Abstract
Alcohol consumption during pregnancy has negative implications for maternal and child health. Appropriate early universal Screening, Brief Intervention and Referral to Treatment (SBIRT) for pregnant women is necessary to identify women at risk and reduce the likelihood of continued drinking. Because SBIRT is not consistently used, the development and use of performance measures to assure implementation of SBIRT are key steps towards intervention and reduction of alcohol consumption during pregnancy. Practice guidelines provide ample support for specific instruments designed for SBIRT in prenatal care. An examination of existing performance measures related to alcohol consumption during pregnancy, however, reveals no comprehensive published performance measure designed to quantify the use of SBIRT for alcohol use in prenatal care. Process performance measures were developed that can determine the proportion of pregnant women who are screened during the course of prenatal care and the proportion of women requiring either brief intervention or referral to substance use disorder treatment who received those interventions. The measures require use of screening instruments validated for use with pregnant women. The two proposed measures would represent a significant step in efforts to assure appropriate intervention for women who drink during pregnancy, hold accountable providers who do not employ SBIRT, and provide a basis from which necessary systemic changes might occur. Pregnancy is a time when many women are motivated to stop drinking. That opportunity should be seized, with timely intervention offering assistance for pregnant women who have not stopped drinking of their own accord.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Alcohol consumption during pregnancy can have negative implications for maternal and child health. Accordingly, medical and public health organizations recommend that women not consume any alcohol during pregnancy [1–6]. Although the effect of prenatal exposure on a fetus depends in part on the timing and extent of exposure and other factors (e.g., prenatal nutrition, maternal age, polysubstance use, post-birth environment) [7–9], the evidence on alcohol exposure is long-standing [7, 8, 10–15], with larger amounts of alcohol, consumed at a faster rate or at greater frequency, most likely to result in Fetal Alcohol Spectrum Disorders [7, 8].
Despite these negative health effects, in 2010 and 2011, an estimated 9.4 % of pregnant women in the United States drank in the past month [16]. Of those pregnant women who drank in 2011, the following percentages reported typically consuming four or more drinks on a single day: ages 15–17 58 %, ages 18–25 31 %, and ages 26–44 17 % [17]. Beyond potential harm to the child, associated costs to society (e.g., education, child welfare, medical and behavioral health care) can be high [18, 19].
Appropriate and universal Screening, Brief Intervention and Referral to Treatment (SBIRT) [20] as part of prenatal care is key to reducing continued alcohol use during pregnancy. SBIRT involves: (1) initial screening to identify women who continue to drink during pregnancy, (2) for those identified as drinking, brief intervention designed to prevent continued drinking, and (3) for those who require it, referral to specialty substance use disorder treatment. For those in need of specialty treatment, effective interventions exist, including Motivational Interviewing, Cognitive Behavioral Therapy and Motivational Enhancement Therapy [21–23]. As discussed below, SBIRT for pregnant women is recommended by practice guidelines. The Affordable Care Act (ACA) also recognizes the importance of universal screening by requiring coverage of alcohol screening without co-payment, co-insurance or application of a deductible, for adults and, in some cases, adolescents, who are covered by many private insurance plans, by Medicare, and by Medicaid in states that participate in the ACA expansion [24–27].
Neither guidelines nor insurance mandates for best practices, however, automatically result in implementation by practitioners. Donabedian’s framework of healthcare quality measurement [28] is the theoretical basis for much of current healthcare performance measurement [e.g., 29–32]. The development and use of well-designed performance measures to assure implementation of SBIRT are key steps towards effective intervention and reduction of alcohol consumption during pregnancy. The development of performance measures that apply, at a minimum to pregnant women, will be an important step in measuring the degree to which actual services adhere to guidelines and to the spirit of the ACA requirement.
To that end, this article addresses: (1) guidelines recommending SBIRT for pregnant women; (2) appropriate screening instruments; (3) evidence regarding implementation of SBIRT for pregnant women; and (4) existing performance measures. This article then proposes performance measures designed to assess adherence to guidelines and makes policy recommendations.
Practice Guidelines
Appropriately validated screening for alcohol use during pregnancy is heavily endorsed in the literature, as is brief intervention and/or referral for specialized treatment. Three organizations that recommend SBIRT for all pregnant women are the National Institute on Alcohol Abuse and Alcoholism (NIAAA)[5], the American College of Obstetricians and Gynecologists (ACOG) [1, 3], and the United States Preventive Services Task Force (USPSTF) [33]. ACOG has issued multiple opinion bulletins [1–3] and takes the position that “physicians have an ethical obligation to learn and use techniques for universal screening questions, brief intervention, and referral to treatment” (p. 9) [3]. One ACOG bulletin incorporates recommended instruments for screening (e.g., TWEAK, T-ACE) and brief intervention (Brief Negotiated Intervention and Referral to Treatment (BNI-ART) Institute Intervention Algorithm) [3]. The USPSTF also recommends routine screening and brief intervention in primary care, including during pregnancy, and specifically endorses use of the TWEAK or T-ACE for screening pregnant women [33]. Evidence for screening pregnant women was strong in 2004 when the USPSTF issued its recommendation, while the evidence for brief intervention was less so; however, the evidence supporting brief intervention for pregnant women subsequently has grown [e.g., 34–36]. Guidelines recommending SBIRT for prenatal alcohol use also have been promulgated by states [e.g., 37, 38], the Veterans Administration [39], health plans (e.g., Neighborhood Health Plan of Rhode Island [40]), and medical societies of other countries (e.g., Canada [41]).
Screening Tools Appropriate for Use in a Prenatal Setting
The national guidelines and endorsements of SBIRT for pregnant women include specific screening and brief intervention tools suitable for use in that population. The two recommended screens, the TWEAK and T-ACE, however, were originally designed to screen for moderate or heavy use, rather than simply any current drinking [42, 43]. Because pregnant women are urged not to drink at all, an initial screening device that assesses any current drinking should be used. The Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System (BRFSS) includes one question that is designed to elicit this information from the general population: “During the past 30 days, how many days per week or per month did you have at least one drink of any alcoholic beverage such as beer, wine, a malt beverage or liquor?”[44]. This survey question, however, was not designed to screen pregnant women and the validity of the question for that group and purpose is unknown. Similar questions, however, are imbedded in the validated “4Ps Plus” [43, 45], and in the related and as yet unvalidated 5 P’S Behavioral Risk Screening Tool (5 P’S) [46, 47], screening instruments designed to elicit information about multiple risk factors as part of prenatal care, including any current use of alcohol, and to do so in an indirect way that does not single out the woman’s alcohol consumption as the sole focus [47]. The 4P’s and 5 P’S are appropriate preliminary screening instruments for pregnant women.
The recommendations of ACOG and the USPSTF regarding use of the TWEAK and T-ACE [3, 33] should not be ignored, however, as both are valid alcohol screens for pregnant women [42, 48]. The TWEAK detects alcoholism, moderate and high-risk drinking [42, 49], and the T-ACE detects current consumption, risky drinking and alcoholism [42, 49]. These instruments certainly should be used if a preliminary screen indicates any drinking during pregnancy, to better ascertain level of risk. It also is the position of NIAAA that the T-ACE can be used to detect “any prenatal alcohol consumption” [50]. There also are other common screening instruments that have not been validated or found effective for pregnant women and are not appropriate for use with that population. These instruments include the CAGE [3, 42, 43, 48, 50, 51], the Michigan Alcoholism Screening Test (MAST) [42] and the Short MAST [51]; these tools should not be used to screen pregnant women. More information on the 4P’s Plus, the 5P’S, the T-ACE and the TWEAK are in the Appendix to this article.
Evidence Regarding Implementation of Practice Guidelines
Even though practice guidelines and recommendations for the application of SBIRT in the care of pregnant women have been available for a number of years, many physicians disregard such guidelines [3, 9] and, when screening does happen, may not use validated instruments [52].
Adherence to practice guidelines generally may be impeded by lack of awareness of or disagreement with guidelines, inability to obtain reimbursement, or inertia [53]. Other reasons often given for not utilizing SBIRT for pregnant women include lack of time, lack of knowledge about screening and referral, misperceptions about alcohol use among women, doubt about treatment usefulness or availability, and discomfort raising the subject [3, 9, 53]. Doctors also worry about breach of confidence when mandated reporting is required upon discovery of substance use by a pregnant woman [3].
These impediments to appropriate prenatal care must be dealt with if such care is to be routinely provided. Inability to obtain reimbursement has been a major obstacle to SBIRT, regardless of the patient population. The Centers for Medicare and Medicaid Services, however, added procedure codes to Medicaid in 2008, so that providers might obtain reimbursement for screening and brief intervention. Adoption of the new codes, however, must be implemented individually by each state, with slow progress being made towards the possibility of universal reimbursement [54]. Increasing numbers of private health plans, however, do now reimburse for screening and brief intervention, as does the Federal Employees Health Benefits Program [55] and the coverage mandate found in the ACA further diminishes reasons not to screen [24–27].
Insufficient time, unfamiliarity with SBIRT tools, and lack of knowledge about treatment services are other reasons cited for not employing SBIRT. Innovative techniques must be developed to resolve this problem. The use of “interventionists” or other trained staff in primary care and obstetrical practice to conduct SBIRT and other screenings (e.g., depression) may be one answer to lack of time and familiarity with the process. These staff could administer both the screening and brief intervention and would have ready knowledge of available treatment facilities if referral were warranted.
Education of providers, incentives to alter entrenched practice patterns (including accountability measures, public reporting, and value-based purchasing), implementation of technology-based practice reminders that facilitate change, such as are used by the Veterans Administration for alcohol screening [56], and clarity regarding mandated reporting requirements, are crucial. Further, as long as women continue to be under-diagnosed with alcohol use disorders, due to misperceptions about alcohol abuse in women [57] and provider discomfort with the subject [9], the medical culture will not be capable of confronting and dealing with alcohol exposure during pregnancy. For this reason, performance measures addressing SBIRT should be developed and used, if not as part of value-based purchasing or public reporting, at least as internal accountability or insurer tools instituted to improve quality of care.
Existing Related Performance Measures
No performance measures exist that are explicitly related to SBIRT, in all its aspects, for alcohol use during pregnancy. We found no comprehensive measure among those listed by the National Quality Measures Clearinghouse or endorsed by the National Quality Forum. Nor do the Center for Quality Assessment and Improvement in Mental Health measure inventory, or the Healthcare Effectiveness Data and Information Set (HEDIS) include such a measure.
Two related performance measures, however, include an Indian Health Service measure and one recently developed by the American Medical Association (AMA). The first was designed to address the risk of Fetal Alcohol Spectrum Disorder in the Native American population, and focuses on women of reproductive age, rather than simply pregnant women. This measure has the advantage of identifying alcohol use among all women, including pre- and inter-conceptually, but does not incorporate brief intervention and referral to treatment [58, 59]. The second measure, promulgated by the AMA in 2012, measures combined screening for depression, alcohol use, tobacco use, drug use, and intimate partner violence [60]. While this measure is a giant step forward because it includes alcohol screening, and other screening that is vitally important for risk assessment, it does not specify that the screening instrument be validated for use with pregnant women, and it does not measure brief intervention or referral to treatment. Indeed, the AMA notes accompanying the measure acknowledge research by Goler et al. [61] indicating that women who are both screened and treated have better birth outcomes than women who screen positive but are not treated. Measuring women who are screened and provided appropriate intervention, in relation to women who were screened but who do not receive an indicated intervention, is imperative if changes in practice patterns are to occur that facilitate the intervention aspect of SBIRT. Measuring screening alone is insufficient.
Proposed Performance Measures
Screening for alcohol use by pregnant women and, if needed, use of brief intervention or referral to treatment, are health interventions for which performance measurement is appropriate. Typical purposes for which performance measures are created include accountability (e.g., public reporting), quality improvement, research, and value-based purchasing (or “pay-for-performance”) [e.g., 32]. Well-developed prenatal performance measures could satisfy all of these purposes, inducing providers to provide best practices to pregnant women, holding accountable providers who do not, and providing a better base for assessment of what systemic changes might be warranted, including provider education.
Although healthcare quality measurement may focus on either structure, process, outcome, patient experience or access [28], in the context of prenatal care, process measures should have the most direct impact. Outcome measures, such as the number of infants born with Fetal Alcohol Spectrum Disorders, would quantify a desired outcome, but without addressing the crucial step of how to obtain that objective. Targeted process measures are more likely to alter practice and, given the measurement difficulties encountered in trying to quantify Fetal Alcohol Spectrum Disorders or even Fetal Alcohol Syndrome [62], outcome measures are premature until processes are well-established.
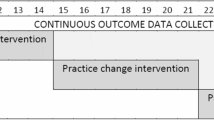
Process measures, focused on application of SBIRT, seem feasible and have the benefit of directly measuring important interventions lacking in the care of many pregnant women. To that end, we propose the following sequence of two process-oriented performance measures:
-
1.
Numerator: all pregnant patients screened for alcohol use during their first prenatal visit (including refusals), utilizing a screening instrument validated for pregnant women.
Denominator: all pregnant patients seen for an initial prenatal visit by a primary care physician, family practitioner, ob-gyn, nurse practitioner or other professional or paraprofessional working under the supervision of one of the specified physicians.
-
2.
Numerator: all pregnant patients receiving: (1) an evidence-based brief intervention for alcohol use during their first prenatal visit or during a later prenatal visit if alcohol use is revealed during that visit, and/or (2) a referral for specialty substance abuse services during their first prenatal visit or during a later prenatal visit if alcohol use was revealed during that visit.
Denominator: all pregnant patients seen for an initial prenatal visit by a primary care physician, family practitioner, ob-gyn, nurse practitioner or other professional or paraprofessional working under the supervision of one of the specified physicians, who screened positive for alcohol use during their first prenatal visit or during a later prenatal visit if alcohol use was revealed during that visit.
The following considerations were taken into account in the construction of these measures:
Specification of Screening and Intervention Tools
Screening, Brief Intervention and Referral to Treatment (SBIRT) should involve putting evidence-based guidelines into practice, rather than leaving the process open to the use of unreliable screening tools or interventions. Thus, measures should explicitly require that the screening and brief intervention methods used be evidence-based. The measures, however, should not specify which evidence-based instruments must be used, to accommodate the evolution of both evidence and practice. Additional information related to recommended screening and brief intervention instruments is in the Appendix to this article.
Application to Prenatal Settings
These performance measures were constructed to apply to prenatal care. Ideally, all women of reproductive age would be routinely screened as part of primary care, with intervention provided as needed. Similarly, SBIRT for pregnant women should not be limited solely to prenatal care. The decision to direct the performance measure at prenatal care, however, targets change at a crucial aspect of pregnancy health care and clearly defines responsibility for provision of services.
Data Sources
For a performance measure to function properly, a reliable data source must be available, which means that screening and brief intervention must be properly documented in the woman’s chart. Additionally, separate coding must be available for: (1) screening and (2) brief intervention and referral to treatment. For quality improvement purposes, this coding permits measurement of whether each is being provided appropriately and allows collection of data regarding screening and the relative number of pregnant women screened who require and receive additional intervention. The addition of billing codes should facilitate data collection, provided individual states activate the Medicaid reimbursement codes and provided healthcare settings actually use available coding. It, however, should not be solely Medicaid providers who are accountable for delivery of these services. Thus, inclusion of the proposed measures in HEDIS measures for private health plans would reach much of the population. Those women still missing, the disenfranchised who do not seek prenatal care [57], unfortunately would continue to be both unmeasured and untreated.
Utilization of administrative data, such as Medicaid or private insurance claims data, should be sufficient for purposes of public reporting, accountability, or value-based purchasing. For quality improvement purposes, however, the existence of electronic health records would be a valuable addition to sources of data with which these measures might be used.
Application of SBIRT for Illicit Drug Use
The assessment of illicit drug use among pregnant women is important, with growing evidence that SBIRT may be beneficial [63, 64]. Illicit drug use during pregnancy, however, raises issues that are less relevant to legal drug use such as alcohol. With illicit drug use, pregnant women and their physicians have additional concerns about possible criminal liability, child custody loss and other social welfare implications such as loss of housing. Therefore, this article does not advocate performance measurement for SBIRT related to illicit substances, unless issues of criminal prosecution and child custody loss are resolved.
Related Policy Recommendations
In addition to adoption of the recommended performance measures, other changes to policy and practice are important if these measures are to be meaningful.
First, the recommended measures are designed to encourage universal SBIRT for pregnant women. The universal application of SBIRT is necessary if disparities in screening and consequences are to be avoided. Rather than permitting providers to make ad hoc judgments as to who should be screened, universal application will capture use by women whom, contrary to the evidence [e.g., 45], doctors may not consider at risk due to preconceptions about race/ethnicity or socio-economic status.
Second, once screening occurs, both brief intervention and referral to treatment must be meaningful. Merely handing a woman a list of treatment facilities is insufficient. A thoughtful brief intervention with subsequent booster sessions and/or carefully coordinated referral and follow-up may make a significant difference.
Third, appropriate training of providers, both professional and paraprofessional, is imperative. Validated screening and brief intervention tools are available and providers should have the training to apply those tools properly.
Fourth, all state Medicaid programs and private insurers must have codes in effect that permit reimbursement. Further, because current Medicaid reimbursements, when available, are so minimal as to discourage use, policymakers should consider both increasing available reimbursement and permitting paraprofessionals such as interventionists or other health workers to perform these tasks, thereby reducing costs.
Finally, although prenatal alcohol use does not entail the potential for criminal prosecution as commonly as use of illicit drugs, women remain at risk for stigmatization and loss of custody. Women need to be able to be screened, and receive treatment, without risk of loss of custody. If universal screening is to occur, society must anticipate and deal with the consequences in a way that encourages treatment rather than fear and avoidance.
Conclusion
Fetal exposure to alcohol continues to be a serious problem that can impose burdens on the child, their family and society. The two proposed measures, if adopted by Medicaid and private health insurers, would represent a significant step in efforts to assure appropriate intervention for women who drink during pregnancy. Moreover, despite the recognized difficulty in inducing pregnant women to be honest about alcohol consumption [3, 8, 42], pregnancy is a time when many women are motivated to stop, as evidenced by the large percentage who do. That opportunity should be seized, with timely intervention offering encouragement and assistance for those women who have not stopped drinking of their own accord.
References
American College of Obstetricians and Gynecologists. (2011). Committee opinion no. 496: At-risk drinking and alcohol dependence: Obstetric and gynecologic implications. Obstetrics and Gynecology, 118, 383–388.
American College of Obstetricians and Gynecologists. (2006). Committee opinion no. 343: Psychosocial risk factors: Perinatal screening and intervention. Obstetrics and Gynecology, 108, 469.
American College of Obstetricians and Gynecologists (2008). Committee opinion no. 422: At-risk drinking and illicit drug use: Ethical issues in obstetric and gynecologic practice [Internet]. Washington, DC: American College of Obstetricians and Gynecologists [cited 2013 Feb 16]. Available from: http://www.acog.org/Resources_And_Publications/Committee_Opinions/Committee_on_Ethics/At_Risk_Drinking_and_Illicit_Drug_Use_Ethical_Issues_in_Obstetric_and_Gynecologic_Practice.
Centers for Disease Control and Prevention. FASD homepage: Alcohol use in pregnancy [Internet]. Atlanta, GA: Centers for Disease Control and Prevention [updated 2010 Oct 6; cited 2013 Feb 17]. Available from: http://www.cdc.gov/NCBDDD/fasd/alcohol-use.html.
United States Department of Health and Human Services. National Institutes of Health. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide [Internet]. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism [updated 2007 Jan; cited 2013 Feb 17]. Available from: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm.
United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. FASD Center for Excellence. Stop and think. If you’re pregnant, don’t drink [Internet]. Rockville, MD: Substance Abuse and Mental Health Services Administration [updated 2013 Jan 30; cited 2013 Feb 17]. Available from: http://www.fascenter.samhsa.gov/index.aspx.
Chiodo, L. M., Da Costa, D. E., Hannigan, J. H., Covington, C. Y., Sokol, R. J., Janisse, J., et al. (2010). The impact of maternal age on the effects of prenatal alcohol exposure on attention. Alcoholism, Clinical and Experimental Research, 34, 1813–1821.
Chiodo, L. M., Janisse, J., Delaney-Black, V., Sokol, R. J., & Hannigan, J. H. (2009). A metric of maternal prenatal risk drinking predicts neurobehavioral outcomes in preschool children. Alcoholism, Clinical and Experimental Research, 33, 634–644.
Clarren, S. K., & Salmon, A. (2010). Prevention of fetal alcohol spectrum disorder: Proposal for a comprehensive approach. Expert review of obstetrics and gynecology, 5, 23–30.
Abel, E. L., & Sokol, R. J. (1987). Incidence of fetal alcohol syndrome and economic impact of FAS-related anomalies. Drug and Alcohol Dependence, 19, 51–70.
Bailey, B., & Sokol, R. J. (2008). Pregnancy and alcohol use: Evidence and recommendations for prenatal care. Clinical Obstetrics and Gynecology, 51, 436–444.
Burd, L., Deal, E., Rios, R., Adickes, E., Wynne, J., & Klug, M. (2007). Congenital heart defects and fetal alcohol spectrum disorders. Congenital heart disease, 2, 250–255.
Burd, L., Klug, M. G., Martsolf, J. T., & Kerbeshian, J. (2003). Fetal alcohol syndrome: Neuropsychiatric phenomics. Neurotoxicology and Teratology, 25, 697–705.
Willford, J., Chandler, L., Goldschmidt, L., & Day, N. (2010). Effects of prenatal tobacco, alcohol and marijuana exposure on processing speed, visual-motor coordination, and interhemispheric transfer. Neurotoxicology and Teratology, 32, 580–588.
Salihu, H. M., Kornosky, J. L., Lynch, O., Alio, A. P., August, E. M., & Marty, P. J. (2011). Impact of prenatal alcohol consumption on placenta-associated syndromes. Alcohol, 45, 73–79.
United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Summary of national findings [Internet]. Rockville, MD: Substance Abuse and Mental Health Services Administration [updated 2012 Dec 11; cited 2013 Feb 17]. Available from: http://www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.htm.
United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health, 2011 [Internet]. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [cited 2013 Feb 17]. Available from: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34481?q=nsduh+2011&permit%5B0%5D=AVAILABLE.
Lupton, C. (2003) The financial impact of fetal alcohol syndrome [Internet]. Rockville, MD: Substance Abuse and Mental Health Services Administration [updated 2012 Dec 27; cited 2013 Feb 17]. Available from: http://www.fasdcenter.samhsa.gov/publications/cost.cfm.
Lupton, C., Burd, L., & Harwood, R. (2004). Cost of fetal alcohol spectrum disorders. Am J Med Genet C Semin Med Genet., 127C, 42–50.
United States Department of Health and Human Services. (2011) Substance Abuse and Mental Health Services Administration. White Paper on Screening, Brief Intervention and Referral to Treatment (SBIRT) in Behavioral Healthcare [Internet]. Rockville, MD: Substance Abuse and Mental Health Services Administration [cited 2013 Feb 17]. Available from :http://www.samhsa.gov/prevention/sbirt/SBIRTwhitepaper.pdf.
Rendall-Mkosi, K., Morojele, N., London, L., Moodley, S., Singh, C., & Girdler-Brown, B. (2012) A randomised controlled trial of motivational interviewing to prevent risk for an alcohol exposed pregnancy in the Western Cape, South Africa. Addiction. doi:10.1111/add.12081.
Ceperich, S. D., & Ingersoll, K. S. (2011). Motivational interviewing + feedback intervention to reduce alcohol-exposed pregnancy risk among college binge drinkers: Determinants and patterns of response. Journal of Behavioral Medicine, 34, 381–395.
Yonkers, K. A., Forray, A., Howell, H. B., Gotman, N., Kershaw, T., Rounsaville, B. J., et al. (2012). Motivational enhancement therapy coupled with cognitive behavioral therapy versus brief advice: A randomized trial for treatment of hazardous substance use in pregnancy and after delivery. General Hospital Psychiatry, 34, 439–449.
The Henry J. Kaiser Family Foundation. (2011) Focus on health reform: Preventive services covered by private health plans under the affordable care act [Internet]. Menlo Park, CA: The Henry J. Kaiser Family Foundation [cited Dec 20, 2012]. Available from: http://www.kff.org/healthreform/upload/8219.pdf.
The Henry J. Kaiser Family Foundation. (2012) Medicaid and the uninsured: Coverage of preventive services for adults in medicaid [Internet]. Menlo Park, CA: The Henry J. Kaiser Family Foundation [cited December 20, 2012]. Available from: http://www.kff.org/medicaid/upload/8359.pdf.
The Commonwealth Fund. (2011) Realizing Health Reform’s Potential: How the affordable care act will strengthen primary care and benefit patients, providers, and payers [Internet]. New York, NY: The Commonwealth Fund [cited Dec 20, 2012]. Available from: http://www.commonwealthfund.org/~/media/Files/Publications/IssueBrief/2011/Jan/1466_Abrams_how_ACA_will_strengthen_primary_care_reform_brief_v3.pdf.
Patient Protection and Affordable Care Act (2010) Pub. L. No. 111–148, 124 Stat. 119.
Donabedian, A. (2005). Evaluating the quality of medical care. Milbank Quarterly, 83, 691–729.
Larson, J. S., & Muller, A. (2002). Managing the quality of health care. Journal of health and human services administration, 25, 261–280.
Watkins, K. E., Keyser, D. J., Smith, B., Mannle, T. E., Kivlahan, D. R., Paddock, S. M. et al. (2010) Transforming mental healthcare in the Veterans Health Administration: A model for measuring performance to improve access, quality, and outcomes. Journal for healthcare quality 32(6):33–42; quiz 42–43.
Rodkey, G. V., & Itani, K. M. (2009). Evaluation of healthcare quality: A tale of three giants. American Journal of Surgery, 198(5 Suppl), S3–S8.
Kilbourne, A. M., Keyser, D., & Pincus, H. A. (2010). Challenges and opportunities in measuring the quality of mental health care. Canadian Journal of Psychiatry, 55, 549–557.
United States Preventive Services Task Force. (2004) Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: Recommendation statement [Internet]. Rockville, MD: United States Preventive Services Task Force [updated 2012 Oct; cited 2013 Feb 16]. Available from: http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrin.htm.
Floyd, R. L., Weber, M. K., Denny, C., & O’Connor, M. J. (2009). Prevention of fetal alcohol spectrum disorders. Developmental disabilities research reviews, 15, 193–199.
O’Connor, M. J., & Whaley, S. E. (2007). Brief intervention for alcohol use by pregnant women. American Journal of Public Health, 97, 252–258.
Gryczynski, J., Mitchell, S. G., Peterson, T. R., Gonzales, A., Moseley, A., & Schwartz, R. P. (2011). The relationship between services delivered and substance use outcomes in New Mexico’s Screening, Brief Intervention, Referral and Treatment (SBIRT) Initiative. Drug and Alcohol Dependence, 118, 152–157.
Michigan Quality Improvement Consortium. Routine prenatal and postnatal care [Internet]. Southfield, MI: Michigan Quality Improvement Consortium; June 2012 [cited 2013 Feb 17]. Available from: http://www.mqic.org/pdf/mqic_routine_prenatal_and_postnatal_care_cpg.pdf.
Michigan Quality Improvement Consortium. (2012) Screening, diagnosis and referral for substance use disorders [Internet]. Southfield, MI: Michigan Quality Improvement Consortium [cited 2013 Feb 17]. Available from: http://www.mqic.org/pdf/mqic_screening_diagnosis_and_referral_for_substance_use_disorders_cpg.pdf.
Department of Veteran Affairs. (2009) Department of Defense. VA/DoD clinical practice guideline for management of pregnancy [Internet]. Washington, DC: Department of Veterans Affairs [updated 2011 Dec 16; cited 2013 Feb 17]. Available from: http://www.healthquality.va.gov/pregnancy.asp.
Neighborhood Health Plan of Rhode Island. Preventive Care Guideline: Prenatal Care [Internet]. [updated 2011 Oct; cited 2013 Feb 17]. Available from: http://nhpri.org/matriarch/documents/PrenatalCareCPG5092-4-11-Updated10-18-11.pdf.
Carson, G., Cox, L. V., Crane, J., Croteau, P., Graves, L., Kluka, S., et al. (2010). Alcohol use and pregnancy consensus clinical guidelines. Journal of obstetrics and gynaecology Canada, 32(8 Suppl 3), S1–S32.
Chang, G. (2001). Alcohol-screening instruments for pregnant women. Alcohol research and health, 25, 204–209.
Chasnoff, I. J., Wells, A. M., McGourty, R. F., & Bailey, L. K. (2007). Validation of the 4P’s Plus screen for substance use in pregnancy validation of the 4P’s Plus. Journal of Perinatology, 27, 744–748.
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; January 27, 2011 [cited 2012 December 30]. Available from: http://www.cdc.gov/brfss/questionnaires/pdf-ques/2011brfss.pdf.
Chasnoff, I. J., McGourty, R. F., Bailey, G. W., Hutchins, E., Lightfoot, S. O., Pawson, L. L., et al. (2005). The 4P’s Plus screen for substance use in pregnancy: Clinical application and outcomes. Journal of Perinatology, 25, 368–374.
Watson, E. (2010). The evolution and application of the 5 P’S behavioral risk screening tool. The Source, 20(2), 27–29.
Kennedy, C., Finkelstein, N., Hutchins, E., & Mahoney, J. (2004). Improving screening for alcohol use during pregnancy: The Massachusetts ASAP program. Maternal and Child Health Journal, 8, 137–147.
Chang, G. Screening and brief intervention in prenatal care settings [Internet]. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism [cited 2012 Dec 30]. Available from: http://pubs.niaaa.nih.gov/publications/arh28-2/80-84.htm.
United States Department of Health and Human Services. (2002) National Institutes of Health. National Institute on Alcohol Abuse and Alcoholism. Alcohol Alert No. 56: Screening for Alcohol Problems—An Update [Internet]. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism [cited 2012 Dec 31]. Available from: http://pubs.niaaa.nih.gov/publications/aa56.htm.
United States Department of Health and Human Services. (2005) National Institutes of Health. National Institute on Alcohol Abuse and Alcoholism. Alcohol Alert No. 65: Screening for Alcohol Use and Alcohol Related Problems [Internet]. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism [cited 2013 Jan 1]. Available from: http://pubs.niaaa.nih.gov/publications/aa65/aa65.htm.
Burns, E., Gray, R., & Smith, L. A. (2010). Brief screening questionnaires to identify problem drinking during pregnancy: A systematic review. Addiction, 105, 601–614.
Anderson, B. L., Dang, E. P., Floyd, R. L., Sokol, R., Mahoney, J., & Schulkin, J. (2010). Knowledge, opinions, and practice patterns of obstetrician-gynecologists regarding their patients’ use of alcohol. Journal of addiction medicine, 4, 114–121.
Taylor, P., Zaichkin, J., Pilkey, D., Leconte, J., Johnson, B. K., & Peterson, A. C. (2007). Prenatal screening for substance use and violence: Findings from physician focus groups. Maternal and Child Health Journal, 11, 241–247.
Fussell, H. E., Rieckmann, T. R., & Quick, M. B. (2011). Medicaid reimbursement for screening and brief intervention for substance misuse. Psychiatric Services (Washington, D. C.), 62, 306–309.
Daly, R. (2008). Use of substance abuse codes growing under Medicaid. Psychiatric news, 43(16), 9.
Williams, E. C., Lapham, G., Achtmeyer, C. E., Volpp, B., Kivlahan, D. R., & Bradley, K. A. (2010). Use of an Electronic Clinical Reminder for Brief Alcohol Counseling is Associated with Resolution of Unhealthy Alcohol Use at Follow-Up Screening. Journal of General Internal Medicine, 25, 11–17.
Uziel-Miller, N. D., & Dresner, N. (2002). Addressing substance abuse in obstetrics and gynecology. Primary care update for Obstetricians and Gynecologists, 9, 98–104.
United States Department of Health & Human Services. Public Health Service. Indian Health Service. Clinical Reporting System User Manual [Internet]. Albuquerque, NM: Indian Health Service; June 2011 [cited 2012 Dec 30]. Available from: http://www.ihs.gov/cio/crs/documents/crsv11/bgp_111u.pdf.
United States Department of Health and Human Services. Indian Health Service. Quality of IHS Health Care. Performance Measures. Behavioral Health—Fetal Alcohol Syndrome Prevention [Internet]. Rockville, MD: Indian Health Service [cited 2013 Jan 1]. Available from: http://www.ihs.gov/qualityofcare/index.cfm?module=chart&rpt_type=gpra&measure=19.
American Medical Association. (2012) PCPI approved quality measures: Maternity care behavioral risk assessment [Internet]. Chicago, IL: American Medical Association [cited 2013 Jan 1]. Available from: http://www.ama-assn.org/apps/listserv/x-check/qmeasure.cgi?submit=PCPI.
Goler, N. C., Armstrong, M. A., Taillac, C. J., & Osejo, V. M. (2008). Substance abuse treatment linked with prenatal visits improves perinatal outcomes: A new standard. Journal of Perinatology, 28, 597–603.
Fox, D. J., & Druschel, C. M. (2003). Estimating prevalence of fetal alcohol syndrome (FAS): Effectiveness of a passive birth defects registry system. Birth Defects Research. Part A, Clinical and molecular teratology, 67, 604–608.
Babor, T. F., & Kadden, R. M. (2005) Screening and interventions for alcohol and drug problems in medical settings: What works? Journal of Trauma 59(3 Suppl): S80–S87; discussion S94–S100.
Madras, B. K., Compton, W. M., Avula, D., Stegbauer, T., Stein, J. B., & Clark, H. W. (2009). Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence, 99, 280–295.
Virginia Department of Behavioral Health and Developmental Services. (2012) Screening instruments for pregnant women and women of childbearing age: Substance use, mental health and intimate partner violence [Internet]. Richmond, VA: Virginia Department of Behavioral Health and Developmental Services [cited 2013 Jan 1]. Available from: http://www.dbhds.virginia.gov/documents/scrn-Perinatal-InstrumentsChart.pdf.
Sokol, R. J., Martier, S. S, & Ager, J. W. (1989) The T-ACE questions: Practical prenatal detection of risk-drinking. American journal of obstetrics and gynecology 160: 863–868; discussion 868–870.
Chan, A. W., Pristach, E. A., Welte, J. W., & Russell, M. (1993). Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcoholism, Clinical and Experimental Research, 17, 1188–1192.
Boston University School of Public Health. The BNI ART Institute. Tools for the Brief Negotiated Interview (BNI) [Internet]. Boston: Boston University [cited 2013 Jan 1]. Available from: http://www.bu.edu/bniart/sbirt-in-health-care/sbirt-educational-materials/sbirt-brief-intervention/.
Acknowledgments
The development of this article was possible through the support of training grant 2T32AA007567-16 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The author would also like to acknowledge feedback and suggestions during the development of the article provided by Drs. Judith Bernstein, Mary Brolin, Deborah W. Garnick, and Maria Torres, and by the anonymous reviewers who provided feedback.
Author information
Authors and Affiliations
Corresponding author
Appendix: Recommended Screening and Brief Intervention Tools
Appendix: Recommended Screening and Brief Intervention Tools
Screening
-
1.
The 4P’s Plus is copyrighted. For permission and rights to use this tool, contact Dr. Ira Chasnoff at NTI Upstream, 180 N. Michigan Ave., Suite 700, Chicago, IL 60601.
-
2.
The 5P’S:
Women’s health can be affected by emotional problems, alcohol, tobacco, other drug use, and violence. Women’s health is also affected when those same problems are present in people close to us. By ‘alcohol,’ we mean beer, wine, wine coolers, or liquor.
-
Smoking: Have you smoked any cigarettes in the past 3 months?
-
Parents: Did any of your parents have a problem with alcohol or other drug use?
-
Peers: Do any of your friends have a problem with alcohol or other drug use?
-
Partner: Does your partner have a problem with alcohol or other drug use?
-
Past: In the past, have you had difficulties in your life due to alcohol or other drugs, including prescription medications?
-
Present: In the past month, have you drunk any alcohol or used other drugs? (1) How many days per month do you drink? (2) How many drinks on any given day? (3) How often did you have 4 or more drinks per day in the last month?
-
Emotional health: Over the last few weeks, has worry, anxiety, depression, or sadness made it difficult for you to do your work, get along with people, or take care of things at home?
-
Violence: “Are you currently or have you ever been in a relationship where you were threatened, controlled, physically hurt, or made to feel afraid?”
-
Scoring: One positive answer to any of the parents, partner or past questions is a positive screen, despite negative answers to the present or peers questions [46]. The 5P’S is in the public domain [46, 65].
-
-
3.
T-ACE:
-
T Tolerance How many drinks does it take to make you feel high?
-
A Have people Annoyed you by criticizing your drinking?
-
C Have you ever felt you ought to Cut down on your drinking?
-
E Eye opener Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover?
-
Scoring: 2 points for positive response on T and 1 point for positive response on each of A, C or E, with 2 or more points indicating current prenatal consumption, pregnancy risk drinking (consumption of 1 oz or more of alcohol per day while pregnant), pre-pregnancy risk drinking (more than 2 drinks per drinking day) and lifetime alcohol diagnoses [50, 66]. The T-ACE is in the public domain [50, 65].
-
-
4.
TWEAK:
-
T Tolerance How many drinks can you hold?
-
W Worry Have close friends or relatives Worried or complained about your drinking in the past year?
-
E Eye opener Do you sometimes take a drink in the morning when you get up?
-
A Amnesia Has a friend or family member ever told you about things you said or did while you were drinking that you could not remember?
-
K(C) Cut down Do you sometimes feel the need to cut down on your drinking?
-
Scoring: 2 points for positive response on each of T and W, 1 point for positive response on each of E, A, and K, with a total score of 2 or more points indicating pregnancy risk drinking (consumption of 1 oz or more of alcohol per day while pregnant)[67]. The TWEAK is in the public domain [65].
-
Brief Intervention
The Brief Negotiated Intervention and Referral to Treatment (BNI-ART) Institute Intervention Algorithm, and other related material, are available on-line in English and Spanish at: http://www.bu.edu/bniart/sbirt-in-health-care/sbirt-educational-materials/sbirt-brief-intervention/. This website also provides materials that are useful for referral to treatment (http://www.bu.edu/bniart/sbirt-in-health-care/sbirt-educational-materials/sbirt-referral-to-treatment/) [68].
Rights and permissions
About this article
Cite this article
O’Brien, P.L. Performance Measurement: A Proposal to Increase Use of SBIRT and Decrease Alcohol Consumption During Pregnancy. Matern Child Health J 18, 1–9 (2014). https://doi.org/10.1007/s10995-013-1257-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-013-1257-2