Abstract
This study estimates the effect of maternal infections during pregnancy on childhood asthma. One-thousand four-hundred and twenty-eight pregnant women were prospectively followed using structured interviews and chart review until their child’s 6th year of life. Infections were identified from outpatient and hospital visits. Childhood asthma was defined as physician diagnosis with symptoms at age six. Adjusted odds ratios were calculated from multivariable logistic regression models. Six-hundred and thirty-five women experienced an infection during pregnancy. Among antepartum infections, maternal urinary tract infections were significantly associated with childhood asthma (aOR 1.60, 95 % CI 1.12–2.29). Chorioamnionitis and maternal group beta streptococcus colonization were not significantly associated with an increased risk in childhood asthma. This study found an increased risk of asthma in children of women diagnosed with urinary tract infections during pregnancy, while other maternal infections did not increase the risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is one of the most common chronic illnesses worldwide with an increasing prevalence and medical burden among children. Growing evidence suggests that an asthmatic phenotype may be programmed during fetal development [1–5]. In-utero exposures to infection are thought to contribute to childhood asthma through early and repetitive antigen exposure, pulmonary remodeling and altered immunologic development that leads to airway hyper-responsiveness later in life [6]. Atopic asthma is an inflammatory disease driven by the Th-2 lymphocyte immune response [7]. While pregnancy and early fetal life requires a Th-2 predominant response this typically transitions in early life to a Th-1 mediated response that is protective against atopic disease. Prenatal and early childhood exposures that deter this Th-2–Th-1 shift are thought to contribute to the development of childhood asthma [8] Previous studies of in utero exposures and atopic disease have found associations with maternal smoking [9, 10], dietary exposures [11], antibiotic use [12, 13] and environmental antigen exposure [14, 15]. The effect of antenatal maternal infection on the development of childhood asthma has been debated in the literature often due to difficulties disentangling the role of infection from antibiotic treatment. According to the hygiene hypothesis, changes in micro-flora caused by antibiotic use, cleanliness and vaccination during early life contribute to aberrant immune system development and an increased risk of asthma and atopic diseases [16, 17]. However, some theorize that while maintaining exposure to commensal flora may be protective against atopic disease, maternal exposure to certain infections and pathogens during pregnancy increases the risk of these diseases. Antenatal infections, particularly bacterial infections, have been associated with an increased risk of childhood asthma [2, 5, 18, 19]. Among the types of maternal infection, vaginitis, febrile illness [5] urinary tract infection [18], intrauterine infection [2, 8] and flu [20] have demonstrated associations with childhood asthma. The direct mechanism by which prenatal infection may translate to childhood asthma has yet to be clearly described. Human and animal models suggest that fetal inflammatory responses to infection are associated with pulmonary remodeling and the development of broncho-pulmonary dysplasia and potentially asthma [21, 22].
Group B streptococcus (GBS) colonizes the recto-vaginal mucosa in 10–30 % of pregnant women [23]. In the absence of antibiotic prophylaxis, vertical transmission of this organism contributes 1,200 cases per year of early onset neonatal sepsis, likely due to fetal aspiration of GBS while in utero or during passage though the birth canal [24]. Colonization with GBS is a unique exposure, in that women are routinely screened and receive antibiotic prophylaxis in the absence of clinical symptoms of infection and the associated inflammatory state. It is not known whether maternal GBS colonization and intrapartum antibiotic prophylaxis are associated with the development of childhood asthma. GBS provides a unique opportunity to distinguish the roles of active intrapartum infection from colonization and antibiotic exposure in the development of childhood asthma.
To examine the effect of maternal infection and GBS recto-vaginal colonization during pregnancy on the risk of childhood asthma, we analyzed data from a prospective cohort study of pregnant women and their offspring followed until 6 years of age. With detailed classification of maternal infections throughout the antepartum and intrapartum periods, we aimed to estimate the effect of maternal infection during pregnancy on childhood asthma.
Materials and Methods
Between April 1997 and June 2000, pregnant women were prospectively enrolled in a study examining the effects of asthma, asthma symptoms and asthma therapy on pregnancy and childhood outcomes. Details of the enrollment procedure have been previously published [25]. Given the outcome of interest, the cohort was enriched to include women with asthma or previous offspring with asthma. Pregnant women with a history of physician-diagnosed asthma (n = 1,343) and a simple random sample of pregnant women without asthma (n = 2,070) were recruited from 56 private obstetric practices and 15 clinics at six hospitals in Southern New England. The Yale University Human Investigations Committee approved the study, and all participants gave informed consent to participate in interviews and allowed access to their own and their children’s medical records. Details of the recruitment and enrollment procedures have been previously published [26]. A flowchart of patients showing inclusion and exclusion criteria applied to the cohort is described in Fig. 1.
At enrollment, trained research assistants interviewed women in their homes before 24 weeks gestation using a structured interview. The initial interview collected maternal demographic information, medical and obstetric history, cigarette use, household allergen exposures and information about asthma symptoms, and medication use during pregnancy and in the year before pregnancy. An adaptation of the Global Initiative for Asthma categories published by Belanger et al. [27] was used to measure the severity of asthma symptoms during pregnancy. All mothers including those without a diagnosis of asthma received an asthma symptom severity score to capture potential undiagnosed cases and differentiate between those with benign and severe disease. A postpartum interview was conducted in the hospital (n = 1,344) or by telephone (n = 544) within 1 month of delivery. Data on pregnancy complications and outcomes, illnesses diagnosed during the pregnancy and intrapartum medication exposure were obtained from hospital delivery records. The final standardized maternal interview (n = 1,505) related to the infancy and early childhood was conducted at home (87.4 %) or by telephone when the child was 6 years (±3 months) of age. Mothers with complete records for all time periods were included in the final analysis (n = 1,428).
Information about infections during pregnancy was obtained from maternal interview data and review of the maternal medical record at the completion of the pregnancy. Trained research assistants completed the Pregnancy Outcome Data Form and recorded all problems followed in the pregnancy, including infectious diseases, the reasons for all hospitalizations and emergency room visits, and intrapartum complications including chorioamnionitis. Antepartum infections included those reported during pregnancy before labor and those identified through medical record review. The data did not include the exact gestational age or dates for infections diagnosed as an outpatient or the number of times any one type of infection occurred. Chorioamnionitis was the only intrapartum infection of interest. The medical record was also reviewed for positive screening for GBS colonization prior to delivery, which we analyzed in a separate category.
Information regarding childhood asthma was obtained when the child was 6 years old (±3 months) at the final structured maternal interview. Mothers were asked: “Has the child ever been diagnosed by a doctor or health professional as having asthma?” and “Has your child had wheezing or whistling in the chest in the last 12 months?” The primary outcome in this analysis was physician-diagnosed asthma ever with history of wheezing at the 6th year of age.
Information on antibiotic use was obtained from the maternal questionnaire administered for the first and third trimester asking participants if they had taken any medications, including name, strength and frequency of use. Antibiotic exposure during labor was extracted by hospital record review conducted by study research assistants. We categorized exposure based upon any antenatal exposure during the first or third trimester alone, intrapartum exposure alone or both. We performed sensitivity analyses to account for the lack of information on second trimester antibiotic exposure.
We analyzed the effect of prenatal infectious exposure on childhood asthma using multivariable logistic regression models using SAS 9.2 (SAS Institute, Inc., Cary, NC, USA). Odds ratios (ORs) and 95 % confidence intervals were estimated for asthma based upon diagnoses of maternal antepartum infection or chorioamnionitis compared with no diagnoses of infection. Adjusted ORs were calculated adjusting for potential confounders from maternal demographics and pregnancy and pregnancy and childhood household exposures. The variables that were found by univariate analysis to be associated with infection or childhood asthma were incorporated into a stepwise logistic-regression model in which the dependent outcome was asthma at age 6. The model was refined by a stepwise selection of variables resulting in a change of 10 % or greater in the parameter estimate of infection exposure remaining in the model. The final variables included in the adjusted model along with the exposure variables of interest included maternal income, pregestational diabetes, maternal asthma severity score, smoking exposure during pregnancy, infant low birth weight status, and the presence of cockroaches in the home during the first year of life. The c statistic for the final model was acceptable at 0.72. The study was able to detect at least a 52 % increased risk of asthma with 90 % power.
Results
Characteristics of the study population at baseline and in relation to having antepartum infection, chorioamnionitis or GBS colonization are described in Table 1. The majority of women were between the ages of 25 and 35 (58 %) and 72 % of the population was white. Eleven percent smoked only during the first trimester of pregnancy and 6 % through the third trimester. Forty-four percent were diagnosed with asthma (which is higher than usual rates, by design). Five percent of births were preterm and 4.2 % low birth weight. Forty-five percent of the study population had an infection diagnosed during pregnancy; 43.2 % (n = 617) of women had an antepartum infection and 4.8 % (n = 68) had chorioamnionitis. Among antepartum infections, respiratory infections were the most common (21 %) followed by urinary tract infections (19 %). Two hundred and ninety-six (20.7 %) women had known recto-vaginal colonization with GBS.
The characteristics associated with antepartum infections listed in Table 1 included many correlates of socioeconomic status including: age <25, being unmarried, ethnicity other than white, less than or up to a high school education, income under $40,000 and smoking during pregnancy. Clinical correlates to antepartum infection included maternal asthma, high maximum asthma severity score, gestational diabetes, antepartum vaginal bleeding and low birth weight. Chorioamnionitis was associated with maternal age, marital status, household income, smoking throughout pregnancy, cesarean delivery, preterm birth and low birth weight. The characteristics associated with GBS colonization included first trimester smoking and high asthma severity.
In the study population, 15.0 % of children had asthma. In the unadjusted analyses (Table 2), the risk of childhood asthma decreased with higher maternal age and higher maternal education. The risk of asthma was increased for children whose mothers were single, African-American or Hispanic, with lower incomes or were smokers during pregnancy. Maternal clinical characteristics associated with childhood asthma included: diagnosed maternal asthma, particularly more severe asthma symptoms during pregnancy, pre-gestational diabetes and obesity and antepartum vaginal bleeding. Preterm and low birth weight infants also demonstrated a higher risk of childhood asthma.
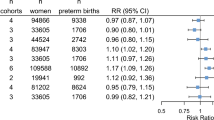
Table 3 demonstrates the unadjusted and adjusted associations between maternal infections and childhood asthma. When antepartum infections and chorioamnionitis are taken together, there was not strong evidence that having any infection in pregnancy was associated with an increased risk of asthma (aOR 1.36, 95 % CI, 0.99–1.85). Antepartum infection alone was marginally associated with an increased risk of childhood asthma (OR 1.34 95 % CI, 1.01–1.88). However, this affect was entirely attributable to the increased risk associated with urinary tract infections which demonstrated a 60 % increase in the odds of childhood asthma (OR 1.60, 95 % CI 1.12–2.29). Other types of antepartum infection, including gynecologic infections, respiratory infections and other infections, were not associated with an increased risk in childhood asthma.
Chorioamnionitis was not associated with childhood asthma at the age of 6 years (aOR 1.06, 95 % CI 0.54–2.07). Group B Strep colonization also did not demonstrate a significant impact on the risk of childhood asthma (aOR 0.87, 95 % CI 0.60–1.27).
Our evaluation of any reported antibiotic exposure during pregnancy revealed a marginal association with the development of childhood asthma (OR 1.34, 95 % CI 1.01–1.81); however, after adjusting for associated confounders, this association did not persist (aOR 1.28, 95 % CI 0.87–1.67). Given the large numbers of women with documented antepartum urinary tract infections (n = 271 (19 %), and the lack of 2nd trimester antibiotic exposure data, the time frame in which we expect most cases of UTI, we performed a sensitivity analysis excluding these subjects who were presumptively all treated. Among the remaining infections with differential exposure to antibiotics, having any antenatal exposure to antibiotics compared to no documented exposure demonstrated a significant association with childhood asthma (aOR 1.40, 95 % CI 1.03–1.91). For each of the individual infections from Table 3, adjustments for antibiotic exposure in the 1st or 3rd trimester did not significantly alter estimates.
Discussion
This analysis demonstrates that childhood asthma is more common among offspring of mothers who experienced a urinary tract infection. Other antepartum infections, intrapartum infection with chorioamnionitis and colonization with GBS were not associated with an increased risk of childhood asthma. Our study also suggests that prenatal antibiotic exposure may account for some component of this increased risk.
Prior studies have associated urinary tract infections with the development of childhood asthma. A retrospective cohort study of 15,609 children in Italy by Rusconi et al. [28] associated maternal urinary tract infections treated with antibiotics with persistent and transient early-onset wheeze in 2 year olds. Algert et al. [18] evaluated in utero infectious exposures and childhood asthma admission in a cohort of over 240,000 children and found a significant association with maternal hospital admission for pyelonephritis or cystitis and childhood asthma (aOR = 1.49, 95 % confidence interval (1.23–1.79)]. They did not find a difference in childhood asthma risk between maternal UTI admissions before or after 28 weeks, however there was evidence of a dose–response relationship, as women with two or more UTI admissions had nearly twice the odds of having a child requiring an asthma admission than those with only one maternal antepartum UTI related hospitalization. This suggests that recurrent or more severe urinary infections may have a greater impact on fetal immunologic or pulmonary development.
Urinary tract infections are the most common bacterial infections diagnosed during pregnancy. The positive findings from this study as well as others that have broadly assessed antepartum exposures suggest that further investigation into the role of urinary tract infections and childhood asthma may be warranted. Asymptomatic bacteriuria affects 2–7 % of pregnant women and 25 % of those women will experience a symptomatic urinary tract infection, which may progress to pyelonephritis [29]. The majority of women who have asymptomatic bacteriuria will screen positive during the first trimester, and most symptomatic renal infections occur in the second trimester. Bacteriuria and urinary infections have been associated with preterm birth and low birth weight [30] however there are no known associated chronic illnesses. There is no clear explanation for how prenatal urinary infections, rather than other infections, might translate to persistent asthma in children. When compared to more remote infections in the respiratory or gastrointestinal tract, it is plausible that a fetus has increased exposure to both pathogens and maternal immune factors when a clinically significant infection occurs within the genitourinary tract. A recent study in a murine model seeking to identify molecular mechanisms by which UTI may induce adverse perinatal outcomes found infiltration of cellular innate immune factors in the uteroplacental tissue of pregnant mice with Escherichia coli cystitis and prolonged elevation of inflammatory cytokines in maternal serum [31]. While this study identified a link to fetal growth restriction, it is possible that these factors could lead to fetal pulmonary remodeling or alterations in immune system development towards a pro-inflammatory, atopic phenotype.
Xu et al. [5] studied the effects of maternal vaginitis and febrile infections on 8,088 children in Finland and found a higher risk of asthma for both prenatal exposures (OR 1.41 and 1.65, respectively). Our results did not find a statistically significant association between childhood asthma and gynecologic infections that included vaginitis (OR 1.05, CI 0.70–1.60). However, there were only 198 women with gynecologic infections in our study, compared to their group of 1,772, which could explain the different findings. Xu additionally reported the association between febrile infections occurring earlier in pregnancy and childhood asthma was stronger. Our data suggests that infections experienced in the antepartum period are more influential than intrapartum infections, supporting the hypothesis that exposures during gestation have a greater potential to impact pulmonary and immunologic development than acute episodes during the perinatal period.
Few women in this cohort were diagnosed with chorioamnionitis (n = 68, 4.6 %), and this was not associated with childhood asthma. Other studies have found a positive association between chorioamnionitis on the development of childhood asthma [2, 3, 14, 19]. Keski-Nisula et al. [2] identified higher rates of asthma at ages 15–17 for the children of mothers with positive streptococcus species or anaerobic bacteria identified by amniotic or intrauterine cultures at the time of cesarean delivery. These findings were consistent with those of Kumar [3] and Getahun et al. [19] who both found an increased risk of asthma in pregnancies complicated by both chorioamnionitis and preterm birth. According to Getahun’s study, the risk of asthma diminished with increasing gestational age, such that full term pregnancies complicated by chorioamnionitis were not associated with childhood asthma. In our study, 58 of the 68 cases of chorioamnionitis occurred in full term pregnancies. Among the 10 preterm pregnancies with chorioamnionitis, there were five cases of childhood asthma. Fetal exposure to inflammatory cytokines including IL-6, -8 and tumor necrosis factor is increased with chorioamnionitis and has been linked to chronic lung disease [32]. However, it is possible that the timing of chorioamnionitis may influence its impact of fetal lung and immunologic development.
We are not aware of other studies that have investigated the association between GBS colonization on childhood asthma. Women that screen positive for GBS during the third trimester, typically receive narrow-spectrum antibiotic therapy during labor to prevent transmission to the infant and diminish the risk of neonatal sepsis. Perinatal antibiotics targeted toward GBS rapidly cross the placenta and are known to enter the fetal bloodstream at significant levels, lasting hours into neonatal life [33]. In this cohort, GBS colonization was not associated with childhood asthma. This suggests that bacterial exposure in the absence of infection and antibiotic exposure during labor alone may not predispose a fetus to asthma later in life.
Rather than maternal infection, antibiotic exposure during pregnancy may primarily influence the development of asthma in children. Prior studies have found associations between antibiotic uses in pregnancy with asthma [13]. In a recent prospective cohort study of 411 children born of mothers with asthma Stensballe demonstrated that exposure to antibiotics for both respiratory and non-respiratory infections increased the risk of asthma after controlling for multiple confounders [34]. Post-natal antibiotic exposure to the children in our study with no history of their own respiratory infection has been reported to increase asthma risk by 66 % [35]. Antibiotics may lead to asthma through alterations in the maternal and neonatal microflora that may adversely modify immune system development towards an atopic phenotype. Treatment of urinary tract infections during pregnancy involves acute antibiotic therapy for at least 7 days followed by suppressive antibiotics for the entirety of the pregnancy in the case of recurrent or severe infection and may in part explain the association found in this study. Studies have demonstrated alterations in microflora and proliferation of resistant bacteria after antibiotic use for as little as 5 days, lasting for months after the exposure [36]. Further studies support that regulating gut microflora through oral lactobacillus supplementation during pregnancy and early infancy may decrease the risk of atopic disease through early childhood [37].
There were several limitations to this study. First, exposure data were collected by patient questionnaire and a review of hospital records at the time of delivery, which may exclude minor infections that were treated as an outpatient. An additional limitation to this study was that antibiotic exposure data were not collected during the second trimester, limiting our ability to fully analyze the effect of antibiotic exposure on childhood asthma. Nor could we quantify the exact number of each type of infection during pregnancy or ascertain a dose–response relationship for disease exposure. Similarly, the outcome of interest, childhood asthma was ascertained by parental report of a physician diagnosis along with current wheeze rather than medical record abstraction, subjecting this measure to some level of potential error. The effect of antepartum infection as well as UTI on childhood asthma diminished after controlling for multiple confounders, several of which (income, marital status, smoking) are strongly associated with socioeconomic status. Infection in pregnancy could be a marker of exposures related to social class that we have not controlled for.
This study found a persistent association between urinary tract infection and childhood asthma after controlling for multiple confounders; however, why this association exists, remains unclear. As urinary tract infections are the most common infection in pregnancy and often require both acute and suppressive antibiotic therapy, it is important to understand if the infection itself or its treatment may contribute to childhood asthma. Future studies regarding the role of antenatal infection on the development of childhood asthma should further explore the illnesses timing, severity and associated pathogens as well as the duration and type of antibiotic therapy used.
References
Jones, C. A., Holloway, J. A., & Warner, J. O. (2002). Fetal immune responsiveness and routes of allergic sensitization. Pediatric Allergy and Immunology, 13(Suppl 15), 19–22.
Keski-Nisula, L., Katila, M. L., Remes, S., Heinonen, S., & Pekkanen, J. (2009). Intrauterine bacterial growth at birth and risk of asthma and allergic sensitization among offspring at the age of 15 to 17 years. Journal of Allergy and Clinical Immunology, 123, 1305–1311.
Kumar, R. (2008). Prenatal factors and the development of asthma. Current Opinion in Pediatrics, 20, 682–687.
McKeever, T. M., Lewis, S. A., Smith, C., & Hubbard, R. (2002). The importance of prenatal exposures on the development of allergic disease: A birth cohort study using the west midlands general practice database. American Journal of Respiratory and Critical Care Medicine, 166, 827–832.
Xu, B., Pekkanen, J., Jarvelin, M. R., Olsen, P., & Hartikainen, A. L. (1999). Maternal infections in pregnancy and the development of asthma among offspring. International Journal of Epidemiology, 28, 723–727.
Kirby, J. G., Hargreave, F. E., Gleich, G. J., & O’Byrne, P. M. (1987). Bronchoalveolar cell profiles of asthmatic and nonasthmatic subjects. The American Review of Respiratory Disease, 136, 379–383.
Lin, H., Mosmann, T. R., Guilbert, L., Tuntipopipat, S., & Wegmann, T. G. (1993). Synthesis of T helper 2-type cytokines at the maternal-fetal interface. Journal of Immunology, 151, 4562–4573.
Kumar, R., Yu, Y., Story, R. E., Pongracic, J. A., Gupta, R., Pearson, C., et al. (2008). Prematurity, chorioamnionitis, and the development of recurrent wheezing: A prospective birth cohort study. Journal of Allergy and Clinical Immunology, 121, 878–884.e6.
Moshammer, H., Hoek, G., Luttmann-Gibson, H., Neuberger, M. A., Antova, T., Gehring, U., et al. (2006). Parental smoking and lung function in children: An international study. American Journal of Respiratory and Critical Care Medicine, 173, 1255–1263.
Wang, C., Salam, M. T., Islam, T., Wenten, M., Gauderman, W. J., & Gilliland, F. D. (2008). Effects of in utero and childhood tobacco smoke exposure and beta2-adrenergic receptor genotype on childhood asthma and wheezing. Pediatrics, 122, e107–e114.
Robison, R., & Kumar, R. (2010). The effect of prenatal and postnatal dietary exposures on childhood development of atopic disease. Current opinion in Allergy and Clinical Immunology, 10, 139–144.
McKeever, T. M., Lewis, S. A., Smith, C., Collins, J., Heatlie, H., Frischer, M., et al. (2002). Early exposure to infections and antibiotics and the incidence of allergic disease: A birth cohort study with the west midlands general practice research database. Journal of Allergy and Clinical Immunology, 109, 43–50.
Murk, W., Risnes, K. R., & Bracken, M. B. (2011). Prenatal or early-life exposure to antibiotics and risk of childhood asthma: A systematic review. Pediatrics, 127, 1125–1138.
Peters, J. L., Suglia, S. F., Platts-Mills, T. A., Hosen, J., Gold, D. R., & Wright, R. J. (2009). Relationships among prenatal aeroallergen exposure and maternal and cord blood IgE: Project ACCESS. Journal of Allergy and Clinical Immunology, 123, 1041–1046.
Miller, R. L., Chew, G. L., Bell, C. A., Biedermann, S. A., Aggarwal, M., Kinney, P. L., et al. (2001). Prenatal exposure, maternal sensitization, and sensitization in utero to indoor allergens in an inner-city cohort. American Journal of Respiratory and Critical Care Medicine, 164, 995–1001.
Yazdanbakhsh, M., Kremsner, P. G., & van Ree, R. (2002). Allergy, parasites, and the hygiene hypothesis. Science, 296, 490–494.
Weiss, S. T. (2008). Asthma in early life: Is the hygiene hypothesis correct? Journal of Pediatrics (Rio Journal), 84, 475–476.
Algert, C. S., Bowen, J. R., Lain, S. L., Allen, H. D., Vivian-Taylor, J. M., & Roberts, C. L. (2011). Pregnancy exposures and risk of childhood asthma admission in a population birth cohort. Pediatric Allergy and Immunology, 22, 836–842.
Getahun, D., Strickland, D., Zeiger, R. S., Fassett, M. J., Chen, W., Rhoads, G. G., et al. (2010). Effect of chorioamnionitis on early childhood asthma. Archives of Pediatrics and Adolescent Medicine, 164, 187–192.
Calvani, M., Alessandri, C., Sopo, S. M., Panetta, V., Tripodi, S., Torre, A., et al. (2004). Infectious and uterus related complications during pregnancy and development of atopic and nonatopic asthma in children. Allergy, 59, 99–106.
Watterberg, K. L., Demers, L. M., Scott, S. M., & Murphy, S. (1996). Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics, 97, 210–215.
Yoon, B. H., Romero, R., Kim, K. S., Park, J. S., Ki, S. H., Kim, B. I., et al. (1999). A systemic fetal inflammatory response and the development of bronchopulmonary dysplasia. American Journal of Obstetrics and Gynecology, 181, 773–779.
Lewin, E. B., & Amstey, M. S. (1981). Natural history of group B streptococcus colonization and its therapy during pregnancy. American Journal of Obstetrics and Gynecology, 139, 512–515.
Verani, J. R., McGee, L., Schrag, S. J., & Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). (2010). Prevention of perinatal group B streptococcal disease-revised guidelines from CDC, 2010. MMWR Recommendations and Reports, 59, 1–36.
Bracken, M. B., Triche, E. W., Belanger, K., Saftlas, A., Beckett, W. S., & Leaderer, B. P. (2003). Asthma symptoms, severity, and drug therapy: A prospective study of effects on 2,205 pregnancies. Obstetrics and Gynecology, 102, 739–752.
Kang, E. M., Lundsberg, L. S., Illuzzi, J. L., & Bracken, M. B. (2009). Prenatal exposure to acetaminophen and asthma in children. Obstetrics and Gynecology, 114, 1295–1306.
Belanger, K., Hellenbrand, M. E., Holford, T. R., & Bracken, M. (2010). Effect of pregnancy on maternal asthma symptoms and medication use. Obstetrics and Gynecology, 115, 559–567.
Rusconi, F., Galassi, C., Forastiere, F., Bellasio, M., De Sario, M., Ciccone, G., et al. (2007). Maternal complications and procedures in pregnancy and at birth and wheezing phenotypes in children. American Journal of Respiratory and Critical Care Medicine, 175, 16–21.
Little, P. J. (1966). The incidence of urinary infection in 5,000 pregnant women. Lancet, 2, 925–928.
Romero, R., Oyarzun, E., Mazor, M., Sirtori, M., Hobbins, J. C., & Bracken, M. (1989). Meta-analysis of the relationship between asymptomatic bacteriuria and preterm delivery/low birth weight. Obstetrics and Gynecology, 73, 576–582.
Bolton, M., Horvath, D. J., Jr, Li, B., Cortado, H., Newsom, D., White, P., et al. (2012). Intrauterine growth restriction is a direct consequence of localized maternal uropathogenic Escherichia coli cystitis. PLoS One, 7, e33897.
Prendergast, M., May, C., Broughton, S., Pollina, E., Milner, A. D., Rafferty, G. F., et al. (2011). Chorioamnionitis, lung function and bronchopulmonary dysplasia in prematurely born infants. Archives of Disease in Childhood Fetal and Neonatal Education, 96(4), F270–F274.
Barber, E. L., Zhao, G., Buhimschi, I. A., & Illuzzi, J. L. (2008). Duration of intrapartum prophylaxis and concentration of penicillin G in fetal serum at delivery. Obstetrics and Gynecology, 112, 265–270.
Stensballe, L. G., Simonsen, J., Jensen, S. M., Bonnelykke, K., & Bisgaard, H. (2012). Use of antibiotics during pregnancy increases the risk of asthma in early childhood. The journal of Pediatrics. doi:10.1016/j.jpeds.2012.09.049.
Risnes, K. R., Belanger, K., Murk, W., & Bracken, M. B. (2011). Antibiotic exposure by 6 months and asthma and allergy at 6 years: Findings in a cohort of 1,401 US children. American Journal of Epidemiology, 173, 310–318.
Edlund, C., & Nord, C. E. (2000). Effect on the human normal microflora of oral antibiotics for treatment of urinary tract infections. Journal of Antimicrobial Chemotherapy, 46(Suppl 1), 41–48; discussion 63–65.
Kalliomaki, M., Salminen, S., Poussa, T., Arvilommi, H., & Isolauri, E. (2003). Probiotics and prevention of atopic disease: 4-year follow-up of a randomised placebo-controlled trial. Lancet, 361, 1869–1871.
Acknowledgments
Supported by Grants AI41040 and DA05484 from the National Institutes of Health.
Conflict of interest
None of the authors have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Collier, C.H., Risnes, K., Norwitz, E.R. et al. Maternal Infection in Pregnancy and Risk of Asthma in Offspring. Matern Child Health J 17, 1940–1950 (2013). https://doi.org/10.1007/s10995-013-1220-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-013-1220-2