Abstract
Breastfeeding benefits both infant and maternal health. Use of epidural anesthesia during labor is increasingly common and may interfere with breastfeeding. Studies analyzing epidural anesthesia’s association with breastfeeding outcomes show mixed results; many have methodological flaws. We analyzed potential associations between epidural anesthesia and overall breast-feeding cessation within 30 days postpartum while adjusting for standard and novel covariates and uniquely accounting for labor induction. A pooled analysis using Kaplan–Meier curves and modified Cox Proportional Hazard models included 772 breastfeeding mothers from upstate New York who had vaginal term births of healthy singleton infants. Subjects were drawn from two cohort studies (recruited postpartum between 2005 and 2008) and included maternal self-report and maternal and infant medical record data. Analyses of potential associations between epidural anesthesia and overall breastfeeding cessation within 1 month included additional covariates and uniquely accounted for labor induction. After adjusting for standard demographics and intrapartum factors, epidural anesthesia significantly predicted breastfeeding cessation (hazard ratio 1.26 [95 % confidence interval 1.10, 1.44], p < 0.01) as did hospital type, maternal age, income, education, planned breastfeeding goal, and breastfeeding confidence. In post hoc analyses stratified by Baby Friendly Hospital (BFH) status, epidural anesthesia significantly predicted breastfeeding cessation (BFH: 1.19 [1.01, 1.41], p < 0.04; non-BFH: 1.65 [1.31, 2.08], p < 0.01). A relationship between epidural anesthesia and breastfeeding was found but is complex and involves institutional, clinical, maternal and infant factors. These findings have implications for clinical care and hospital policies and point to the need for prospective studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The importance of breastfeeding to the short- and long-term health of children and their mothers is significant and well documented [1]. The American Academy of Pediatrics recommends exclusive breastfeeding for 6 months and continued breastfeeding after the introduction of solid foods for at least 1 year, and for as long thereafter as mother and baby desire [2]. Exclusive breastfeeding defined as no other food or drink except breast milk is recommended for the first 6 months of life [3]. Oral rehydration solutions, medications, and vitamins are allowed. At 6 months postpartum, among US infants, only 44.3 % are breastfeed and only 14.8 % are breastfeed exclusively (2008 provisional data), both below the Healthy People 2020 objectives of 60.6 and 25.5 % respectively [4]. Maternal, infant, professional, hospital and workplace practices contribute to these low rates [2]. Other factors have anecdotal support, but lack scientific evidence. For example, epidural anesthesia during labor may affect breastfeeding outcomes but research findings are inconclusive [5, 6].
Epidural anesthesia is employed variously during the intrapartum period including pain relief during labor and anesthesia during cesarean sections. This regional anesthetic, considered the most effective form of pharmacologic labor pain relief, is injected into the lumbar epidural space via a catheter providing pain relief to the lower part of the body without causing complete loss of sensation [7–10]. Based on the practitioner it can contain different amounts and combinations of medications including local anesthetics and opioids. Of note a Cochrane review of 20 randomized clinical trials of epidural anesthesia assessed numerous intervention effects (e.g. pain, maternal satisfaction and safety of interventions (e.g. cesarean delivery) [11]. Although identified as an outcome of interest by the review’s authors, only one included study assessed a breastfeeding outcome: time of initiation of lactation [12]. No difference was found between epidural anesthesia groups; duration of breastfeeding was not assessed.
Numerous epidemiologic studies, with varying results, specifically analyzed the relationship between intrapartum epidural use and breastfeeding behaviors such as infant suckling, infant hand movements, and hormone release in terms of breastfeeding outcomes including initiation, exclusivity, and duration. Multiple studies found that epidurals are negatively associated with some breastfeeding behaviors, hormone release, and outcomes [5, 13–22]. By contrast, other studies found no such relationships [17, 23–27], including one randomized clinical trial [6]. Some argue that this one trial has settled the discussion about a potential deleterious relationship between breastfeeding and use of epidural [28]. As with many of the epidural and breastfeeding studies, the trial’s analyses did not include covariates well-known to be associated with breastfeeding (e.g. breastfeeding intention, goal; marital/partner status). Further it was not powered to detect differences in breastfeeding rates and was conducted in the United Kingdom where practices and supports for breastfeeding likely differ from those in the US.
All of these studies varied in design, sample size, outcome definition, exposure definition, control group, potential confounders included, and overall rigor making assessment of aggregate evidence difficult. One common major limitation was the use of heterogeneous comparison groups (e.g. combining mothers receiving lower dose epidurals, other analgesia, or no epidural, or including cesarean and vaginal deliveries (medicated and unmedicated). This increases the likelihood of spurious results and complicates interpretation of findings. Another common limitation was how authors defined epidural use (e.g. medical record data on dose, medication, length of anesthesia/labor). Some used maternal self-report. Given these methodological issues, the association between epidural use and breastfeeding outcomes remains uncertain.
Another avenue of research (both animal and human) sheds light on the complex mechanisms by which epidural use may lead to lower oxytocin levels during and following labor, and the role of exogenous oxytocin [29]. Lower levels are associated with compromised mother-offspring interactions in animals and in humans with poor initial and ongoing breastfeeding outcomes [30–35].
Given the complexity of these relationships, the Academy of Breastfeeding Medicine in 2006 questioned whether epidurals are either associated with poor breastfeeding outcomes or may be a proxy for another mechanism that contributes to poor breastfeeding outcomes. In view of breastfeeding’s importance to both infants’ and mothers’ health, the relationship between epidural use and breastfeeding outcomes warrants further study [36]. Therefore using additional covariates and a novel methodology, which accounts for medications given at different doses over time, we explored the potential association between intrapartum epidural anesthesia use and overall breastfeeding cessation within 1 month postpartum.
Methods
Setting
Over 8,000 births occur annually in Monroe County, in upstate New York. The area is served primarily by three community hospitals and one regional perinatal center. Obstetric care is comparable across the hospitals with high risk mothers concentrated in the latter and lower risk mothers distributed across all four. Women presenting in labor or for induction of labor may be admitted to high or low risk labor-delivery-recovery or labor-delivery-recovery-postpartum units. Ambulation while allowed, depending on fetal heart rate monitoring needs, is unusual in the active phase of labor. Exogenous oxytocin (e.g. Pitocin®) is administered to approximately 25 % of mothers (for intrapartum induction or augmentation), and for the majority of mothers immediately after delivery to prevent uterine atony. When used, intrapartum exogenous oxytocin is infused at rates ranging from 1 μ/min to >20 μ/min, with durations ranging from hours to days. Postpartum, administration may be intravenously (IV) or intramuscularly (IM). Epidural anesthesia during labor is common (52 %) and often receive several liters of fluid during labor and delivery. Postpartum, rooming-in and breastfeeding are encouraged; at discharge approximately 74 % of mothers are breastfeeding [37].
To maximize the number of mothers with the exposure of interest (intrapartum epidural anesthesia) we drew subjects from two local cohort studies, one prospective and one retrospective. The former evaluated in-hospital breastfeeding support [Feeding Your Infant (FYI) study] and the latter evaluated perinatal breastfeeding support [Infant Feeding (IF) study]. During 2005 the FYI study enrolled 842 breastfeeding mothers from two community hospitals. Maternal inclusion factors were: English speaking, age 18 and above, low risk pregnancy and a singleton term birth. Participants completed an interviewer-administered survey at hospital enrollment and provided written informed consent to release of data from the maternal and infant hospital records and hospital birth certificate (BC).
The original study tracked breastfeeding until age 6 months, via mailed surveys.
Relevant to this analysis mothers completed a survey at 2-weeks and 3-months.
Twenty-three % of the sample consisted of minority women (African-American or Hispanic) and 48 % were primiparas. Most (93 %) were high school graduates. During 2008, the IF study enrolled 419 mothers at area WIC clinics (Special Supplemental Nutrition Program for Women, Infants and Children) who delivered at one of three hospitals. Eligible mothers had to be <15 months postpartum at enrollment, at least age 16 at the time of birth, and have intended to breastfeed. As in the FYI study they all had low-risk pregnancies and singleton term births.
Written informed consent was obtained. Subsequently, participants completed an interviewer-administered survey and provided authorization enabling access to their maternal and infant hospital, prenatal and WIC records and BC.
Enrolled mothers were primarily Black and/or Hispanic (79 %). Additionally 43 % were primiparous, and 63 % had completed high school. Hospital BC data were gathered by trained hospital birth registrars using standardized protocols [38]. Both studies received approval from the Research Subjects Review Board at the University of Rochester.
Study Population
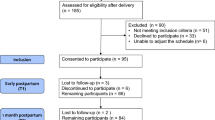
Analyses were restricted to 727 healthy mothers from these two cohorts with healthy term singleton vaginal deliveries and who had initiated breastfeeding (ever breastfeed once).
Birth Hospitals
Subjects delivered at one of three hospitals. One community hospital (Level I nursery) and the perinatal center (Neonatal ICU) are part of the same health system. The other community hospital is in a different health system, has a Level II nursery and was a Baby Friendly designated hospital (BFH) since 2000. While there were commonalities across anesthesiologists, none of the hospitals had standardized epidural anesthesia practices.
Data Sources/Measurement
For two hospitals, medical record data were abstracted from electronic hospital records capturing one-time and recurring events during the obstetric period. Manual medical record abstraction occurred at the BFH using the same variables. Trained research staff abstracted all data. An obstetric anesthesiologist verified epidural anesthesia use and other relevant details.
To assess possible early epidural anesthesia effects the primary study outcome was breastfeeding cessation within 1 month (30 days) (maternal self-report). Epidural anesthesia use was dichotomized with “yes” defined as any anesthetic agent(s) in the epidural or peridural space; this included bolus doses, continuous labor infusions, and patient controlled pumps, and excluded local, spinal, or general anesthesia.
Maternal age, education, race/ethnicity, parity, income status, and mode of delivery were obtained from the hospital BC [38]. Abstraction of these data are considered to have acceptable reliability [38–40]. Anyone with either prenatal WIC enrollment (maternal self-report on the survey or BC) or, with a Medicaid-funded delivery (per BC) were categorized as “low income: yes.” Birth hospital and breastfeeding data, obtained from the maternal surveys, included postpartum confidence in ability to breastfeed (high, medium, neutral or low), prenatal breastfeeding plan (none, timed goal [e.g. “6 months”], specific milestone [e.g. “until baby gets teeth”]), and age of infant at cessation of overall breastfeeding or if still breastfeeding. Administration of either IV or IM oxytocin and presence of postpartum edema were collected through maternal medical records (Table 1).
Statistical Methods
Bivariate analyses compared mothers who had and had not received epidural anesthesia, across identified demographic, obstetric, and breastfeeding factors. To describe differences in the distribution of these factors across exposure groups, Chi-square tests detected covariates associated with epidural anesthesia use for inclusion in multivariable analyses.
We employed the Kaplan–Meier method and corresponding log-rank test to evaluate the crude relationship between time and cessation of breastfeeding (30 days) and epidural anesthesia use. Since our interest is in cessation rather than continuation of breastfeeding, we defined an ‘event’ as cessation of breastfeeding within 1 month postpartum. A modified Cox Proportional Hazard model applied an independent incremental approach to account for the recurring use of exogenous oxytocin at different doses (referred to as time-varying discussed below) and estimated the multivariable effect of epidural anesthesia on overall breastfeeding cessation, producing hazard ratios (HR) and corresponding 95 % confidence intervals (CI). Key covariates of interest were included in multivariable analyses, and this model was adjusted for standard demographics (age, education, race, parity, income, and birth hospital), exogenous oxytocin (separating IM and IV), documentation of postpartum edema, planned breastfeeding duration, and confidence in ability to breastfeed during initial postpartum period.
This analysis statistically accounts for changes in exogenous oxytocin use during labor. This time-varying methodology counts a sequence of events across time within a single subject [41, 42]. The resulting risk estimates are iteratively weighted across each increment. Hazard ratio interpretation is the same as the standard interpretation and explains the probability of breastfeeding cessation within 1 month. This approach requires independence across subjects [43]. To account for potential non-independence between these increments within individuals, as recommended, we applied a robust variance estimator (Sandwich) to inflate the standard error associated with confidence interval estimation [41, 42].
Using the log rank test comparing two survival curves and a two-sided alpha of 0.05, we had over 80 % power to detect a 12 % difference in breastfeeding cessation within 1 month postpartum between epidural anesthesia groups. Analyses were conducted in Statistical Analysis Systems, version 9.2 (SAS Institute, Cary, NC, USA). All p-values were two-sided, and significance was set at p < 0.05.
Results
As depicted in Table 2, relative to mothers not receiving epidural anesthesia, those who did were significantly more likely to be primiparous, give birth at a non-BFH, receive IV oxytocin intrapartum, not receive IM oxytocin postpartum and have lower confidence in their ability to breastfeed. No significant differences were observed across other demographic, obstetric, or breastfeeding factors.
Kaplan–Meier curves depicted a significant crude relationship between epidural anesthesia use and breastfeeding cessation within 1 month (p < 0.01; Fig. 1). While the overall censoring rate was 84.3 %, the percentage of left-censored data (unknown if breastfeeding cessation had occurred by 30 days) was fairly low (11.7 %) relative to right-censored data (72.6 %) (breastfeeding cessation had not occurred by 30 days).
As depicted in Fig. 1, some mothers ceased of breastfeeding starting the first postpartum day. This is not surprising since ever breastfeed was the inclusion criteria. Using a modified Cox Proportional Hazard approach that adjusted for standard demographics, breastfeeding factors, and time time-varying effects of IV and IM oxytocin, epidural anesthesia significantly predicted breastfeeding cessation (HR 1.26; [95 %CI: 1.10, 1.44]); other significant risk factors included birth hospital, maternal age, income, education, planned breastfeeding goal and breastfeeding confidence (Table 3).
Comparison of BFH status (Yes/No) using post hoc analysis resulted in two modified Cox models (Table 3). In both stratified models, epidural anesthesia significantly predicted overall breastfeeding cessation (BFH HR: 1.19 [1.01, 1.41], p < 0.04; non-BFH HR 1.65 [1.31, 2.08], p < 0.01); IV oxytocin protected against early breastfeeding cessation (BFH model) (HR 0.67 [0.53, 0.86], p < 0.01) but increased the risk of early breastfeeding cessation in the non-BFH model (HR 1.50 [1.25, 1.80]). Regardless of hospital status, mothers with epidural anesthesia were significantly more likely to cease breastfeeding within 1 month; significant independent risk factors across the stratified models included maternal education, income, and planned breastfeeding goal.
Since both epidural anesthesia and IV oxytocin were significant in the stratified modified Cox models, we assessed the multiplicative effect of epidural anesthesia and IV oxytocin. While the overall interaction was not significant, the combination of both epidural anesthesia and IV oxytocin negatively affected breastfeeding (HR: 1.34 [1.00, 1.79]). The absence of both factors was protective (HR: 0.88 [7.70, 0.93]) (data not shown).
Discussion
These analyses, using a multivariable Cox model and including both common confounders and unique covariates, found an association between epidural anesthesia and breastfeeding cessation at 1 month among mothers with healthy, term vaginal births. These analyses included additional refinements to account for exogenous oxytocin, differentiating between modes of oxytocin administration and accounting for variable timing of doses. Other factors independently associated with breastfeeding cessation at 1 month included younger age, lower income, less education, lack of timed breastfeeding goal and low breastfeeding confidence. Our findings also suggest that mothers receiving both epidural anesthesia and IV oxytocin represent the group most likely to cease breastfeeding within 1 month postpartum, while mothers receiving neither represent the lowest risk group.
Subsequent analyses examined between hospital differences. Two post hoc analyses (BFH only; non-BFH) also demonstrated a significant relationship between early breastfeeding cessation and epidural anesthesia. Low income, less education, and no breastfeeding goal continued to predict early cessation. Interestingly both stratified analyses demonstrated a significant relationship with IV oxytocin administration; in the BFH hospital it was protective, while in the other hospitals it increased the risk of early cessation. The different direction of these associations may be due to practice and policy differences attributable to institutional rather than BFH-specific practices.
These analyses not only included a large number of confounders but also several covariates absent from other secondary analyses (income, breastfeeding plan, breastfeeding confidence, oxytocin use, and postpartum edema) [44]. While several contributed to early breastfeeding cessation, several well-known confounders were not consistently significant: race, parity, and age. Clinical and hospital practices may override their effect on breastfeeding. Alternatively, as described by Wieczorek et al. [27] substantial prior breastfeeding experience may offset the effect of epidural anesthesia.
In the United States, epidural anesthesia rates are increasing [28]. At the same time, despite additional programs, policies and funding to support breastfeeding, improvements in breastfeeding duration are marginal. Since 2004 the average annual change in duration at 6 months and exclusive breastfeeding at 3 months are .07 and 1.13 % respectively [4]. Furthermore epidural anesthesia may interfere with the establishment and maintenance of full lactation in some women, but not in others. Our findings reinforce the importance of clarifying whether the relationship between epidural anesthesia and breastfeeding has implications for clinical practice.
If a relationship exists, there are several potential mechanisms. First, the agents administered in epidurals, like many other maternal medications, cross the placenta and may affect the infant’s suckling ability [19, 21]. Poor suckling could contribute to delayed initiation, less breast milk consumption, low infant weight gain, and early formula supplementation [21, 45–47].
An alternate explanation warranting further exploration is the inter-relationship between epidurals, exogenous oxytocin use, endogenous oxytocin levels, and breastfeeding outcomes. Epidural anesthesia is associated with exogenous oxytocin, that in turn is associated with delayed breastfeeding initiation and in-hospital formula supplementation [21]. Epidural anesthesia is also independently associated with decreased endogenous oxytocin levels [30]. Exogenous oxytocin may interfere with endogenous oxytocin release or uptake; mothers receiving both epidural anesthesia and exogenous oxytocin administered by the obstetrician demonstrated significantly lower mean endogenous oxytocin levels while breastfeeding within 2 days postpartum [22]. Furthermore, exogenous oxytocin may be a marker of or a factor contributing to obstetric stress. A study of 63 mothers observed higher cortisol levels (stress indicator) during skin-to-skin breastfeeding within 2 days postpartum among mothers receiving both epidurals and exogenous oxytocin relative to those receiving epidurals alone [48].
It is unclear whether the relationship between epidural anesthesia with overall breastfeeding cessation represents a direct effect or whether epidurals are a marker for other unmeasured confounding factors. Alternatively, any effect on breastfeeding outcomes could be a result of synergism i.e., the combination of epidurals, prolonged labor, and related care practices associated with exogenous oxytocin. While biologically plausible, the exact mechanism is not known.
When possible, we addressed several criticisms associated with previous research to further clarify the association between epidural anesthesia and breastfeeding cessation. Our analysis was adequately powered and we established a clearly defined, homogeneous comparison group thereby minimizing exposure misclassification. Furthermore, we included many relevant demographic and obstetric variables not used in previous analyses so both known and novel potential confounders were included. We reaffirmed a potential synergistic relationship between epidural anesthesia and IV oxytocin interaction [5]. Lastly, we accounted for the time-varying periods of use and non-use by applying a novel statistical methodology [49].
Despite the above efforts, this study has limitations. Our analysis was limited to the primary studies’ inclusion criteria; results are only generalizable to similar mothers (those with vaginal deliveries, full-term singleton infants). Secondly, as with other epidural analyses, breastfeeding outcomes were self-reported and potentially biased, however breastfeeding duration reported within 3 years postpartum is considered reliable and valid [50]. Our breastfeeding cessation endpoint, close to the infants’ birth (≤1 month) minimizes recall bias. Additionally, the original studies were not designed to measure the effect of epidural anesthesia on breastfeeding thus any recall or social desirability biases should be non-differential; mothers are more likely to report longer breastfeeding, thus underestimating the reported effect. This is a secondary analysis. Detailed data for several relevant variables are lacking (e.g. length of second stage of labor; perineal trauma; labor difficulties). Using more detailed data regarding specific intra-partum analgesia agents, length of labor, epidural timing and doses, and concomitant obstetric/labor medication might further clarify this association and increase the validity of risk estimates [27]. Additionally different data collection methods could bias our results. Data missing from electronic records were coded as missing; in paper records data was deemed missing if not available anywhere in the record. Results may measure hospital documentation rather than hospital practice differences. Lastly, the observed association between epidural anesthesia and breastfeeding may be due to unmeasured confounding.
Although social and economic factors are considered major predictors of breastfeeding outcomes, in some circumstances clinical or institutional practices may offset their effect. The association between epidural anesthesia use and BF cessation presented herein, when viewed with other research findings, highlights the complex interrelationships among institutional, clinical, maternal and infant factors. Understanding these relationships, (e.g. potential synergy with IV oxytocin), and the extent to which direct, indirect or no causal relationships are identified, would inform clinical recommendations, hospital policies about labor management and whether and to whom additional breastfeeding support would be advisable. Detailed prospective studies, including a randomized clinical trial if appropriate, that account for a broad array of potential factors and their potential interrelationships are warranted.
References
Ip, S., Chung, M., Raman, G., Chew, P., Magula, N., DeVine, D., et al. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep), 153, 1–186.
Gartner, L. M., Morton, J., Lawrence, R. A., Naylor, A. J., O’Hare, D., Schanler, R. J., et al. (2005). Breastfeeding and the use of human milk. Pediatrics, 115(2), 496–506.
WHO, Unicef, USAID, AED, UCDAVIS, & IFPRI. (2008). Indicators for assessing infant and young child feeding practices. Part I definitions. World Health Organization: Geneva.
Breastfeeding Report Card—United States. (2011). August 11 2011. http://www.cdc.gov/breastfeeding/data/reportcard.htm. Accessed 28 Dec 2011.
Torvaldsen, S., Roberts, C. L., Simpson, J. M., Thompson, J. F., & Ellwood, D. A. (2006). Intrapartum epidural analgesia and breastfeeding: a prospective cohort study. International Breastfeed Journal, 1, 24. Available from: http://www.internationalbreastfeedingjournal.com/content/1/1/24. Accessed 28 Dec 2011 (Internet).
Wilson, M. J., MacArthur, C., Cooper, G. M., Bick, D., Moore, P. A., & Shennan, A. (2010). Epidural analgesia and breastfeeding: A randomised controlled trial of epidural techniques with and without fentanyl and a non-epidural comparison group. Anaesthesia, 65(2), 145–153.
Leighton, B. L., & Halpern, S. H. (2002). The effects of epidural analgesia on labor, maternal, and neonatal outcomes: a systematic review. American Journal of Obstetrics and Gynecology, 186(5 Suppl Nature), S69–S77.
Britton. C., McCormick, F. M., Renfrew, M. J., Wade, A., & King, S. E. (2007). Support for breastfeeding mothers. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD001141. doi:10.1002/14651858.CD001141.pub3.
Dyson, L., McCormick, F. M., & Renfrew, M. J. (2005). Interventions for promoting the initiation of breastfeeding. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD001688. doi:10.1002/14651858.CD001688.pub2.
Abdulwadud, O. A., & Snow, M. E. (2007). Interventions in the workplace to support breastfeeding for women in employment. Cochrane Database of Systematic Reviews, Issue 3. Art. No.: CD006177. doi:10.1002/14651858.CD006177.pub2.
Anim-Somuah, M., Smyth, R. M. D., & Howell, C. J. (2005). Epidural versus non-epidural or no analgesia in labour. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD000331. doi:10.1002/14651858.CD000331.pub2.
Chen, L. K., Hsu, H. W., Lin, C. J., Huang, C. H., Tsai, S. K., Lee, C. N., et al. (2000). Effects of epidural fentanyl on labor pain during the early period of the first stage of induced labor in nulliparous women. Journal of the Formosan Medical Association, 99(7), 549–553.
Baumgarder, D. J., Muehl, P., Fischer, M., & Pribbenow, B. (2003). Effect of labor epidural anesthesia on breastfeeding of healthy full-term newborns delivered vaginally. Journal of the American Board of Family Practice, 16(1), 7–13.
Beilin, Y., Bodian, C. A., Weiser, J., Hossain, S., Arnold, I., Feierman, D. E., et al. (2005). Effect of labor epidural analgesia with and without fentanyl on infant breastfeeding: A prospective, randomized, double-blind study. Anesthesiology, 103(6), 1211–1217.
Henderson, J. J., Dickinson, J. E., Evans, S. F., McDonald, S. J., & Paech, M. J. (2003). Impact of intrapartum epidural analgesia on breastfeeding duration. Australian and New Zealand Journal of Obstetrics and Gynaecology, 43(5), 372–377.
Jordan, S., Emery, S., Bradshaw, C., Watkins, A., & Friswell, W. (2005). The impact of intrapartum analgesia on infant feeding. BJOG, 112(7), 927–934.
Radzyminski, S. (2003). The effect of ultra low dose epidural analgesia on newborn breastfeeding behaviors. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 32(3), 322–331.
Ransjo-Arvidson, A. B., Matthiesen, A. S., Lilja, G., Nissen, E., Widstrom, A. M., & Uvnas-Moberg, K. (2001). Maternal analgesia during labor disturbs newborn behavior: Effects on breastfeeding, temperature, and crying. Birth., 28(1), 5–12.
Riordan, J., Gross, A., Angeron, J., Krumwiede, B., & Melin, J. (2000). The effect of labor pain relief medication on neonatal suckling and breastfeeding duration. Journal of human Lactation, 16(1), 7–12.
Volmanen, P., Valanne, J., & Alahuhta, S. (2004). Breastfeeding problems after epidural analgesia for labour: A retrospective cohort study of pain, obstetrical procedures and breastfeeding practices. International Journal of Obstetrics and Anesthesia, 13(1), 25–29.
Wiklund, I., Edman, G., & Andolf, E. (2007). Cesarean section on maternal request: Reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstetricia et Gynecologica Scandinavica, 86(4), 451–456.
Jordan, S., Emery, S., Watkins, A., Evans, J. D., Storey, M., & Morgan, G. (2009). Associations of drugs routinely given in labour with breastfeeding at 48 hours: Analysis of the Cardiff Births Survey. BJOG, 116(12), 1622–1629.
Chang, Z. M., & Heaman, M. I. (2005). Epidural analgesia during labor and delivery: Effects on the initiation and continuation of effective breastfeeding. Journal of Human Lactation, 21(3), 305–314.
Halpern, S. H., Levine, T., Wilson, D. B., MacDonell, J., Katsiris, S. E., & Leighton, B. L. (1999). Effect of labor analgesia on breastfeeding success. Birth, 26(2), 83–88.
Rosen, A., & Lawrence, R. A. (1994). The effect of epidural anesthesia on infant feeding. Journal of University of Rochester Medical Center, 6(1), 3–7.
Stuebe, A. M., Greenberg, J. A., Ecker, J. L., & McElrath, T. F. (2006). The effects of parity, epidural anesthesia, and cesarean delivery on early breastfeeding. Obstetrics and Gynecology, 107(4 suppl), 68S–69S.
Wieczorek, P. M., Guest, S., Balki, M., Shah, V., & Carvalho, J. C. A. (2010). Breastfeeding success rate after vaginal delivery can be high despite the use of epidural fentanyl: An observational cohort study. International Journal of Obstetric Anesthesia, 19, 273–277.
Devroe, S., De Coster, J., & Van de Velde, M. (2009). Breastfeeding and epidural analgesia during labour. Current Opinion in Anaesthesiology, 22(3), 327–329.
Jonas, K., Johansson, L. M., Nissen, E., Ejdeback, M., Ransjo-Arvidson, A. B., & Uvnas-Moberg, K. (2009). Effects of intrapartum oxytocin administration and epidural analgesia on the concentration of plasma oxytocin and prolactin, in response to suckling during the second day postpartum. Breastfeed Medicine, 4(2), 71–82.
Rahm, V. A., Hallgren, A., Hogberg, H., Hurtig, I., & Odlind, V. (2002). Plasma oxytocin levels in women during labor with or without epidural analgesia: A prospective study. Acta Obstetricia et Gynecologica Scandinavica, 81(11), 1033–1039.
Jonas, W., Nissen, E., Ransjo-Arvidson, A. B., Matthiesen, A. S., & Uvnas-Moberg, K. (2008). Influence of oxytocin or epidural analgesia on personality profile in breastfeeding women: A comparative study. Archives of Women’s Mental Health, 11(5–6), 335–345.
Williams, G. L., Gazal, O. S., Leshin, L. S., Stanko, R. L., & Anderson, L. L. (2001). Physiological regulation of maternal behavior in heifers: Roles of genital stimulation, intracerebral oxytocin release, and ovarian steroids. Biology of Reproduction, 65(1), 295–300.
Slattery, D. A., & Neumann, I. D. (2008). No stress please! Mechanisms of stress hyporesponsiveness of the maternal brain. Journal of Physiology, 586(2), 377–385.
Levy, F., Kendrick, K. M., Keverne, E. B., Piketty, V., & Poindron, P. (1992). Intracerebral oxytocin is important for the onset of maternal behavior in inexperienced ewes delivered under peridural anesthesia. Behavioral Neuroscience, 106(2), 427–432.
Feldman, R., Weller, A., Zagoory-Sharon, O., & Levine, A. (2007). Evidence for a neuroendocrinological foundation of human affiliation: plasma oxytocin levels across pregnancy and the postpartum period predict mother–infant bonding. Psychological Science, 18(11), 965–970.
Montgomery, A., & Hale, T. W. (2006). ABM clinical protocol #15: Analgesia and anesthesia for the breastfeeding mother. Breastfeed Medicine, 1(4), 271–277.
Glantz, C. (2011). Finger Lakes region 2008 statistics 2009 http://www.urmc.rochester.edu/flrpp/summary-reports/index.cfm. Accessed 22 Dec 2011.
Roohan, P. J., Josberger, R. E., Acar, J., Dabir, P., Feder, H. M., & Gagliano, P. J. (2003). Validation of birth certificate data in New York state. Journal of Community Health, 28(5), 335–346.
Northam, S., & Knapp, T. (2006). The reliability and validity of birth certificates. JOGNN, 35(1), 3–12.
DiGiuseppe, D., Aron, D., Random, L., Harper, D., & Rosenthal, G. (2002). Reliability of birth certificate data: A multi-hospital comparison to medical record information. Maternal and Child Health Journal, 6(3), 169–179.
Andersen, P. K., & Gill, R. D. (1982). Cox’s regression model for countin processes: A large sample study. The Annals of Statistics, 10(4), 1110–1120.
Box-Steffensmeier, J. M., & Zorn, C. (2002). Duration models for repeated events. Journal of Politics, 64(4), 1069–1094.
Fleming, T. H., & Harrington, D. P. (1991). Counting processes and survival analysis. New York: Wiley.
Martens, P. J., & Romphf, L. (2007). Factors associated with newborn in-hospital weight loss: Comparisons by feeding method, demographics, and birthing procedures. Journal of Human Lactation, 23(3), 233–241.
Walker, M. (1997). Do labor medications affect breastfeeding? Journal of Human Lactation, 13(2), 131–137.
Mizuno, K., Fujimaki, K., & Sawada, M. (2004). Sucking behavior at breast during the early newborn period affects later breastfeeding rate and duration of breastfeeding. Pediatrics International, 46(1), 15–20.
Dewey, K. G., Nommsen-Rivers, L. A., Heinig, M. J., & Cohen, R. J. (2003). Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics, 112(3 Pt 1), 607–619.
Handlin, L., Jonas, W., Petersson, M., Ejdeback, M., Ransjo-Arvidson, A. B., Nissen, E., et al. (2009). Effects of sucking and skin-to-skin contact on maternal ACTH and cortisol levels during the second day postpartum-influence of epidural analgesia and oxytocin in the perinatal period. Breastfeed Medicine, 4(4), 207–220.
Stricker, B. H., & Stijnen, T. (2010). Analysis of individual drug use as a time-varying determinant of exposure in prospective population-based cohort studies. European Journal of Epidemiology, 25(4), 245–251.
Li, R., Scanlon, K. S., & Serdula, M. K. (2005). The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews, 63(4), 103–110.
Acknowledgments
The authors are grateful to the outstanding assistance provided by Barbara Suter, RN, MPH who coordinated the recruitment and data collection for the TS-1388 project, along with Alice Nelson, Holly Widanka, MA and Jennie Clement who supervised detailed medical record abstraction used for these analyses, the invaluable data management work of Joseph Duckett and the essential input from Dr. Vanessa Stevens on use of the time varying analysis. Data collection funded by: ATPM Cooperative agreement with Centers for Disease Control, Baby-Friendly’s impact on duration and exclusivity; T-1267 (2004–2006); and Prenatal and Peer Breastfeeding Support: Linking Participant Exposure to Results; TS-1388 (2007–2008). Data analysis funded by: NIH PHS Grant # RO1-HD055191, Community Partnership for Breastfeeding Promotion and Support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dozier, A.M., Howard, C.R., Brownell, E.A. et al. Labor Epidural Anesthesia, Obstetric Factors and Breastfeeding Cessation. Matern Child Health J 17, 689–698 (2013). https://doi.org/10.1007/s10995-012-1045-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-1045-4