Abstract
Previous studies have shown that birth weight and other birth characteristics may be associated with risk for type 2 diabetes and cardiovascular disease (CVD) later in life; however, results using large US national survey data are limited. Our goal was to determine the aforementioned associations using nationally representative data. We studied children and adolescents 6–15 years using data from the National Health and Nutrition Examination Survey cycles 2001–2010. Survey and examination data included demographic and early childhood characteristics, current health status, physical activity information, anthropometric measurements, dietary data (total energy, saturated fat, sodium, and sugar intakes), biomarkers related to selected risk factors of CVD [systolic blood pressure (SBP), plasma C-reactive protein (CRP) and lipid profiles], and type 2 diabetes [fasting glucose, insulin, and homeostasis model assessment (HOMA)]. Birth weight (proxy-reported) was inversely associated with SBP among girls; SBP levels increased 1.4 mmHg for each 1,000 g decrease in birth weight (p = 0.003) after controlling for potential confounders. Birth weight was not associated with levels of CRP or lipid profiles across the three racial groups. In addition, birth weight was inversely related to levels of fasting insulin and HOMA among non-Hispanic Whites; for each 1,000 g decrease in birth weight, fasting insulin levels increased 9.1 % (p = 0.007) and HOMA scores increased 9.8 % (p = 0.007). Birth weight was inversely associated with the levels of SBP, fasting insulin, and HOMA. These results support a role for birth weight, independent of the strong effects of current body weight status, in increasing risk for CVD and type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous research has shown that birth weight may play an important role in the development of cardiovascular disease (CVD). Low birth weight has been associated with hypertension, ischaemic and coronary heart disease [1–3] in large epidemiologic studies. On the other hand, high birth weight is positively related to childhood obesity [4, 5], and obese children are more likely to have elevated concentrations of serum cholesterol and glucose, which put them at higher risk for heart disease [6, 7]. Obese children also have notable changes in the mechanical properties of their arteries compared to healthy children including lower arterial compliance and distensibility and increased arterial wall stiffness [8]. This endothelial dysfunction may trigger the development of heart disease even in early life.
Barker and Hales initially proposed the “thrifty phenotype hypothesis”, which demonstrated the inverse relationship between birth weight and type 2 diabetes [9]. They proposed that prenatal growth stress, for instance, malnutrition, may lead to metabolic reprogramming beginning in utero. As a result, insulin sensitivity shifts to insulin resistance in the fetus to allow for maximum uptake of available energy and nutrients. This metabolic adaptation remains after birth and in turn can trigger rapid postnatal growth with a potential increased risk of type 2 diabetes. Research by groups led by Hales et al. [10] and Cook et al. [11] first demonstrated that low birth weight and lower body weight at 1 year were related to β cell dysfunction, impaired glucose tolerance, and increased incidence of type 2 diabetes later in life.
A number of pediatric studies have provided evidence that extremes in birth weight influence risk factors for heart disease and type 2 diabetes among children and adolescents [12–14]; however, only limited research has been conducted with large nationally representative datasets. We evaluated the associations between birth weight and selected risk factors for CVD [systolic blood pressure (SBP), C-reactive protein (CRP), and lipid profiles] and type 2 diabetes [fasting glucose, insulin, and homeostasis model assessment (HOMA)] using the National Health and Nutrition Examination Survey (NHANES) cycles 2001–2010.
Research Design and Methods
The NHANES
The continuous NHANES is a large, annual, cross-sectional survey that is designed to evaluate the nutrition and health status of the US population. Data releases are available in 2-year increments. Details regarding the survey design, data collection and procedures can be found elsewhere (CDC/NHANES analytic guidelines). Anthropometric and blood collection, handling and assay methods are described in the NHANES Laboratory Methods and Laboratory Procedures Manuals [15]. Data from cycles beginning in 2001–2002 and through 2009–2010 were combined to increase statistical power.
Participants
Data of children and adolescents aged 6–15 years (n = 10,758) from NHANES 2001 to 2010 were analyzed. Birth weight data are only available for subjects 15 years and younger. Of 10,747 boys and non-pregnant girls included in the 2001–2010 cycles of NHANES, 10,153 had proxy-reported birth weight data in both pounds and ounces (5.6 % were missing). Subjects (n = 6,699) also provided data including demographic (ethnicity/race and poverty-to-income ratio), and early childhood characteristics (mother’s age when subject was born and mother’s smoking status during pregnancy), diabetes (history/presence of diabetes and use of related medications), serum cotinine measurements (an objective indicator of cigarette smoke exposure), physical activity, and anthropometric measurements. In addition, current health status (head or chest cold, flu, pneumonia, or ear infection), dietary data and the outcomes of interest (SBP, plasma CRP, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C) measurements) were also included. Participants aged 12 years and older who fasted 8.5–12 h and were examined in the morning were asked to provide blood for fasting low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), glucose, and insulin assessment. We excluded subjects with CRP concentrations higher than 10 mg/L to rule out the influence of acute inflammation [16]. We also excluded subjects with diabetes or used related medications. Homeostatic model assessment (HOMA), an indicator for insulin resistance and beta-cell function, was calculated as follows: fasting insulin (uU/mL) × fasting glucose (mmol/L)/22.5 [17]. Birth weight was recorded to the nearest ounce as reported by the parent/guardian and later converted to grams. Birth weight group was categorized as low (<2,500 g), normal (2,500–4,000 g), and high (>4,000 g, CDC). Socioeconomic status was evaluated using the poverty income ratio and categorized as <1.0, 1.0–1.9, and ≥2.0 [18]. Age- and sex specific BMI percentiles were calculated using the US. Centers for Disease Control and Prevention SAS Program for the Growth Charts (CDC). Current weight status was classified as obese (≥95th percentile BMI-for-age), overweight (85th to <95th percentile), and under/normal weight (<85th percentile).
Statistical Analysis
All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC, USA). The 10-year sample weighting and specific survey procedures were used to account for unequal selection probability, survey non-response, and clustered design. Subjects who reported race/ethnicity other than Mexican-American, non-Hispanic Black, or non-Hispanic White were excluded from the data analysis due to small numbers. Variables that did not follow a normal distribution were log-transformed for statistical analyses. PROC SURVEYFREQ was used to determine frequencies of categorical variables and χ2 tests were conducted to examine the bivariate relation between demographic characteristics and variables of interest. Pairwise comparisons (PROC SURVEYREG) were performed to estimate univariate means and standard errors (SE) or geometric means and 95 % confidence interval (95 % CI) and to evaluate the differences in the outcome variables between birth weight categories (low/normal/high) for each variable of interest. Tukey tests were conducted to adjust for multiple comparisons. Multiple linear regression models (PROC SURVEYREG) were used to evaluate the association between selected outcome variables and birth weight as both continuous and as categorical predictor variables. Potential covariates, including survey cycle, age, gender, race/ethnicity, socioeconomic status, subject’s smoking status, BMI-for-age percentile, physical activity, maternal age when the subject was born, maternal smoking during pregnancy, and total dietary energy, saturated fat, sodium, and total sugar intakes were examined. Interactions between birth weight and related covariates were examined and non-significant interactions were removed from the final models. Statistical significance was set at p < 0.05.
Results
Demographic Characteristics
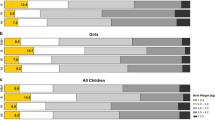
Selected demographic characteristics of subjects are presented in Table 1. Birth weights for about 80 % of subjects were in the normal range, above 10 % weighed more than 4,000 g and <10 % weighed <2,500 g. At examination, about 65 % of children and adolescents were under/normal weight and 16 % each were overweight and obese, respectively. The sample contained equal proportions of males and females and was 70 % non-Hispanic white with the remaining 30 % made up of equal proportions of Mexican-American and Non-Hispanic Black children.
The distribution of risk factors across birth weight categories are presented in Table 2. Subjects with high birth weights had significantly lower mean levels of TC (155.0 mg/dL; 95 % CI 152.7–157.4) than those subjects with low (159.4 mg/dL; 95 % CI 156.8–162.0) or normal (159.8 mg/dL; 95 % CI 158.6–161.1) birth weights (overall p = 0.002). Subjects with high birth weights had lower mean non-HDL-C levels (101.9 mg/dL; 95 % CI 99.6–104.2) while those subjects with normal birth weights had higher non-HDL-C levels (105.8 mg/dL; 95 % CI 104.6–107.0; overall p = 0.007). On average, subjects with low birth weights had significantly higher levels of fasting insulin (12.4 μU/mL; 95 % CI 11.1–13.8; overall p = 0.020) and HOMA-IR (2.87; 95 % CI 2.58–3.20; overall p = 0.014) compared to those participants with normal or high birth weights. We did not observe significant differences for other risk factors across birth weight categories.
Regression coefficients of SBP on birth weight overall and by gender are presented in Table 3. Overall, SBP levels were inversely associated with birth weight (β = −0.9; p = 0.002 after controlling for covariates). For girls, birth weight was inversely associated with SBP levels; SBP levels increased 1.4 mmHg for each 1,000 g decrease of birth weight (β = −1.4, p = 0.003). For boys, the association between birth weight and SBP was not statistically significant (β = −0.5, p = 0.199). When stratified by birth weight category, SBP levels were 1.1 mmHg lower for high birth weight subjects than those participants with normal birth weights among the whole group (β = −1.1, p = 0.036). SBP levels were 1.8 mmHg lower for high birth weight girls compared to the normal birth weight girls (β = −1.8, p = 0.041). Birth weight was significantly related to DBP levels; DBP levels increased 0.9 mmHg for each 1,000 g increase of birth weight (β = 0.9; p = 0.006) overall. Similar associations were observed among girls (β = 1.1, p = 0.006) but no significant associations were observed among boys. In addition, no significant differences cross birth weight categories were observed.
The relationship between plasma CRP concentrations and either continuous or categorical birth weight was not significant overall or when stratified by racial groups after controlling for covariates (Table 4).
The relationships between lipid levels and birth weight as continuous variables are presented in Table 4. We observed a significant interaction between race/ethnicity and fasting TG (p = 0.010). The overall and results stratified by race/ethnicity are presented for TG and for the other outcomes (for completeness) although no other statistically significant interactions were observed. In general, the associations between birth weight (continuous) and lipid profiles were no significant. When stratified by birth weight category, high birth weight subjects had 2.9 % lower TC levels (β = 0.971; p < 0.001) and 4 % lower non-HDL-C levels (β = 0.960; p = 0.001) compared to the normal birth weight subjects in the group as a whole. Mexican-Americans with high birth weights had 26 % higher levels of HDL-C (β = 1.026, p = 0.060) and the participants with low birth weights had 33.4 % higher levels of fasting TG (β = 1.334, p = 0.005) compared to subjects with normal birth weights. Birth weight category was not significantly associated with the lipid outcomes among non-Hispanic Blacks. Among non-Hispanic Whites, high birth weight subjects had 3.5 % lower levels of TC and 4.7 % lower levels of non-HDL-C compared to normal birth weight subjects (β = 0.965, p = 0.001 and β = 0.953, p = 0.002, respectively). In addition, low birth weight subjects had 13 % lower levels of LDL-C compared to normal birth weight subjects (β = 0.870, p = 0.045).
The relationships between biomarkers of type 2 diabetes and birth weight are presented in Table 5. Fasting glucose concentrations were not significantly associated with birth weight (continuous) in the whole group or across the three racial groups. Both fasting insulin concentrations and HOMA-IR were significantly associated with birth weight across all participants. For non-Hispanic White youth, a 9.1 % increase of fasting insulin concentration was associated with each 1,000 g decrease of birth weight (β = 0.909; p = 0.007). HOMA-IR levels increased 9.8 % with every 1,000 g decrease in birth weight (β = 0.902; p = 0.007).
In the categorical birth weight models for the whole group, compared to the participants with normal birth weights, subjects with high birth weights had 2.2 % lower fasting glucose levels (β = 0.978; p = 0.015), subjects with low birth weights had 13.6 % higher fasting insulin levels (β = 1.136; p = 0.025) and 14.9 % higher levels of HOMA-IR (β = 1.149; p = 0.022). When separated by racial groups, Mexican-Americans with low birth weights had higher levels of fasting glucose (β = 1.034, p = 0.014), fasting insulin (β = 1.176, p = 0.081), and HOMA (β = 1.206, p = 0.048) than subjects with normal birth weights. Low birth weight Non-Hispanic Blacks had fasting glucose concentrations 3.1 % higher (β = 1.031, p = 0.033) than subjects with normal birth weights. Non-Hispanic Whites with low birth weights had higher levels of fasting glucose (β = 1.045, p = 0.060) and fasting insulin (β = 1.137, p = 0.094) than participants with normal birth weights.
Discussion
In the present study, we found an inverse association between birth weight and SBP, especially in girls. Other studies have observed a significant inverse association of approximately the same magnitude between birth weight and SBP among girls [2, 12, 19, 20] and inconsistent results for boys. Although the precise mechanism the observed association has not been elucidated, both animal and human studies have observed that low birth weight is associated with a congenital deficit in nephron number [21], which plays a role in increasing renal renin-angiotensin system activity [22] and may result in hypertension.
Our results showed that birth weight was not associated with CRP levels among children and adolescents aged 6–15 years. The findings are in agreement with other large cross-sectional studies [23, 24]. Conversely, several studies observed elevated CRP concentrations among adults born at low birth weight [25–28]. This disagreement may be because that NHANES is nationally representative while other studies may have enrolled participants with higher-than-average CRP levels. For example, in the study of 132 rural Bangladesh children aged 5 years [27], children with low birth weights had significantly higher CRP concentrations than children with normal birth weights (0.65 vs. 0.10 mg/dL; p = 0.02). However, bacterial infection among low birth weight children was also significantly more prevalent than for normal birth weight children (p = 0.03). In addition, CRP levels over 3 mg/L are a predictor of future cardiovascular events among adults [29]; however, <10 % children and adolescents in the present study had CRP levels higher than 3 mg/L. Perhaps, any adverse effects of birth weight on circulating CRP emerge later in life.
In this study, levels of TC, non-HDL-C, and LDL-C were not associated with birth weight as a continuous variable, but across the birth weight categories were significant among non-Hispanic Whites. The relationship between birth weight and lipid profiles has been studied worldwide over the past two decades. Two recent meta-analysis studies [30, 31] demonstrated inverse associations between TC and birth weight. These studies included not only children and adolescents but middle-aged and older adults with mostly recorded birth weights. Other studies either used random TC data (fasting or non-fasting) for the analyses [32] or did not specify fasting state [33]. Since fasting TC is commonly considered for CVD assessment [34], we refined our analyses by including the fasting data available only for a subset of participants (n = 1,329). In the subsample, we observed that non-Hispanic Whites (n = 443) with either low or high birth weights had lower fasting TC levels. Compared to children with normal birth weights, children with low birth weights had 7.3 % lower TC levels (β = 0.927, p = 0.055) and children with high birth weights had 5.5 % lower TC levels (β = 0.945, p = 0.047).
Several large observational studies including participants of all races have demonstrated that TC and LDL-C concentrations increase from birth to pre-puberty, temporarily fall in early puberty, and then persistently increase to adult levels [35–37]. Racial differences in maturation rates among children are well-known; African American children enter puberty earlier than Mexican-American and Caucasian children [38]. Thus, we compared the means of age across the three racial groups and found that non-Hispanic Whites were older than Mexican-Americans and non-Hispanic Blacks (data not shown). Possibly age and timing of puberty contributed to physiological differences in TC and LDL-C levels across racial/ethnic groups. Unfortunately information related to timing of puberty was unavailable; thus, residual confounding may have contributed to the variability of results across the racial groups.
Additionally, many studies observed that extreme birth weights may play a vital role in onset of puberty. For example, low birth weight and small for gestational age status are related to earlier menarche [39, 40], which may be due to higher levels of circulating adrenal androgens and estrogens [41, 42], which usually results in earlier puberty. Moreover, high birth weight girls may also reach earlier menarche [43]; however, growth velocity during childhood contributes to this association [44, 45]. High birth weight infants are more likely to remain heavier and to have a higher risk for obesity than normal birth weight infants [4, 46]. Excess body fats result in elevated circulating leptin levels, which may stimulate the timing of puberty [47, 48]. Since TC and LDL-C levels temporary decline early in puberty [35–37], extreme birth weights may be related to lower TC and LDL-C levels during puberty.
Although the results varied across racial/ethnic groups, we observed that birth weight, independent of current body weight status, was inversely associated with at least one type 2 diabetes risk factor (fasting glucose, fasting insulin, or HOMA). Our NHANE cross-sectional findings are consistent with many [49–51] but not all studies [13, 52, 53] that either included older adults or children with type 2 diabetes [13, 53]. Highlighting the independent effect of birth weight on type 2 diabetes risk factors is important. Our observations are supportive of the Barker and Hales thrifty phenotype hypothesis. If metabolic reprogramming starts in the utero, then low birth weight, an indicator of prenatal growth stress, may be a direct predictor for type 2 diabetes risks later in life.
Diabetes is an independent risk factor for CVD in both men and women. About 65 % of individuals with diabetes die from some form of CVD [54]. Public health studies have confirmed that people with type 2 diabetes are prone to conditions e.g. dyslipidemia, hypertension, physical inactivity, and central obesity, which contribute the development of CVD. Our findings are in agreement with others who have observed that adverse effects of low birth weight on diabetes and CVD may emerge in childhood [55, 56].
The influence of childhood obesity on chronic disease development has been studied worldwide for decades. Obese children have significantly higher levels of blood pressure, TC, fasting LDL-C and TG, and lower levels of HDL-C than non-obese or normal subjects [7, 57]. Moreover, hyperinsulinemia is more common among adolescents with BMIs above the 90th percentile [58]. We found that birth weight was significantly positively related to current BMI-for-age percentile. When we focused on the subjects with low birth weights, subjects who were obese at examination had either marginally or significantly higher levels of SBP, CRP, non HDL-C, fasting insulin, and HOMA and significantly lower levels of HDL-C compared to subjects who were under/normal weight or overweight (data not shown).
Our study has several strengths. To our knowledge, our study is the first study to evaluate the relationship between birth weight and risk factors of type 2 diabetes and CVD among both older children and adolescents using the national representative NHANES database. Secondly, the NHANES includes a large socioeconomically and racially/ethnically-diverse sample. NHANES participants are not selected for factors such as family history of CVD or type 2 diabetes or some other characteristics that may be associated with the outcomes of interest. In addition, the NHANES data included current measured anthropometry and serum cotinine concentrations, which are objective and more accurate than proxy-reported data on body weight and smoking status. Next, the current study controlled for several important covariates including maternal age and smoking status during pregnancy, and physical activity, which will rule out their potential influences on the relationships between birth weight and the outcomes of interest.
The present study has a few limitations. The data are cross-sectional and birth weight is retrospectively proxy-reported; therefore, we are unable to evaluate the relationship between birth weight and the risk factors with the precision of a prospective analysis. However, research by others has shown that mothers’ reports of their infants’ birth weight are consistently close to medical record or birth certificate data [59, 60] with high accuracy and reliability years after delivery [61]. Next, data were lacking about breastfeeding duration and the family history of dyslipidemia, CVD, and type 2 diabetes for the current population; therefore, we were unable to assess genetic and several early environmental effects on the outcomes of interest. Finally, birth weight data are only available for subjects aged 15 years and younger; we were unable to evaluate the associations between birth weight and CVD and type 2 diabetes among older adolescents and adults.
In conclusion, this study adds to the growing evidence that low birth weight, independent of body weight status at interview, is related to risk factors for CVD and type 2 diabetes among older children and adolescents. Health practitioners should monitor children and adolescents with low birth weight more closely to identify early biomarkers suggestive of elevated risk for the development of these chronic disorders.
References
Johansson, S., Iliadou, A., Bergvall, N., Tuvemo, T., Norman, M., & Cnattingius, S. (2005). Risk of high blood pressure among young men increases with the degree of immaturity at birth. Circulation, 112(22), 3430–3436.
Barker, D. J., Winter, P. D., Osmond, C., Margetts, B., & Simmonds, S. J. (1989). Weight in infancy and death from ischaemic heart disease. Lancet, 2(8663), 577–580.
Lawlor, D. A., Ronalds, G., Clark, H., Smith, G. D., & Leon, D. A. (2005). Birth weight is inversely associated with incident coronary heart disease and stroke among individuals born in the 1950s: Findings from the Aberdeen children of the 1950s prospective cohort study. Circulation, 112(10), 1414–1418.
Binkin, N. J., Yip, R., Fleshood, L., & Trowbridge, F. L. (1988). Birth weight and childhood growth. Pediatrics, 82(6), 828–834.
Gillman, M. W., Rifas-Shiman, S., Berkey, C. S., Field, A. E., & Colditz, G. A. (2003). Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics, 111(3), e221–e226.
Manson, J. E., Colditz, G. A., Stampfer, M. J., Willett, W. C., Rosner, B., Monson, R. R., et al. (1990). A prospective study of obesity and risk of coronary heart disease in women. New England Journal of Medicine, 322(13), 882–889.
Freedman, D. S., Dietz, W. H., Srinivasan, S. R., & Berenson, G. S. (1999). The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics, 103(6 Pt 1), 1175–1182.
Tounian, P., Aggoun, Y., Dubern, B., Varille, V., Guy-Grand, B., Sidi, D., et al. (2001). Presence of increased stiffness of the common carotid artery and endothelial dysfunction in severely obese children: A prospective study. Lancet, 358(9291), 1400–1404.
Hales, C. N., & Barker, D. J. (1992). Type 2 (non-insulin-dependent) diabetes mellitus: The thrifty phenotype hypothesis. Diabetologia, 35(7), 595–601.
Hales, C. N., Barker, D. J., Clark, P. M., Cox, L. J., Fall, C., Osmond, C., et al. (1991). Fetal and infant growth and impaired glucose tolerance at age 64. British Medical Journal, 303(6809), 1019–1022.
Cook, J. T., Levy, J. C., Page, R. C., Shaw, J. A., Hattersley, A. T., & Turner, R. C. (1993). Association of low birth weight with beta cell function in the adult first degree relatives of non-insulin dependent diabetic subjects. British Medical Journal, 306(6873), 302–306.
Whincup, P., Cook, D., Papacosta, O., & Walker, M. (1995). Birth weight and blood pressure: Cross sectional and longitudinal relations in childhood. British Medical Journal, 311(7008), 773–776.
Wadsworth, M., Butterworth, S., Marmot, M., Ecob, R., & Hardy, R. (2005). Early growth and type 2 diabetes: Evidence from the 1946 British birth cohort. Diabetologia, 48(12), 2505–2510.
Ferrie, J. E., Langenberg, C., Shipley, M. J., & Marmot, M. G. (2006). Birth weight, components of height and coronary heart disease: Evidence from the Whitehall II study. International Journal of Epidemiology, 35(6), 1532–1542.
CDC. National Health and Nutrition Examination Survey. Available from: http://www.cdc.gov/nchs/nhanes.htm.
Clyne, B., & Olshaker, J. S. (1999). The C-reactive protein. Journal of Emergency Medicine, 17(6), 1019–1025.
Matthews, D. R., Hosker, J. P., Rudenski, A. S., Naylor, B. A., Treacher, D. F., & Turner, R. C. (1985). Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia, 28(7), 412–419.
Xu, X., Dailey, A. B., Freeman, N. C., Curbow, B. A., & Talbott, E. O. (2009). The effects of birthweight and breastfeeding on asthma among children aged 1–5 years. Journal of Paediatrics and Child Health, 45(11), 646–651.
Lawlor, D. A., Ebrahim, S., & Davey Smith, G. (2002). Is there a sex difference in the association between birth weight and systolic blood pressure in later life? Findings from a meta-regression analysis. American Journal of Epidemiology, 156(12), 1100–1104.
Doyle, L. W., Faber, B., Callanan, C., & Morley, R. (2003). Blood pressure in late adolescence and very low birth weight. Pediatrics, 111(2), 252–257.
Hinchliffe, S. A., Lynch, M. R., Sargent, P. H., Howard, C. V., & Van Velzen, D. (1992). The effect of intrauterine growth retardation on the development of renal nephrons. British Journal of Obstetrics and Gynaecology, 99(4), 296–301.
Zandi-Nejad, K., Luyckx, V. A., & Brenner, B. M. (2006). Adult hypertension and kidney disease: The role of fetal programming. Hypertension, 47(3), 502–508.
Gillum, R. F. (2003). Association of serum C-reactive protein and indices of body fat distribution and overweight in Mexican American children. Journal of the National Medical Association, 95(7), 545–552.
Dowd, J. B., Zajacova, A., & Aiello, A. E. (2010). Predictors of inflammation in US children aged 3–16 years. American Journal of Preventive Medicine, 39(4), 314–320.
Sattar, N., McConnachie, A., O’Reilly, D., Upton, M. N., Greer, I. A., Davey Smith, G., et al. (2004). Inverse association between birth weight and C-reactive protein concentrations in the MIDSPAN Family Study. Arteriosclerosis, Thrombosis, and Vascular Biology, 24(3), 583–587.
Bhuiyan, A. R., Srinivasan, S. R., Chen, W., Azevedo, M. J., & Berenson, G. S. (2011). Influence of low birth weight on C-reactive protein in asymptomatic younger adults: The Bogalusa heart study. BMC Research Notes, 4, 71.
Raqib, R., Alam, D. S., Sarker, P., Ahmad, S. M., Ara, G., Yunus, M., et al. (2007). Low birth weight is associated with altered immune function in rural Bangladeshi children: A birth cohort study. American Journal of Clinical Nutrition, 85(3), 845–852.
McDade, T. W., Rutherford, J., Adair, L., & Kuzawa, C. W. (2010). Early origins of inflammation: Microbial exposures in infancy predict lower levels of C-reactive protein in adulthood. Proceedings of the Biological Science, 277(1684), 1129–1137.
Ridker, P. M., Rifai, N., Rose, L., Buring, J. E., & Cook, N. R. (2002). Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. New England Journal of Medicine, 347(20), 1557–1565.
Huxley, R., Owen, C. G., Whincup, P. H., Cook, D. G., Colman, S., & Collins, R. (2004). Birth weight and subsequent cholesterol levels: Exploration of the “fetal origins” hypothesis. Journal of the American Medical Association, 292(22), 2755–2764.
Lawlor, D. A., Owen, C. G., Davies, A. A., Whincup, P. H., Ebrahim, S., Cook, D. G., et al. (2006). Sex differences in the association between birth weight and total cholesterol. A meta-analysis. Annals of the Epidemiology, 16(1), 19–25.
Owen, C. G., Whincup, P. H., Odoki, K., Gilg, J. A., & Cook, D. G. (2003). Birth weight and blood cholesterol level: A study in adolescents and systematic review. Pediatrics, 111(5 Pt 1), 1081–1089.
Kawabe, H., Shibata, H., Hirose, H., Tsujioka, M., Saito, I., & Saruta, T. (1999). Sexual differences in relationships between birth weight or current body weight and blood pressure or cholesterol in young Japanese students. Hypertension Research, 22(3), 169–172.
Mora, S., Rifai, N., Buring, J. E., & Ridker, P. M. (2008). Fasting compared with nonfasting lipids and apolipoproteins for predicting incident cardiovascular events. Circulation, 118(10), 993–1001.
Frerichs, R. R., Srinivasan, S. R., Webber, L. S., & Berenson, G. R. (1976). Serum cholesterol and triglyceride levels in 3,446 children from a biracial community: The Bogalusa Heart Study. Circulation, 54(2), 302–309.
Hickman, T. B., Briefel, R. R., Carroll, M. D., Rifkind, B. M., Cleeman, J. I., Maurer, K. R., et al. (1998). Distributions and trends of serum lipid levels among United States children and adolescents ages 4–19 years: Data from the third National Health and Nutrition Examination Survey. Preventive Medicine, 27(6), 879–890.
Ford, E. S., Li, C., Zhao, G., & Mokdad, A. H. (2009). Concentrations of low-density lipoprotein cholesterol and total cholesterol among children and adolescents in the United States. Circulation, 119(8), 1108–1115.
Sun, S. S., Schubert, C. M., Chumlea, W. C., Roche, A. F., Kulin, H. E., Lee, P. A., et al. (2002). National estimates of the timing of sexual maturation and racial differences among US children. Pediatrics, 110(5), 911–919.
Cooper, C., Kuh, D., Egger, P., Wadsworth, M., & Barker, D. (1996). Childhood growth and age at menarche. British Journal of Obstetrics and Gynaecology, 103(8), 814–817.
Persson, I., Ahlsson, F., Ewald, U., Tuvemo, T., Qingyuan, M., von Rosen, D., et al. (1999). Influence of perinatal factors on the onset of puberty in boys and girls: Implications for interpretation of link with risk of long term diseases. American Journal of Epidemiology, 150(7), 747–755.
Ong, K. K., Potau, N., Petry, C. J., Jones, R., Ness, A. R., Honour, J. W., et al. (2004). Opposing influences of prenatal and postnatal weight gain on adrenarche in normal boys and girls. Journal of Clinical Endocrinology and Metabolism, 89(6), 2647–2651.
Ruder, E. H., Hartman, T. J., Rovine, M. J., & Dorgan, J. F. (2011). Birth characteristics and female sex hormone concentrations during adolescence: Results from the Dietary Intervention study in children. Cancer Causes and Control, 22(4), 611–621.
dos Santos Silva, I., De Stavola, B. L., Mann, V., Kuh, D., Hardy, R., & Wadsworth, M. E. (2002). Prenatal factors, childhood growth trajectories and age at menarche. International Journal of Epidemiology, 31(2), 405–412.
Davison, K. K., Susman, E. J., & Birch, L. L. (2003). Percent body fat at age 5 predicts earlier pubertal development among girls at age 9. Pediatrics, 111(4 Pt 1), 815–821.
Wang, Y., Dinse, G. E., & Rogan, W. J. (2012). Birth weight, early weight gain and pubertal maturation: A longitudinal study. Pediatric Obesity, 7(2), 101–109.
Cnattingius, S., Villamor, E., Lagerros, Y. T., Wikstrom, A. K., & Granath, F. (2012). High birth weight and obesity—A vicious circle across generations. International Journal of Obesity (London), 36(10), 1320–1324.
Clayton, P. E., Gill, M. S., Hall, C. M., Tillmann, V., Whatmore, A. J., & Price, D. A. (1997). Serum leptin through childhood and adolescence. Clinical Endocrinology (Oxford), 46(6), 727–733.
Cheung, C. C., Thornton, J. E., Kuijper, J. L., Weigle, D. S., Clifton, D. K., & Steiner, R. A. (1997). Leptin is a metabolic gate for the onset of puberty in the female rat. Endocrinology, 138(2), 855–858.
Clausen, J. O., Borch-Johnsen, K., & Pedersen, O. (1997). Relation between birth weight and the insulin sensitivity index in a population sample of 331 young, healthy Caucasians. American Journal of Epidemiology, 146(1), 23–31.
Carlsson, S., Persson, P. G., Alvarsson, M., Efendic, S., Norman, A., Svanstrom, L., et al. (1999). Low birth weight, family history of diabetes, and glucose intolerance in Swedish middle-aged men. Diabetes Care, 22(7), 1043–1047.
Mzayek, F., Sherwin, R., Fonseca, V., Valdez, R., Srinivasan, S. R., Cruickshank, J. K., et al. (2004). Differential association of birth weight with cardiovascular risk variables in African-Americans and Whites: The Bogalusa heart study. Annals of Epidemiology, 14(4), 258–264.
Wei, J. N., Sung, F. C., Li, C. Y., Chang, C. H., Lin, R. S., Lin, C. C., et al. (2003). Low birth weight and high birth weight infants are both at an increased risk to have type 2 diabetes among schoolchildren in Taiwan. Diabetes Care, 26(2), 343–348.
Harder, T., Rodekamp, E., Schellong, K., Dudenhausen, J. W., & Plagemann, A. (2007). Birth weight and subsequent risk of type 2 diabetes: A meta-analysis. American Journal of Epidemiology, 165(8), 849–857.
Geiss, L. S., Herman, W. H., & Smith, P. J. (1995). Mortality among persons with non-insulin dependent diabetes. Diabetes in America (2nd ed., pp. 233–258). Bethesda: National Institute of Health.
Franco, M. C., Christofalo, D. M., Sawaya, A. L., Ajzen, S. A., & Sesso, R. (2006). Effects of low birth weight in 8- to 13-year-old children: Implications in endothelial function and uric acid levels. Hypertension, 48(1), 45–50.
Park, B., Park, E., Cho, S. J., Kim, Y., Lee, H., Min, J., et al. (2009). The association between fetal and postnatal growth status and serum levels of uric acid in children at 3 years of age. American Journal of Hypertension, 22(4), 403–408.
Chu, N. F., Rimm, E. B., Wang, D. J., Liou, H. S., & Shieh, S. M. (1998). Clustering of cardiovascular disease risk factors among obese schoolchildren: The Taipei Children Heart Study. American Journal of Clinical Nutrition, 67(6), 1141–1146.
Jiang, X., Srinivasan, S. R., & Berenson, G. S. (1996). Relation of obesity to insulin secretion and clearance in adolescents: The Bogalusa Heart Study. International Journal of Obesity and Related Metabolic Disorders, 20(10), 951–956.
Tate, A. R., Dezateux, C., Cole, T. J., & Davidson, L. (2005). Factors affecting a mother’s recall of her baby’s birth weight. International Journal of Epidemiology, 34(3), 688–695.
Ruder, E. H., Dorgan, J. F., Kranz, S., Kris-Etherton, P. M., & Hartman, T. J. (2008). Examining breast cancer growth and lifestyle risk factors: Early life, childhood, and adolescence. Clinical Breast Cancer, 8(4), 334–342.
Catov, J. M., Newman, A. B., Kelsey, S. F., Roberts, J. M., Sutton-Tyrrell, K. C., Garcia, M., et al. (2006). Accuracy and reliability of maternal recall of infant birth weight among older women. Annals of Epidemiology, 16(6), 429–431.
Acknowledgments
We would like to thank Jacqueline Vernarelli (Ph.D.) and Diane Mitchell (M.S.) for their help with data interpretation. The authors’ contributions were as follows: Z.Z. designed the research, conducted data analysis for the research, and had primary responsibility for the manuscript; T.J.H. and P.K.E. contributed to data interpretation and manuscript preparation.
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Kris-Etherton, P.M. & Hartman, T.J. Birth Weight and Risk Factors for Cardiovascular Disease and Type 2 Diabetes in US Children and Adolescents: 10 Year Results from NHANES. Matern Child Health J 18, 1423–1432 (2014). https://doi.org/10.1007/s10995-013-1382-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-013-1382-y