Abstract
To examine whether an excess risk of maternal mortality exists among migrant women in Western Europe. We searched electronic databases for studies published 1970 through 2013 for all observational studies comparing maternal mortality between the host country and a defined migrant population. Results were derived from a random-effects meta-analysis, and statistical heterogeneity assessed by the I 2 statistic. In sub-analyses we also calculated summary estimates stratified by direct and indirect death causes. We included 13 studies with more than 42 million women and 4,995 maternal deaths. Compared with indigenous born women, the pooled risk estimate (RR) was 2.00 with 95 % confidence interval (CI) of 1.72, 2.33. Migrant women had a non-significantly higher risk of dying from direct than indirect death causes; pooled RRs of 2.65 CI 1.88, 3.74 and 1.83 CI 1.37, 2.45. This meta-analysis provides evidence that migrant women in Western European countries have an excess risk of maternal mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maternal mortality, defined as the death of a woman during pregnancy or within 42 days of delivery [1], is a principal indicator of maternal health and a marker of the quality of and access to maternal health care. The rapid decrease in maternal mortality in developed countries [2] and, to a lesser extent, in developing countries [3], has been ascribed to improved quality of antenatal care and obstetric techniques and services [4]. Despite the fact that Western European countries have some of the lowest maternal mortality rates in the world [3], progress in further decreasing maternal mortality has been uneven, and inequity continues to exist, not only between but also within countries [5, 6]. Regardless of an increased risk of pregnancy complications that can progress to maternal mortality in the migrant population, Western host countries have the capacity to offer to women of all ethnicities and nations, the availability and utilization of timely and adequate obstetrical care [7]. Although universal or partially universal health care systems with similar entitlements to legal migrants have a potential to eliminate some access barriers to maternal care [8] other aspects remain unexplored.
The majority of Western European countries have health care organizations which are based on universal or partly universal access to health care with similar entitlements to legal immigrants as the non-immigrant population, and for that reason it is of particular interest to conduct a quantitative assessment of whether an excess risk of maternal mortality exist among migrant women in Western Europe. Hence, we undertook a meta-analysis of all published observational studies from Western European countries comparing the risk of maternal mortality between the receiving country women and a defined migrant population.
Methods
Search Strategy
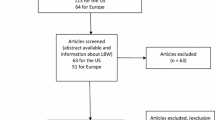
We conducted the meta-analysis in accordance with the guidelines for Meta-analysis of Observational Studies in Epidemiology (MOOSE) [9]. We searched electronic databases; Medline (1970–2013), EMBASE (1974–2013), Cochrane Library (1970–2013) and CINAHL (1981–2013) for papers with restriction to English language and human studies. The following MeSH and EMTREE search terms was used with and without restrictions: (Ethnic OR ethnic group OR migrant OR immigrant OR minority OR disparity OR “foreign nationality” OR “foreign nationals”) AND (“maternal mortality” OR “pregnancy-related mortality” OR “pregnancy-related death” OR “maternal deaths”). Title and abstract of the found studies were reviewed, and if found eligible for further investigation the entire paper was extracted (Fig. 1). Reference lists of the 28 extracted studies were screened and personal contacts were made with authors and experts within the field. The search strategy was independently assessed by two reviewers. In case of disagreement on title or abstract, the full text of the papers was retrieved and discussed.
Inclusion and Exclusion Criteria
We included studies if they met the following criteria; published 1970 through April 2013 in the English language, conducted in Western European countries as defined by the United Nations [10]; observational study design comparing the risk of maternal mortality of the host country or majority population with that for a defined foreign-born population; reported relative risks (RR) or odds ratios (OR) with 95 % confidence intervals (CI), or data to calculate these.
Data Extraction
Data extraction was also independently assessed by two reviewers any disagreements were resolved by consensus. From each retrieved article we extracted the following: year of publication, country of origin, study design, study period, definition of the included study populations, definition of maternal mortality, total number of women, total number of cases and subgroups of direct and indirect cases, confounders, and the mortality rates, mortality ratios, relative risks, or odds ratios with corresponding 95 % CI’s or standard errors (SE). If papers had inadequate information on either sample size or confidence limits we contacted the corresponding authors with a request for additional data.
Classification of Maternal Mortality
Maternal mortality is according to the World Health Organization (WHO) defined as—death of women during pregnancy, childbirth, or in the 42 days after delivery [11]. All studies, except one [12], had defined maternal deaths based on the International Classification of Diseases (ICD) codes (Table 1). ICD-classifications changed during the included study period (1969–2008) from ICD-8 over ICD-9 to the latest ICD-10. The ICD-9 and ICD-10 reclassified the subgroups of direct (obstetric causes) and indirect (causes aggravated by pregnancy) causes, as well as early postpartum (<42 days after childbirth) and late postpartum (42–356 days after childbirth) maternal death and an additional category of coincidental (fortuitous) deaths [13]. Despite changes, all main codes of maternal mortality remained the same. Seven of the included studies also reported late post-partum deaths (see Table 2). The most common denominator used throughout the included studies was the total number of pregnancies associated with a live birth. Seven studies reported pregnancies both associated with still and live births [8, 12, 14–17].
Migrant Women
The definition of migrants and the countries of origin used in the individual studies are provided in Table 2. Migrant women were defined by a different country of origin or nationality than the receiving country women. Nine studies had defined women by their specific country of origin or nationality. Four studies had defined the women based on country of birth, divided into White and non-White subgroups. Despite heterogeneity in the composition of migrant women, all studies had included a clear division into receiving country nationality (majority population) and a defined migrant (minority) population.
Statistical Analysis
We pooled risk ratio (OR or RR) estimates and 95 % CIs from each study for maternal mortality using a random-effects meta-analysis. Because maternal mortality is a rare event, we treated odds ratios as an approximation of the risk ratio. The statistical heterogeneity between the studies was assessed by calculation of the I 2 statistics quantified by low (25 %), moderate (50 %) and high (75 %) degree of heterogeneity [19]. To further accommodate the heterogeneity between studies we also added the prediction interval (PI). The PI provides a predicted range for the effect of the exposure in an individual study, and is perceived to have a better appreciation of the uncertainty around the effect estimate [20, 21].
Publication bias was assessed by plotting the point estimate against the SE for each study in a funnel asymmetry plot and by performing the Egger asymmetry test [22].
In sub-analyses we ran separate pooled analyses of direct deaths and indirect death causes. We also calculated the pooled relative risks, dividing studies into two roughly different time periods: (1) 1969–1995 and (2) 1996–2008. Two of the included studies [23, 24] had subdivided data into several additional time periods, and these periods were use in the analyses stratified by periods. Some of the studies had slightly overlapping time periods, and one study period ranged from 1991 to 1999 and was despite overlap included in the second time period.
To assess the absolute difference in maternal mortality between host country and foreign-born women across all studies we calculated an absolute risk difference (RD) including a CI using the formula; RD = maternal mortality incidence × (pooled RR − 1) [25]. The maternal mortality incidence (average 8.7/100,000 per year) was calculated from all the included countries combined from 4 time points (1980, 1990, 2000, 2008) based on data from Hogan et al. [3] The average combined incidence varied from 7/100,000 to 20/100,000 maternal deaths per year from 1980 to 2008.
We ran a number of sensitivity analyses.
First we assessed whether pooled estimates could have been markedly affected by a single study by excluding studies one at a time to assess changes in the pooled estimate. Also results were repeated using a fixed-effects model to test differences between the random and fixed effect results to explore heterogeneity across studies. Further separate meta-regression analyses were conducted to assess differences in between study variance that might be explained by selected categorical covariates; study period and design. All statistical analyses were conducted in STATA version 12 (Stata Corp, College Station, TX).
Results
Search Strategy
The detailed steps of the literature search are shown in Fig. 1. We retrieved a total of 558 studies, of which title and abstract was searched. Of these, 28 papers were identified for full examination. After full review, 18 studies were further excluded; ten did not include data on migrant status or only included racial categories, six were duplicate studies reporting on the same cases [26–31], one study was a short communication [32] and one was a case-fatality study [33]. From a careful search of all references we found four additional reports (Confidential Enquiries) on maternal mortality. Data from three of these reports were further included [8, 14, 16], one report had to be excluded due to inadequate denominator data [33]. Thirteen final studies were included in the meta-analysis; five nationwide register studies [23, 24, 35–36], six Confidential Enquiries [8, 14–16, 38, 39] and two national case–control studies [12, 17] which had sampled controls from national representative cohorts (Table 2).
Study Characteristics
Across all studies, there were a total of 3,764 maternal deaths among 36,187,991 host country births and 1,231 maternal deaths among 6,102,663 migrant births (Table 2). Included studies had been conducted in England (5), The Netherlands (2), Germany (2), France (2), Spain (1) and Switzerland (1) during the period from 1969 to 2008. The migrant composition, as described in the studies was a mix of labor immigrants, refugees, asylum seekers, and family reunified women. Some of the largest immigrant groups that recurred between the included studies were immigrant of Turkish, North and Sub-Saharan African- and Far East-Asian origin. Three studies had adjusted for different confounding factors; maternal age, year of death, marital status, work status, hospitalization during pregnancy, autonomous region. Whereas the remaining majority of studies provided only crude risk estimates.
Maternal Mortality
Migrant women had a higher risk of maternal mortality than non-migrants, with a pooled risk estimate (RR) of 2.00 CI 1.72, 2.33. A high degree of heterogeneity was observed among the studies (I 2 = 78.1 %, p < 0.001) (Fig. 2). Substantial heterogeneity resulted in a wide PI of: 1.16–3.44. Based on the pooled relative risk and a combined maternal mortality incidence in the countries included, we estimated the RD of 9 additional maternal deaths per 100,000 deliveries (live births) per year for migrant women (CI 5.9, 15.2).
Relative risk of maternal mortality comparing migrant to non-migrant women. The summary estimates were obtained using a random-effects model. The data markers the relative risks (RRs) with 95 % confidence intervals. The size of the data markers indicates the weight of the study. The diamond data marker indicates the pooled RR. The prediction interval is shown with lines extending from the diamond
The 13 studies were reasonably symmetrically distributed around the summary estimate in the funnel plot (Fig. 3). Egger’s test of asymmetry was none significant (p = 0.77).
From seven of the included studies we were able to further extract data on underlying direct death causes [8, 15, 16, 23, 35, 39, 40] and from six of these (excluding Ibison et al.) also indirect deaths causes. Direct death causes were primarily from hypertensive disorders with the largest proportion due to pre-eclampsia/eclampsia. Also deep vein thrombosis and pulmonary embolisms was described as main causes of direct maternal deaths. Indirect deaths causes were not further categorized in the included studies. Analysis showed a higher risk of dying from direct causes pooled RR of 2.65 CI 1.88, 3.74 (I 2 = 82.1 %, p < 0.0001), when compared with indirect causes pooled RR 1.83 CI 1.37, 2.45 (I 2 = 57.9 %, p = 0.037), (Figs. 4, 5).
Relative risk of maternal mortality from direct death causes comparing migrant to non-migrant women. The summary estimates were obtained using a random-effects model. The data markers the relative risks (RRs) with 95 % confidence intervals. The size of the data markers indicates the weight of the study. The diamond data marker indicates the pooled RR. The prediction interval is shown with lines extending from the diamond
Relative Risk of maternal mortality from indirect death causes comparing migrant to non-migrant women. The summary estimates were obtained using a random-effects model. The data markers the relative risks (RRs) with 95 % confidence intervals. The size of the data markers indicates the weight of the study. The diamond data marker indicates the pooled RRs. The prediction interval is shown with lines extending from the diamond
We found a small difference in the pooled summary estimates when divided into two time periods, yet with overlapping CIs. Studies undertaken in the first time period (1969–1995) had a pooled RR of 1.81 CI 1.30, 2.51, with a high degree of heterogeneity (I 2 = 88.9, p < 0.001), whereas studies conducted in the second time period (1996–2008) had a pooled RR of 2.04 CI 1.75, 2.37, with a medium degree of heterogeneity (I 2 = 52.2, p = 0.022) (Supplementary Figure 6 & 7). A formal test of time period in a meta-regression analysis showed no difference.
Sensitivity Analyses
Repeating the meta-analysis with a fixed-effects model did not change the overall results RR of 2.02 CI 1.89, 2.15. Removal of the individual studies separately did not considerably influence the pooled summary estimate (Supplementary Table 1). Excluding the three studies which had included covariates did not appreciably change the overall summary estimate RR of 2.05 CI 1.72, 2.45, (I 2 = 77.0, p < 0.0001).
Further separate meta-regression analyses including study design as a covariate showed that pooled estimates from Confidential Enquiries (p = 0.07) and case–control studies (p = 0.37) were higher than pooled results from register studies, though not significantly.
Discussion
The main findings of this meta-analysis showed that migrant women in Western European countries have a doubled risk of dying during or after pregnancy when compared with indigenous born women, corresponding to an estimated absolute additional risk of 9 maternal deaths per 100,000 deliveries among migrant women per year. Results also indicated that migrants may have a higher risk of dying from direct as oppose to indirect causes.
Globally, the two most common pregnancy complications and causes of maternal deaths according to WHO are hemorrhage and hypertensive disorders [7], though only life-threatening if not treated in a timely and adequate manner. An excess risk of maternal death from both disorders (direct causes of death), has been found among immigrant women in France, Germany and The Netherlands [12, 32, 37]. Our separate pooled analysis of direct deaths causes showed a two and a half times increased risk of maternal mortality among migrants, and an almost double excess risk from indirect causes. A predominance of direct causes of death could suggest that substandard obstetric care is responsible for the excess mortality among migrants, whereas indirect deaths may be more an indicator of the health status of the conceiving women. This subdivision may be especially important with respect to migrant women coming from countries where indirect death causes (e.g. malaria, tuberculosis, anemia) is a serious concern [41]. Even though fewer studies were included in these sub-analyses, this gives us an indication that an excess risk may be caused by differences in maternal care. Despite the fact that the majority of Western European countries have more or less universal health care systems [30, 42, 18], lack of access to timely and high quality obstetrical care has been identified as one of the primary causes of maternal mortality globally [7]. Inadequate follow-up during pregnancy, poorer quality of services and undiagnosed symptoms both pre- and post-partum has been found among migrants [12, 32, 43–45]. Results from a Confidential Enquiries conducted in England [14] found that nearly half of the women who booked antenatal care late (beyond 20 weeks) or were poor attendees were from an ethnic minority group. Especially language and communication barriers have been suggested as a key obstacle leading to substandard antenatal care [43, 46, 47]. However, the increased risk of death among migrant women may be due in part to increased incidence of different diseases and pre-pregnancy health [48]. Women from some parts of the world, and especially from subtropical Africa are more often anemic, chronically malnourished, grand multipara, hypertensive, or have had multiple caesarean sections, all factors that can have fatal consequences in subsequent pregnancies [41].
Generally, the highest risks within studies were seen among the most recent migrant groups, most often of non-European nationality, while lower risk was seen among less recent migrants and migrants from middle and high-income countries. The latter group are known to have overall better language skills including use and knowledge of the health care system [23, 49]. Knowledge of and utilization of antenatal care may well be one of the main underlying causes of the observed excess risk. Insufficient knowledge in labor situations have show to lead to misjudgments or an elevated percentage of unnecessary caesarean section [50]. An increased fear of dying from anesthesia has been shown to refrain immigrant women from seeking medical advice for obstetrical problems [51].
Also, a higher frequency of unwanted or unplanned pregnancies [52], unassisted births and home deliveries may explain part of the found differences [12, 30]. Although we know the country of origin of the women we do not know the underlying migrant type. Asylum seekers, undocumented migrants and trafficking women may constitute particular vulnerable groups.
Methodological Considerations
All the included studies were national studies drawing from the source population of all births during the study period, yielding a very large total sample size of more than 42 million births and over 4,900 maternal deaths. The measures of maternal mortality in all studies were derived from high quality civil registration systems with routine registration of birth and death. Despite some variation in data source and linkage between countries, vital registration is one of the best measures of maternal mortality [3]. All studies, except the two case–control studies, were nationwide and all were conducted in large Western European countries, and data may well be a reasonable approximation of the status of reproductive health among migrants in Western Europe.
This meta-analysis has limitations that need attention. We found a high degree of heterogeneity between studies, which could be explained by different factors. Heterogeneity may have been caused by differences in the definition of migrants (nationality vs. ethnicity) and the individual proportion of migrants and migrant types between the included studies and also over time. Interpretation of PIs did not change the overall conclusion of the meta-analysis. However, it should be noted that we observed substantial overlap of PIs between the different subgroups analyses.
Recent trends within countries have shown a more favorable decline in maternal mortality rates among native-born as compared to immigrant women [12, 23, 37]. Our stratified analysis of time periods leads in the same direction, despite a non-significant effect of time period. We saw a lower degree of heterogeneity among studies in the second time period, which could be explained by less between-country variation in the more recent studies.
It has been found that migrants of certain countries fare less well of than others [53]. Unfortunately, data were too scarce to be able to pool the data by specific immigrant subgroups. Thus, further evaluation of effect modification by i.e. immigrant sub-group is needed from large individual participant pooled analyses. Also, research suggest that host country receiving policies affect migrant reproductive health outcomes [54]. We acknowledge that integrations policies and actual utilization of the health care systems during pregnancy and birth could account for a significant proportion of the observed between study heterogeneity. We were unfortunately not able to evaluate the effect of these factors, but a side from this we still argue that the overall notion of migrant women as compared with host country women may well apply between countries, despite dissimilarities.
Even though the main death codes remained the same across ICD-8, 9 and 10, changes in coding practices could have affected maternal mortality rates across time. Studies from the US [55] and Europe [40] did find that changes in ICD-codes and especially the inclusion of late death increased maternal death rates. Nevertheless, on average in ICD-10 <2 % of maternal deaths are coded as late maternal deaths [3], and there is no reason to assume that coding changes should specifically have been related to migrants status.
General underreporting of maternal mortality has been found in several European countries [26, 40, 43]. The observed changes in risk over time could potentially be explained by underreporting of maternal mortality in the earliest study years. In Germany a lack of accuracy in linking death and pregnancy has been found [37]. Generally, linkage may also have missed women who died after a birth that occurred outside the country. Also, delayed prenatal care among migrants [56] may influence correct assigned pregnancy status on death records [57].
Generally, Confidential Enquiries have shown to report higher rates of maternal mortality than those based on death certificates alone [16]. Potential underreporting of maternal mortality rates in the register and case–control studies, especially among migrants, would have led us to underrate the true excess risk among migrant women. Nonetheless, we did not see significant differences between study designs when running a meta-regression with study design included as a covariate. In relation to this, estimated RDs were calculated from an average incidence of maternal mortality based on data from 1980 to 2008 [3]. Since trends in mortality rates have shown a steadily decline in most studies during the included study period, RDs may be slightly underestimated due to exclusion of the earliest years (1969–1980).
Our pooled risk estimate fail to account for potential confounding factors, such as higher parity, older ages at childbirth and lower socioeconomic status among migrant women. Excluding studies including covariates did not notably change the overall pooled estimate.
Despite little evidence of publication bias, we cannot eliminate this type of bias, since non-included data from unpublished studies, grey literature, non-English language studies and potentially missed studies could have influenced findings. It should be noted that five of the studies has been conducted in the UK and an overrepresentation of UK in total number of deaths may have influenced our findings. Nonetheless, the large sample size makes it less likely that the overall findings would be changed by additional studies.
Overall, these findings give an accurate picture of the size of the level of differences in maternal mortality among migrant in Western Europe. As maternal deaths represent the tip of the iceberg of disease; a much larger number of women suffer from so called “near-miss” morbidity [58]. Studies have also shown strong ethnic disparities in maternal morbidity [59–61], and combining studies of “near-miss” maternal mortality can complement enquiries into maternal death and assist to investigate risk factors for both the occurrence of disease and progression to death and other severe complications.
Conclusion
In summary, this meta-analysis showed that immigrant women in Western European countries have a doubled risk of dying during or after pregnancy when compared with indigenous born women. We also observed indications of a higher risk of deaths from direct causes, which point towards that substandard obstetric care, may be responsible for the majority of the excess deaths among migrant women. As most of these deaths are preventable, it is an urgent matter to pinpoint the underlying direct causes and institute programs to prevent unnecessary deaths to vulnerable immigrant women. Better use of registry data to look at specific death causes, especially the timing of deaths, to identify modifiable risk factors of health care practices are of high importance.
References
Say, L., Pattinson, R. C., & Gulmezoglu, A. M. (2004). WHO systematic review of maternal morbidity and mortality: The prevalence of severe acute maternal morbidity (near miss). Reproductive Health, 1(1), 3.
Salanave, B., Bouvier-Colle, M. H., Varnoux, N., et al. (1999). Classification differences and maternal mortality: A European study. MOMS Group. MOthers’ Mortality and Severe morbidity. International Journal of Epidemiology, 28(1), 64–69.
Hogan, M. C., Foreman, K. J., Naghavi, M., et al. (2010). Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet, 375(9726), 1609–1623.
De Brouwere, V., Tonglet, R., & Van Lerberghe, W. (1998). Strategies for reducing maternal mortality in developing countries: What can we learn from the history of the industrialized West? Tropical Medicine & International Health, 3(10), 771–782.
Tobias, M., & Jackson, G. (2001). Avoidable mortality in New Zealand, 1981–97. Australian and New Zealand Journal of Public Health, 25(1), 12–20.
Levine, R. S., Foster, J. E., Fullilove, R. E., et al. (2001). Black-white inequalities in mortality and life expectancy, 1933–1999: Implications for healthy people 2010. Public Health Reports, 116(5), 474–483.
Paxton, A., & Wardlaw, T. (2011). Are we making progress in maternal mortality? New England Journal of Medicine, 364(21), 1990–1993.
Lewis, G. (2012). Saving Mothers’ Lives: The continuing benefits for maternal health from the United Kingdom (UK) confidential enquires into maternal deaths. Seminars in Perinatology, 36(1), 19–26.
Stroup, D. F., Berlin, J. A., Morton, S. C., et al. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA, 283(15), 2008–2012.
Nations U. (2013). In geographical region and composition. United Nations Statistics Division. http://unstats.un.org/unsd/methods/m49/m49regin.htm Accessed 9-10-2013.
WHO U, UNFPA, & The World Bank. (2007). Maternal mortality in 2005. WHO Library Cataloguing-in-Publication Data.
Philibert, M., Deneux-Tharaux, C., & Bouvier-Colle, M. H. (2008). Can excess maternal mortality among women of foreign nationality be explained by suboptimal obstetric care? BJOG, 115(11), 1411–1418.
WHO. (1993). International statistical classification of diseases, and related health problems, 10th revision (ICD-10). Geneva: World Health Organization.
Lewis, G., & Drife, J. (2001). Why mothers die 1997–1999: The confidential enquiries into maternal deaths in the United Kingdom. London.
Lewis, G., & Drife, J. (2004). Why mothers die 2000–2002, the sixth report of the confidential enquiries into maternal deaths in the United Kingdom. London.
Lewis, G. (2007). The Confidential Enquiry into Maternal and Child Health (CEMACH). Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer-2003–2005. In The seventh report on confidential enquiries into maternal deaths in the United Kingdom. London.
Saucedo, M., Deneux-Tharaux, C., & Bouvier-Colle, M. H. (2012). Understanding regional differences in maternal mortality: A national case-control study in France. BJOG: An International Journal of Obstetrics and Gynaecology, 119(5), 573–581.
Cantwell, R., Clutton-Brock, T., Cooper, G., et al. (2011). Saving mothers’ lives: Reviewing maternal deaths to make motherhood safer: 2006–2008. The eighth report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG, 118(Suppl 1), 1–203.
Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558.
Chiolero, A., Santschi, V., Burnand, B., et al. (2012). Meta-analyses: With confidence or prediction intervals? European Journal of Epidemiology, 27(10), 823–825.
Egger, M., Davey Smith, G., Schneider, M., et al. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634.
Bollini, P., Wanner, P., & Pampallona, S. (2011). Trends in maternal mortality in Switzerland among Swiss and foreign nationals, 1969–2006. International Journal of Public Health, 56(5), 515–521.
Welsch, H., Krone, H. A., & Wisser, J. (2004). Maternal mortality in Bavaria between 1983 and 2000. American Journal of Obstetrics and Gynecology, 191(1), 304–308.
Murad, M. H., Montori, V. M., Walter, S. D., et al. (2009). Estimating risk difference from relative association measures in meta-analysis can infrequently pose interpretational challenges. Journal of Clinical Epidemiology, 62(8), 865–867.
Schutte, J. M., Steegers, E. A., Schuitemaker, N. W., et al. (2010). Rise in maternal mortality in the Netherlands. BJOG, 117(4), 399–406.
Luque Fernandez, M. A., Bueno Cavanillas, A., & de Mateo, S. (2010). Excess of maternal mortality in foreign nationalities in Spain, 1999–2006. European Journal of Obstetrics & Gynecology and Reproductive Biology, 149(1), 52–56.
Fassler, M. Z. R., & Quack Lotscher, K. C. (2010). Maternal mortality in Switzerland 1995–2004. Swiss Medical Weekly, 140(1–2), 25–30.
Deneux-Tharaux, C. P. M., & Bouvier-Colle, M.-H. (2009). Excess maternal mortality among foreign women in France and quality of obstetric care: A national study 1996–2001. Bulletin épidémiologique hebdomadaire, 9(3), 77–80.
Stirbu, I., Kunst, A. E., Bos, V., et al. (2006). Differences in avoidable mortality between migrants and the native Dutch in The Netherlands. BMC Public Health, 6, 78.
Marmot, M. G., Adelstein, A. M., & Bulusu, L. (1984). Immigrant mortality in England and Wales 1970–1978. London: Her Majesty's Stationery Office (HMSO).
van Roosmalen, J., Schuitemaker, N. W., Brand, R., et al. (2002). Substandard care in immigrant versus indigenous maternal deaths in The Netherlands. BJOG, 109(2), 212–213.
Zwart, J. J., Richters, J. M., Ory, F., et al. (2008). Severe maternal morbidity during pregnancy, delivery and puerperium in the Netherlands: A nationwide population-based study of 371,000 pregnancies. BJOG, 115(7), 842–850.
Lewis, G., & Drife, J. (1998). Why mothers die 1994–1996: Report on confidential enquiries into maternal deaths in the United Kingdom. London.
Ibison, J. M., Swerdlow, A. J., Head, J. A., et al. (1996). Maternal mortality in England and Wales 1970–1985: An analysis by country of birth. British Journal of Obstetrics and Gynaecology, 103(10), 973–980.
Luque Fernandez, M. A., Bueno Cavanillas, A., & de Mateo, S. (2010). Excess of maternal mortality in foreign nationalities in Spain, 1999–2006. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 149(1), 52–56.
Razum, O., Jahn, A., Blettner, M., et al. (1999). Trends in maternal mortality ratio among women of German and non-German nationality in West Germany, 1980–1996. International Journal of Epidemiology, 28(5), 919–924.
Schuitemaker, N., van Roosmalen, J., Dekker, G., et al. (1998). Confidential enquiry into maternal deaths in The Netherlands 1983–1992. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 79(1), 57–62.
de Graaf, J. P., Schutte, J. M., Poeran, J. J., et al. (2012). Regional differences in Dutch maternal mortality. BJOG, 119(5), 582–588.
Deneux-Tharaux, C., Berg, C., Bouvier-Colle, M. H., et al. (2005). Underreporting of pregnancy-related mortality in the United States and Europe. Obstetrics and Gynecology, 106(4), 684–692.
Ronsmans, C., & Graham, W. J. (2006). Maternal mortality: Who, when, where, and why. Lancet, 368(9542), 1189–1200.
Hjern, A., Haglund, B., Persson, G., et al. (2001). Is there equity in access to health services for ethnic minorities in Sweden? European Journal of Public Health, 11(2), 147–152.
Atri, J., Falshaw, M., Linvingstone, A., et al. (1996). Fair shares in health care? Ethnic and socioeconomic influences on recording of preventive care in selected inner London general practices. Healthy Eastenders Project. BMJ, 312(7031), 614–617.
Essen, B., Hanson, B. S., Ostergren, P. O., et al. (2000). Increased perinatal mortality among sub-Saharan immigrants in a city-population in Sweden. Acta Obstetricia et Gynecologica Scandinavica, 79(9), 737–743.
Almeida, L. M., Caldas, J., Ayres-de-Campos, D., et al. (2013). Maternal healthcare in migrants: A systematic review. Maternal and Child Health Journal, 17(8), 1346–1354.
Saastad, E., Vangen, S., & Froen, J. F. (2007). Suboptimal care in stillbirths—a retrospective audit study. Acta Obstetricia et Gynecologica Scandinavica, 86(4), 444–450. doi:10.1080/00016340701207724778247970.
Bouvier-Colle, M. H., Varnoux, N., Salanave, B., et al. (1997). Case-control study of risk factors for obstetric patients’ admission to intensive care units. European Journal of Obstetrics & Gynecology and Reproductive Biology, 74(2), 173–177.
Filippi, V., Ronsmans, C., Campbell, O. M., et al. (2006). Maternal health in poor countries: The broader context and a call for action. Lancet, 368(9546), 1535–1541.
Esscher, A., Haglund, B., Hogberg, U., et al. (2012). Excess mortality in women of reproductive age from low-income countries: A Swedish national register study. European Journal of Public Health, 23(2), 274–279.
Bragg, R. (2008). Maternal deaths and vulnerable migrants. Lancet, 371(9616), 879–881.
Essen, B., Johnsdotter, S., Hovelius, B., et al. (2000). Qualitative study of pregnancy and childbirth experiences in Somalian women resident in Sweden. BJOG, 107(12), 1507–1512.
Alderliesten, M. E., Vrijkotte, T. G., van der Wal, M. F., et al. (2007). Late start of antenatal care among ethnic minorities in a large cohort of pregnant women. BJOG, 114(10), 1232–1239.
Higgins, J. P., Thompson, S. G., & Spiegelhalter, D. J. (2009). A re-evaluation of random-effects meta-analysis. Journal of the Royal Statistical Society Series A, 172(1), 137–159.
Small, R., Gagnon, A., Gissler, M., et al. (2008). Somali women and their pregnancy outcomes postmigration: Data from six receiving countries. BJOG: An International Journal of Obstetrics and Gynaecology., 115(13), 1630–1640.
Bollini, P., Pampallona, S., Wanner, P., et al. (2009). Pregnancy outcome of migrant women and integration policy: A systematic review of the international literature. Social Science and Medicine, 68(3), 452–461.
Hoyert, D. L. (2007). Maternal mortality and related concepts. Vital & Health Statistics 3, 33, 1–13.
Delvaux, T., Buekens, P., Godin, I., et al. (2001). Barriers to prenatal care in Europe. American Journal of Preventive Medicine, 21(1), 52–59.
Elebro, K., Roost, M., Moussa, K., et al. (2007). Misclassified maternal deaths among East African immigrants in Sweden. Reproductive Health Matters, 15(30), 153–162.
Tuncalp, O., Hindin, M. J., Souza, J. P., et al. (2012). The prevalence of maternal near miss: A systematic review. BJOG: An International Journal of Obstetrics and Gynaecology, 119(6), 653–661.
Jonkers, M., Richters, A., Zwart, J., et al. (2011). Severe maternal morbidity among immigrant women in the Netherlands: Patients’ perspectives. Reproductive Health Matters, 19(37), 144–153.
Urquia, M. L., Ying, I., Glazier, R. H., et al. (2012). Serious preeclampsia among different immigrant groups. Journal of Obstetrics and Gynaecology Canada, 34(4), 348–352.
Small, M. J., James, A. H., Kershaw, T., et al. (2012). Near-miss maternal mortality: Cardiac dysfunction as the principal cause of obstetric intensive care unit admissions. Obstetrics and Gynecology, 119(2 Pt 1), 250–255.
Acknowledgments
This work was funded by The Health Insurance Foundation (Grant No. 2009B071) and The Oticon Foundation.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10995_2013_1403_MOESM2_ESM.pptx
Figure 6. Relative Risk of maternal mortality comparing migrant to non-migrant women in the first time period from 1969-1995. The summary estimates were obtained using a random-effects model. The data markers the relative risks (RRs) with 95 % confidence intervals. The size of the data markers indicates the weight of the study. The diamond data marker indicates the pooled RRs. The prediction interval is shown with lines extending from the diamond. (PPTX 68 kb)
10995_2013_1403_MOESM3_ESM.pptx
Figure 7. Relative Risk of maternal mortality comparing migrant to non-migrant women in the second time period from 1996-2008. The summary estimates were obtained using a random-effects model. The data markers the relative risks (RRs) with 95 % confidence intervals. The size of the data markers indicates the weight of the study. The diamond data marker indicates the pooled RRs. The prediction interval is shown with lines extending from the diamond. (PPTX 69 kb)
Rights and permissions
About this article
Cite this article
Pedersen, G.S., Grøntved, A., Mortensen, L.H. et al. Maternal Mortality Among Migrants in Western Europe: A Meta-Analysis. Matern Child Health J 18, 1628–1638 (2014). https://doi.org/10.1007/s10995-013-1403-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-013-1403-x