Abstract
Objectives In light of the potential physical and emotional costs to both woman and child, this study was conducted to assess pregnancy complications and birth outcomes in primiparae at very advanced maternal age (VAMA, aged ≥45) compared to younger primiparae. Methods Retrospective cohort study comparing 222 VAMA primiparae and a reference group of 222 primiparae aged 30–35, delivering at Sheba Medical Center from 2008 through 2013.Results VAMA primiparae were more likely than younger primiparae to be single, to have chronic health conditions, and higher rates of gestational diabetes mellitus (GDM), gestational-hypertension (GHTN) and preeclampsia-eclampsia. VAMA primiparae conceived mostly by oocyte donation. They were more likely to be hospitalized during pregnancy, to deliver preterm and by cesarean birth. Infants of VAMA primiparae were at greater risk for low birthweight and Neonatal Intensive Care Unit admission. There were no differences in outcomes between VAMA primiparae with or without preexisting chronic conditions, or between those aged 45–49 and ≥50. In multivariable analysis VAMA was an independent risk factor for GDM, GHTN and preeclamsia-eclampsia, with adjusted odds ratio of 2.38 (95 % CI 1.32, 4.29), 5.80 (95 % CI 2.66, 12.64) and 2.45 (95 % CI 1.03, 5.85); respectively. The effect of age disappeared in multiple pregnancies. Conclusions Primiparity at VAMA holds a significant risk for adverse pregnancy and birth outcomes. The absence of chronic medical conditions or the use of a young oocyte donor does not improve these outcomes. Multiple pregnancies hold additional risk and may diminish the effect of age. Primiparity at an earlier age should be encouraged.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Delayed childbearing is on the rise and expected to rise further. It has been associated with adverse outcomes. However, existing information specifically regarding primiparity at the extreme ages of conception is limited.
What this study adds? This study, focusing on primiparae aged ≥45, reveals exceptionally high rates of pregnancy complications and adverse birth outcomes, compared to younger primiparae, and demonstrates that the absence of chronic conditions or the use of a young oocyte donor does not improve these outcomes. The costs in physical and emotional terms should be considered in pursuing very-advanced-age primiparity.
Introduction
The past decades have seen a steep rise in the proportion of advanced-age maternity among all births in the Western world, and in the number of advanced-age primiparae in particular [1, 2]. In the US, from 1970 to 2006 the proportion of first births among women aged ≥35 increased nearly eight-fold [2]. In Israel, the number of first births to women aged ≥45 rose by more than 230 % between 1998 and 2008 [3]. Progress in assisted reproductive technology (ART), including oocyte donation (OD), expands the boundaries of fertility, enabling an increasing number of women to give birth for the first time in their fifth, sixth or even seventh decades [4, 5]. Therefore, recent literature relates to very advanced maternal age (VAMA), a term coined by Dildy et al. [6], referring to women aged ≥45. A positive association has been reported between advanced-age maternity and adverse pregnancy and obstetric outcomes [7], with their associated expense in terms of health expenditures [8]. However, existing information regarding VAMA primiparity is limited, and in research this group is often embedded within a larger population, which is primarily multiparae [9–11] and/or of wider age range [7, 12]. In Israel, where fertility treatments are covered by National Health Insurance for the first two children [13] and where the use of ART is relatively extensive [14], studies have heretofore been limited by small sample size, lack of control groups and/or not relating specifically to VAMA primiparae [15–19]. As the number of VAMA primiparae is growing and expected to rise further, it is necessary to determine whether they constitute a specific risk group requiring a unique clinical approach. In light of the potential physical and emotional costs to both woman and child, this study was conducted to assess pregnancy complications and birth outcomes in primiparae aged ≥45 as compared to younger primiparae, in order to assist the effort of providing a more informed consultation to these women when planning a pregnancy.
Methods
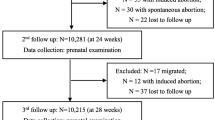
This historical cohort study included all primiparae aged ≥45 who delivered at Sheba Medical Center between January 1, 2008 and December 31, 2013 (the VAMA group), and a Control group (Controls) of 222 primiparae aged 30–35 who delivered at the same facility during these years. Delivery refers to any pregnancy that resulted in the birth of a fetus, deceased or alive, spontaneously, by induction or by Cesarean birth (CB). Participants were identified from the computerized delivery room records. The Control group was compiled systematically by selecting the next parturient who met Controls inclusion criteria (primiparity and age 30–35) listed after each VAMA primiparae. Data were abstracted from participants’ computerized medical records using a pre-constructed de-identified data sheet. The term ‘chronic condition’ refers to any persistent or constantly recurring medical condition that existed prior to the pregnancy. Data regarding antenatal screening exams were analyzed by comparing the rate of participants who underwent a complete or partial antenatal battery of standard examinations. A complete battery included: nuchal translucency, early scan, triple test and anomaly (late) scan. If one or more of these tests were not done, the screening was considered partial. Gestational diabetes mellitus (GDM) was diagnosed by exceeding ≥2 of Carpenter and Coustan criteria [20]. Hypertensive disorders of pregnancy were defined according to the 2013 ACOG Taskforce report on Hypertension in Pregnancy [21]. Gestational age was based on last menstrual period that was corroborated in first trimester ultrasound. Preterm premature rupture of membranes (PPROM) was defined as rupture of membranes before onset of labor and before 37 weeks of gestation. Gestational size was calculated according to Dolberg et al. [22]. Small for gestational age (SGA) was defined as infant body weight <10th percentile for the gestational age. Preterm birth (PTB) was defined as birth between 20 0/7 weeks of gestation and 37 weeks of gestation. Low birth-weight (LBW) was defined as <2500 g. The study was approved by the Sheba Medical Center IRB (No: 920051170/3656, January 15, 2013).
Statistical Analyses
Statistical analysis was conducted using SAS for Windows, Version 9.2. Univariate analyses included t test and Mann–Whitney for continuous variables and Chi square for categorical variables or Fisher’s exact test for small cell sizes. Missing data were not included in the analyses. A P value of ≤0.05 was considered significant. Multivariable logistic regression explored the relationships between adverse outcomes while adjusting for demographic and clinical variables. Variables were included for their significance upon univariate analysis, as well as for their clinical relevance to the outcome under consideration. Interactions between age and plurality were examined, and where borderline or significant, additional logistic regression models were constructed according to breakdowns of the sample by plurality. Additional multivariate analysis compared ART pregnancies among the VAMA and among Controls to naturally conceived pregnancies among the Controls. Further univariate analyses for the VAMA group were conducted by dividing the VAMA into two sets of sub-groups: by the existence or absence of pre-pregnancy chronic condition and by age of 45–49 or ≥50.
Results
Of the 22,402 primiparae who delivered at Sheba Medical Center during 2008–2013, 222 were ≥45 years of age (range 45–61) (Table 1). Significantly higher rates of unmarried women and prior pregnancies were seen among the VAMA compared to the Controls. The VAMA group also had a significantly higher rate of pre-pregnancy chronic conditions; the rate of VAMA with ≥2 chronic conditions was double that of the Controls. Over 96 % of the women in the VAMA group reported conceiving through ART, compared to 24 % among the Controls (P < 0.0001). IVF was the primary method of conception in the VAMA group and 80.3 % of those who underwent IVF reported using OD. Multiple pregnancies were more prevalent among the VAMA compared to the Controls (P < 0.0001). Eight participants underwent fetal reduction. Three of them were reduced from multiple to singleton pregnancies, but were considered as multiple in the analysis. No difference was found in terms of antenatal screening exams between the VAMA and Controls, and rates of those who completed the battery were high among both groups (86.0 vs. 90.5 %, respectively; P = 0.14).
Obstetric outcomes are shown on Table 2. Significantly higher rates of pregnancy complications, including GDM, gestational hypertension (GHTN), preeclmsia-eclampsia (PEE) and cervical insufficiency requiring cerclage were seen in the VAMA group compared to the Control group and over twice the rate of VAMA suffered at least one pregnancy complication compared to the Controls. Over twice the rate of VAMA participants were hospitalized during pregnancy compared to those in the Control group, although there was no difference in number of admissions or length of stay. The earliest gestational age for delivery in the current study was 22 weeks (stillbirth). The overall PTB rate (<37 weeks) among the VAMA was nearly triple that of the Controls (30.7 vs. 11.3 %). Cesarean births were significantly more prevalent in the VAMA group than in the Control group, with CB due to maternal request more prevalent in the former and unplanned CB more prevalent in the latter. The main reasons for unplanned CB were non-reassuring fetal monitor (31.4 %), PEE (28.4 %), labor progression interference (14.0 %) and PROM/PPROM (7.0 %). Prolonged post-delivery hospitalization, even when accounting for mode of delivery, was nearly triple the rate among the VAMA than among the Controls (P < 0.0001).
During the study period, the participants delivered 503 liveborn infants (Table 3). Seven infants in the VAMA group and two in the Control group were stillborn, and are not included in neonatal-related analyses. The rates of LBW (1500–2499 g) and very LBW (VLBW; <1500 g) infants were higher among the VAMA compared to the Controls, and significantly higher rates of VAMA newborns were admitted to Neonatal Intensive Care Unit (NICU) compared to newborns in the Control group.
In multivariable analysis (Table 4), VAMA primiparity was found to be an independent risk factor for GDM, GHTN, PEE, hospitalization during pregnancy and prolonged post-delivery hospitalization. Multiple pregnancy was an independent risk factor in most outcomes. Adjusted odds ratio by plurality for outcomes that were borderline or significant for interaction between age and plurality, neutralized the effect of age in multiple pregnancies. Additional multivariate analysis revealed that while women of the control group conceived by ART had no additional significant risk for GDM, GHTN or PEE compared to naturally conceived ones, the VAMA did (data not shown).
Subgroup analysis (Table 5) revealed no significant differences in rates of the examined outcomes between VAMA primiparae with or without chronic condition, or between VAMA age subgroups.
Discussion
This study presents obstetric and perinatal characteristics and outcomes of VAMA primiparity. In contrast to most other studies relating to VAMA [9–11, 16–19, 23] this study population included only primiparae. This, may in part explain the extent of the effect on some outcomes, and may suggest the heightened impact of primiparity at these ages. The main findings indicated that VAMA primiparity bears a considerable physical and potentially emotional cost to both woman and child. Compared to the younger participants, VAMA primiparae suffered from higher rates of chronic conditions, pregnancy complications such as GDM, GHTN, PEE, PTB, and higher rates of CB and poorer neonatal outcomes. In addition to the immediate issues, there may be longer-term costs inherent in raising a child who may have developmental problems associated with prematurity and LBW [24].
The rate of VAMA participants who were married or had a stable partner at delivery stands in contrast to other studies that have reported higher rates of steady partners among VAMA parturients [10, 23]. This difference may be due the exclusive inclusion of primiparae in this study, socio-demographically distinguishing this group from general VAMA population. Fewer than half of the VAMA primiparae were primigravidae, possibly reflecting the low success rate of fertilization treatments in this age [25], focusing attention on the cost-effectiveness of trying to achieve and preserve pregnancies at VAMA.
Forty percent of the women in the VAMA group suffered from some chronic condition. Lower but similar rates were reported by Glasser et al. [15]. The rate of chronic hypertension among the VAMA was significantly higher than that among the Controls, and consistent with that found in other Israeli studies relating to the general VAMA population [16, 17], but higher than that reported in other countries [9, 10]. Since there is evidence of a link between chronic hypertension and PEE [21], thorough screening before fertility treatments is advised. Importantly, however, the present findings indicate that the risk for adverse pregnancy complications and birth outcomes among VAMA primiparae was not significantly different for those with or without chronic conditions, suggesting that good health among women in this group does not ensure better pregnancy outcomes. Antenatal screening exams rates were similar between the study and reference groups and reflected the rates reported in Israel, reducing the likelihood that the VAMA primiparae were over diagnosed due to a more extensive follow-up.
Nearly all VAMA participants conceived using ART, mostly IVF and OD. It is likely that the proportion of OD might even be higher and was underreported. Other Israeli studies have also reported high OD rates among VAMA women [15, 16], in contrast to findings in other countries reporting significantly lower rates of ART use [9, 11]. This discrepancy might be due to the fact that in Israel the cost of fertility treatments (with OD) is covered by the National Health Insurance Law for women up to the age of 54 [13, 26], as well as to the fact that this study included only primiparae, while others included both primi- and multiparae [9, 11].
The rate of multiple pregnancies among the VAMA was over triple that of the Controls, likely due to the nearly exclusive use of ART among the former. Over one-third of the newborns in the VAMA group were twins, a higher rate than the 25 % reported in the general population for this age group in Israel [27]. Multiple pregnancy is considered a major risk factor for adverse obstetric outcomes [28], and as found by Simchen et al. [29], multiple pregnancies achieved by IVF-OD are at even greater risk for adverse outcomes such as PTB and LBW, compared to non-OD multiple pregnancies. In our study, multiple pregnancy was an independent risk factor for most outcomes, indicating that this type of pregnancy add to the risk in this already high-risk group. Multivariable analysis by plurality neutralized the effect of maternal age on outcomes in multiple pregnancies, emphasizing the heightened risk. Therefore, despite the possible controversy in terms of cost-effectiveness (“two babies for the ‘price’ of one”), the alternative of transferring a single, good-quality embryo might be the preferred option in women of this age group. Furthermore, the findings of this study may also indicate that using a young oocyte donor does not improve pregnancy outcome.
Pregnancy complications were more prevalent among the VAMA primiparae compared to the younger ones. Nearly one-third of the VAMA suffered from GDM, a much higher rate than that reported in most other studies relating to VAMA [9–11, 16, 19]. The high incidence of GDM may in part be explained by undiagnosed cases of pre-gestational diabetes, emphasizing again the necessity of better screening these women before pregnancy. One-quarter of the VAMA participants suffered from GHTN. Together with those who suffered from chronic hypertension, these women, more than 30 % of the VAMA group, constitute a high-risk group for PEE; indeed the rate of PEE among them was quadruple that in the Control group. This finding is supported by Glasser et al. [15], but is higher than that reported by other studies of VAMA that did not relate exclusively to primiparae [9, 10, 16], lending strength to the evidence that primiparity is an independent risk factor for PEE [21]. Another possible explanation for this was proposed by Le Ray et al. [11], who reported higher rates of preeclmpsia among VAMA women who underwent IVF-OD, compared to those who underwent IVF alone or did not undergo IVF at all, suggesting an association between IVF-OD and preeclamsia. Nevertheless, our results suggest that despite the additional risk inherent in ART, VAMA primiparity remains an independent risk factor for GDM, GHTN and PEE.
Almost one-third of the VAMA women were hospitalized during pregnancy, consistent with the findings of Simchen et al. [19], and reflecting their high rate of pregnancy complications. The association of VAMA with GDM, GHTN, PEE and hospitalization during pregnancy remains even when adjusting for other demographic, medical and obstetric factors.
Preterm birth was significantly more prevalent among the VAMA compared to the Controls, consistent with the established association between prematurity and advanced maternal age [30], and with the increased rate of complications in the VAMA group. Other studies that included a mixed population of primi- and multiparae subjects reported lower rates of PTB among their VAMA participants, possibly due to lower complications rates [10], lower rates of ART pregnancies [16], and including only singleton pregnancies [17, 31], as the association between ART and multiple pregnancies to PTB has been reported [30].
The vast majority of VAMA women delivered by CB, similar to the 94 % reported by Glasser et al. [15], although higher than those found by others [9, 10]. In the present study this high rate may in part reflect the high rate of multiple gestations and the predominant elective factor for CB in the VAMA group. Additional possible contributors were the increased rates of previous gynecological surgeries and pregnancy complications among the VAMA, which may have led to medical indications requiring CB. Considering the reasons for CB, the rate of “CB upon maternal request” among the VAMA was over six times that among the Controls, possibly reflecting the state of mind regarding mode of delivery among the VAMA primiparae, who may be more prone to request CB, and/or their caregivers who may be prone to recommend it [32, 33]. Lower rates of unplanned CB were seen among the VAMA compared to the Controls likely since the elective factor among the VAMA primiparae was significant, and many deliveries were performed before labor onset. Indeed, labor-related indications comprised almost half of the unplanned CB.
Generally, neonate-related outcomes were poorer in the VAMA group compared to the Control group. Although the rate of stillborns was triple among the VAMA primiparae than among the Controls, this was not statistically significant due sample size limitation. Nearly one-third of the newborns in the VAMA group were LBW, about twice the rate in the Control group, and higher than that reported by others who included both primi- and multiparae [9, 16]. Glasser et al. [15], who included only primiparae reported a rate of 42 %. The VLBW and SGA rates among the VAMA were also higher than those reported in other studies [11, 16]. Nevertheless, unlike Carolan et al. [9], we found no difference in the rate of SGA between the study and reference groups, possibly due to the heightened risk inherent in primiparity to this outcome. This is borne out by the limited analysis performed by Carolan et al. [9] for CB, PTB and LBW by parity, which revealed significantly higher rates of these outcomes among the primiparae in both study and reference groups, rates which are very similar to the ones found in our study. Neonatal intensive care unit admission rate of VAMA newborns was almost twice the rate of 11 % reported by Yogev et al. [16], most of whose VAMA subjects were multiparae.
Sub-group analysis of the VAMA group revealed no differences between women aged 45–49 and ≥50. These findings are partially in contradiction to those of other studies that reported higher rates of GDM, PEE, PTB [16] and LBW [19] among women aged ≥50. However, those studies included both primi-and multiparae subjects. This might imply that, despite the incremental risk by the rise in maternal age seen in the general VAMA population, VAMA primiparae are at such high risk in the first place, that this increment in maternal age has no further negative effect on them.
The present study had several limitations. Firstly, this is a retrospective cohort study based on computerized medical records. This prevented complete access to potentially important data, such as reason for infertility, maternal BMI, level of education, socio-economic status and smoking habits. Also, pregnancies that were miscarried or terminated and have not resulted in a birth (still or live) were out of the scope of this study, and should be taken into account when relating to general outcome of conceiving in VAMA. Secondly, the study population included only women who gave birth at Sheba Medical Center, which is a Level 3 maternity hospital, and may not represent the level or methods of treatment in other hospitals, or the general maternity population in Israel. However, comparing Sheba Medical Center to other Israeli hospitals, it is apparent that Sheba Medical Center is not very different from other tertiary centers in terms of the rates of primiparae parturients, CB rates and instrumental deliveries [34]. Thirdly, the sample size of the study population limits the ability to further examine rare outcomes, such as intra-uterine growth restriction, hemolysis, elevated liver enzymes, low platelet count syndrome (HELLP) and stillbirth. Wide confidence intervals for some outcomes suggest lack of power.
In conclusion, this study population focused on primiparae, distinguishing it from most other studies relating to VAMA. The findings reveal different characteristics, higher rates of pregnancy complications, and adverse birth outcomes among VAMA primiparae compared to younger primiparae. These findings reflect the potentially high cost–the “double jeopardy”–of primiparity at VAMA. The absence of chronic conditions or the use of a young oocyte donor does not necessarily improve the outcome of these pregnancies. Multiple pregnancies hold additional risk and may diminish the effect of age. Efforts should be made to reduce their number. In light of this, primiparity at an earlier age should be encouraged, and awareness of the risks of VAMA primiparity should be heightened, even for women who do not suffer from chronic condition. Considering the considerable resources invested in achieving and preserving these pregnancies, and as their rates are expected to rise, a better understanding of their consequences is necessary in order to provide better-informed consultation to this unique risk group. It is recommended that further research be conducted on larger groups of VAMA primiparae, in order to clarify the risks of rare but serious negative outcomes, as well as longitudinal studies on the short- and long-term outcomes. Also, the financial costs of these pregnancies involving ART should be considered in determining health policy. These costs were beyond the scope of the present study, but in light of chronically limited health care resources such assessment is recommended. It is hoped that the findings of this study can contribute to this effort and can assist caregivers, couples and individuals planning such pregnancies.
References
Heffner, L. J. (2004). Advanced maternal age—how old is too old. New England Journal of Medicine, 351(19), 1927–1929.
Mathews, T., & Hamilton, B. (2009). Delayed childbearing: More women are having their first child later in life.. USA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
Ministry of Health. (2010). Health in Israel: Selected data 2010. Jerusalem: Ministry of Health.
Antinori, S., Gholami, G., Versaci, C., Cerusico, F., Dani, L., Antinori, M., et al. (2003). Obstetric and prenatal outcome in menopausal women: A 12-year clinical study. Reproductive biomedicine online, 6(2), 257–261.
Paulson, R. J., Boostanfar, R., Saadat, P., Mor, E., Tourgeman, D. E., Slater, C. C., et al. (2002). Pregnancy in the sixth decade of life: Obstetric outcomes in women of advanced reproductive age. JAMA, 288(18), 2320–2323.
Dildy, G. A., Jackson, G. M., Fowers, G. K., Oshiro, B. T., Varner, M. W., & Clark, S. L. (1996). Very advanced maternal age: Pregnancy after age 45. American Journal of Obstetrics and Gynecology, 175(3 Pt 1), 668–674.
Cleary-Goldman, J., Malone, F. D., Vidaver, J., Ball, R. H., Nyberg, D. A., Comstock, C. H., et al. (2005). Impact of maternal age on obstetric outcome. Obstetrics and Gynecology, 105(5 Pt 1), 983–990.
Chambers, G. M., Sullivan, E. A., Ishihara, O., Chapman, M. G., & Adamson, G. D. (2009). The economic impact of assisted reproductive technology: A review of selected developed countries. Fertility and Sterility, 91(6), 2281–2294.
Carolan, M. C., Davey, M.-A., Biro, M., & Kealy, M. (2013). Very advanced maternal age and morbidity in Victoria, Australia: A population based study. BMC Pregnancy Childbirth, 13(1), 80.
Jacobsson, B., Ladfors, L., & Milsom, I. (2004). Advanced maternal age and adverse perinatal outcome. Obstetrics and Gynecology, 104(4), 727–733.
Le Ray, C., Scherier, S., Anselem, O., Marszalek, A., Tsatsaris, V., Cabrol, D., & Goffinet, F. (2012). Association between oocyte donation and maternal and perinatal outcomes in women aged 43 years or older. Human Reproduction, 27(3), 896–901.
Klemetti, R., Gissler, M., Sainio, S., & Hemminki, E. (2014). Associations of maternal age with maternity care use and birth outcomes in primiparous women: A comparison of results in 1991 and 2008 in Finland. BJOG, 121(3), 356–362.
National Helath Insurance Law, 1994. Book of laws, 1469 Page 156 Available from: http://fs.knesset.gov.il//13/law/13_lsr_211132.PDF. Accessed 21 Jan 2015 [in Hebrew]
Sullivan, E., Zegers-Hochschild, F., Mansour, R., Ishihara, O., de Mouzon, J., Nygren, K., & Adamson, G. (2013). International Committee for Monitoring Assisted Reproductive Technologies (ICMART) world report: Assisted reproductive technology 2004. Human Reproduction: det036.
Glasser, S., Segev-Zahav, A., Fortinsky, P., Gedal-Beer, D., Schiff, E., & Lerner-Geva, L. (2011). Primiparity at very advanced maternal age (>/=45 years). Fertility and Sterility, 95(8), 2548–2551.
Yogev, Y., Melamed, N., Bardin, R., Tenenbaum-Gavish, K., Ben-Shitrit, G., & Ben-Haroush, A. (2010). Pregnancy outcome at extremely advanced maternal age. American Journal of Obstetrics and Gynecology, 203(6), e551–e558.
Laskov, I., Birnbaum, R., Maslovitz, S., Kupferminc, M., Lessing, J., & Many, A. (2012). Outcome of singleton pregnancy in women >/=45 years old: a retrospective cohort study. Journal of Maternal-Fetal & Neonatal Medicine, 25(11), 2190–2193.
Laskov, I., Michaan, N., Cohen, A., Tsafrir, Z., Maslovitz, S., Kupferminc, M., Lessing, J., & Many, A. (2013). Outcome of twin pregnancy in women >/=45 years old: A retrospective cohort study. Journal of Maternal-Fetal & Neonatal Medicine, 26(7), 669–672.
Simchen, M. J., Yinon, Y., Moran, O., Schiff, E., & Sivan, E. (2006). Pregnancy outcome after age 50. Obstetrics and Gynecology, 108(5), 1084–1088.
Carpenter, M. W., & Coustan, D. R. (1982). Criteria for screening tests for gestational diabetes. American Journal of Obstetrics and Gynecology, 144(7), 768–773.
American College of Obstetricians and Gynecologists. (2013). Hypertension in pregnancy. Report of the American college of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obstetrics and Gynecology, 122(5), 1122.
Dollberg, S., Haklai, Z., Mimouni, F. B., Gorfein, I., & Gordon, E.-S. (2005). Birth weight standards in the live-born population in Israel. Israel Medical Association Journal, 7(5), 311–314.
Salihu, H. M., Shumpert, M. N., Slay, M., Kirby, R. S., & Alexander, G. R. (2003). Childbearing beyond maternal age 50 and fetal outcomes in the United States. Obstetrics and Gynecology, 102(5 Pt 1), 1006–1014.
Aarnoudse-Moens, C. S. H., Weisglas-Kuperus, N., van Goudoever, J. B., & Oosterlaan, J. (2009). Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics, 124(2), 717–728.
Gnoth, C., Maxrath, B., Skonieczny, T., Friol, K., Godehardt, E., & Tigges, J. (2011). Final ART success rates: a 10 years survey. Human Reproduction, 26(8), 2239–2246.
Law of Oocyte Donation, 2010. Book of laws, 2242, Page 520. Available from: http://fs.knesset.gov.il//18/law/18_lsr_300729.pdf. Accessed 21 Jan 2015 [in Hebrew].
Israel Central Bureau of Statistics, Newborns in Single and Multiple Births, by Mother’s Population Group, Religion and Age 2010 [Internet] 2013. Available from: http://www.cbs.gov.il/reader/shnaton/shnatone_new.htm?CYear=2013&Vol=64&CSubject=30. Accessed 15 Dec 2014
American College of Obstetricians and Gynecologists. (2004). Multiple gestation: complicated twin, triplet, and high-order multifetal pregnancy. ACOG Practice Bulletin, 56, 1–15.
Simchen, M. J., Shulman, A., Wiser, A., Zilberberg, E., & Schiff, E. (2009). The aged uterus: Multifetal pregnancy outcome after ovum donation in older women. Human Reproduction, 24, 2500–2503.
Goldenberg, R. L., Culhane, J. F., Iams, J. D., & Romero, R. (2008). Epidemiology and causes of preterm birth. Lancet, 371(9606), 75–84.
Luke, B., & Brown, M. B. (2007). Elevated risks of pregnancy complications and adverse outcomes with increasing maternal age. Human Reproduction, 22(5), 1264–1272.
Weaver, J., Statham, H., & Richards, M. (2001). High caesarean section rates among women over 30. High rates may be due to perceived potential for complications. BMJ (Clinical Research Ed.) 323(7307), 284–285.
Lin, H.-C., & Xirasagar, S. (2005). Maternal age and the likelihood of a maternal request for cesarean delivery: A 5-year population-based study. American Journal of Obstetrics and Gynecology, 192(3), 848–855.
Israeli Society of Maternal Fetal Medicine. Obstetrics in Israel, Report for 2012. Annual conference of Israeli Society of Maternal Fetal Medicine. November 2012. Ramat-Gan, Israel.
Acknowledgments
The authors wish to express their appreciation to Dana Fructer, MSc (Women & Children’s Research Unit, Gertner Institute) for her advice and assistance on the statistical analysis of the data, and to Daphna Pollack, MPH (Computer and Informatics Unit, Gertner Institute) for the SAS database programming assistance. No compensation was provided to either Ms. Fructer or Ms. Pollack for their assistance on this research.
Source of Funding
There has been no significant financial support for this work that could have influenced its outcome.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflict of interest.
Rights and permissions
About this article
Cite this article
Ben-David, A., Glasser, S., Schiff, E. et al. Pregnancy and Birth Outcomes Among Primiparae at Very Advanced Maternal Age: At What Price?. Matern Child Health J 20, 833–842 (2016). https://doi.org/10.1007/s10995-015-1914-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1914-8