Abstract
Objectives To examine the association between adverse childhood experiences (ACEs) and pregnancy outcomes; to explore mediators of this association including psychiatric illness and health habits. Methods Exposure to ACEs was determined by the Early Trauma Inventory Self Report Short Form; psychiatric diagnoses were generated by the Composite International Diagnostic Interview administered in a cohort of 2303 pregnant women. Linear regression and structural equation modeling bootstrapping approaches tested for multiple mediators. Results Each additional ACE decreased birth weight by 16.33 g and decreased gestational age by 0.063. Smoking was the strongest mediator of the effect on gestational age. Conclusions ACEs have an enduring effect on maternal reproductive health, as manifested by mothers’ delivery of offspring that were of reduced birth weight and shorter gestational age.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
There is little prospective information available on whether and how traumatic experiences prior to the age of 18 influence pregnancy outcomes. This report provides such information on a well-articulated, longitudinal cohort of pregnant women.
Background
Adverse childhood experiences that occur prior to the age of 18 have been associated with unfavorable future health outcomes [e.g. chronic obstructive pulmonary disorder, ischemic heart disease, tumor growth, major depressive disorder, post-traumatic stress disorder (PTSD)] [1–5], risky health behaviors (illicit drug abuse, alcohol abuse and early initiation of sexual activity) [6–9] and neurodevelopmental deficits [10]. Typically, adverse child experiences are divided into three classes of events occurring prior to the child’s 18th birthday: (1) abuse, including emotional, physical and sexual; (2) neglect, including emotional and physical and (3) household dysfunction, including interpersonal violence, household substance abuse, household mental illness, parental separation or divorce and incarceration of a household member [11].
Numerous investigators have examined the impact of major life events, including severe trauma experienced in pregnancy and chronic stress, on risk of low birth weight and preterm birth (see recent reviews by Dunkel Schetter) [12, 13]. The preponderance of evidence suggests that major life events and traumatic events that occur during pregnancy predict birth weight and preterm birth, with even more robust effects observed for chronic stressors. However, there is little prospective information available on whether and how traumatic experiences prior to the age of 18 influence pregnancy outcomes. An exception is a small literature that has focused on childhood sexual abuse as a risk factor for preterm birth and low birth weight. Several studies [14–16], found no association between childhood sexual abuse and birth outcomes; a case–control study, limited by small sample size (n = 28) found that women with childhood sexual abuse had longer pregnancies and more protracted labor than control women [17]. A diagnosis of PTSD mediated the relationship between child abuse and either birth weight or gestational age in a prospective study of 174 women who were survivors of childhood sexual abuse [18] and alcohol use mediated the relationship between childhood sexual abuse and preterm birth [19].
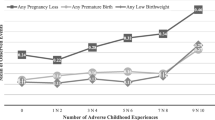
A larger literature suggests a dose response relationship exists between the number of reported adverse childhood events and risk of having an operative delivery, or infant’s admission to the neonatal intensive care unit. Adverse childhood experiences have also been related to [20, 21], suicidality and depressive symptoms in pregnancy [22, 23], somatic complaints in pregnancy [24] and maternal and infant health complications after childbirth [15, 21]. While the mechanisms underlying these associations are not yet clear some speculate that pregnancy related health behaviors such as substance abuse, smoking, prescription medication use or demographic factors such as marital status and education could also potentially mediate the relationship between adverse childhood events and sub-optimal pregnancy outcomes [16, 18, 25]. However, whether factors such as psychiatric disorders [5, 26] and health behaviors [16, 19] are part of the direct causal pathway between adverse childhood events and birth outcomes or confounding factors, is not clear.
To our knowledge, there are no prospective studies examining shortened gestational age or other adverse pregnancy outcomes (lower birth weight) for women reporting a wide range of adverse childhood experiences including, but not limited to childhood sexual abuse. It is also unclear whether women who have experienced a wide range of adverse childhood experiences are at high risk for adverse pregnancy outcomes and/or whether a current diagnosis of PTSD or other psychiatric disorders in such women may mediate this association. Accordingly, the objectives of the study were: (1) to examine if there is an association between adverse childhood experiences and pregnancy outcomes (gestational age and birth weight). If an association was evident, we sought to (2) explore possible causal pathways between adverse childhood experiences and pregnancy outcomes.
Methods
Study Design
The methods of this study are presented in full elsewhere [27] but are described briefly herein. Data were derived from a large prospective cohort study of pregnant women who were enrolled between March of 2005 and May of 2009 with the primary aims of examining whether a diagnosis of major depressive disorder and/or use of a psychotropic medication were associated with adverse birth outcomes. Women were recruited from 137 obstetrical practices and hospital-based clinics throughout Connecticut and Western Massachusetts via informational letters and other printed methods of advertising. For this study, women were interviewed in-person prior to 16 completed weeks gestation and re-interviewed by phone at 28 (±2) weeks gestation and again at 8 (±4) weeks postpartum.
Inclusion/Exclusion Criteria
Women were eligible to participate if they were at least 18 years of age, had not yet completed their 16th week of pregnancy and were willing to provide written informed consent. Women were ineligible if they: (1) had a known multi-fetal pregnancy, (2) suffered from insulin-dependent diabetes, (3) did not speak English or Spanish, (4) did not have access to a telephone, (5) had plans to relocate or (6) intended to terminate their pregnancy.
Assessment Procedures
Staff administered a structured screening questionnaire that collected information about pregnancy dates, depressed mood, history of depressive episodes, antidepressant treatment, trauma exposure, and plans to relocate or terminate the pregnancy. We used these results to invite participation from all otherwise eligible women who used antidepressant medication, experienced a significant trauma, and/or screened positive for a probable major depressive episode, and/or reported a diagnoses of major depressive disorder (MDD) within the 5 years prior to screening. We randomly selected and invited participation from one of every three women who did not have these exposures. We obtained written consent during the in-person interview. Human subjects approval was granted by the Yale School of Medicine and hospitals affiliated with the study.
Exposure and Outcome Measures
At each assessment point, we gathered data on MDD and depressive symptoms, post traumatic stress and trauma symptoms, psychiatric medication use (including antipsychotics), licit and illicit drug and medication use and pregnancy complications. Information about psychiatric symptoms were obtained at each assessment point through administration of the depressive disorder and panic disorder modules of the WMH-CIDI [28], and the modified PTSD Symptom Scale (MPSS) [29] to determine a diagnosis of PTSD and post traumatic symptoms. Possible presence of adverse childhood events was assessed by administration of a modified version of the Early Trauma Inventory Self Report Short Form (ETI-SF) [30]. The main modification of the instrument was to collapse the sexual events before the age of 18 questions into 1 question asking about childhood sexual abuse prior to age 18. The question read, “Thinking about events that may have occurred before the age of 18, “Were you ever sexually molested, that is, someone touched you in a way that made you feel uncomfortable? In a comparison of the ETI-SR to the ETI-SR11, domain scores for the shortened version correlated highly with the original list for general trauma (r = 0.91), and physical (r = 0.94), emotional (r = 0.97), and sexual abuse (r = 0.97). The ETI-SR11 was administered once in pregnancy during the second interview (28 weeks gestation ±2). Acceptable validity and internal consistency have been reported for the ETI-SR11.
Trained medical record reviewers who were masked to a woman’s psychiatric, adverse childhood event history and/or medication status obtained data on preterm birth and low birth weight. To corroborate gestational age we used a first trimester ultrasound. If that was unavailable, we used the participants stated last menstrual period and if the date for the last menstrual period was unreliable, we used an ultrasound conducted later in pregnancy.
Interviewers and Quality Control
Interviewer training included a minimum of 4 days of didactics, review of training tapes that illustrated interview techniques and administration of the interview, completion of at least six practice interviews and a minimum of four supervised interviews before becoming eligible to conduct independent interviews (see Yonkers et al. [27] for full description of methods). We audiotaped interviews with permission of participants and randomly selected a subset of tapes for quality control assessment.
Study Recruitment
Figure 1 illustrates study recruitment. An initial 9525 women volunteered to be screened, of whom 1905 (20 %) met entrance criteria and screened positive for a depressive episode within the last 5 years and/or experienced trauma with flashbacks and/or were undergoing antidepressant treatment. An additional group of 4533 (48 %) met entrance criteria and screened negative for these clinical characteristics. We invited all women who screened positive and randomly selected 1612 (36 %) and who screened negative to participate. Of these 3517 potential participants, we interviewed 2793. Women were included in the analytic cohort if they were delivered of a singleton live birth and provided complete data for adverse childhood events and demographics (n = 2303). Most missing data were due to women falling out of contact for the second interview, when the modified ETI-SR was administered. Non-completion was most likely due to a move or a phone number that was no longer in service. However, women with first trimester PTSD (as a marker for mental illness) were somewhat more likely to fall out of contact. Twenty (6 %) of the 351 excluded women had first trimester PTSD, compared to 58 (3 %) of the 2303 women with complete data.
Statistical Procedures
Gestational age at delivery (weeks) and birth weight (grams) were the outcome variables of interest. The main independent variable of interest, the number of unique adverse childhood events was calculated for each respondent. To examine the association between adverse childhood events and pregnancy outcomes (Aim #1) we used linear regression models that contained the number of adverse childhood events as a predictor. Beta coefficients and standard errors were calculated for these models.
To address our second aim, we explored mediators of the association between adverse childhood experiences and birth outcomes. We hypothesized a role for the following possible factors (Fig. 2): marital status, illicit substance use and alcohol use during pregnancy, serotonin reuptake inhibitor (SRI) use during pregnancy, any psychiatric disorder during pregnancy, education, smoking during pregnancy and social support during pregnancy. To test this aim, we used a multiple mediation model that allows for a causal relationship to be mediated by more than one factor. The analysis entailed a structural equation modeling (SEM) bootstrapping approach [31]. We decomposed the differential effect (the difference between the magnitude of effects c and c’ in Fig. 2) of adverse childhood events on birth outcomes with (indirect paths) and without (direct path) mediators; the various mediators were resolved into unique indirect pathways. These indirect pathways are termed “ab” pathways in reference to being a combination of each pathway “a” (independent variable to mediator) and pathway “b” (mediator to outcome). The bootstrapping SEM approach is an alternative to the more widely used Sobel test [32]; it allows for more than one mediator and does not require that outcome data be normally distributed. Standard errors were calculated on the basis of 5000 random subsamples (authors of the method recommend re-sampling at least 1000 times). We used a SAS macro called “indirect.” Another advantage of this approach is that it allows for adjustment for non-mediating covariates. Each analysis was adjusted for race/ethnicity; a factor we hypothesized was outside of the causal pathway between adverse childhood events and birth outcomes.
Results
Demographics are presented in Table 1. The study population was predominantly white (76 %) and Hispanic/other (17 %) and married or living with a partner (90 %). The average age was 31 and average number of years of education was over 15. The mean birth weight for infants born to women in the cohort was 3392 g (SD = 531.60) and mean gestational age was 38.71 weeks (SD = 1.71). Fifty percent of women reported experiencing at least one adverse childhood event prior to the age of 18: 21 % (n = 493) reported one, 11 % reported two and 17 % of women (n = 397) reported exposure to three or more adverse childhood events prior to the age of 18 (Table 1). The most common reported event was substance abuse by a parent (22 %), followed by sexual molestation/abuse (16 %).
Associations Between Mediators, Adverse Childhood Experiences and Pregnancy Outcomes
Correlations between mediators and adverse childhood experiences and outcomes are presented in Table 2. Adverse childhood experiences were strongly associated with many hypothesized mediators, most strongly with psychiatric disorders (major depressive episode, panic disorder, generalized anxiety disorder, and post-traumatic stress disorder), smoking and fewer years of education. Smoking and substance use were most strongly associated with lower birth weights and shorter gestations. Education was positively associated with birth weight. Psychiatric disorders as a group and individually were associated with shorter gestations and lower birth weights, with similar associations across disorders.
Mediation of the Association Between Adverse Childhood Experiences and Pregnancy Outcomes
Figure 2 shows direct and indirect c and c’ pathways and mediation estimates for adverse childhood experiences on birth weight and gestational age. Most of the effect of adverse childhood experiences on birth weight and gestational age were accounted for by the hypothesized mediating factors. An examination of birth weight and gestational age as continuous variables allowed for us to quantify the impact of ACEs in a manner that was clinically meaningful in the sense we could specify the impact on gestational age by week and birth weight by grams. In particular, for each additional adverse childhood event, birth weight decreased by 16.33 g, after accounting for race/ethnicity. After further adjustment for potential mediators, each unit increase in adverse childhood experiences, decreased birth weight by only 2.53 g. Viewed another way, the total decrease in birth weight attributable to adverse childhood experiences was 13.79 g. The pattern was similar for gestational weeks in that the mediators together explained most of the effect of adverse childhood experiences. After accounting for only race/ethnicity, there was a decrease in gestational weeks of 0.063 for each unit increase of adverse childhood experiences. The total decrease in the effect of adverse childhood experiences was 0.042 g.
Table 3 provides estimates for indirect effects of adverse childhood experiences on birth outcomes through each potential mediator. Smoking and substance use accounted for most of the differential effect of adverse childhood events on birth weight. Smoking in particular was a very strong mediator, accounting for 9.48 g of the total of 13.71 g (bias corrected) decrease in the effect of adverse childhood experiences after adjustment for all possible mediating factors. Pathways via psychiatric disorders, marital status, and use of a serotonin reuptake inhibitor were the next most common mediators. Smoking was also the strongest mediator of the effect of adverse childhood experiences on gestational age. Of the 0.041 week (bias corrected) decrease associated with adverse childhood experiences for gestational age, smoking accounted for 0.020 weeks, or slightly less than half of this differential effect. Psychiatric disorder was the next most common mediator followed by use of a serotonin reuptake inhibitor and education.
Discussion
To our knowledge, this is the first study to gather prospective data on pregnancy outcomes and examine gestational age at delivery and infant birth weight as they relate to a wide range of adverse childhood experiences. Our findings support two hypotheses that have been long suspected, but not adequately tested in the literature: (1) adverse childhood experiences themselves may result in adverse birth outcomes; (2) the health behaviors of people who have experienced adverse childhood experiences, are implicated in poor pregnancy outcomes and/or (3) adverse childhood experiences result for some in adverse birth outcomes mediated by psychiatric disorders and prenatal smoking. These mechanisms warrant further testing with future research that examines models where psychiatric disorders/mental health indicators are tested not only as outcomes, but also as mediating variables.
We found that adverse childhood experiences, which occurred in a woman’s life prior to the age of 18, seem to have a long-lasting impact on reproductive health, measured in our study as reduced birth weight and gestational age. In particular, it appears that adverse childhood experiences’ impact on birth outcomes explained nearly all of the estimated effects, and thus our data suggest that there may be minimal impact of other factors not examined. In our cohort, smoking was the main mechanism through which adverse childhood experiences in the mother affect birth outcomes.
Our study illustrates the importance of a wide range of childhood adversity on women’s reproductive health trajectories and the prevalence of adverse childhood experiences in a cohort of mostly Caucasian, college-educated, pregnant women. Although the sample is primarily Caucasian (24 % black/African American, Hispanic non-white) and thus the generalizability of our findings is limited, it is important to note that adverse childhood experiences were relatively common in this cohort of relatively middle class pregnant women (50 % of women in our cohort reported experiencing at least one adverse childhood event and 17 % reported at least 3).
While our study employed significant methodological improvements over past research, specifically gestational age determined by medical record review, prospective data on pregnancy outcomes, overall high retention rates, and the rigorous assessment of plausible mediators, there are limitations to our findings. We included many potential mediators of the relationship between adverse childhood experiences and birth outcomes in our analyses and as mentioned previously, the factors we examined did explain the majority of the effect of adverse childhood experiences on birth outcomes. It remains possible that there are additional pathways (e.g. maternal early socioeconomic status, self-esteem, social support [33], early parenting environment and genetic makeup) that we did not include that explain some of the additional effect. Additionally, it is possible, as is the case with many trauma inventories, that a family afflicted by a general medical illness may also manifest many of the variables listed in Table 1 leading to one overall traumatic experience for a family counted multiple times. However, as we note above, the number of traumatic events and type of events are comparable to other epidemiological samples, and as with any type of traumatic event inventory of early life, may result in over estimation of the effect of trauma by virtue of capturing the same traumatic event under different questions. This potential over estimation is balanced by that fact that although our overall retention rate in our cohort was high, an additional limitation is the inclusion in the analytic sample of women who were somewhat healthier with respect to PTSD than the full sample (differential attrition). This means that our findings may have underestimated the true effect of adverse childhood experiences on birth outcomes. The strength of psychiatric disorder as a mediator may have also been underestimated as a result. Due to the fact we examined birth weight and gestational age as continuous variables, we did not distinguish an overall effect of ACEs on low birth weight or preterm birth as compared to healthy birth weight and term infants. However, our classification of the outcome variables as continuous measures allowed for us to draw conclusions on the impacts of ACEs that quantify the total decrease in birth weight attributable to adverse childhood experiences (13.79 g).
Finally, our sample was not based on a probability sample, but rather a community sample of pregnant women seeking obstetrical care. Thus our results should be interpreted with the caution that they are representative only of a subset of pregnant, women seeking prenatal care and not a systematic epidemiological sample. Additionally, any retrospective reporting of early adverse childhood experiences is biased, yet we believe this bias in our study is not likely to occur differentially across groups (adverse birth outcomes vs. non adverse birth outcomes).
Because of its multiple pernicious effects on infant and child health, an understanding of the antecedents to smoking in pregnancy, such as early childhood adversity, is helpful in preventing adverse birth outcomes. Adverse childhood experiences should be considered as a life-course determinant of adult pregnancy outcomes and necessitate consideration in clinical models of prenatal and interconceptional care and future research on adverse pregnancy outcomes.
References
Fagundes, C., Glaser, R., Johnson, S., Andridge, R., Yang, E., DiGregorio, M., et al. (2012). Basal cell carcinoma: Stressful life events and the tumor environment. Archives of General Psychiatry, 69(6), 618–626.
Felitti, V., & Anda, R. (2009). The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: Implications for healthcare. In R. Lanius & E. Vermetten (Eds.), The hidden epidemic: The impact of early life trauma on health and disease. Cambridge: Cambridge University Press.
Shonkoff, J. P., Garner, A. S., The Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Child Adoption DC, & Section of Developmental and Behavioral Pediatrics. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), 232–246.
Danese, A., Moffitt, T. E., Harrington, H., Milne, B., Polanczyk, G., Pariante, C., et al. (2009). Adverse childhood experiences and adult risk factors for age-related disease. Archives of Pediatrics and Adolescent Medicine, 163(12), 1135–1143.
Springer, K., Sheridan, J., Kuo, D., & Carnesb, M. (2007). Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse and Neglect, 31, 517–530.
Mamun, A., Rosa, A., O’Callaghan, M., Hayatbakhsh, M., O’Callaghan, F., Najman, J., et al. (2011). Does childhood sexual abuse have an effect on young adults’ nicotine disorder (dependence or withdrawal)? Evidence from a birth cohort study. Addiction, 102, 647–654.
Anda, R. F., Chapman, D. P., Felitti, V. J., Edwards, V., Williamson, D. F., Croft, J. B., et al. (2002). Adverse childhood experiences and risk of paternity in teen pregnancy. Obstetrics and Gynecology, 100(1), 37–45.
Anda, R., Croft, J., Felitti, V., Nordenberg, D., Giles, W., Williamson, D., et al. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282, 1652–1658.
Hillis, S., Anda, R., Dube, S., Felitti, V., Marchbanks, P., & Marks, J. (2004). The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics, 113(2), 320–327.
Teicher, M., Andersen, S., Polcari, A., Anderson, C., & Navalta, C. (2002). Developmental neurobiology of childhood stress and trauma. Psychiatric Clinics of North America, 25(2), 397–426.
Felitti, V., Anda, R., Nordenberg, D., Williamson, D., Spitz, A., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258.
Dunkel Schetter, C., & Tanner, L. (2012). Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr Opin Psychiatry, 25(2), 141–148.
Dunkel Schetter, C. (2011). Pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology, 62, 531–558.
Benedict, M., Paine, L., Paine, L., Brandt, D., & Stallings, R. (1999). The association of childhood sexual abuse with depressive symptoms during pregnancy, and selected pregnancy outcomes. Child Abuse and Neglect, 23(7), 659–670.
Leeners, B., Stiller, R., Block, E., Görres, G., & Rath, W. (2010). Pregnancy complications in women with childhood sexual abuse experiences. Journal of Psychosomatic Research, 69(5), 503–510.
Grimstad, H., & Schei, B. (1999). Pregnancy and delivery for women with a history of child sexual abuse. Child Abuse and Neglect, 23(1), 81–90.
Jacobs, J. (1992). Victimization and later sequelae during pregnancy and childbirth. Journal of Child Sexual Abuse, 1(1), 103–112.
Seng, J., Low, L., Sperlich, M., Ronis, D., & Liberzonf, I. (2011). Post-traumatic stress disorder, child abuse history, birthweight and gestational age: A prospective cohort study. BJOG, 118(13), 1329–1339.
Noll, J. G., Schulkin, J., Trickett, P. K., Susman, E. J., Breech, L., & Putnam, F. W. (2007). Differential pathways to preterm delivery for sexually abused and comparison women. Journal of Pediatric Psychology, 32(10), 1238.
Chung, E. K., Nurmohamed, L., Mathew, L., Elo, I. T., Coyne, J. C., & Culhane, J. F. (2010). Risky health behaviors among mothers-to-be: The impact of adverse childhood experiences. Academic Pediatrics, 10(4), 245–251.
Möhler, E., Matheis, V., Marysko, M., Finke, P., Kaufmann, C., Cierpka, M., et al. (2008). Complications during pregnancy, peri- and postnatal period in a sample of women with a history of child abuse. Journal of Psychosomatic Obstetrics and Gynecology, 29(3), 193–198.
Chung, E., Mathew, L., Elo, I., et al. (2008). Depressive symptoms in disadvantaged women receiving prenatal care: The influence of adverse and positive childhood experiences. Ambulatory Pediatrics, 8(2), 109–116.
Farber, E., Herbert, S., & Reviere, S. (1996). Childhood abuse and suicidality in obstetric patients in a hospital-based urban prenatal clinic. General Hospital Psychiatry, 18, 56–60.
Lukasse, M., Schei, B., Vangen, S., & Oian, P. (2009). Childhood abuse and common complaints in pregnancy. Birth, 36(3), 190–199.
Greenfield, E. (2010). Childhood sexual abuse as a life-course social determinnant of adult health. Maturitas, 66(66), 51–55.
Seng, J., Sperlich, M., & Low, L. (2008). Mental health, demographic, and risk behavior profiles of pregnant survivors of childhood and adult abuse. Journal of Midwifery and Women’s Health, 53(6), 511–521.
Yonkers, K. A., Norwitz, E. R., Smith, M. V., Lockwood, C. J., Gotman, N., Luchansky, E., et al. (2012). Depression and serotonin reuptake inhibitor treatment as risk factors for preterm birth. Epidemiology, 23(5), 677–685.
Kessler, R., & Ustun, T. B. (2004). The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). The International Journal of Methods in Psychiatric Research, 13(2), 93–121.
Falsetti, S., Resnick, H., Pesick, P., & Kilpatrick, D. (1993). The modified PTSD symptom scale: A brief self-report measure of posttraumatic stress disorder. Behavior Therapist, 16, 161–162.
Bremner, J. D. (2007). Neuroimaging in posttraumatic stress disorder and other stress-related disorders. Neuroimaging Clinics of North America, 17(4), 523.
Preacher, K., & Hayes, A. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers, 36, 717–731.
MacKinnon, D., Lockwood, C., Hoffman, J., West, S., & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104.
Hill, T. D., Kaplan, L. M., French, M. T., & Johnson, R. J. (2010). Victimatization in early life and mental health in adulthood: An examination of the mediating and moderating influences of psychosocial resources. Journal of Health and Social Behavior, 51(1), 48–63.
Acknowledgments
Author received Grants K12 DA031050 (Smith) and R01 HD045735 (Yonkers) from the National Institute of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Yonkers has the following conflicts to disclose: she has received study medication from Pfizer for an NIMH trial and has received royalties from Up to Date. All other investigators do not have any conflicts of interest.
Rights and permissions
About this article
Cite this article
Smith, M.V., Gotman, N. & Yonkers, K.A. Early Childhood Adversity and Pregnancy Outcomes. Matern Child Health J 20, 790–798 (2016). https://doi.org/10.1007/s10995-015-1909-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1909-5