Abstract
To examine the association between maternal depressive symptoms during early childhood of their offspring and later overweight in the children. Only children (n = 1,090) whose weights and heights were measured at least once for three time points (grades one, three and six) from the National Institute of Child Health and Human Development Study were included. Maternal depressive symptoms, defined as a Center for Epidemiologic Studies Depression Scale (CES-D) score of 16 or greater, were assessed using CES-D when the child was 1, 24, and 36 months. Childhood overweight was based on standardized height and weight measures taken during the interviews, and was defined according to appropriate CDC age- and sex-specific BMI percentiles. Generalized estimating equation was used to examine the impact of maternal depressive symptoms on the childhood overweight after adjusting for covariates. Compared to children of mothers without depression at any of the three time points, when children were one, 24 and 36 months of age, children of mothers with depression at all three time points were 1.695 times more likely to be overweight after adjusting for other child characteristics (95 % CI = 1.001–2.869). When further adjusted for maternal characteristics, children of mothers with depression at all three time points were 2.13 times more likely to be overweight (95 % CI = 1.05–4.31). Persistent maternal depressive symptoms may be associated with an increased risk of childhood overweight in their offspring. Children of mothers with depression may benefit from special attention in terms of obesity prevention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Childhood obesity is a significant public health problem in the United States (US). Ogden and colleagues have reported that approximately one in four US children aged 2–5 years and one in three school-aged children are overweight or obese [1]. Obesity in children aged 2 years or older has doubled in the last 25 years and tripled over the past 30 years [2]. Obese children and adolescents are more likely to have cardiovascular disease risk factors, such as high blood pressure, high cholesterol, and Type 2 diabetes [3]. Studies have shown that obese children and adolescents are at increased risk of adult obesity [4–7]. It is estimated that four-fifths of children who are overweight at age 10–15 years are obese at age 25 years [7]. Furthermore, adult obesity is more likely to be severe if the overweight or obesity status began prior to 8 years of age [8].
The reasons for the rapid increase in overweight or obesity over the past three decades are not fully understood [9]. Recent studies have suggested that maternal depression may play an important role in the development of childhood overweight or obesity [10, 11]. Research has shown that such depression significantly interferes with self-care and parenting and thereby contributes to childhood overweight or obesity [12].
Several studies have examined the role of maternal depression in childhood obesity and did not find an association. One cross-sectional study did not find an association for maternal depression and obesity in 6–13 years old children [13]. A recent longitudinal study reported no association between maternal postpartum distress and overweight in children 7 years of age [12]. A study by Taveras et al. [14] did show an association between maternal antenatal depression and early childhood obesity, however this association disappeared after controlling for potential confounding factors. The contradictory results might be explained by any combination of a variety of possible reasons, including study design differences, different populations, the specific variables included in the analysis, and small sample sizes. One possibility is that children might adapt well to short-term exposure to maternal depressive symptoms but be more vulnerable to long-term exposure. Perhaps mothers exposed to longer durations of depression are more likely to have a higher risk for an unhealthy lifestyle, feeding, and sleep practices [15, 16]. This might lead to parental neglect which has been found to be related to increased risk of childhood overweight [17–19].
To our knowledge, there have been few longitudinal studies examining the long-term association of maternal depressive symptoms and child overweight at multiple time points in later childhood. The purpose of our study was to evaluate the persistent impact of maternal depression on the development of childhood overweight in their offspring as compared to the children of mothers without any depressive symptoms or mothers who have depressive symptoms episodically. We evaluated both the proximal and distal impacts of maternal depressive symptoms on childhood overweight. Our study builds on the results of a recent cross-sectional study that used the Center for Epidemiologic Studies Depression Scale (CES-D) and suggested that maternal depressive symptoms are associated with a higher risk of overweight in 6–24 month old children [11]. In an effort to better understand the development of overweight in later childhood, the current study utilized a large national dataset to examine the association of maternal depressive symptoms and childhood overweight at multiple long-term follow-up time points.
Methods
Data Source and Participants
The National Institute of Child Health and Human Development (NICHD) Study of Early Child Care and Youth Development (SECCYD) was initiated at 10 sites in 1991 across the US and used conditional random sampling to minimize selection bias [20]. The 1,364 children in the study cohort were born in 1991 and grew up during the period when childhood obesity in the US nearly tripled [2, 21]. Growth data for the children were collected from birth through adolescence (from 1991 to 2005). Data on other variables was periodically collected using extensive observational and questionnaire methods.
The 1,364 families enrolled in the study were similar to non-responder families for major demographic characteristics. Eligible mothers were 18 years or older, English-speaking, and without a known or acknowledged substance abuse problem. Eligible infants were those who had not been hospitalized for more than 7 days since birth and had no obvious disabilities. Exclusion criteria included very low birth weight, premature, or sick infants. For Phases I through III of NICHD SECCYD, children were followed from birth to grade 6. A more complete description of the data collection procedures can be found in the Manuals of Operation for the NICHD Study of Early Child Care (http://www.nichd.nih.gov/research/supported/seccyd/overview.cfm).
In this study, we restricted the analysis to the 1,090 children, out of the total 1,364, who had BMI measured for at least one of the following three time points: grades one, three and six. Our study was approved by the Institutional Review Board at East Tennessee State University. Study protocols were approved by the institutional review boards of participating universities.
Study Variables
Maternal Depressive Symptoms
Maternal depressive symptoms were measured using CES-D. The CES-D provides an index of depressive symptoms and has been previously validated for use in nonclinical populations (α ranged from 0.90 to 0.91). Reliability and validation studies have shown the CES-D to be internally consistent and moderately stable over weeks (rs ≈ 0.57) [22] and months (rs ≈ 0.50) [23]. The CES-D has a strong correlation with other measures of depression. In our study mothers who scored 16 or more on the CES-D scale were classified as having depressive symptoms [22]. Maternal depressive symptoms were assessed when the child was 1 month old, 24 months old and 36 months.
Childhood Overweight
Standardized procedures were used to measure height and weight during the interviews. Height was measured with children standing without shoes, feet together, and their backs against a calibrated 7-foot measuring stick. Weight was measured using a physician’s 2-beam scale. Scales were calibrated monthly using certified calibration weights. Weight was measured with children in minimal clothing and recorded twice, each time to the nearest 0.25 pound (0.1 kg). Body mass index (BMI), defined as weight in kilograms divided by squared height in meters, was used to determine whether the child was overweight. The Centers for Disease Control and Prevention (CDC) BMI age and gender specific growth charts were used to determine a percentile score and corresponding standardized BMI z-scores (zBMI) [24]. Children were dichotomized into normal weight (BMI <85th percentile) and overweight (≥85th percentile) weight categories.
Maternal and Child Covariates
Birth weight was obtained from medical chart review. Some variables were determined at the interview when the child was 1 month of age, including child gender and race. Due to small sample size only three race categories were used: whites, blacks, and others. Maternal education was classified into five categories: (1) less than high school, (2) high school or equivalent (3) some college or associate degree (4) bachelor and (5) graduate school. Maternal age in years was analyzed as a continuous variable. Maternal employment was a dichotomous variable: (1) employed or (2) not employed, as was marital status: (1) single or (2) not-single. Family income was reported by mothers at each data collection time point, and an income-to-needs ratio (total family income relative to the federal poverty line for a family of a particular size) was calculated as an indicator of socioeconomic status. If the ratio of income to needs was less than 1, households were considered below poverty level while households with 1 and above were considered at or above poverty level. Mothers were asked whether they were currently breastfeeding at the visit when the child was 1 month of age. Breastfeeding was dichotomized: (1) breastfeeding and (2) absence of breastfeeding. The antenatal smoking variable was assessed by questions that addressed “The Year before My Child Was Born”. Smoking was dichotomized into (1) never smoked and (2) ever smoked. Social support was measured as a continuous variable based on a self-administered “Relationships with Other People” questionnaire. Eleven items were rated on a 6-point scale ranging from 1 = “none of the time” up to 6 = “all of the time”. High scores indicate more social support. Maternal sensitivity scores were measured as continuous variable assessed by observing maternal behaviors that were rated on a series of 4- or 7-point rating scales.
Statistical Analysis
Simple descriptive statistics, including means, standard deviations and proportions were used to describe maternal depressive symptoms and child body weight at different ages of children. By using the Chi-square and student t tests, participants’ characteristics of subjects included in the analytic sample (n = 1,090) were compared with subjects not included because of incomplete data (n = 274). The proportions of overweight children were assessed in grades one, three and six while maternal depressive symptoms were assessed at 1, 24 and 36 months. Simple logistic regression was used to estimate an unadjusted risk of childhood overweight at the different assessment time points (grades one, three and six) and maternal depressive symptoms were measured at 1, 24 and 36 months. At all three ages when childhood overweight was assessed, maternal depressive symptoms were measured as ranging from 0 to 3, in which 0 indicated the absence of maternal depressive symptoms at any age, 1 indicated one occurrence, 2 indicated two occurrences, and 3 indicated three occurrences. To account for the within-subject correlation of response on dependent variables of different distributions [25], we used the generalized estimating equation (GEE) method to estimate the parameters, because in comparison with traditional regression analysis at one time point (cross-sectional) or analysis of variance (ANOVA) to compare a certain outcome variable between two different time points, longitudinal GEE considers all repeated measurements of the outcome accounting for their dependency [26]. In this study, the GEE model was used to account for within-subject correlation across the three age-related time points of measurements for childhood overweight status. The sample (n = 1,090) used for analysis contained the following missing data: 99 missing (9.1 %) in grade one, 152 missing (13.9 %) in grade three, and 173 missing (15.9 %) in grade six. GEE compares the same subjects at the three time points, allowing for some missing data, and more than 80 % subjects had complete data at all three time points. Auto-regressive with first order was used as the working correlation structure in the analysis. All data analyses were performed using PASW version 19.0 statistical software (IBM SPSS, Chicago, Illinois).
Results
Maternal Depressive Symptoms and Child Body Weight at Different Ages of Children
Table 1 shows mean CES-D scores and the prevalence of maternal depressive symptoms (CES-D ≥16) at different time points, from child’s age of 1 month through grade six. The mean CES-D score was highest at month one and had decreased by 21 % at 24 months, and then remained relatively stable through grade six. The prevalence of maternal depressive symptoms was highest at month one (25.6 %) and decreased slightly at 24 months (18.3 %) and then varied from 16.8 to 19.2 %. The zBMI score and the prevalence of overweight at different time points during childhood are also presented in Table 1. The mean of zBMI score and prevalence of overweight increased gradually from 24 months to grade six. The prevalence of overweight was highest for children in grade six (34.0 %).
Comparison of Participants’ Characteristics in the Analytic Sample with Those Not Included Because of Incomplete Data
In the analytic sample (n = 1,090), average maternal age was 28.5 years, and mean birth weight was 3502.4 g (Table 2). More than 80 % of children were white and 50.7 % were males. 22.0 % of mothers smoked within the year before the child was born. About one-third of mothers had finished high school or less, one-third had finished some college and one third had a bachelor’s degree or above. More than half of the children were breastfed at 1 month of age. Approximately one-fifth of mothers lived under the poverty line, two-fifths were not employed, and 13.4 % were single. The mean score of social support was 5.2 out of a 6-point scale, indicating high social support. Compared to the analytic sample, mothers excluded from analysis due to incomplete data (n = 274) were more likely to be younger at the time of delivery (p < 0.0001), have lower education (p < 0.0001), to be single (p = 0.018), to be below the poverty line (p < 0.0001), to not breastfeed (p < 0.0001), to smoke before birth (0.002) and to not be employed (p < 0.001). However, the prevalence of maternal depression at each analytic time point was not significantly different between the analytic sample and those not analyzed: p = 0.525 at 1 month, p = 0.214 at 24 months, and p = 0.833 at 36 months. Children that were not included in the analytic sample were not significantly different from the analytic sample for gender (p = 0.160), ethnicity (p = 0.218) and mean birth weight (p = 0.061).
Maternal Depressive Symptoms at 1, 24 and 36 Months in Relation to Childhood Overweight in Grades One, Three and Six
Table 3 compares the proportions of overweight children for mothers with and without depressive symptoms at different age-related time points. In general, the overweight proportion was higher for children whose mothers were depressed at all three time points compared to mothers not depressed at any time point. It was found that maternal depressive symptoms at 1 month of child’s age was associated with an increased risk of childhood overweight in grade six (OR = 1.42, 95 % CI = 1.04–1.94); Maternal depressive symptoms at 24 months were associated with an increased risk of childhood overweight in grade six (OR = 1.66, 95 % CI = 1.17–2.35); Maternal depressive symptoms at 36 months were associated with an increased risk of childhood overweight in grade three (OR = 1.45, 95 % CI = 1.02–2.08). Compared to children of mothers who did not have depression at any time point, children of mothers who had two times of occurrence were 1.88 times more likely to be overweight in grade six (OR = 1.88, 95 % CI = 1.20–2.94). Children of mothers who had three times of occurrence were more likely to be overweight in grades one (OR = 1.88, 95 % CI = 1.01–3.47), three (OR = 1.88, 95 % CI = 1.02–3.49), and six (OR = 2.01, 95 % CI = 1.08–3.76).
Association Between Maternal Depressive Symptoms and Child Weight after Adjusting for Covariates
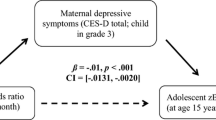
GEE (Table 4) did not show a significant association for maternal depressive symptoms at any single age after birth (1, 24 or 36 months) adjusted for child or maternal characteristics. However, when there were maternal depressive symptoms for all three time points at child’s age of 1, 24 and 36 months, compared to no depressive symptoms at any time point, children of mothers who had two times of occurrence of depression were 1.47 times more likely to be overweight (OR = 1.47, 95 % CI = 1.02–2.13). It was found that compared to children of mothers who did not have depression at any of the three time points, there was an almost two fold increased likelihood of childhood overweight (OR = 1.83, 95 % CI = 1.09–3.07). After adjusting for child’s characteristics (Table 4, Model 2), children of mothers who had three times of occurrence of depression were 1.695 times more likely to develop overweight (OR = 1.695, 95 % CI = 1.001–2.869). When maternal characteristics were added to the adjustment (Table 4, Model 3), children of mothers with three times of depression were 2.13 times more likely to develop overweight (OR = 2.13, 95 % CI = 1.05–4.31).
Discussion
Our study results provide evidence that maternal depressive symptoms may play an important role in development of overweight in children from grades one to six. Studies that have examined maternal depressive symptoms and the risk of overweight in childhood offspring have had inconsistent results. Some studies show a relationship between maternal depressive symptoms and an increased risk of children being overweight while other studies have not shown such a relationship [13, 27, 28]. One explanation may be that the impact of maternal depression occurs through interactions with other proximal, but unexamined, factors related to childhood obesity [10], such as family structure. The unadjusted results of our study showed that children of mothers who had depressive symptoms in early childhood were more likely to be overweight in grades three and six. This association might be due to the many changes and challenges mothers face during the postpartum period. These challenges include such factors as hormonal changes, weight changes, and disturbed sleep, all of which might contribute to mental health changes, including postpartum depression [29]. Postpartum depression may result in a higher risk for irritability and impaired interactions between mothers and children [30–33].
We assessed maternal depressive symptoms when the child was 1 month old, 24 months old and 36 months old. Our adjusted results using GEE found that when maternal depressive symptoms were present at more of the age-related assessment time points, there was an increased risk of a child offspring being overweight, demonstrating evidence of chronicity. These findings are in disagreement with the results of another study that found prolonged maternal depressive symptoms were associated with a lower risk for gaining weight [34]. Perhaps this difference is related to how prolonged maternal depressive symptoms were defined. In the other study, prolonged maternal depressive symptoms were defined as lasting up to 48 months [35]. Another study collected data similar to our study but did not analyze the long-term relationship of maternal depressive symptoms and childhood overweight because of a very small sample size of mothers [28]. However, our findings are consistent with a recent study that examined a large, geographically diverse sample and found a positive association between maternal depressive symptoms and increased childhood BMI [10].
Possible mechanisms for the association of maternal depressive symptoms and increased likelihood of childhood overweight may be the influence of maternal depressive symptoms on other identified risk factors for the risk of overweight in children. It has been hypothesized that maternal depressive symptoms may be related to a disordered child feeding style that could result in childhood weight problems, including underweight or obesity [11]. The results of a cross-sectional study were supportive of the viewpoints and reported that maternal depressive symptoms and socioeconomic status may be related to a permissive parenting style with an increased risk of childhood obesity [36].
Our study has several strengths. Use of US prospective cohort NICHD SECCYD data allowed for the examination of a large number of demographic, family, and environmental variables as potential risk factors for the development of overweight during childhood. The relatively large sample size of geographically diverse participants allowed for the adjustment of numerous confounders. Standardized procedures were used in our study to measure height and weight for calculating the child’s BMI. The use of self-reported heights and weights has been shown to be less accurate than direct measures [37]. The use of CES-D for determining maternal depressive symptoms was important because this instrument has been widely used and well validated. Depressive symptoms based on the CES-D have been demonstrated to be related to clinical ratings of depression [22]. GEE was used to adjust for confounding while evaluating the impact of maternal depressive symptoms on childhood overweight at multiple age-related specific time points. The findings of our study add to the current literature regarding the relationship between chronic maternal depressive symptoms and the risk of overweight developing in childhood offspring. If replicated by other studies, maternal depressive symptoms may need to be addressed as one factor to deal with childhood overweight or obesity.
As is true with most studies, our study had several limitations. Some selection bias may have occurred because of loss to follow up and incomplete data. Particularly, the sample selected for analysis was less likely to the poverty level income and more likely to have a higher education. Since low socioeconomic status (SES) may be associated with higher risk of children becoming obese [38], the potential selection bias in our study may have weakened the strength of our results. This would be due to the more likely exclusion of low SES subjects from analysis. An important limitation of our study was the lack of data for parental BMI and dietary intake in the children. These factors have been suggested as predictors of childhood obesity by the results of previous studies [39, 40] and their inclusion would have strengthened our ability to assess potential confounding. Although the potential of residual confounding remains, the nature and direction of that confounding has not been established and the role of maternal depressive symptoms should be more fully evaluated. An important strength was the CES-D to determine depressive symptoms in mothers. CES-D has been validated as an adequate screening tool and useful for epidemiologic studies, although it is not as accurate as more clinically-based evaluation tools [41, 42].
Conclusions
Persistent maternal depressive symptoms may be associated with an increased risk of overweight in childhood offspring. Additional studies that are able to include such important variables as parental BMI and the dietary intake of children are needed to replicate our findings and to provide additional evidence regarding the nature of the association of maternal depressive symptoms and the increased risk of overweight children. If our findings are confirmed, there is the potential benefit for development of childhood overweight or obesity interventions that incorporate maternal mental health status into obesity prevention strategies.
Abbreviations
- NICHD SECCYD:
-
The National Institute of Child Health and Human Development Study of Early Child Care and Youth Development
- CES-D:
-
Center for Epidemiologic Studies Depression Scale
References
Ogden, C. L., Carroll, M. D., Curtin, L. R., et al. (2010). Prevalence of high body mass index in US children and adolescents, 2007–2008. The Journal of the American Association (JAMA), 303(3), 242–249.
Ogden, C. L., Flegal, K. M., Carroll, M. D., et al. (2002). Prevalence and trends in overweight among US children and adolescents, 1999–2000. The Journal of the American Association (JAMA), 288(14), 1728–1732.
Freedman, D. S., Mei, Z., Srinivasan, S. R. et al. (2007). Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. The Journal of Pediatrics, 150(1), 12.e2–17.e2.
Bouchard, C. (1997). Obesity in adulthood—the importance of childhood and parental obesity. New England Journal of Medicine, 337(13), 926–927.
McLanahan, S., & Sandefur, G. (1994). Growing up with a single parent: What hurts, what helps. Cambridge, MA: Harvard University Press.
Serdula, M. K., Ivery, D., Coates, R. J., et al. (1993). Do obese children become obese adults? A review of the literature. Preventive Medicine, 22(2), 167–177.
Whitaker, R. C., Wright, J. A., Pepe, M. S., et al. (1997). Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine, 37(13), 869–873.
Freedman, D. S., Khan, L. K., Dietz, W. H., et al. (2001). Relationship of childhood overweight to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics, 108(3), 712–718.
Anderson, P. M., Butcher, K. F., & Levine, P. B. (2003). Maternal employment and overweight children. Journal of Health Economics, 22, 477–504.
McConley, R. L., Mrug, S., Gilliland, M. J., et al. (2011). Mediators of maternal depression and family structure on child BMI: Parenting quality and risk factors for child overweight. Obesity, 19, 345–352.
Surkan, P. J., Kawachi, I., & Peterson, K. E. (2008). Childhood overweight and maternal depressive symptoms. Journal of Epidemiology and Community Health, 62, e11.
Ajslev, T. A., Andersen, C. S., Ingstrup, K. G., et al. (2010). Maternal postpartum distress and childhood overweight. PLoS One, 30, e11136.
Gibson, L. Y., Byrne, S. M., Davis, E. A., et al. (2007). The role of family and maternal factors in childhood obesity. The Medical Journal of Australia (MJA), 186, 591–595.
Taveras, E. M., Gillman, M. W., Kleinman, K., Rich-Edwards, J. W., & Rifas-Shiman, S. L. (2010). Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics, 125, 686–695.
George, G. C., Milani, T. J., Hanss-Nuss, H., et al. (2005). Compliance with dietary guidelines and relationship to psychosocial factors in low-income women in late postpartum. Journal of the American Dietetic Association, 105, 916–926.
Paulson, J. F., Dauber, S., & Leiferman, J. A. (2006). Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics, 118, 659–668.
Knutson, J. F., Taber, S. M., Murray, A. J., et al. (2010). The role of care neglect and supervisory neglect in childhood obesity in a disadvantaged sample. Journal of Pediatric Psychology, 35, 523–532.
Lissau, I., & Sorensen, T. I. (1994). Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet, 343, 324–327.
Whitaker, R. C., Phillips, S. M., Orzol, S. M., et al. (2007). The association between maltreatment and obesity among preschool children. Child Abuse and Neglect, 31, 1187–1199.
Study of Early Child Care and Youth Development Phase I Manuals. (2008). Chapter 4: Recruitment procedures. Retrieved Sep 18, 2010, from https://secc.rti.org/display.cfm?t=m&i=Chapter_4.
Strauss, R. S., & Pollack, H. A. (2001). Epidemic increase in childhood overweight, 1986–1998. The Journal of the American Association (JAMA), 286, 2845–2848.
Radloff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401.
Lewinsohn, P. M., Hoberman, H. M., & Rosenbaum, M. (1988). A prospective study of risk factor for unipolar depression. Journal of Abnormal Child Psychology, 97, 251–264.
Kuczmarski, R. J., Ogden, C. L., Guo, S. S. et al. (2000). CDC growth charts for the United States: Methods and development. Vital Health Statistics, 11(246), 1–190.
Zeger, S. L., & Liang, K. Y. (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 42, 121–130.
Twisk, J. W. R. (2003). Applied longitudinal data analysis for epidemiology: A practical guide (pp. 120–144). Cambridge: Cambridge University Press.
O’Brien, M., Nader, P. R., Houts, R. M., et al. (2007). The ecology of childhood overweight: A 12-year longitudinal analysis. International Journal of Obesity, 31, 1469–1478.
Grote, V., Vik, T., Kries, R. V., et al. (2010). Maternal postnatal depression and child growth: A European cohort study. BMC Pediatrics, 10, 14.
Nemeroff, C. B. (2008). Understanding the pathophysiology of postpartum depression: Implications for the development of novel treatments. Neuron, 59, 185–186.
Brockington, I. (2004). Postpartum psychiatric disorders. Lancet, 363, 303–310.
Knutson, J. F., Taber, S. M., Murray, A. J., et al. (2010). The role of care neglect and supervisory neglect in childhood obesity in a disadvantaged sample. Journal of Pediatric Psychology, 35, 523–532.
O’Hara, M. W. (2009). Postpartum depression: What we know. Journal of Clinical Psychology, 65, 1258–1269.
Wisner, K. L., Parry, B. L., & Piontek, C. M. (2002). Clinical practice. Postpartum depression. New England Journal of Medicine, 347, 194–199.
Hendrick, V., Smith, L. M., Hwang, S., et al. (2003). Weight gain in breastfed infants of mothers taking antidepressant medications. Journal of Clinical Psychiatry, 64, 410–412.
Santos, I. S., Matijasevich, A., Domingues, M. R., Barros, A. J., & Barros, F. C. (2010). Long-lasting maternal depression and child growth at 4 years of age: A cohort study. Journal of Pediatrics, 157(3), 401–416.
Topham, G. L., Page, M. C., Hubbs-Tait, L., et al. (2010). Maternal depression and socio-economic status moderate the parenting style/child obesity association. Public Health Nutrition, 13, 1237–1244.
Timperio, A., Salmon, J., Telford, A., et al. (2005). Perceptions of local neighbourhood environments and their relationship to childhood overweight and obesity. International Journal of Obesity, 29, 170–175.
Wang, Y. (2001). Cross-national comparison of childhood obesity: The epidemic and the relationship between obesity and socioeconomic status. International Journal of Epidemiology, 30, 1129–1136.
Vandewater, E. A., & Huang, X. (2006). Parental weight status as a moderator of the relationship between television viewing and childhood overweight. Archives of Pediatrics and Adolescent Medicine, 160, 425–431.
Huang, T. T., Howarth, N. C., Lin, B. H., Roberts, S. B., & McCrory, M. A. (2004). Energy intake and meal portions: Associations with BMI percentile in US children. Obesity Research, 12(11), 1875–1885.
Coyne, J. C., & Schwenk, T. L. (1997). The relationship of distress to mood disturbance in primary care and psychiatric populations. Journal of Consulting and Clinical Psychology, 65, 161–168.
Santor, D. A., & Coyne, J. C. (1997). Shortening the CES-D to improve its ability to detect cases of depression. Psychological Assessment, 9, 233–243.
Acknowledgments
Some data from this study were presented orally at the 2010 Greg Alexander Outstanding Students Papers Session in Maternal and Child Health for the 138th American Public Health Association Annual Meeting in Denver, November 8, 2010.
Conflict of interest
The authors have no disclosures of competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, L., Anderson, J.L., Dalton III, W.T. et al. Maternal Depressive Symptoms and the Risk of Overweight in Their Children. Matern Child Health J 17, 940–948 (2013). https://doi.org/10.1007/s10995-012-1080-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-1080-1