Christophi, C. A., Metzger, B. E., Dabelea, D., Bennett, P. H., Pi-Sunyer, X., … The Diabetes Prevention Program Research Group. (2008). Prevention of diabetes in women with a history of gestational diabetes: Effects of metformin and lifestyle interventions. Journal of Clinical Endocrinology and Metabolism, 93(12), 4774–4779.
Rayburn W. F., Petterson, S. M., & Bazemore, A. (2014). Preferences of sites for office-based care by reproductive-aged women. Obstetrics & Gynecology, 123, 88S. doi:10.1097/01.AOG.0000447420.16812.c8.
Rodgers, L., Conrey, E. J., Wapner, A., Ko, J. Y., Dietz, P., & Oza-Frank, R. (2014). Primary healthcare providers’ knowledge and attitudes regarding care for women with histories of gestational diabetes. Preventing Chronic Disease, 11, 1403–1408.
Stormo, A. R., Saraiya, M., Hing, E., Henderson, J. T., & Sawaya, G. F. (2014). Women’s clinical preventive services in the United States: Who is doing what? Journal of the American Medical Association Internal Medicine, 174(9), 1512–1514.
Vesco, K. K., Dietz, P. M., Bulkley, J., Bruce, F. C., Callaghan, W. M., England, L., … Hornbrook, M. C. (2012). A system-based intervention to improve postpartum diabetes screening among women with gestational diabetes. American Journal of Obstetrics and Gynecology, 207(4), 281–286.
Weber, M. B., Bouchard, J., Conrey, E., Shellhaas, C., & Oza-Frank, R. (2015). Type 2 diabetes screening, risk and prevention among low-income women with a history of gestational diabetes [abstract]. Diabetes, 64(Supplement 1), A674.
Yarrington, C., & Zera, C. (2015). Health systems approaches to diabetes screening and prevention in women with a history of gestation diabetes. Current Diabetes Report, 15, 114–119.
Acknowledgments
Clinical subject matter experts: Steven Gabbe MD; Mark Landon, MD; Stephen Thung, MD—The Ohio State University College of Medicine, Division of Maternal Fetal Medicine. Toolkit development: Health Services Advisory Group—Phoenix, Arizona. Pilot sites: Akron Children’s Hospital Maternal Fetal Medicine—Akron, Ohio; Center for Health Services at Promedica—Toledo, Ohio; Cleveland Clinic Foundation, Cleveland, Ohio; Diabetes Wellness Center of Atrium Medical Center—Middletown, Ohio; Madison County Hospital—London, Ohio; Mercer Health Disease Management Clinic—Coldwater, Ohio; Mercy Health Anderson OB/GYN Care Center—Cincinnati, Ohio; OB/GYN Specialists of Lima—Lima, Ohio; Ohio Health O’Bleness Hospital, Athens Medical Associates—Athens, Ohio; Ohio State University Maternal Fetal Medicine—Columbus, Ohio; Ohio State University OB/GYN Clinics—Columbus, Ohio; Pickaway Health Center of Berger Health Systems—Circleville, Ohio; Summa Health System—Akron, Ohio; University of Cincinnati Medical Center—Cincinnati, Ohio; University Hospitals MacDonald Women’s Hospital—Cleveland, Ohio.
Funding
The Ohio Office of Health Transformation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Jo Bouchard—Retired from The Ohio Department of Health
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shellhaas, C., Conrey, E., Crane, D. et al. The Ohio Gestational Diabetes Postpartum Care Learning Collaborative: Development of a Quality Improvement Initiative to Improve Systems of Care for Women. Matern Child Health J 20 (Suppl 1), 71–80 (2016). https://doi.org/10.1007/s10995-016-2170-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-2170-2