Abstract
Large scale investment in the National Rural Health Mission is expected to increase the utilization and reduce the cost of maternal care in public health centres in India. The objective of this paper is to examine recent trends in the utilization and cost of hospital based delivery care in the Empowered Action Group (EAG) states of India. The unit data from the District Level Household Survey 3, 2007–2008 is used in the analyses. The coverage and the cost of hospital based delivery at constant price is analyzed for five consecutive years preceding the survey. Descriptive and multivariate analyses are used to understand the socio-economic differentials in cost and utilization of delivery care. During 2004–2008, the utilization of delivery care from public health centres has increased in all the eight EAG states. Adjusting for inflation, the household cost of delivery care has declined for the poor, less educated and in public health centres in the EAG states. The cost of delivery care in private health centres has not shown any significant changes across the states. Results of the multivariate analyses suggest that time, state, place of residence, economic status; educational attainment and delivery characteristics of mother are significant predictors of hospital based delivery care in India. The study demonstrates the utility of public spending on health care and provides a thrust to the ongoing debate on universal health coverage in India.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The last decade has seen increasing political commitment, a steady rise in public health spending and the introduction of the National Rural Health Mission (NRHM) to improve access to basic health services in India. Health spending by the central government has increased from 0.8 % of GDP in 2004–2005 to 1.1 % in 2008–2009 and is expected to be 3 % of GDP by 2022 [1–3]. The NRHM was introduced in April 2005 with the primary objective of improving the availability of and accessibility to quality health services in 18 high-focused statesFootnote 1[1]. About three-fourths of central government spending on health was under the NRHM. The implementation of NRHM includes conditional cash transfer schemes, accreditation of private health centres for delivery, grants for drugs and improving the health infrastructure, recruitment of health personnel and other human resources in the country.
The Janani Suraksha Yojana (JSY), a conditional cash transfer scheme in India (under the NRHM) provides cash incentives to women who deliver in public or accredited health centres. While the incentives are provided to all the pregnant women delivering in public or an accredited private health centre in high priority states (Rs. 1,400/- in rural areas and Rs. 1,000/- in urban areas), these were meant for women below the poverty line households and aged 19 years and above in low priority states (Rs. 700/- for rural and Rs. 600/- for urban) [4]. The JSY is the largest ever conditional cash transfer program in the world that targeted 26 million women in 2009–2010 [5]. Given the nature and size of investment, the NRHM has been a subject of considerable discussion among planners, policy makers, public health professionals, nongovernment organizations, academia and researchers, both nationally and globally. While policymakers focus on improving maternal and child health indicators in the country through the effective implementation of the NRHM, the public hopes to pay less for the use of improved basic services. The successful implementation of NRHM will help to achieve health related Millennium Development Goals (MDGs) and may be illustrative for the implementation of Universal Health Coverage in India.
Over the last three decades, the conditional cash transfer programs have been operational in many low and middle income countries to reduce poverty and to improve the educational attainment of children and the health of the population. Evaluative studies suggest mixed impact of these programs. Studies from Colombia, Mexico and Nicargua showed that the conditional cash transfer programs were useful in increasing the school enrollment rate, improving preventive health care and raising household consumption [6]. Jones et al. [5] in their comprehensive review of conditional cash transfer schemes found that the program is a value addition to safe motherhood needs and broader human development goals. On the other hand, some studies outlined the small and insignificant impact of public spending on health outcomes [7]. Others maintained that the linkages of public health spending and health outcomes are not automatic and that they are influenced by effective governance [8].
Though maternity care is provided free of cost in public health centres in India, the cost differs among the states due to varying registration fees, expenditures on drugs, diagnostic tests, bed charges, food and informal fees. Often the maternal health expenditures in private health centres are catastrophic for poor and illiterate women [9, 10] and the informal fees in public health centres are significantly higher than the formal fees [11]. Studies documented that out-of-pocket (OOP) expenditures on delivery care are significantly high for women who delivered in a private health centre and had caesarean delivery [12]. Though these studies provide contextual determinants of the cost of delivery, no attempt has been made to understand the recent changes in the utilization and cost of delivery care in the Empowered Action Group (EAG) states. In this context, this study examines the recent trends in utilization and cost of hospital based delivery in the EAG states of India.
The study has been conceptualized with the following rationale. First, public spending under the NRHM is large compared to any other program in the country. Though the NRHM covers all the states in India, the central focus of the program is to improve maternal care utilization in the EAG states that constitute about half of the population in the country. The improvement in the basic health situation (referred to as maternal and child health), in the country, is largely contingent on the successful implementation of the NRHM in the EAG states, as these states lag in basic health infrastructure and health outcomes. During 2004–2008, more than half of births in India were in the EAG states and many of them were unsafe. Hence, a study of recent trends in the utilization of delivery care in the EAG states will be of great interest to policy makers and program managers. Second, studies also suggest the link between public spending and health outcomes may be negligible due to crowding out of private sector provision, poor targeting or leakage in public spending and weak institutional capacity [8]. Though the EAG states are homogenous in many demographic and socio-economic indicators, they differ with respect to state policies, political commitment and administrative efficiency. Third, it is expected that the increased spending under the NRHM will eventually reduce the cost of delivery care to the end user. Thus, the analyses of household cost of delivery by economic status and educational attainment would reflect whether increased spending under the NRHM is benefiting poor and illiterate women in the EAG states. Fourth, if the increased spending under the NRHM is effective in reducing the OOP expenditure on delivery care, it will have implications on the recommendations of the High Level Expert Group (HLEG) that advocates a central role for public services in achieving universal health coverage [3].
Materials and Methods
We have used the unit data from the third round of the District Level Household Survey (DLHS 3) to understand the utilization and cost of delivery care in India over time. The DLHS 3 is the largest ever population based survey in India to date conducted during December 2007–December 2008 by 17 research organizations under the technical supervision of the International Institute of Population Sciences (IIPS), Mumbai. The prime objective of DLHS 3 was to provide key monitoring indicators on reproductive and child health in the districts of India. The DLHS 3 used a multistage systematic sampling design; a two stage stratified sampling for rural areas and a three stage stratified sampling for urban areas. The villages in rural areas and wards in urban areas comprised the primary sampling unit (PSU). In the first stage, the PSUs in both rural and urban areas were selected using the probability proportion to size sampling (PPS). In the second stage, households were selected in rural areas and census enumeration blocks (CEB) in urban areas. In the third stage, the households in urban areas were selected from census enumeration block (CEB). The households in each PSU were drawn using circular systematic sampling. Sampling weights were provided in the data set for household, ever married women and unmarried girls. The survey covered a representative sample of 720,320 households and 643,944 ever married women aged 15–49 years in 601 districts, in India. The details of the survey design and findings are available in the national report [13].
Along with other demographic and socioeconomic characteristics, the women’s schedule in DLHS 3 collected information on place and type of delivery, year of birth, cost of delivery and transportation from women who delivered after January 1, 2004. For the analysis, the place of delivery is broadly classified into public health centres, private health centres and others (home deliveries). The deliveries conducted in a public health centre or in a private health centre constitute hospital based (institutional) delivery. There were two questions on the cost of delivery care: “How much did the transportation to the health facility for delivery cost you?” and “How much cost did you incur for delivery, excluding transport cost?”. We analyzed the cost of delivery excluding the transportation cost (direct financial cost to the women which is synonymous with OOP expenditure. The utilization and cost of delivery were analyzed by place of delivery for five consecutive years (2004–2008). About 0.4 % women who did not provide any information on the cost of delivery were excluded from the analyses. The cost of delivery was independent of the incentives received under JSY. The national women’s weight was used for the national and group analyses (EAG and non-EAG states), and the state women’s weight was used for the state level analyses. Health expenditures were collected from the annual financial statement of the union budget (http://indiabudget.nic.in/afs.asp) for each year under the revenue and capital account for medical and public health and family welfare [14].
Methods
Descriptive statistics, principal component analyses (PCA), multinomial logistic regression and ordinary least square (OLS) regression were used in the analyses. The PCA was used to construct a wealth index as there was no direct economic measure (income or total household consumption expenditure) available in the dataset. We have constructed the wealth index separately for rural and urban areas to get reliable estimates [15]. A multinomial logistic regression model was used to provide the determinants of institutional delivery in EAG states. The dependent variable was categorized into, delivery in a public health centre, delivery in a private health centre and others. The independent variables used in the regression model were time, place of residence, educational attainment, order of birth, type of delivery, borrowed money, JSY beneficiary and wealth quintile. The results of the multinomial logistic regression are presented in adjusted percentages for easy interpretation. To understand the determinants of cost of delivery care, an OLS regression was attempted for the EAG states. We have taken the log of cost of delivery care at constant prices as the dependent variable. The independent variables are age of women (log), years of schooling (log), place of residence, year, birth order, place of delivery, type of delivery, borrowed money for delivery, JSY beneficiaries and wealth quintiles. The multinomial logistic regression model and the OLS are used depending on the nature of the dependent variable (categorical for utilization and continuous for cost of delivery care). It should be mentioned that the increase in the general price level (inflation) was 4 % between 2004 and 2005, 10 % between 2004 and 2006, 15 % between 2004 and 2007 and 25 % between 2004 and 2008 [16] and the estimates are provided at 2004 prices.
Results
Public Health Expenditure and Institutional Delivery in India
Figure 1 presents the public spending on health at constant prices for 2004–2011. The year 2004 was the pre-NRHM period, and the successive years constitute the NRHM period. During 2004–2011, the central government expenditure on health had increased more than three fold. The maximum increase was observed at the beginning of the NRHM period (49 % during 2005–2006), and the increase was considerably high in successive years (17 % during 2006–2007, 23 % during 2007–2008, 19 % during 2008–2009, 12 % during 2009–2010 and 7 % during 2010–2011).
Trends in Central Government Expenditure (in crores of rupees) on Health and Family Welfare in India at 2004 prices, 2004–2011. Source: Compiled from http://exim.indiamart.com/indian-budget/union-budget-archive.html (revenue and capital account under medical and public health and family welfare)
The utilization of delivery services from public health centres in India showed an increasing trend (24 % in 2004–34 % in 2008), while, that from private health centres showed a marginal decline (Fig. 2). From Figs. 1 and 2, we may infer that the increased spending under the NRHM has probably boosted the use of maternal services in public health centres and reduced the use of services from private health centres.
Trends in Institutional Delivery and the Cost of Delivery Care in the EAG States
Table 1 presents the trends in utilization of delivery services, in public and private health centres of EAG states, over a period of five years. During 2004–2008, the deliveries in public health centres, in the EAG states, have increased by 141 % (from 13 % in 2004 to 32 % in 2008) compared to an increase of 5 % in the non-EAG states. The increase was observed in all the eight EAG states with a maximum in Bihar followed by Chhattisgarh and Madhya Pradesh. On the other hand, the deliveries in private health centres declined in all the EAG states except Uttar Pradesh and Uttarakhand and the maximum decline was observed in Odisha followed by Madhya Pradesh.
Table 2 presents the mean cost of delivery and the coefficient of variation in public and private health centres, in the EAG states. During 2004–2008, the mean cost of delivery care (at constant prices) in public health centres declined for all the EAG states but not in private health centres. Among all the EAG states, the decline in cost of delivery in public health centres was greatest in Chhattisgarh, followed by Madhya Pradesh. In general, reduction in the cost of delivery in the EAG states was 52 % in public health centres compared to 17 % in private health centres. The cost of delivery in private health centres has increased in Bihar, Rajasthan, Uttar Pradesh and Uttarakhand. While the decline in cost of delivery care in public health centres in the EAG states was statistically significant, it was not so in private health centres. The coefficient of variation was 1.8 in the EAG states and 1.6 in the non-EAG states. Among the EAG states, the coefficient of variation ranged from 1.5 in Odisha to 2.0 each in Madhya Pradesh and Uttar Pradesh. We observed that the increase in the utilization and reduction, in the cost of delivery, was more pronounced in public health centres compared to private health centres in the EAG states. The decline in the mean cost of delivery in public health centres in the EAG states was possibly due to improved facilities and better availability of drugs.
Education and Wealth Differentials in the Utilisation and Cost of Delivery in the EAG states of India, 2004–2008
Studies have established that education and economic status of women are the key predictors of delivery care in India [17–19]. We have presented the education and wealth differentials in utilization of delivery care services in EAG states for 2004, 2005–2006 and 2007–2008 (Table 3). During 2004–2008, the percentage of delivery in public health centres has increased across all the educational and wealth subgroups in India and the EAG states. Interestingly, the increase in the proportion of deliveries in public health centres was significantly higher among the less educated and the poor women belonging to EAG states. Within the EAG states, the increase in utilization of delivery care services in public health centres was more pronounced among less educated women in Bihar, Madhya Pradesh and Uttarakhand. The pattern is similar among the poorest and poorer women in the EAG states but does not hold true for deliveries in private health centres.
To understand the effect of NRHM spending on the poor women who availed themselves of facility based delivery, we have presented the mean cost of delivery care by deciles of wealth index and by type of health centre. A decile divides a distribution into 10 equal parts; the first decile represents the poorest 10 % and the 10th decile represents the richest 10 % of the distribution. It is expected that the program should benefit the poor and the mean cost should decline over time. During 2004–2008, the mean cost of delivery care declined among women who had delivered in a public health centre, irrespective of their economic status, in the EAG states. However, the decline was relatively lower among the richest and richer sections of the population. For example, the mean cost of delivery had declined by 41 % in the first decile, 47 % in the second decile, 44 % in the third decile, 22 % in the ninth decile and 17 % in the tenth decile (Fig. 3). This pattern was observed in all the eight EAG states indicating that the cost of delivery care has declined in these states over time.
The mean cost of delivery among women who delivered in private health centres in the EAG states has increased or remained similar except in the tenth decile (Fig. 4).
The differentials in mean cost of delivery by wealth quintile and educational attainment of women showed a declining trend in public health centres of the EAG states (“Appendix”). Among women having less than five years of schooling, we found a 46 % decline in the cost of delivery in the public health centres, in the EAG states compared to 21 % in the non EAG states.
Determinants of Utilization and Cost of Institutional Delivery in the EAG States of India
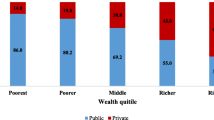
Table 4 show the results of multinomial logistic regression in terms of adjusted percentage of deliveries in public and private health centres in India. The significant predictors in the model are time, place of residence, educational attainment, order of birth, type of delivery, borrowed money, JSY beneficiary and wealth quintile. Adjusting for socioeconomic variable, time is a significant predictor of utilization of delivery care. For example, the adjusted percentage of delivery in a public health centre had increased from 13.3 to 32.3 % during 2004–2008 and the adjusted percentage of delivery in a private health centre had declined from 13.5 to 10.7 % during the same period. The adjusted percentage of delivery in a public health centre was significant in 2007 and 2008 but not in 2005 and 2006, possibly because the NRHM was intensified during the later period. Similarly, mother’s socioeconomic status is a significant predictor of institutional delivery. For example, only 5.5 % of women in the poorest wealth quintile went to a private health centre for delivery compared to 36.1 % of women in the richest wealth quintile. A similar pattern was observed in the case of public health centres (15.3 % in the poorest quintile to 26.9 % in the richest quintile). Apart from the socioeconomic status, being a JSY beneficiary was also a significant predictor for institutional delivery. Among the EAG states, we found that delivery in a public health centre was significantly higher in Madhya Pradesh (39.7 %), Odisha (37.3 %) and Rajasthan (36.6 %) compared to Uttarakhand (19.3 %).
The result of OLS regression on cost of delivery care is presented in Table 5. All the regression coefficients are in the expected direction and are significant. For example, age and education are positively and significantly associated with cost of delivery, while time, birth order and JSY beneficiaries are negatively and significantly associated with cost of delivery care in the EAG states. The regression coefficient with respect to age is 0.32 indicating that with an increase in age the cost of delivery care increases. Those who delivered in private health centres were likely to spend 78 % more than those who delivered in public health centres. The regression coefficient with respect to wealth quintile suggests that those in the richest wealth quintile are likely to spend 42 % more than those in the poorest wealth quintile.
Discussion and Conclusion
Cost and utilization of health services are interlinked. Large scale survey findings in India indicate that, among women who do not deliver at a health centre, 25 % of them cite cost as a barrier to avail themselves of facility based care. Studies also document that the cost of delivery is often catastrophic to women who are poor, less educated, rural and slum dwellers [9, 10]. To scale up the use of hospital based delivery and reduce the cost of delivery care to the end user, the Government of India has undertaken a number of reforms in the health sector. One of the benchmarks was the introduction of NRHM that aimed to improve basic health care services in public health centres in India. Though the NRHM aimed at integrating health with nutrition, sanitation and hygiene and safe drinking water, the main focus continued to be on the improvement of maternal and child health in the country. The NRHM, introduced in 2005 addressed both supply and demand side constraints by increasing public spending on health with special emphasis on the EAG states. Evaluative studies indicate that the NRHM has been successful in increasing the number of deliveries in public health centres by creating the demand for health services and reducing perinatal, neonatal and maternal deaths [20–22]. The need for human resource and managerial services is also advocated to improve delivery care in public health centres [23]. Though there is evidence of a reduction in maternal and neo-natal deaths, in the country, in recent years, little is known about recent trends in utilization and cost of delivery care in public health centres in the EAG states. The DLHS 3 with a large sample size, which recorded births in a five-year period, provides us an opportunity to delve into the effectiveness of the NRHM program in the EAG states. Accordingly, the aim of this paper is to understand whether the increased public spending by the central government under the NRHM has increased the utilization and reduced the cost of hospital based delivery in the EAG states.
Our results indicate four key findings. First, increased spending under the NRHM has indeed increased institutional delivery in the public health centres, in all the EAG states of India. On the other hand, the proportion of deliveries in the private health centres has declined in all the EAG states except Uttar Pradesh and Uttarakhand. This indicates the possibility of “crowding out” of services from private health centres. Second, we found a sharp increase in utilization and a substantial reduction in cost of delivery in public health centres of the EAG states compared to the non-EAG states. During 2004–2008, among women who delivered in a public health centre, the mean OOP expenditure declined to 52 % in the EAG states compared to 21 % in non-EAG states. The decline in mean OOP expenditures on delivery care in the public health centres, in the EAG states, is noticed even at current prices. Third, the inter-state variations in the utilization of delivery care are large even among the EAG states indicating the variability in implementation of the NRHM program by the state government. The maximum increase in delivery care from the public health centres was observed in Bihar followed by Madhya Pradesh. This perhaps was due to varying political commitment, administrative efficiency, state spending on health and utilization of central funds under the NRHM. On the other hand, political instability in Jharkhand and the leakages in the public health system in Uttar Pradesh have possibly lead to a small increase in the utilization of delivery care in public health centres. Fourth, the gap in the utilization of delivery care in the public health centres has narrowed across education and wealth groups in all the EAG states. This is because the increase in institutional delivery, in the public health centres, was more pronounced among the less educated and the poor.
The findings provide insights into the efficacy of public spending on health that has some implications for the outreach of health services for the poor and the marginalized, the role of the state government in the implementation of NRHM and the ongoing debate around universal health coverage in India. First, as the program is successful in improving service coverage and reducing the cost of delivery care in public health centres, we suggest that the cash incentive program under the JSY should continue. Second, the co-ordination of the central and state governments is essential for the effective implementation of NRHM. Third, improvement in the coverage of health services and reduction in cost under NRHM is illustrative of the efficacy of public spending in India. Recently, the working group on drug and food regulation for the twelfth Five Year Plan (2012–2017), Government of India, has recommended provision of free medicine under the NRHM/National Urban Health Mission (NUHM) in public health centres [24] and the proposal is likely to be approved soon. Such initiatives will further reduce the household cost for delivery care and save many families from catastrophic health spending. It may be mentioned that Tamil Nadu and Rajasthan provide free drugs under NRHM and have recorded an increase in the utilization of services in public health centres. Fourth, if the investment in NRHM is successful in reducing the OOP expenditures on delivery care, there is a need for similar investment in the prevention of non-communicable diseases such as cardio-vascular diseases and geriatric care in the wake of demographic and epidemiological transitions.
We also put forward the following limitations of the study. First, the segregation of cost due to doctor’s fees, medicine and diagnostic tests was not possible such information was not collected in the survey. Second, the analyses were limited to the cost of delivery in private and public health centres. A significantly higher proportion of deliveries was carried out at home and not included in the analyses.
Notes
The 18 high focused states covered under the NRHM include three broad categories, eight Empowered Action Group (EAG) states (Uttar Pradesh, Bihar, Madhya Pradesh, Rajasthan, Jharkhand, Chhattisgarh, Uttarakhand and Odisha), seven north-eastern states (Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Tripura, Sikkim) and others (Assam, Jammu and Kashmir and Himachal Pradesh).
References
Ministry of Health and Family Welfare (MOHFW), & Government of India. (2005). National Rural Health Mission (2005–2012), Mission document. Accessed through http://mohfw.nic.in/NRHM/Documents/Mission_Document.pdf.
Ministry of Health and Family Welfare (MOHFW), & Government of India. (2009). National Health Accounts India 2004–2005.
High Level Expert Group. (2011). High Level Expert Group Report on Universal Health Coverage for India, (New Delhi).
Ministry of Health and Family Welfare (MOHFW), & Government of India. (2006). Maternal Health Division, New Delhi. Janani Suraksha Yojana: Features & frequently asked questions and answers. New Delhi: Ministry of Health and Family Welfare, Government of India. Accessed March 8, 2012.
Jones, N., Samuels, F., Gisby, L., & Presier-Marshall, E. (2011). Rethinking cash transfers to promote maternal health: Good practice from developing countries. Background Note, Overseas Development Institute.
Rowlings, L. B., & Rubio, G. M. (2005). Evaluating the Impact of conditional cash transfer programs. International Bank for Reconstruction and Development. Oxford: The World Bank, OUP.
Filmer, D., & Prichett, L. (1999). The impact of public spending on health: does money matter? Social Science and Medicine, 49(10), 1309–1323.
Rajkumar, S. A., & Swaroop, V. (2008). Public spending and outcome: Does governance matter? Journal of Development Economics, 86(2008), 96–111.
Bonu, S., Bhushan, I., Rani, M., & Anderson, I. (2009). Incidence and correlates of ‘catastrophic’ maternal health care expenditure in India. Health Policy and Planning, 24, 445–456.
Skordis-Worrall, J., Pace, N., Bapat, U., Das, S., More, N. S., Joshi, W., Pulkki-Brannstron, A. M., Osrin, D. (2011). Maternal and neonatal health expenditure in Mumbai slums (India): A cross sectional study. BMC Public Health. Accessed through www.biomedcentral.com/content/pdf/1471-2458-11-150.pdf.
Sharma, S., Smith, S., Pine, M., & Winfrey, W. (2005). Formal and informal Reproductive Healthcare User Fees in Uttaranchal, India. Washington: United States Agency for International Development.
Mohanty, S. K., & Srivastava, A. (2012). Out-of-pocket (OOP) expenditure on institutional delivery in India. Health Policy and Planning. doi:10.1093/heapol/czs05.
International Institute for Population Sciences (IIPS). (2010). District level household and facility survey (DLHS-3), 2007–08. Mumbai, India: International Institute for Population Sciences.
Union Budget and Economic Survey. (2012–2013). Annual Financial Statement. Accessed through http://indiabudget.nic.in/afs.asp, on June 12, 2012.
Mohanty, S. K. (2009). Alternate wealth index and health estimates in India. Genus, 65(2), 113–137.
Ministry of Finance, Government of India. (2009). Economic Survey 2008–09. New Delhi: Oxford University Press.
Navaneetham, K., & Dharamalingam, A. (2002). Utilisation of maternal health care, services in Southern India. Social Science and Medicine, 55(10), 1849–1869.
Pathak, P. K., Singh, A., & Subramanian, S. V. (2010). Economic inequalities in maternal health care: Prenatal care and skilled birth attendance in India, 1992–2006. PLoS ONE, 5(10), e13593.
Mohanty, S. K. (2012). Multiple deprivation on maternal care in India. International Perspectives on Sexual and Reproductive Health, 38(1), 6–14.
Lim, S. S., Dandona, L., Hoisington, J. A., James, S. L., Hogan, M. C., & Gakidou, E. (2010). India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet, 375(9730), 2009–2023.
Khan, M. E., Hazra, A., & Bhatnagar, I. (2010). Impact of Janani Suraksha Yojana on selected family health behaviour in rural Uttar Pradesh. The Journal of Family Welfare, 56(Special Issue), 9–22.
Office of the Registrar General of India (ORGI). (2011). Special bulletin on maternal mortality in India 2007–09. New Delhi, India: Office of the Registrar General.
Sharma, A. K. (2009). National Rural Health Mission: Time to Take Stock. Indian Journal of Community Medicine, 34(3), 175–182.
Ministry of Health and Family Welfare (MOHFW), & Government of India. (2011). Report of the working group on Drugs & Food Regulations. Accessed through http://planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_4drugs.pdf.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 6.
Rights and permissions
About this article
Cite this article
Mohanty, S.K., Srivastava, A. Cost and Utilisation of Hospital Based Delivery Care in Empowered Action Group (EAG) States of India. Matern Child Health J 17, 1441–1451 (2013). https://doi.org/10.1007/s10995-012-1151-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-1151-3